Abstract
Introduction
Normothermic ex vivo lung perfusion (EVLP) is used to evaluate and condition donor lungs for transplantation. The objective of this study was to determine whether administration of exogenous nitric oxide during EVLP contributes to improvement of lung health.
Methods
A multicenter, blinded, two-arm, randomized pilot study evaluated the effect of gaseous nitric oxide (gNO) administered during EVLP on donor lungs rejected for transplantation. gNO introduced into the perfusate at 80 parts per million (ppm) was compared with perfusate alone (P). An open-label substudy assessed inhaled nitric oxide gas (iNO) delivered into the lungs at 20 ppm via a ventilator. Primary endpoints were an aggregate score of lung physiology indicators and total duration of stable EVLP time. Secondary endpoints included assessments of lung weight and left atrium partial pressure of oxygen (LAPO2).
Results
Twenty bilateral donor lungs (blinded study, n = 16; open-label substudy, n = 4) from three centers were enrolled. Median (min, max) total EVLP times for the gNO, P, and iNO groups were 12.4 (8.6, 12.6), 10.6 (6.0, 12.4), and 12.4 (8.7, 13.0) hours, respectively. In the blinded study, median aggregate scores were higher in the gNO group compared to the P group at most time points, suggesting better lung health with gNO (median score range [min, max], 0–3.5 [0, 7]) vs. P (0–2.0 [0, 5] at end of study). In the substudy, median aggregate scores did not improve for lungs in the iNO group. However, both the gNO and iNO groups showed improvements in lung weight and LAPO2 compared to the P group.
Conclusions
The data suggest that inclusion of gNO during EVLP may potentially prolong duration of organ stability and improve donor lung health, which warrants further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out the study? |
There is a substantial unmet need for patients with end-stage lung disease resulting from a shortage of lifesaving transplantable lungs, partially due to high discard rates. |
This study sought to determine whether ex vivo lung perfusion (EVLP), an evolving approach used to assess and recondition otherwise unsuitable donor lungs, showed a greater improvement in lung health with the addition of gaseous nitric oxide (gNO) to the perfusate or with inhaled nitric oxide (iNO) via a ventilator. |
What was learned from the study? |
Compared with lungs treated with perfusate alone, the addition of gNO to the perfusate improved the health of donor lungs, as demonstrated by an increased aggregate score of lung physiology, whereas administration of iNO via the ventilator did not; however, both gNO and iNO appeared to provide some beneficial effects on lung weight and oxygenation. |
These results support ongoing research regarding the possible inclusion of gNO during EVLP to potentially increase the number of suitable donor lungs for transplantation. |
Introduction
Lung transplantation is the solitary lifesaving treatment for patients with end-stage lung disease, and there remains a large gap between demand and supply. Over the last two decades, end-stage lung disease has grown to be the third leading cause of disease-related death in the US [1] and has likely become even more prevalent during the global COVID-19 pandemic. Although the lung transplant numbers are increasing every year, so too is the waiting list. In 2018, 3134 candidates were added to the U.S. lung waitlist, which was a 42% increase from 2008 [2]. This issue is further complicated by the high discard rates of donated lungs (only about 20–25% of lungs from multiorgan donors are transplanted) [3, 4]. Ultimately, in the US, 10–20% of patients listed for lung transplantation die before a suitable donor lung is found and many more patients dying of lung disease are never listed [5, 6].
Ex vivo lung perfusion (EVLP) is an evolving approach that may be used to assess and repair otherwise unsuitable donor lungs [5, 7,8,9,10]. EVLP has been shown to aid in the assessment of potential donor lungs and help with reconditioning of marginal or unacceptable lungs, thus potentially expanding the donor pool [11,12,13]. EVLP also allows for the treatment of lungs with adjuncts including anti-inflammatory gene therapy (interleukin [IL]-10) [14, 15], antibiotics or antifungals [16], surfactant lung lavage [17], and exogenous surfactant replacement [18]. Despite the promise of EVLP, discard rates of perfused lungs following EVLP remain high [19, 20].
Endogenous production of nitric oxide (NO) decreases during lung transplantation, and exogenous delivery of NO has vasodilatory, anti-inflammatory, and anti-apoptotic effects in the lung transplant setting [21,22,23,24,25,26]. NO ventilation of rat lungs during ischemia, during ex vivo perfusion, and after transplant has suggested beneficial effects from NO [27]. Thus, it is hypothesized that administration of NO during EVLP could have a positive effect on donor lungs [4, 21,22,23,24,25,26].
The primary objective of this proof-of-concept pilot study was to investigate the effects of dissolved gaseous NO (gNO) in the EVLP perfusate on the health of donor lungs during EVLP. A substudy including inhaled NO via the ventilator (iNO) was also performed. We hypothesized that administration of gNO during EVLP would prolong the stability of lungs while on EVLP, improve lung physiologic health, and attenuate overall lung injury.
Methods
Study Design
This was a randomized, multicenter, blinded, two-arm, proof-of-concept pilot study conducted at Duke University Medical Center, the University of Pittsburgh Medical Center, and the University of Texas Southwestern Medical Center. This study was conducted in agreement with the Declaration of Helsinki and the Declaration of Istanbul, and was in strict compliance with the International Society for Heart and Lung Transplantation (ISHLT) guidelines for transplant ethics. Lungs utilized for research from deceased donors, such as those procured for this study, do not meet the requirement for human subjects and are exempt from Institutional Review Board (IRB) approval. Each investigator obtained an IRB exemption from their institution before initiating the study, including the Duke University Health System IRB, the University of Pittsburgh IRB, and the University of Texas Southwestern Medical Center IRB.
Randomization was performed by unblinded statisticians and implemented via the IBM Clinical Development system at each of the three study centers before the lungs were procured; treatment groups remained blinded through the end of perfusion. Three independent, blinded evaluators carried out the lung suitability assessments (the study-site investigator, a trained independent observer at the study site, and a trained, central reader).
The effects of gNO plus perfusate (acellular STEEN solution™) on donor lungs perfused ex vivo were compared to perfusate alone (P). The study group received gNO (80 parts per million [ppm]) delivered into the perfusate via the membrane oxygenator on the XVIVO Perfusion System (XPS™), while the control group received standard perfusate alone. The gNO was provided by INO Therapeutics. An open-label substudy was also performed that included four bilateral donor lungs not considered transplantable. These lungs received iNO (20 ppm) directly via the ventilatory system along with perfusate in the XPS device. The comparator for the open-label substudy was the gNO group from the randomized study. A higher concentration (80 ppm) of gNO was used in the randomized blinded study because gNO was indirectly administered to the lungs via the oxygenator in the XPS device. A lower concentration of gNO (20 ppm) was used in the open-label substudy because gNO was administered directly to the lungs via the ventilator.
All lungs were kept on the perfusion devices for a minimum of 6 h. Physiologic measurements were recorded every hour during perfusion. If the delta PO2 (pulmonary vein partial pressure of oxygen − pulmonary artery partial pressure of oxygen) was < 200 mmHg and the static compliance of the lungs (CSTAT) decreased by > 20% of the baseline value on two consecutive assessments after 6 h of EVLP, the lungs were considered nonviable and EVLP was terminated.
Study Population
Inclusion criteria were based on modified inclusion criteria for standard donor organs but considered not suitable for human transplantation. All the enrolled lungs had been declined for human transplant for quality concerns (e.g., low arterial partial pressure of oxygen to fraction of inspired oxygen ratio [PaO2/FiO2], pulmonary edema) after proceeding through the match run and were offered for research purposes by the responsible organ procurement organization. Enrolled lungs were required to be bilateral grafts from brain-dead donors aged 18 to 70 years and without evidence of sepsis, significant trauma, or history of major thoracic surgery and malignancy. A PaO2 between 150 and 400 mmHg with positive end-expiratory pressure (PEEP) of 5 cm H20 on a FiO2 of 1.0 was also required. Lungs were declined for the study if there was evidence of significant lobar consolidation, moderate or worse emphysema, and/or significant pulmonary edema.
The EVLP Process
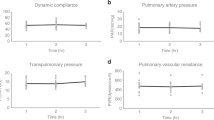
An overview of the EVLP process is illustrated in Fig. 1 and was consistent with standard clinical XPS use. The gas oxygenator was connected to a tank with a gas mixture of oxygen (6%), carbon dioxide (8%), and nitrogen (86%). The lungs were gradually rewarmed over a period of 45 min. Lung perfusion was begun at a flow rate of 0.10 to 0.15 L/min and gradually increased in parallel with rewarming to a final pulmonary artery delivery of 40% of the estimated cardiac output for the donor (at 70 mL/kg/min). Pulmonary artery pressure was targeted to remain below 20 mmHg and left atrium pressure less than 5 mmHg. During the rewarming phase, oxygen supply to the graft was delivered by the membrane oxygenator. Catheters were placed in situ to continuously measure pulmonary artery and left atrium pressure through the EVLP process. Mechanical ventilation of the lungs was initiated when the temperature of the perfusate from the left atrial cuff reached 32 °C. The static and dynamic compliance of the lungs were continuously monitored, in addition to other parameters including pulmonary vascular resistance (PVR) and left atrium partial pressure of oxygen (LAPO2).
A concentration of 80 ppm gNO was administered via the oxygenator of the XPS device in the randomized study, and a sham was included for the control (P) group. All EVLP participants were blinded to the intervention. For the open-label substudy, iNO was administered via the ventilator of the XPS device at 20 ppm, which is the recommended dose for iNO, commonly used in clinical practice. A higher concentration (80 ppm) of gNO was used in the blinded study to compensate for indirect administration of gNO with the oxygenator. Doses of iNO up to 80 ppm were previously used in a live animal study [28].
Endpoints
The two a priori primary endpoints were: (1) health of the perfused lungs measured at baseline (1 h following initiation of EVLP) and at hours 2, 3, 4, 5, 6, 8, 10, and end of study (EOS) using a novel Graded System Aggregate Score composed of delta PO2, CSTAT, and PVR where 0 = worst possible outcome and 10 = best possible outcome (Table 1), and (2) the average EVLP time for each cohort of lungs. The scoring system is novel but was defined a priori based on standard evaluated physiologic parameters used to assess lung health on EVLP. All lungs were perfused for a minimum of 6 h. After 6 h, if the lungs met predetermined end parameters defined above, they were removed from EVLP.
Secondary endpoints included clinical assessments of transplantation suitability (at hours 4 and 6, and EOS), LAPO2, and change in lung weight from baseline during EVLP.
Histologic evaluations were carried out on each lung at the time of organ procurement, at 1 and 4 h following the start of EVLP, and again at the end of the study. The severity of alveolar injury, interstitial/vascular changes, and apoptosis/necrosis were each graded by 2 blinded, trained pathologists on a four-point scale as 0, absent; 1, mild; 2, moderate; and 3, severe. The sum of these parameter scores resulted in a lung injury score (LIS), which could range from 0 to 12. Similar approaches have previously been used for assessment of lung injury following EVLP via histologic assessments or quantitation of inflammation markers in perfusate [29, 30]. The left atrial partial pressure of oxygen (LAPO2) and changes in lung weight from baseline were documented at specified time points during EVLP.
Statistical Analysis
Summary descriptive statistics were determined for numeric or continuous variables. For categorical variables, frequency and percentages were calculated. Due to the small sample size of this proof-of-concept pilot study, it was not sufficiently powered to determine statistical significance between treatment groups.
Results
Donor Lungs
Twenty bilateral lungs were enrolled across three study centers. Sixteen were included in the blinded study and four were in the open-label substudy. In aggregate, randomization worked well, as both groups were overall similar in baseline demographic features (Table 2). The mean donor age and LAPO2 at the time of study inclusion were lowest for the gNO group at 40.5 years and 319.3 mmHg, respectively, compared to 46.5 years and 379.5 mmHg, respectively, for the P group.
Primary Endpoints
In the randomized blinded study, gNO lungs had higher median grading system aggregate scores than the P controls, except at hours 2, 8, and 10, when both groups scored equally (Fig. 2). At hour 6, the final hour at which all lungs were still enrolled, the median score was 1.5 for the gNO lungs, compared to 0 for the control. In the substudy, median aggregate scores for the gNO group were consistently higher than the iNO group, except at hour 8. Aggregate scores are charted for every donor lung at each time point in Supplementary Fig. 1. The results for the individual components of the aggregate score at each time point are presented in Supplementary Table 1.
The median organ stability while on EVLP time was longer for lungs in the gNO group (12.4 h) compared with lungs in the P group (10.6 h; Table 3). No clinically meaningful difference was observed for EVLP time in the open-label substudy comparing gNO with iNO. The percentage change in delta PO2 from baseline showed increases for both NO groups except at 8 h in the iNO group (Table 3). At every time point, the gNO group demonstrated higher mean delta PO2 change from baseline compared to control.
Secondary Endpoints
More lungs were found suitable for transplantation by the site investigator than by the other observers during the course of the study (Table 4). In the blinded study, 43.8% (7/16) of total lungs in the gNO and P groups together were judged suitable for transplantation by the site investigator at hour 4 vs. 18.8% (3/16) and 31.3% (5/16) of lungs judged by the independent site observer and central observer, respectively. The suitability for transplant of the donor lungs peaked at hour 6, when lungs found suitable for transplantation in the blinded study were 60.0%, 18.8% and 13.3% by the site investigator, independent reader, and central reader, respectively. However, by the EOS, the suitability dropped to 25% by the site investigator and 18.8% by both other observers. Overall, evaluators did not find a notable difference in the suitability of perfused lungs between the gNO and control cohorts. The proportion of lungs from the iNO group found suitable for transplantation at hour 4 was 50% (2/4) by both the site investigator and the independent site observer and 25% (1/4) by the central observer. However, at hour 6 and EOS, none of the iNO lungs were found suitable for transplantation.
In the blinded study, mean LAPO2 tended to increase from baseline during EVLP in the gNO group, whereas the control group generally showed a decrease at each point through 6 h (Fig. 3). In the substudy, the iNO group demonstrated modest increases in LAPO2 from baseline during EVLP, except at hour 6 where the change was −2.8 mmHg (Supplementary Fig. 2).
Mean wet lung weight in the gNO group increased from 1406.9 g at baseline to 1604.3 g at end of EVLP; in the P group, mean weight increased from 1615.6 to 2255.6 g. The mean change (increase) in lung weight from baseline through hour 6 of EVLP was lower at each timepoint for the gNO group vs. the P group (Fig. 4). In the substudy, mean wet lung weight in the iNO group was 3881.3 g at baseline and substantially decreased through hour 6 of EVLP (Supplementary Fig. 3).
Results of histologic lung injury score analysis following EVLP are described in Supplementary Table 2. All three study groups showed decreasing mean LIS during EVLP, although no meaningful differences were seen between the groups. The mean (SD) score decreased from 4.3 (1.0) prior to initiation of EVLP to 2.3 (0.9) at end of study in the gaseous nitric oxide group (gNO), and from 4.1 (1.6) prior to EVLP to 1.5 (0.8) at end of study in the perfusate-only (control, P) group. A similar trend was observed in the inhaled nitric oxide group (iNO) in the open-label substudy, with mean (SD) scores decreasing from 4.0 (1.4) prior to EVLP to 2.3 (0.5) at end of study. It was concluded that the EVLP process resulted in overall improvement of the lung injury score, both in the absence or presence of exogenous nitric oxide.
Discussion
The demand for transplantable lungs far exceeds the supply due to a shortage of suitable organs [2, 31]. The process of EVLP helps mitigate this by increasing the proportion of donor lungs suitable for transplantation [8, 9, 31]. Even so, discard rates of perfused lungs following EVLP remain high and the overall impact on organ availability has been relatively muted [19, 20]. Part of the appeal of EVLP resides in the potential for addition of adjuncts to the perfusate that may have a beneficial impact on the health of the graft. The administration of NO has shown benefits in other areas of lung transplantation and injury and was hypothesized to have a positive effect on lungs during EVLP [4, 21,22,23,24,25,26].
The lungs recruited in this pilot study had been rejected for transplantation after attempts at organ allocation by the respective organ procurement organizations. It is important to realize that these pulmonary allografts were also deemed unsuitable for clinical EVLP, which highlights a challenge in performing research on discarded lungs not intended for transplantation. In these otherwise unacceptable organs, the addition of gNO during the EVLP process showed a potential improvement of overall lung health, while in contrast, there was a deterioration in the health of lungs treated with perfusate alone. Importantly, the duration of stable EVLP time was maintained longer in lungs treated with NO vs. those that received perfusate alone. In severely damaged lungs, the addition of NO to the perfusate may slow or delay deterioration of the allograft during EVLP. The lungs in both NO groups demonstrated a mean increase from baseline delta PO2 at almost every EVLP time point, suggesting that the introduction of exogenous gNO may improve the ability of lungs to oxygenate. Given that PaO2 is important for decision-making for use of marginal lungs in transplantation, responsiveness to gNO through improvement in PaO2 could be a meaningful assessment to predict integrity of the alveolar-capillary membrane and overall quality of the allograft. Another positive observation was the delta weight of the lungs. Although both study groups in the randomized blinded study showed an increase in lung weight as perfusion progressed, the gNO group exhibited a lower increase in lung weight compared to P alone. However, despite the promising findings presented here, it should be noted that no substantial differences in organ suitability between gNO and control groups were noted by blinded evaluators.
One unexpected result was the disparity of findings among evaluators, with the on-site evaluator consistently finding a greater proportion of lungs to be suitable for transplantation than other observers. According to the on-site EVLP specialist, 45% of the rejected lungs were appropriate for human transplantation after 4 h of perfusion. This is clinically relevant, as the community considers different logistics to organ perfusion (i.e., remote perfusion centers, on-site perfusion, or portable devices). It may be beneficial for multiple trained personnel, in addition to the procuring surgeon or EVLP specialist, to carry out evaluations for transplantation suitability. Clearly, there is variability in terms of what constitutes a usable pulmonary allograft with or without the use of EVLP, and more definitive objective data are needed to make the process less subjective. The novel aggregate donor score provided in this study is one example of a possible objective scoring system to judge lungs during EVLP. Validated clinical parameters may provide the best real-time assessment for organ usability, although the determination of lungs to be suitable for transplant will continue to be center/surgeon-specific.
It is important to highlight that despite the differences among evaluators regarding the numbers of lungs that were transplantable, all the evaluators at all time points during the EVLP run found one or more lungs to be transplantable from the gNO and P groups. This is an intriguing finding that probably reflects some degree of conservativeness in the transplant community regarding organ selection practices. Even the strictest evaluator in this study found that 3 of 16 lungs from either group were transplantable at some point after EVLP (18.75%). If this is extrapolated broadly, it would lead to a substantial increase in the number of available lung donors each year, albeit at an equally substantial increase in cost.
Limitations
The study is strengthened by its rigorous protocol, randomized cohorts, and blinded participants. The primary limitation was the small sample size. It is important to note that this was a proof-of-concept study and was not powered for determination of statistical significance between groups. Given that carefully selected donor lungs were rejected for transplantation and for clinical EVLP, acquiring larger sample sizes may be a challenge faced by similar future studies. The difficulty in acquiring a sample size powered to show significant differences between lungs highlights the importance of finding consistent trends in the data. Another challenge is the lack of a clear tool to assess lung quality on EVLP and the inherently subjective nature of lung evaluation. Moreover, outcome improvements in patients who receive transplants with lungs previously treated with NO via EVLP, and the clinical relevance of improvements in aggregate scores, lung weight, and so on, remain to be seen and should be evaluated in future studies. Although additional costs are incurred with inclusion of NO to EVLP, these may potentially be offset by an increased proportion of transplantable lungs.
Despite the limitations, the data suggest that the overall health of the lungs treated with NO showed improvement compared with those that received perfusate alone, as seen in the oxygenation and lung weights. This is not surprising, given that endogenous production of NO is decreased during the lung transplant process and that exogenous delivery of NO is known to have vasodilatory, anti-inflammatory, and anti-apoptotic effects in the lung transplant setting [4, 21,22,23,24,25,26]; it was also shown to improve oxygenation and reduce pulmonary artery pressure in patients with impaired oxygenation [32,33,34]. Especially given that NO is a readily available agent, our observations warrant further investigation to determine whether administration of NO would have a clinically meaningful effect following transplantation.
Conclusions
The results and the data trends observed in this pilot study suggest that the addition of gNO to the perfusate during EVLP may potentially improve the health of donor lungs compared to perfusate alone, as demonstrated by an aggregate score of lung physiology, whereas administration of iNO via the ventilator did not provide improvement in the aggregate score. However, both gNO and iNO appeared to have some beneficial effect on several endpoints. Overall, these findings suggest a possible role for the inclusion of gNO during EVLP with the aim of increasing the number of suitable donor lungs for transplantation and that a larger appropriately powered study is warranted to confirm these results and to determine significant differences between treatment groups.
References
Heron M. Deaths: leading causes for 2017. Natl Vital Stat Rep. 2019;68(6):1–77.
Valapour M, Lehr CJ, Skeans MA, Smith JM, Uccellini K, Goff R, et al. OPTN/SRTR 2018 annual data report: lung. Am J Transpl. 2020;20(Suppl s1):427–508.
Divithotawela C, Cypel M, Martinu T, Singer LG, Binnie M, Chow CW, et al. Long-term outcomes of lung transplant with ex vivo lung perfusion. JAMA Surg. 2019;154(12):1143–50.
George TJ, Arnaoutakis GJ, Beaty CA, Jandu SK, Santhanam L, Berkowitz DE, et al. A physiologic and biochemical profile of clinically rejected lungs on a normothermic ex vivo lung perfusion platform. J Surg Res. 2013;183(1):75–83.
Andreasson AS, Dark JH, Fisher AJ. Ex vivo lung perfusion in clinical lung transplantation—state of the art. Eur J Cardiothorac Surg. 2014;46(5):779–88.
Verleden GM, Dupont L, Yserbyt J, Schaevers V, Van Raemdonck D, Neyrinck A, et al. Recipient selection process and listing for lung transplantation. J Thorac Dis. 2017;9(9):3372–84.
Popov AF, Sabashnikov A, Patil NP, Zeriouh M, Mohite PN, Zych B, et al. Ex vivo lung perfusion—state of the art in lung donor pool expansion. Med Sci Monit Basic Res. 2015;21:9–14.
Possoz J, Neyrinck A, Van Raemdonck D. Ex vivo lung perfusion prior to transplantation: an overview of current clinical practice worldwide. J Thorac Dis. 2019;11(4):1635–50.
van der Mark SC, Hoek RAS, Hellemons ME. Developments in lung transplantation over the past decade. Eur Respir Rev. 2020;29(157):190132–48.
Van Raemdonck D, Neyrinck A, Cypel M, Keshavjee S. Ex-vivo lung perfusion. Transpl Int. 2015;28(6):643–56.
Boffini M, Ricci D, Barbero C, Bonato R, Ribezzo M, Mancuso E, et al. Ex vivo lung perfusion increases the pool of lung grafts: analysis of its potential and real impact on a lung transplant program. Transpl Proc. 2013;45(7):2624–6.
Cypel M, Yeung JC, Liu M, Anraku M, Chen F, Karolak W, et al. Normothermic ex vivo lung perfusion in clinical lung transplantation. N Engl J Med. 2011;364(15):1431–40.
Zych B, Popov AF, Stavri G, Bashford A, Bahrami T, Amrani M, et al. Early outcomes of bilateral sequential single lung transplantation after ex-vivo lung evaluation and reconditioning. J Heart Lung Transpl. 2012;31(3):274–81.
Cypel M, Liu M, Rubacha M, Yeung JC, Hirayama S, Anraku M, et al. Functional repair of human donor lungs by IL-10 gene therapy. Sci Transl Med. 2009;1(4):4ra9.
Yeung JC, Wagnetz D, Cypel M, Rubacha M, Koike T, Chun YM, et al. Ex vivo adenoviral vector gene delivery results in decreased vector-associated inflammation pre- and post-lung transplantation in the pig. Mol Ther. 2012;20(6):1204–11.
Andreasson A, Karamanou DM, Perry JD, Perry A, Özalp F, Butt T, et al. The effect of ex vivo lung perfusion on microbial load in human donor lungs. J Heart Lung Transpl. 2014;33(9):910–6.
Inci I, Ampollini L, Arni S, Jungraithmayr W, Inci D, Hillinger S, et al. Ex vivo reconditioning of marginal donor lungs injured by acid aspiration. J Heart Lung Transpl. 2008;27(11):1229–36.
Nakajima D, Liu M, Ohsumi A, Kalaf R, Iskender I, Hsin M, et al. Lung lavage and surfactant replacement during ex vivo lung perfusion for treatment of gastric acid aspiration-induced donor lung injury. J Heart Lung Transpl. 2017;36(5):577–85.
Cypel M, Yeung JC, Machuca T, Chen M, Singer LG, Yasufuku K, et al. Experience with the first 50 ex vivo lung perfusions in clinical transplantation. J Thorac Cardiovasc Surg. 2012;144(5):1200–6.
Pan X, Yang J, Fu S, Zhao H. Application of ex vivo lung perfusion (EVLP) in lung transplantation. J Thorac Dis. 2018;10(7):4637–42.
Meyer KC, Love RB, Zimmerman JJ. The therapeutic potential of nitric oxide in lung transplantation. Chest. 1998;113(5):1360–71.
Moreno I, Vicente R, Mir A, León I, Ramos F, Vicente JL, et al. Effects of inhaled nitric oxide on primary graft dysfunction in lung transplantation. Transpl Proc. 2009;41(6):2210–2.
Pasero D, Martin EL, Davi A, Mascia L, Rinaldi M, Ranieri VM. The effects of inhaled nitric oxide after lung transplantation. Minerva Anestesiol. 2010;76(5):353–61.
Pinsky DJ, Naka Y, Chowdhury NC, Liao H, Oz MC, Michler RE, et al. The nitric oxide/cyclic GMP pathway in organ transplantation: critical role in successful lung preservation. Proc Natl Acad Sci USA. 1994;91(25):12086–90.
Warnecke G, Strüber M, Fraud S, Hohlfeld JM, Haverich A. Combined exogenous surfactant and inhaled nitric oxide therapy for lung ischemia-reperfusion injury in minipigs. Transplantation. 2001;71(9):1238–44.
Yerebakan C, Ugurlucan M, Bayraktar S, Bethea BT, Conte JV. Effects of inhaled nitric oxide following lung transplantation. J Card Surg. 2009;24(3):269–74.
Dong BM, Abano JB, Egan TM. Nitric oxide ventilation of rat lungs from non-heart-beating donors improves posttransplant function. Am J Transpl. 2009;9(12):2707–15.
Potter CF, Dreshaj IA, Haxhiu MA, Stork EK, Chatburn RL, Martin RJ. Effect of exogenous and endogenous nitric oxide on the airway and tissue components of lung resistance in the newborn piglet. Pediatr Res. 1997;41(6):886–91.
Medeiros IL, Pêgo-Fernandes PM, Mariani AW, Fernandes FG, do Vale Unterpertinger F, Canzian M, et al. Histologic and functional evaluation of lungs reconditioned by ex vivo lung perfusion. J Heart Lung Transpl. 2012;31(3):305–9.
Sage AT, Richard-Greenblatt M, Zhong K, Bai XH, Snow MB, Babits M, et al. Prediction of donor related lung injury in clinical lung transplantation using a validated ex vivo lung perfusion inflammation score. J Heart Lung Transpl. 2021;40(7):687–95.
Cypel M, Keshavjee S. Extracorporeal lung perfusion (ex-vivo lung perfusion). Curr Opin Organ Transpl. 2016;21(3):329–35.
Blanco I, Ribas J, Xaubet A, Gómez FP, Roca J, Rodriguez-Roisin R, et al. Effects of inhaled nitric oxide at rest and during exercise in idiopathic pulmonary fibrosis. J Appl Physiol (1985). 2011;110(3):638–45.
Bronicki RA, Fortenberry J, Schreiber M, Checchia PA, Anas NG. Multicenter randomized controlled trial of inhaled nitric oxide for pediatric acute respiratory distress syndrome. J Pediatr. 2015;166(2):365-9.e1.
Öztürk E, Haydin S, Tanıdır İC, Özyılmaz İ, Ergül Y, Erek E, et al. Use of inhaled nitric oxide in pediatric cardiac intensive care unit. Turk Kardiyol Dern Ars. 2016;44(3):196–202.
Acknowledgements
Funding
This study and the journal’s Rapid Service Fee were funded by Mallinckrodt Pharmaceuticals.
Medical Writing and/or Editorial Assistance
Professional writing and editorial support were provided by MedLogix Communications, LLC, Itasca, Illinois, under the direction of the authors and was funded by Mallinckrodt Pharmaceuticals.
Authorship
All authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors were involved in the conception and design of the study, data collection and analysis, writing of the manuscript, and approval of the final version for submission.
Disclosures
Matthew Hartwig is a consultant for BioMed Innovations and Paragonix; has received grant/research support from Mallinckrodt Pharmaceuticals, Transmedics, and BioMed Innovations; and has other/educational relationships with Intuitive. Jacob Klapper has no financial relationships with commercial interests to disclose. Nagaraju Poola is a former employee of Mallinckrodt Pharmaceuticals. Amit Banga has no financial relationships with commercial interests to disclose. Pablo G. Sanchez has no financial relationships with commercial interests to disclose. John S. Murala has no financial relationships with commercial interests to disclose. Jim L. Potenziano is a former employee of Mallinckrodt Pharmaceuticals.
Compliance with Ethics Guidelines
The study was conducted in compliance with the principles of the Declaration of Helsinki of 1964 and its later amendments and the Declaration of Istanbul, and was in strict compliance with the ISHLT guidelines for transplant ethics. The lungs procured for this study did not meet the requirement for human subjects and were exempt from Institutional Review Board (IRB) review. Each investigator obtained an IRB exemption from their institution before initiating the study, including the Duke University Health System IRB, the University of Pittsburgh IRB, and the University of Texas Southwestern Medical Center IRB.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hartwig, M.G., Klapper, J.A., Poola, N. et al. A Randomized, Multicenter, Blinded Pilot Study Assessing the Effects of Gaseous Nitric Oxide in an Ex Vivo System of Human Lungs. Pulm Ther 9, 151–163 (2023). https://doi.org/10.1007/s41030-022-00209-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-022-00209-5