Abstract
Introduction
Cystic fibrosis (CF) is a life-limiting genetic disease caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene. Elexacaftor/tezacaftor/ivacaftor (ELX/TEZ/IVA) is a CFTR modulator (CFTRm) that targets the underlying cause of CF. Based on safety and efficacy demonstrated in clinical trials, ELX/TEZ/IVA is approved in the US for the treatment of CF in people aged ≥ 2 years who have ≥ 1 F508del-CFTR mutation or a CFTR mutation that is responsive to ELX/TEZ/IVA based on in vitro data. While ELX/TEZ/IVA demonstrated unprecedented improvements in lung function and dramatic reductions in pulmonary exacerbations (PEx) and associated hospitalizations in clinical trials, a limited number of studies have examined the impact of ELX/TEZ/IVA on healthcare resource utilization (HCRU) and associated costs in a real-world setting. The aim of this retrospective study was to evaluate changes in PEx, HCRU, and associated non-CFTRm healthcare costs following initiation of ELX/TEZ/IVA among people with CF aged ≥ 12 years in the US.
Methods
We evaluated the rates of PEx, HCRU, and associated costs before and after initiation of ELX/TEZ/IVA in people with CF aged ≥ 12 years using data from the Merative MarketScan® Commercial Claims and Encounters Database and the Merative Multi-State Medicaid Database from April 21, 2019 to December 31, 2020. Because the study period included time following the onset of the COVID-19 pandemic, we limited our primary analysis to the period prior to the pandemic (October 21, 2019 to March 12, 2020). Outcomes following the onset of the pandemic (March 13 to December 31, 2020) were examined in an exploratory analysis.
Results
In both commercially insured and Medicaid-insured people with CF, ELX/TEZ/IVA was associated with reductions in PEx, hospitalizations, and associated costs prior to the COVID-19 pandemic, and these reductions were maintained following the onset of the pandemic.
Conclusions
These findings suggest that ELX/TEZ/IVA reduces the burden and costs associated with PEx and hospitalizations in people with CF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Elexacaftor/tezacaftor/ivacaftor (ELX/TEZ/IVA) is a combination regimen of cystic fibrosis (CF) transmembrane conductance regulator modulators that has demonstrated safety and efficacy in people with CF in clinical trials. |
A limited number of studies have examined the real-world impact of ELX/TEZ/IVA on healthcare resource utilization (HCRU) and associated healthcare costs. |
In this retrospective analysis, we used US health insurance claims data to evaluate changes in pulmonary exacerbations (PEx), HCRU, and associated healthcare costs following initiation of ELX/TEZ/IVA in people aged ≥ 12 years with CF. |
What was learned from the study? |
ELX/TEZ/IVA was associated with reductions in PEx, hospitalizations, and associated costs. |
Findings suggest that ELX/TEZ/IVA reduces the burden and costs associated with PEx and hospitalizations in people with CF. |
Introduction
Cystic fibrosis (CF) is a life-limiting genetic disease caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene [1, 2]. CF-causing mutations result in reduced quantity and/or function of CFTR ion channels, leading to multisystemic disease characterized by progressive lung function decline, pancreatic insufficiency, nutritional deficits, and other complications [1,2,3]. Despite improvements in standard of care and survival over the past few decades, CF still imposes a substantial healthcare burden on people with CF, their caregivers, as well as society [2, 4,5,6].
Elexacaftor/tezacaftor/ivacaftor (ELX/TEZ/IVA) is a triple combination regimen of CFTR modulators (CFTRm) that targets the underlying cause of CF [7]. It includes ivacaftor, which increases the probability of CFTR ion channels opening at the cell surface, in combination with tezacaftor and elexacaftor, which facilitate the processing and trafficking of CFTR to the cell surface [7]. The safety and efficacy of ELX/TEZ/IVA has been established in nine phase 3 registrational trials, with approximately 900 people with CF aged ≥ 2 years having received ELX/TEZ/IVA; unprecedented improvements have been demonstrated in lung function, reductions in pulmonary exacerbations (PEx) and associated hospitalizations and intravenous (IV) antibiotic use, and improvements in respiratory-related quality of life [8,9,10,11,12,13,14,15]. ELX/TEZ/IVA was initially approved in 2019 by the United States Food and Drug Administration (FDA) for the treatment of CF in people aged ≥ 12 years with ≥ 1 F508del-CFTR mutation [7]; approval was subsequently expanded to include additional CFTR mutations that are responsive to ELX/TEZ/IVA based on in vitro data and to include children aged 2–11 years [16]. In 2021, the US Cystic Fibrosis Foundation Patient Registry (CFFPR) reported that more than 19,000 people with CF in the US were prescribed ELX/TEZ/IVA [4]; therefore it is important to evaluate the effectiveness of ELX/TEZ/IVA beyond the clinical trial setting using real-world studies.
Real-world studies have demonstrated that the use of ELX/TEZ/IVA in routine clinical practice is associated with substantial reductions in hospitalizations and antibiotic use [17,18,19]; however, a limited number of studies have examined the real-world impact of ELX/TEZ/IVA on healthcare resource utilization (HCRU) and associated costs. The aim of this retrospective study was to evaluate changes in PEx, HCRU, and associated non-CFTRm healthcare costs following initiation of ELX/TEZ/IVA among people with CF aged ≥ 12 years in the US.
Methods
Study Design and Data Sources
This retrospective, observational cohort study examined changes in PEx, HCRU, and their associated healthcare costs following initiation of ELX/TEZ/IVA (Fig. 1) using data from the Merative MarketScan® Commercial Claims and Encounters Database and the Merative Multi-State Medicaid Database, the study period was April 21, 2019 to December 31, 2020. The Commercial Claims and Encounters Database comprises healthcare claims and enrolment information from employer-sponsored plans for people in the US aged < 65 years, including employees, their spouses, and dependents. The Multi-State Medicaid Database includes healthcare claims and enrolment information for people in the US with Medicaid managed-care plans or Medicaid fee-for-service plans. Collectively, these databases include information on healthcare encounters for millions of people in the US. The Commercial Claims and Encounters Database and Multi-State Medicaid Database included information on 4249 and 2959 people ≥ 12 years old diagnosed with CF during the study period, respectively. Data from the Merative MarketScan® Medicare Supplemental and Coordination of Benefits Database were not included in the analyses due to the limited sample size (n = 10). The commercially insured and Medicaid-insured cohorts were summarized separately and were not directly compared because these data were (1) from different sources (2) with notably different payment and reimbursement structures (3) which frequently have different sample characteristics. Because all person-level data were fully deidentified, the study protocol was reviewed and deemed exempt from ethical review requirements by Advarra, an institutional review board. All MarketScan data were accessed through a licensing agreement with Merative, Vertex Pharmaceuticals, Inc., and Policy Analysis, Inc.
Baseline data were collected for each person for the 6 months prior to ELX/TEZ/IVA initiation (preindex period). An index date was designated for each person as the date of his or her first dispensed outpatient prescription for ELX/TEZ/IVA. Annualized all-cause HCRU (inpatient admissions and outpatient encounters), PEx (reported overall and by event type), and all-cause healthcare costs (estimated from reimbursed claims) other than those associated with CFTRm were compared during the 6-month period prior to ELX/TEZ/IVA initiation and the period after ELX/TEZ/IVA initiation (postindex period). All individuals were followed until the end of their period of health plan enrolment (reflected in the study database) or December 31, 2020, whichever occurred first.
Because the study period included time following the onset of the COVID-19 pandemic, which impacted HCRU patterns for people with CF and the US population as whole [20,21,22], we excluded people with index dates after March 2020 from the study sample and limited our primary analysis to follow-up data prior to the onset of the pandemic (i.e., prepandemic, postindex period). The prepandemic, postindex period was defined as the period from October 21, 2019 (the date of the initial US FDA approval of ELX/TEZ/IVA [23]), to March 12, 2020 (the day before the COVID-19 pandemic was declared a national emergency in the US [24]); people therefore could contribute a maximum of 5 months of follow-up data prior to the start of the pandemic (Fig. 1). Exploratory analyses examined the period following the onset of the pandemic (i.e., peripandemic, postindex period). The peripandemic, postindex period was defined as the period from March 13 to December 31, 2020; people could contribute a maximum of nine additional months of follow-up data following the onset of the pandemic.
Study Population
People who filled ≥ 1 outpatient prescription for ELX/TEZ/IVA between October 21, 2019 and March 12, 2020, who were ≥ 12 years old on the index date, and diagnosed with CF (based on ≥ 1 diagnosis code for CF [E84x] according to the International Classification of Diseases, 10th revision, during the preindex period or on the index date) were included in the analysis. People with any gaps in health plan enrolment during the 6-month period preceding initiation of ELX/TEZ/IVA were excluded.
Outcomes
Key outcomes included: the number of PEx (overall and by type; i.e., requiring hospitalization and/or antibiotics), number of all-cause hospitalizations and hospital days, number of all-cause outpatient visits (overall and by care setting), and healthcare costs associated with hospitalizations, PEx, and outpatient visits. For those with Medicaid insurance, analyses of costs were limited to people with indemnity plans in which fees are paid for individual services received. PEx were identified based on the occurrence of PEx events defined as: (1) hospitalizations with a diagnosis code for CF with pulmonary manifestations, (2) hospitalizations with a diagnosis code for respiratory infection, (3) ambulatory encounters for IV antibiotic administration, or (4) outpatient prescriptions for oral antibiotics (excluding those used for chronic treatment); this definition is consistent with those of prior claims analyses in CF [5]. A gap of 7 days between hospital discharge or end of antibiotic prescription days (i.e., date of prescription claim + days supplied for oral or inhaled antibiotics; date of encounter + 14 days for IV antibiotics) and subsequent hospitalization or prescription was used to identify unique PEx events; events occurring ≤ 7 days after the end of a previous event were considered part of the same PEx event [5]. Selected non-CFTRm outpatient prescriptions (including antibiotics [inhaled, oral, intravenous, and other types], bronchodilators, antidiabetic agents [long-acting, short-acting, and other insulin agents; and noninsulin agents], antidepressants, antifungals, antihypertensives, anti-inflammatory agents, appetite stimulants, constipation treatments, digestive or pancreatic enzymes, immunosuppressants, mucolytics [dornase alfa, acetylcysteine, hypertonic saline, and mannitol], opioids, ursodeoxycholic acid, and vitamins) were evaluated as an exploratory outcome.
Statistical Analysis
Baseline characteristics were summarized using descriptive statistics. Categorical variables were reported as counts and percentages, and continuous variables were reported as means with standard deviations. Monthly and annualized mean values for PEx, HCRU, and associated healthcare costs were calculated during the preindex and postindex periods; the Kaplan–Meier sample average method [25] was used to calculate monthly mean values during the postindex period, adjusting for differences in the duration of follow-up. Ninety-five percent confidence intervals (CIs) were estimated using nonparametric bootstrapping.
The primary analysis was based on the prepandemic, postindex period (October 21, 2019 through March 12, 2020) to mitigate the impact of the COVID-19 pandemic. Outcomes during the peripandemic, postindex period (March 13 through December 31, 2020) were compared with those during the preindex period in exploratory analyses. Subgroup analyses of the prepandemic, postindex period stratified by age at ELX/TEZ/IVA initiation (12–17 years, 18–26 years, 27–34 years, and ≥ 35 years) and treatment history (prior CFTRm use vs. no prior CFTRm use) were also performed. To evaluate potential confounding due to seasonality, a sensitivity analysis was conducted in which the preindex period began 1 year before the start of the postindex period and ended 1 year before the end of the postindex period. Thus, in this sensitivity analysis, each person contributed the same calendar months of data to the preindex and postindex periods, and only those with health plan enrolment during the preindex period were included. No formal statistical testing was prespecified in the protocol given the size of the study population and time period limitations due to the COVID-19 pandemic. All analyses are descriptive in nature; measures were expressed using means and 95% CIs.
Compliance with Ethical Guidelines
This study was conducted in accordance with the Declaration of Helsinki, the International Society for Pharmacoepidemiology Guidelines for Good Pharmacoepidemiology Practices, and the International Society for Pharmacoeconomics and Outcomes Research Good Practices for Outcomes Research. The study protocol was reviewed and determined exempt from ethical review requirements by an institutional review board because it was limited to the analysis of deidentified data from the Merative MarketScan® Commercial Claims and Encounters Database and the Merative Multi-State Medicaid Database.
Results
Population
A total of 1696 people with CF who had ≥ 1 claim for ELX/TEZ/IVA were identified in the Merative MarketScan® Commercial Claims and Encounters Database (n = 1017) and the Merative Multi-State Medicaid Database (n = 678) (Fig. 2), among whom 851 and 650 people with commercial and Medicaid insurance, respectively, were included in the analysis. Baseline demographics and clinical characteristics are reported in Table 1. Mean age at index was 27.6 years (SD = 11.7 years) in the commercially insured cohort and 21.5 years (SD = 8.2 years) in the Medicaid-insured cohort. Common comorbidities (i.e., prevalence > 20% in either cohort) included pancreatic insufficiency, distal intestinal obstruction syndrome, chronic sinus disease, bronchiectasis, pulmonary illness/infection, diabetes, asthma, gastroesophageal reflux disease, anxiety, pneumonia, and depression. Approximately 58% of the commercially insured cohort and 48% of the Medicaid-insured cohort had received prior treatment with a CFTRm other than ELX/TEZ/IVA. Among people included in this study, ELX/TEZ/IVA initiation among those in the Medicaid-insured cohort lagged slightly behind initiation in the commercially insured cohort (Figure S1 in Supplementary Material). On average, people who initiated ELX/TEZ/IVA earlier were more likely to have prior CFTRm use and tended to have higher disease burden at baseline, with higher rates of PEx and pancreatic insufficiency than in those who initiated later (Figure S2 in Supplementary Material). During the prepandemic, postindex period, the medication possession ratio of ELX/TEZ/IVA was 0.97 (95% CI 0.96, 0.97) in the commercially insured cohort and 0.92 (95% CI 0.91, 0.94) in the Medicaid-insured cohort.
Pulmonary Exacerbations (PEx)
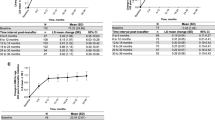
In both the commercially insured and Medicaid-insured cohorts, a decline in the monthly rate of PEx requiring hospitalization or IV antibiotics was observed in the first month following ELX/TEZ/IVA initiation; this reduction was sustained over the 5-month prepandemic, postindex period (Fig. 3A). The mean annualized rate of PEx requiring hospitalization or IV antibiotics decreased by 57.39% (95% CI 46.17, 67.11) in the commercially insured cohort and by 52.18% (95% CI 40.25, 62.43) in the Medicaid-insured cohort from the preindex period to the prepandemic, postindex period (Table 2). Similarly, the mean annualized rate of PEx (all types [i.e., requiring hospitalization, IV antibiotics, or oral antibiotics]) decreased by 34.31% (95% CI 26.64, 42.07) in the commercially insured cohort and by 40.83% (95% CI 32.18, 48.61) in the Medicaid-insured cohort during this time. Comparable trends were also observed for PEx requiring oral antibiotics, with a 19.39% (95% CI 6.95, 31.05) decrease in the commercially insured cohort and a 29.91% (95% CI 15.86, 41.98) decrease in the Medicaid-insured cohort.
Further declines in the rates of PEx were also noted following the onset of the COVID-19 pandemic. Mean rates of PEx requiring hospitalization or IV antibiotics declined by 74.76% (95% CI 68.52, 80.51) in the commercially insured cohort and by 71.58% (95% CI 64.92, 77.27) in the Medicaid-insured cohort, from the preindex period to the peripandemic, postindex period (Table 2). Mean rates of PEx (all types) fell by 68.11% (95% CI 63.75, 72.13) in the commercially insured cohort and by 61.45% (95% CI 56.33, 66.00) in the Medicaid-insured cohort during this time.
Healthcare Resource Utilization: All-Cause Hospitalizations, Outpatient Visits, and Medication Prescriptions
In both the commercially insured and Medicaid-insured cohorts, a decline in the monthly rate of all-cause hospitalizations was observed in the first month following initiation of ELX/TEZ/IVA that was sustained throughout the prepandemic, postindex period (Fig. 3B). In the commercially insured cohort, the mean annualized number of all-cause hospitalizations declined by 57.27% (95% CI 44.29, 68.76), and the mean annualized number of all-cause hospital days declined by 65.24% (95% CI 51.26, 76.01) from the preindex period to the prepandemic, postindex period (Table 3). In the Medicaid-insured cohort, comparable reductions were observed, with a 54.87% decline (95% CI 44.38, 64.75) in all-cause hospitalizations and a 62.76% decline (95% CI 52.10, 72.48) in all-cause hospital days.
After the onset of the pandemic, hospitalizations continued to decline (Table 3). In the commercially insured cohort, the annualized number of all-cause hospitalizations decreased by 71.97% (95% CI 64.47, 78.38) during the peripandemic, postindex period compared with the preindex period, and the corresponding number of hospitalization days decreased by 76.04% (95% CI 67.59, 82.91). In the Medicaid-insured cohort, the annualized number of all-cause hospitalizations decreased by 71.57% (95% CI 63.66, 77.68), and the corresponding number of hospitalization days decreased by 77.47% (95% CI 70.26, 83.00) during the peripandemic, postindex period.
Use of outpatient services was largely unchanged from the preindex period to the prepandemic, postindex period (Table 3). During the peripandemic, postindex period, outpatient visits decreased by 25.00% (95% CI 18.68, 30.83) in the commercially insured cohort and by 15.49% (95% CI 8.31, 22.72) in the Medicaid-insured cohort.
Use of selected non-CFTRm outpatient prescriptions differed by medication class but was largely unchanged between the preindex period and the prepandemic, postindex period in both cohorts (Table S1 in Supplementary Material). During the peripandemic, postindex period, the number of antibiotic prescriptions in the commercially insured cohort decreased by 33.93% (95% CI 26.91, 40.44), and the number of bronchodilator prescriptions decreased by 25.99% (95% CI 15.34, 35.13) compared with the preindex period. In the Medicaid-insured cohort, the number of antibiotic prescriptions decreased by 33.04% (95% CI 25.15, 39.71), and the number of bronchodilator prescriptions decreased by 18.04% (95% CI 8.97, 26.39) from the preindex period to the peripandemic, postindex period. The use of other types of non-CFTRm outpatient prescriptions was largely unchanged between the preindex period and the peripandemic, postindex period.
Healthcare Costs
Costs in US dollars associated with PEx requiring hospitalization or IV antibiotics decreased by 67.80% (95% CI 51.15, 81.50) in the commercially insured cohort (costs reduced by $17,701 per person per year) and by 69.11% (95% CI 49.21, 83.68) in the Medicaid-insured cohort (costs reduced by $26,869 per person per year) from the preindex period to the prepandemic, postindex period (Fig. 4 and Table 4). Similarly, compared with the preindex period, in the prepandemic, postindex period, PEx-related costs (all types) decreased by 67.45% (95% CI 51.76, 81.13), a cost reduction of $17,721 per person per year, in the commercially insured cohort and by 68.48% (95% CI 49.10, 83.07), a cost reduction of $26,766 per person per year, in the Medicaid-insured cohort.
Costs of all-cause hospitalizations decreased following ELX/TEZ/IVA initiation, with a 59.55% decrease (95% CI 36.48, 74.33) in the commercially insured cohort (reduced costs by $20,201 per person per year) and a 69.95% decrease (95% CI 51.87, 83.23) in the Medicaid-insured cohort (reduced costs by $31,038 per person per year) in the prepandemic, postindex period compared with the preindex period (Table 4).
PEx-related costs and all-cause hospitalization costs continued to decline after the onset of the pandemic (Table 4). In both the commercially insured and Medicaid-insured cohorts, costs associated with PEx requiring hospitalization or IV antibiotics and with all types of PEx decreased by approximately 77% in the peripandemic, postindex period compared with the preindex period, corresponding to reduction in costs of $20,074 per person per year in the commercially insured cohort and $30,041 per person per year in the Medicaid-insured cohort. Costs of hospitalizations decreased by 73.71% (95% CI 62.62, 82.48) and 75.06% (95% CI 63.56, 84.45), corresponding to a reduction in costs of $25,007 and $33,304 per person per year for the commercially insured and Medicaid-insured cohorts, respectively.
Costs of outpatient visits were largely unchanged from the preindex period to the prepandemic, postindex period in the Medicaid-insured cohort (Table 4). However, costs of outpatient visits decreased by 18.61% (95% CI 9.11, 24.46) in the commercially insured cohort during this time. Changes in the costs of selected non-CFTRm outpatient prescriptions from the preindex period to the prepandemic, postindex period differed by medication class (Table S2 in Supplementary Material). While costs were largely unchanged in the commercially insured cohort, increases in the costs of some medication types were observed in the Medicaid-insured cohort (Table S2 in Supplementary Material). After the onset of the pandemic, costs of outpatient visits decreased in both the commercially insured cohort (by 43.77% [95% CI 34.36, 52.24]) and Medicaid-insured cohort (by 28.93% [95% CI 20.84, 36.32]) compared with the preindex period (Table 4). In both the commercially insured and Medicaid-insured cohorts, changes in the costs of selected non-CFTRm prescriptions during the peripandemic, postindex period varied by medication class (Table S2 in Supplementary Material). In the commercially insured cohort, costs of antibiotics decreased by 29.10% (95% CI 16.14, 40.20), costs of bronchodilators decreased by 24.44% (95% CI 10.95, 36.57), and costs of mucolytics decreased by 16.52% (95% CI 7.20, 24.87), while the costs of other medication types were unchanged. In the Medicaid-insured cohort, costs of antifungals decreased by 98.67% (95% CI 17.68, 99.58) and costs of appetite stimulants decreased by 47.97% (95% CI 11.77, 68.61), while costs of digestive or pancreatic enzymes increased by 16.18% (95% CI 2.79, 31.83) and costs of other medication types were unchanged.
Subgroup and Sensitivity Analyses
In subgroup analyses stratified by age, the decreases observed in PEx (Table S3 in Supplementary Material), hospitalizations (Table S4 in Supplementary Material), and their associated costs (Table S5 in Supplementary Material) from the preindex period to the prepandemic, postindex period were generally consistent across all age groups. As an exception, reductions in the annualized number of PEx requiring hospitalization or IV antibiotics and in the number of all-cause hospitalizations were not observed among those in the Medicaid-insured cohort aged ≥ 35 years, in contrast to all other age groups. However, reductions in the annualized number of PEx (all types), all-cause hospital days, and costs associated with PEx and hospitalizations were observed in this age group, consistent with reductions in both the primary analysis and other age groups.
In subgroup analyses stratified by prior CFTRm use, consistent reductions in PEx (Table S6 in Supplementary Material), hospitalizations (Table S7 in Supplementary Material), and their associated costs (Table S8 in Supplementary Material) were observed regardless of prior CFTRm use in both the commercially insured and Medicaid-insured cohorts. In seasonality-adjusted sensitivity analyses, the reductions in PEx (Table S9 in Supplementary Material), hospitalizations (Table S10 in Supplementary Material), and associated costs (Table S11 in Supplementary Material) were consistent with the primary analysis.
Discussion
Using data from two healthcare claims databases, results from this retrospective study indicate that use of ELX/TEZ/IVA is associated with reductions in PEx, all-cause hospitalizations, and associated costs among people with CF aged ≥ 12 years during the observed study period. These reductions were largely consistent irrespective of insurance types (commercial vs Medicaid), age, and treatment history (prior CFTRm use vs. no prior use). Overall, this study suggests that ELX/TEZ/IVA can reduce the burden and costs associated with PEx and hospitalizations in people with CF.
High rates of PEx and hospitalizations were noted in the month preceding initiation of ELX/TEZ/IVA therapy. This may be because some people with CF were prescribed ELX/TEZ/IVA following a PEx that required hospitalization. Reductions in the monthly rates of PEx and hospitalization were observed in the first month after ELX/TEZ/IVA initiation compared with the 5 months preceding ELX/TEZ/IVA initiation. These reductions were sustained throughout the prepandemic, postindex period. Reductions in PEx requiring hospitalization or IV antibiotics were broadly consistent with findings from a phase 3 clinical trial among people with CF ≥ 12 years of age with F/MF genotypes, in which treatment with ELX/TEZ/IVA resulted in a 63% reduction in PEx compared with the placebo [8]. In this study, the monthly rates of PEx requiring hospitalization or IV antibiotics and all-cause hospitalizations were higher among the Medicaid-insured cohort compared with the Commercially insured cohort during both the preindex period and prepandemic postindex periods, though the reduction during the postindex period was consistent between the cohorts. These data are also consistent with previous reports and are likely a reflection of the higher disease burden seen in the Medicaid-insured cohort at baseline, which may be explained by the fact that the Medicaid-insured cohort are a more vulnerable patient population due to adverse social determinants of health [26,27,28].
Subgroup analyses demonstrated that decreases in PEx, hospitalizations, and their associated costs were largely consistent across age groups and occurred regardless of prior CFTRm use. However, in contrast to all other age groups, decreases in the annualized number of PEx requiring hospitalization or IV antibiotics or in the number of all-cause hospitalizations were not observed among those in the Medicaid-insured cohort aged ≥ 35 years. It is possible that the relatively small number (n = 43) of people in this age group may have contributed to these discrepancies, but this trend was not observed in commercially insured people of the same age.
After the onset of the COVID-19 pandemic, PEx, hospitalizations, and associated non-CFTRm costs continued to decline in people receiving ELX/TEZ/IVA. Restrictions on social interactions and changes in care-seeking behavior were reported during the pandemic [21, 22] (e.g., avoidance of healthcare settings), and treatment for conditions other than COVID-19 were being postponed if possible [29]. These factors may have contributed to the reductions in PEx and HCRU that were observed following the onset of the pandemic. However, overall trends observed in the peripandemic period were consistent with those observed in the prepandemic period, suggesting that ELX/TEZ/IVA reduced healthcare burden independent of the impact of pandemic-related risk mitigation measures. The reductions in PEx are also consistent with earlier clinical and real-world studies conducted prior to the onset of the COVID-19 pandemic that showed substantial reductions in PEx with ELX/TEZ/IVA [8, 30].
The substantial reductions seen in hospitalizations following ELX/TEZ/IVA initiation could have widespread impact on the healthcare system. In this study, commercially insured people with CF had, on average, nearly five fewer hospital days on an annualized basis following initiation of ELX/TEZ/IVA. An even larger reduction of 11 fewer hospital days was observed among those with Medicaid insurance. To estimate the impact this reduction in hospital days among people with CF could have on the healthcare system more broadly, we multiplied the per-person reductions in hospital days observed in this study by estimates from the CFFPR of the population of people with CF aged ≥ 12 years who are eligible for ELX/TEZ/IVA. When projected to the total eligible population in this manner, ELX/TEZ/IVA initiation is projected to result in 14,924 and 17,250 fewer hospital days per year for commercially insured and Medicaid-insured people with CF, respectively. This suggests that, despite the relatively small proportion of people in the US with CF, treatment with ELX/TEZ/IVA may have a meaningful impact on hospital utilization.
The number of outpatient visits and the use of non-CFTRm outpatient prescriptions were, for the most part, unchanged following initiation of ELX/TEZ/IVA treatment up to the onset of the COVID-19 pandemic; thereafter, however, use of antibiotics and bronchodilators decreased. Trends in costs associated with outpatient visits and non-CFTRm outpatient prescriptions were mixed. The relatively short follow-up in the postindex, prepandemic period (5 months) may have limited changes in outpatient prescription patterns due to the routine care plan followed by people with CF, consistent with current CF care guidelines, which do not recommend withdrawing standard-of-care therapies following a prescription for a CFTRm [31]. Further studies with longer follow-up may show a trend towards withdrawal of standard-of-care therapies because emerging evidence has shown, for example, that the use of inhaled mucoactive therapies may not be required to maintain pulmonary function with ELX/TEZ/IVA [32].
The observed reductions in PEx, hospitalizations, and associated costs, taken together with the substantial and clinically meaningful improvements in lung function, nutritional parameters, and quality of life observed in previous studies [8,9,10,11, 33], suggest that, overall, ELX/TEZ/IVA provides meaningful benefit to people with CF.
Several limitations should be considered. First, this study focused on the impact of ELX/TEZ/IVA use on the costs associated with PEx and HCRU. As all people included in the study were receiving ELX/TEZ/IVA treatment, ELX/TEZ/IVA costs were not required to address our research objectives. Additionally, because this study was limited to administrative claims data from people with commercial, employer-sponsored insurance or Medicaid in the US, findings may not be generalizable to people lacking health insurance, those with other forms of insurance, or to those outside the US. ELX/TEZ/IVA initiation was identified from October 21, 2019 through March 12, 2020. As a result, people with the longest duration of follow-up are those who initiated ELX/TEZ/IVA earliest. Earlier initiators tended to have higher disease burden at baseline (i.e., prior to ELX/TEZ/IVA initiation) than those who initiated ELX/TEZ/IVA later. Because all individuals contributed an equal amount of data to the preindex period, while the earliest initiators contributed the longest follow-up to the postindex period, the experience of sicker people may be overrepresented in the postindex period, resulting in a biased estimate of the impact of ELX/TEZ/IVA. Additionally, because this study was limited to people who initiated ELX/TEZ/IVA prior to March 12, 2020, and all people were required to have continuous enrollment, the results may not be fully generalizable to all people with CF who are eligible for ELX/TEZ/IVA and we are unable to make any conclusions about patients without continuous healthcare plan enrollment. Finally, the duration of follow-up also limits exploration of impacts of ELX/TEZ/IVA on outpatient clinic visits and non-CFTRm prescription trends. As longer-term follow-up data become available, further research may inform any conclusions around the impact of ELX/TEZ/IVA on HCRU over the longer term.
Conclusions
Overall, the substantial reductions in PEx, hospitalizations, and their associated costs suggest that ELX/TEZ/IVA reduces the burden and costs associated with PEx and hospitalization in people with CF. These findings add to the body of evidence demonstrating that ELX/TEZ/IVA provides substantial benefits to people with CF and support its value in treating CF.
Data Availability
The datasets analyzed in this study are available from Merative: https://www.ibm.com/products/marketscan-research-databases.
References
Bell S, Mall M, Gutierrez H, Macek M, Madge S, Davies J, et al. The future of cystic fibrosis care: a global perspective. Lancet Respir Med. 2020;8(1):65–124.
Elborn J. Cystic fibrosis. Lancet. 2016;388(10059):2519–31.
Ratjen F, Bell S, Rowe S, Goss C, Quittner A, Bush A. Cystic fibrosis. Nat Rev Dis Primers. 2015;1:15010.
Cystic Fibrosis Foundation. Cystic Fibrosis Foundation Patient Registry 2021 Annual Data Report. https://www.cff.org/medical-professionals/patient-registry. Accessed 10 Nov 2022.
Hassan M, Bonafede M, Limone B, Hodgkins P, Sawicki G. The burden of cystic fibrosis in the Medicaid population. Clinicoecon Outcomes Res. 2018;10:423–31.
Thorat T, McGarry L, Bonafede MM, Limone BL, Rubin JL, Jariwala-Parikh K, et al. Healthcare resource utilization and costs among children with cystic fibrosis in the United States. Pediatr Pulm. 2021;56(9):2833–44.
Trikafta (elexacaftor/tezacaftor/ivacaftor). Prescribing information. Boston: Vertex Pharmaceuticals Incorporated. Revised October 2019.
Middleton P, Mall M, Dřevínek P, Lands L, McKone E, Polineni D, et al. Elexacaftor–tezacaftor–ivacaftor for cystic fibrosis with a single phe508del allele. N Engl J Med. 2019;381(9):1809–19.
Heijerman H, McKone E, Downey D, Van Braeckel E, Rowe S, Tullis E, et al. Efficacy and safety of the elexacaftor plus tezacaftor plus ivacaftor combination regimen in people with cystic fibrosis homozygous for the F508del mutation: a double-blind, randomised, phase 3 trial. Lancet. 2019;394(10212):1940–8.
Barry P, Mall M, Álvarez A, Colombo C, de Winter-de Groot K, Fajac I, et al. Triple therapy for cystic fibrosis Phe508del-gating and -residual function genotypes. N Engl J Med. 2021;385(9):815–25.
Zemanick E, Taylor-Cousar J, Davies J, Gibson R, Mall M, McKone E, et al. A phase 3 open-label study of elexacaftor/tezacaftor/ivacaftor in children 6 through 11 years of age with cystic fibrosis and at least one F508del allele. Am J Respir Crit Care Med. 2021;203(12):1522–32.
Goralski JL, Hoppe JE, Mall MA, McColley SA, McKone E, Ramsey B, et al. Phase 3 open-label clinical trial of elexacaftor/tezacaftor/ivacaftor in children aged 2–5 years with cystic fibrosis and at least one F508del allele. Am J Respir Crit Care Med. 2023;208(1):59–67.
Griese M, Tullis E, Chilvers MA, et al. Long-term safety and efficacy of elexacaftor/tezacaftor/ivacaftor in people with cystic fibrosis and at least one F508del allele: 144-week interim results from an open-label extension study. Poster presented at North American Cystic Fibrosis Conference. Nov 3–5, 2022, Philadelphia, PA.
Chmiel J, Barry PJ, Colombo C, et al. Long-term safety and efficacy of elexacaftor/tezacaftor/ivacaftor in people with cystic fibrosis heterozygous for F508del-CFTR and a gating or residual function mutation. Poster presented at North American Cystic Fibrosis Conference. Nov 3–5, 2022, Philadelphia, PA.
Wainwright CE, McColley SA, McNally P, Powers MR, Ratjen FA, Rayment JH, et al. Long-term safety and efficacy of elexacaftor/tezacaftor/ivacaftor in children aged ≥6 years with cystic fibrosis and at least one F508del allele: a phase 3, open-label clinical trial. Am J Respir Crit Care Med. 2023;2018(1):68–78.
Trikafta (elexacaftor/tezacaftor/ivacaftor). Prescribing information. Boston: Vertex Pharmaceuticals Incorporated. Revised October 2023.
Smith S, Borchardt M. Analyzing the use and impact of elexacaftor/tezacaftor/ivacaftor on total cost of care and other health care resource utilization in a commercially insured population. J Manag Care Spec Pharm. 2022;28(7):721–31.
Miller A, Harris L, Cavanaugh J, Alaiwa M, Stoltz D, Hornick D, et al. The rapid reduction of infection-related visits and antibiotic use among people with cystic fibrosis after starting elexacaftor-tezacaftor-ivacaftor. Clin Infect Dis. 2022;75(7):1115–22.
Bower JK, Volkova N, Ahluwalia N, Sahota G, Xuan F, Chin A, et al. Real-world safety and effectiveness of elexacaftor/tezacaftor/ivacaftor in people with cystic fibrosis: interim results of a long-term registry-based study. J Cyst Fibros. 2023. https://doi.org/10.1016/j.jcf.2023.03.002.
Albon D, Bruschwein H, Soper M, List R, Jennings D, Gettle L, et al. Impact of COVID-19 on social determinants of health for adults with cystic fibrosis. Ther Adv Respir Dis. 2021;15:17534666211037459.
Hong K, Zhou F, Tsai Y, Jatlaoui T, Acosta A, Dooling K, et al. Decline in receipt of vaccines by Medicare beneficiaries during the COVID-19 pandemic—United States, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(7):245–9.
Xu S, Glenn S, Sy L, Qian L, Hong W, Ryan D, et al. Impact of the COVID-19 pandemic on health care utilization in a large integrated health care system: retrospective cohort study. J Med Internet Res. 2021;23(4): e26558.
US Food and Drug Administration. FDA approves new breakthrough therapy for cystic fibrosis. News release https://www.fda.gov/news-events/press-announcements/fda-approves-new-breakthrough-therapy-cystic-fibrosis. Accessed 8 Nov 2022.
US Federal Emergency Management Agency. Bringing Resources to State, Local, Tribal & Territorial Governments. https://www.fema.gov/disaster/coronavirus/governments Accessed 8 Nov 2022.
Lin D, Feuer E, Etzioni R, Wax Y. Estimating medical costs from incomplete follow-up data. Biometrics. 1997;53(2):419–34.
Schechter MS, Shelton BJ, Margolis PA, Fitzsimmons SC. The association of socioeconomic status with outcomes in cystic fibrosis patients in the United States. Am J Respir Crit Care Med. 2001;163(6):1331–7.
Sanders DB, Ostrenga JS, Rosenfeld M, Fink AK, Schechter MS, Sawicki GS, et al. Predictors of pulmonary exacerbation treatment in cystic fibrosis. J Cyst Fibros. 2020;19(3):407–14.
Schechter MS, McColley SA, Regelmann W, Millar SJ, Pasta DJ, Wagener JS, et al. Socioeconomic status and the likelihood of antibiotic treatment for signs and symptoms of pulmonary exacerbation in children with cystic fibrosis. J Pediatr. 2011;159(5):819–24 e1.
Gertz AH, Pollack CC, Schultheiss MD, Brownstein JS. Delayed medical care and underlying health in the United States during the COVID-19 pandemic: a cross-sectional study. Prev Med Rep. 2022;28: 101882.
Dwight M, Marshall B. CFTR modulators: transformative therapies for cystic fibrosis. J Manag Care Spec Pharm. 2021;27(2):281–4.
Ren CL, Morgan RL, Oermann C, Resnick HE, Brady C, Campbell A, et al. Cystic Fibrosis Foundation pulmonary guidelines: use of cystic fibrosis transmembrane conductance regulator modulator therapy in patients with cystic fibrosis. Ann Am Thorac Soc. 2018;15(3):271–80.
Mayer-Hamblett N, Ratjen F, Russell R, Donaldson SH, Riekert KA, Sawicki GS, et al. Discontinuation versus continuation of hypertonic saline or dornase alfa in modulator treated people with cystic fibrosis (SIMPLIFY): results from two parallel, multicentre, open-label, randomised, controlled, non-inferiority trials. Lancet Respir Med. 2023;11(4):329–40.
Sutharsan S, McKone E, Downey D, Duckers J, MacGregor G, Tullis E, et al. Efficacy and safety of elexacaftor plus tezacaftor plus ivacaftor versus tezacaftor plus ivacaftor in people with cystic fibrosis homozygous for F508del-CFTR: a 24-week, multicentre, randomised, double-blind, active-controlled, phase 3b trial. Lancet Respir Med. 2022;10(3):267–77.
Medical Writing and Editorial Assistance
Medical writing and editorial support were provided under the direction of the authors by Jackie Highland, PhD, CMPP, of ArticulateScience LLC, which received funding from Vertex Pharmaceuticals Incorporated.
Funding
The journal’s Rapid Service Fee and this study were funded by Vertex Pharmaceuticals Incorporated, Boston, MA, USA.
Author information
Authors and Affiliations
Contributions
Michael S. Schechter, Natalia Sabater-Anaya, Gerry Oster, Derek Weycker, Emilio Arteaga-Solis, Sukirti Bagal, Lisa J. McGarry, Kate Van Brunt, and Jessica Morlando Geiger contributed to the conceptualization or design of the study, and to data analysis and/or the interpretation. Hongsheng Wu contributed to data acquisition, analysis, and interpretation. All authors reviewed and critically revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
All authors received nonfinancial support (assistance with manuscript preparation) from ArticulateScience LLC, which was funded by Vertex Pharmaceuticals. Additional disclosures are as follows: Michael S. Schechter reports consulting fees and grants to his institution from Vertex Pharmaceuticals; grants to his institution from GSK, the US Cystic Fibrosis Foundation, and National Institutes of Health; speaker fees from Sanofi; participation on an advisory or safety monitoring board for AstraZeneca; payments for participation on US Cystic Fibrosis Foundation committees; unpaid participation on the US Cystic Fibrosis Foundation Virginia Chapter Board of Directors; and personal payments for expert testimony in malpractice litigation. Natalia Sabater-Anaya, Gerry Oster, Derek Weycker, and Hongsheng Wu are employees of Policy Analysis Inc., which received research funding from Vertex Pharmaceuticals. Emilio Arteaga-Solis, Lisa J. McGarry, Kate Van Brunt, and Jessica Morlando Geiger are employees of Vertex Pharmaceuticals and may own stock or stock options in that company. Sukirti Bagal was a former employee of Vertex Pharmaceuticals and is now an employee of Celldex Therapeutics and may own stock or stock options in that company.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki, the International Society for Pharmacoepidemiology Guidelines for Good Pharmacoepidemiology Practices, and the International Society for Pharmacoeconomics and Outcomes Research Good Practices for Outcomes Research. The study protocol was reviewed and determined exempt from ethical review requirements by an institutional review board because it was limited to the analysis of deidentified data from the Merative MarketScan® Commercial Claims and Encounters Database and the Merative Multi-State Medicaid Database.
Additional information
Prior Presentation: Results from this study were previously presented at the AMCP Nexus 2022 annual meeting, National Harbor, MD, October 11–14, 2022.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Schechter, M.S., Sabater-Anaya, N., Oster, G. et al. Impact of Elexacaftor/Tezacaftor/Ivacaftor on Healthcare Resource Utilization and Associated Costs Among People With Cystic Fibrosis in the US: A Retrospective Claims Analysis. Pulm Ther 9, 479–498 (2023). https://doi.org/10.1007/s41030-023-00241-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-023-00241-z