Abstract
Introduction
The aim of our observational study was to understand how patients with uncontrolled severe asthma perceive asthma control, and to assess their views on the role of healthcare professionals (HCPs) and other stakeholders in asthma management.
Methods
In total, 200 patients with uncontrolled, severe asthma living in Canada, France, Germany, Italy, Spain, the UK, or the USA registered on the Carenity asthma community responded to a patient survey.
Results
While 62% of respondents indicated they knew a lot about asthma, they were not entirely satisfied with its control. The two most helpful tools considered important in long-term asthma control were centered on learning, with tips on asthma control (76%), as well as information on asthma and its causes (67%). Although asthma education programs were accessible to less than half (44%) of the respondents, 72% said they would find them useful. In the previous year, most patients (78%) consulted a specialist; however, while 54% of respondents participated in shared decision-making (SDM) concerning their treatment, less than one-third (29%) felt their opinion had been considered, and only 27% said it helped their HCPs to develop an informed action plan. However, 48% believed that SDM would help them feel more confident in achieving long-term control. Most respondents consulted emergency room doctors or nurse practitioners because of their uncontrolled severe asthma, finding them persuasive sources of information. Additionally, patient advocacy organizations (PAGs) were considered as a preferred (12%) or persuasive (6%) source by only a few patients.
Conclusion
Most people with uncontrolled severe asthma were well informed about their disease. However, better information on asthma management would be useful for patients, with HCPs involved in this process. SDM was welcomed by respondents, but, to be successful, the patients’ opinions should be taken into consideration when forming an asthma management action plan.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Asthma is a chronic respiratory disease that represents a significant burden for patients, and is estimated to affect 358 million people worldwide |
The study was conducted to understand the level of disease control and management, to discover new perspectives on severe asthma control experiences (or the lack of control), to understand the motivations for better disease control among people with uncontrolled severe asthma, and to gain insights into the behavioral changes that patients undergo when taking steps towards better asthma control |
People with uncontrolled severe asthma describe themselves as very knowledgeable, but wish for practical tips on how to control asthma |
Patients want to participate in shared decision-making with healthcare professionals when managing their asthma, but find that their opinions are not always considered |
Patients think smartphone apps, websites or asthma education programs are useful, but many do not have access to them |
Introduction
Asthma is a chronic respiratory disease that represents a significant burden for patients, and is estimated to affect 358 million people worldwide [1, 2]. It is characterized by the presence of bronchial obstruction that can cause bronchial muscle contraction, inflammation of the bronchial wall, or hypersecretion of mucus [3]. Asthma is a multifactorial disease resulting from a combination of genetic predisposition and environmental risk factors (allergens, tobacco, pollution, etc.) [4, 5]. The underlying intensity of asthma is determined by the types (and doses) of treatments needed to achieve and sustain disease control. To that end, the Global Initiative for Asthma (GINA) has defined severe asthma as asthma that requires step 4 or 5 treatment, e.g., high-dose inhaled corticosteroids/long-acting beta agonists (ICS-LABA), to prevent it from becoming uncontrolled, or asthma that remains “uncontrolled” despite this treatment [2]. Severe asthma is differentiated from uncontrolled asthma, which is defined as asthma with poor symptom control (frequent symptoms or reliever use, activity limited by asthma, night waking due to asthma), or frequent exacerbations (≥ 2/year) requiring oral corticosteroids (OCS) or serious exacerbations (≥ 1/year) requiring hospitalization. Severe uncontrolled asthma is thought to affect 5–10% of the total asthma population [6]. In adults, uncontrolled asthma can affect their daily quality of life by impacting breathing, sleeping, cognition, vitality, and sexual activity [7]. In children, asthma-related absenteeism from school is associated with poorly controlled asthma [8]. Despite the potentially serious consequences of severe asthma, the under recognition of asthma severity by patients and clinicians alike has been identified as a factor in patient mortality, mostly because of underreporting of symptoms by patients to physicians [9, 10]. In an online European survey (Recognise Asthma and Link to Symptoms and Experience), 8,000 adults with asthma responded to an online questionnaire; the majority believed that their asthma was under control, although only 20% of respondents had controlled asthma as defined by GINA according to parameters [11]. It is therefore important to further increase awareness on the symptoms of severe asthma to get it under control. Severe asthma may also be impacted by comorbidities, and psychological and behavioral factors. Educating patients and healthcare professionals (HCPs) on identifying and managing these traits—such as sleep apnea, chronic rhinosinusitis, and obesity—may help improve asthma management [12].
In this context, we conducted a study to understand the level of disease control and management, to discover new perspectives on severe asthma control experiences (or the lack of control), to understand the motivations for better disease control among people with uncontrolled severe asthma, and to gain insights into the behavioral changes that patients undergo when taking steps towards better asthma control.
Methods
Study Design
An observational study was conducted via the Carenity (a global online patient community) international online platform. Adult patients self-reporting as living with uncontrolled severe asthma received an online survey consisting of two sections: a screener questionnaire to select for people with uncontrolled severe asthma, followed by questions on asthma control and severity.
Study Population and Treatment
Carenity is a leading online digital patient platform with 500,000 patients and caregivers registered worldwide. It aims to facilitate the sharing of patient experiences, helping them find health-related information on their medical condition, and subsequently contributing to medical research through patient participation in online studies to highlight their experiences. The study population consisted of registered Carenity members from the asthma community. Eligible patients were defined as adult patients (18 years or older) living in Canada, France, Germany, Italy, Spain, the UK, or the USA, having self-reported uncontrolled severe asthma, and being members of the Carenity community. A screener was used in the first part of the survey to select for patients with uncontrolled severe asthma only; therefore, patients affected by chronic bronchitis or chronic obstructive pulmonary disease, as well as patients with controlled asthma, were excluded from the study population and did not go on to complete the second part of the survey. People with uncontrolled severe asthma were identified through the following inclusion criteria: use of rescue inhaler more than two to three times a week; being heavily impacted by symptoms, disturbed sleep, limitation of activities (including school or work) on daily life; visiting an emergency room or urgent care; and use of OCS. For severe asthma, the criteria were: being under current treatment with either biologics or (OCS + either ICS or ICS/LABA) or [OCS + LABA + either long-acting muscarinic antagonists (LAMA) or leukotriene receptor antagonists], or ICS + LABA (each individually) + either LTRA or LAMA, or OCS + LABA (combination) + either LTRA or LAMA.
Data Collection
Patients registered in the asthma community on the Carenity platform and living in Canada, France, Germany, Italy, Spain, the UK, or the USA were invited by email to participate in an online patient survey. The questionnaire was conducted online between from February 1, 2021 to April 5, 2021. Patients were included in the study if they completed all elements of the baseline questionnaire. The collected data included self-reported sociodemographic and medical profiles, as well as information about the patients’ perception of severe asthma, its control, and its management. The ad hoc questionnaire comprised single-choice, multiple-choice, sliding-scale, or free-text answers. The questionnaire was designed by Carenity, and subsequently reviewed by one expert in severe asthma. Additionally, as the questionnaire was programmed in local languages for the different Carenity worldwide platforms, it was also validated by native speakers to ensure compliance for each country involved. Data collected on the Carenity platform are hosted in France on a secured computer server in accordance with the requirements of the “Commission Nationale de l’Informatique et des Libertés” (CNIL), declaration number no. 1484083, dated March 29, 2011.
Ethical Considerations
As the aim of the study was to determine patient perception of their asthma control and how to gain better asthma control, the survey was considered as a Market Research or “patient satisfaction survey”. The study was conducted online and no healthcare practitioners were involved in the patients’ recruitment. The survey falls under the scope of market research and does not fall under the scope of regulations regarding observational studies nor research implying human beings. For this reason, submission to an ethical committee was neither required nor sought. Study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments. Informed consent regarding participation and publication of outcomes were obtained from all individual participants included in the study. The participants’ privacy and confidentiality were guaranteed following health care personal data protection laws and regulations (GDPR, General Data Protection Regulation).
Statistical Analysis
Statistical analyses were performed using the statistical software R Studio (v.3.5.0, The R Foundation, Vienna, Austria). Demographics and clinical characteristics were summarized using descriptive statistics. Summary statistics for continuous variables include number, mean, and standard deviation (SD). For categorical variables, numbers and percentages of patients are reported. Estimates are presented with 95% confidence intervals. The p values were calculated using ANOVA, chi-squared, or Wilcoxon methods, with a confidence interval of 95%; a p value < 0.05 was considered statistically significant.
Results
Respondents’ Profile
Selected Study Population
Among the 9352 asthma patients invited to participate in the survey, 575 people with uncontrolled severe asthma started to answer the online questionnaire (Fig. 1). Overall, 329 patients were excluded as they did not fulfill the inclusion criteria; 46 additional patients who did not answer all the questions were also ineligible. In total, the valid study population consisted of eligible 200 patients who fully completed the survey.
Sociodemographic Profile
Table 1 presents the sociodemographic profile of the respondents. The country of residence of most patients were the USA (42%, n = 85/200), followed by France (11%, n = 22/200), the UK (11%, n = 22/200), Italy (10%, n = 19/200), Spain (10%, n = 19/200), Germany (9%, n = 18/200), and Canada (8%, n = 15/200). An equal distribution was observed between patients located in Europe (50%) and North America (50%). Just over half of the patients were men (53%, n = 106/200), and 79% (n = 158/200) of the study population was 50 years old or younger. The European patients tended to be older than the North American ones. Indeed, 34% (n = 34/100) of European patients were younger than 30 years old, 42% (n = 42/100) were aged between 31 and 50 years old, and 24% (n = 24/100) were older than 50 years old, compared to, respectively, 17% (n = 17/100), 65% (n = 65/100), and 18% (n = 18/100) of North American patients. However, Italian participants were on average much older, whereas the proportion of older German patients was quite low [respectively, 57% (n = 11/19) vs. 6% (n = 1/18) of patients were older than 51 years old]. Similarly, gender differences were observed across participating countries: on average, and compared to the mean rate (47%, n = 94/200), the female rate was higher in Germany (72%, n = 13/18) and Italy (63%, n = 12/19), and lower in Spain (37%, n = 7/19). Note that female patients were more frequent among the European participants than among those living in North America [52%, (n = 52/100) vs. 43%, (n = 43/100)].
Disease Characteristics
The clinical characteristics are presented in Table 2. On average, patients were initially diagnosed with asthma 15 years ago (SD, 13.2), with 15% (n = 30/200) of them diagnosed less than 5 years ago and 13% (n = 26/200) for more than 30 years. While no relevant difference was observed in the time elapsed since diagnosis between asthma patients in Europe or North America, on the country level, disparities were noticeable; with a mean duration since diagnosis of only 8 years (SD, 5.4) in Germany, but 20 years in the UK (SD, 11.7) or France (SD, 16.4).
In total, 55% (n = 111/200) of patients mentioned having another medical condition in addition to their uncontrolled severe asthma, mainly allergies (38%, n = 75/200), anxiety (24%, n = 48/200), and eczema (14%, n = 27/200). On average, patients indicated one comorbidity in addition to their uncontrolled severe asthma.
Concerning the management of their uncontrolled severe asthma over the past year, respondents have, on average, required eight courses of oral corticosteroids, visited emergency rooms or urgent care, and were hospitalized two to three times a year, and visited emergency rooms or urgent care, and were released three to four times a year because of their uncontrolled severe asthma.
Among different treatments currently available to treat uncontrolled severe asthma, OCS were the main treatments taken at least once by patients (72%, n = 143/200), followed by biologics (68%, n = 135/200), and ICS/LABA (64%, n = 128/200). On average, patients took four (SD, 1.6) different types of treatments to deal with their uncontrolled severe asthma.
Level and Perception of Asthma Control
Figure 2 summarizes the manifestation of asthma during the past 3 months. Overall, 46% (n = 92/200) of patients used a rescue inhaler at least once a day, 39% (n = 78/200) experienced daily asthma symptoms, 38% (n = 76/200) reported that their asthma daily limited their activities, and 34% (n = 68/200) mentioned having daily disturbed sleep. Although less common, 21% (n = 42/200) declared having also missed school or work on at least 1 day because of their asthma.
Asthma control seems to be a critical challenge for patients living with uncontrolled severe asthma: with 66% (n = 133/200) of respondents declaring that they think about controlling their asthma whether they were experiencing symptoms or not, 22% (n = 44/200) reported thinking about it only when having symptoms, and 12% (n = 23/200) without having symptoms. The proportion of patients who thought about controlling their asthma, both when they had symptoms and when they did not, increased with age, with 53% (n = 27/51) of patients aged 18–30 years thinking about symptoms compared with 66% (n = 71/107) of patients aged 31–50 years old, and 83% (n = 35/42) of respondents who were 51 years old or older.
Most respondents thought that the control of their asthma symptoms was completely dependent on the actions they took (mean: 4.7 out of 6, with 6 being “Strongly agree with the statement “).
Regarding patients being confident in their ability to achieve long-term control of their asthma, the mean confidence level among all participants was 7.3 (with 10 being “very confident”), and 38% (n = 75/200) of them reaching a confidence level rated higher than 8.0 out of 10.0. Therefore, we can conclude that patients tended to be confident in their ability to achieve long-term control of their asthma (p < 0.001 for mean scores of 7.0–10.0 compared to categories 0–6.0) (Fig. 3). Additionally, the more people with uncontrolled severe asthma perceived they were knowledgeable about their disease, the more confident they were about achieving long-term control, with respondents who claimed to know a lot about their medical condition reaching a mean confidence level of 7.7 out of 10.0, whereas participants knowing only a little scored at 6.1 out of 10.0 (p < 0.001).
All patients indicated that knowing and understanding the underlying causes of asthma was important when managing it, with 81% (n = 162/200) of patients describing it as “very important”, 18% (n = 36/200) as “important”, and 1%, (n = 2/200) as “somewhat important”. Patients spontaneously mentioned the presence of fewer symptoms (58%, n = 116/200) and less disruption of daily life (55% n = 109/200) as the two main components associated with good asthma control. Moreover, patients qualitatively described a life without asthma as “less constraining”, “better”, and “more active”.
On the other hand, patients did not seem to be entirely satisfied with their current level of asthma control and asthma management, with a mean score of 6.8 for “asthma control”, 7.1 for “medicines used to manage asthma” and 6.6 for “lifestyle practices used to manage asthma” on a 10-point scale, with 10 indicating “very satisfied”. Interestingly, patients older than 50 years expressed less satisfaction compared to younger ones (18–30 years old) in terms of asthma control (mean, 6.0 vs. 7.3; p = 0.023) and lifestyle practices (mean, 5.7 vs. 7.2; p = 0.011) (Fig. 4a). Similarly, European respondents appeared to be statistically significantly less satisfied than North American ones, especially concerning lifestyle practices (mean, 6.3 vs. 6.9; p = 0.038), medicines used to manage asthma (mean, 6.8 vs. 7.4; p = 0.019), or asthma control (mean, 6.5 vs. 7.2; p = 0.012) (Fig. 4b). Additionally, male patients were significantly more satisfied than female participants with their asthma control (mean, 7.6 vs. 6.1; p < 0.001) and asthma management [mean, 7.6 vs. 6.6 (p < 0.001) for medicines used; 7.3 vs. 5.9 (p = 0.004) for lifestyle practices used] (Fig. 4c).
Satisfaction level with asthma management and control. a per gender, with p value comparing male versus female; b per geographic area of residence, with p value assessing Europe versus North America; c per age, with p value evaluating older patients (> 50 years old) to younger ones (18–30 years old). A score of 0 indicates “not satisfied at all”, while a score of 10 indicates “very satisfied”
Overall, 87% (n = 175/200) of responders mentioned having at least one concern about maintaining long-term asthma control, while 39% (n = 77/200) reported their asthma treatment may stop working, 34% (n = 68/200) struggled to understand when their asthma was under control, 34% (n = 68/200) were afraid they could not avoid asthma triggers, and 28% (n = 56/200) felt that asthma control was not something they could achieve.
Involvement of the Healthcare Professionals in Asthma Management
In the past 12 months, 78% (n = 155/200) of patients hadconsulted a specialist (pulmonologist, allergist, or ear, nose, and throat specialists (ENT)]. A pulmonologist (48%, n = 95/200) or a general practitioner (GP) (47%, n = 93/200) were considered as the primary manager for asthma (Fig. 5), with a mean of 2.5 HCPs mentioned. Primary healthcare manager for asthma seemed however to be country-dependent, with GPs being the most mentioned manager in the UK (64%, n = 14/22) versus pulmonologist in France (68%, n = 15/22) and asthma nurses in Germany (50%, n = 9/18).
Patients felt comfortable asking questions and being honest and transparent with the physician who treated their asthma (mean, 5.4 out of 6.0, with 6 being “strongly agree with the statement”; less than 25% of responders scored 5.0 or less).
Outcomes were improved and satisfaction higher when HCPs and patients work together to decide upon the best care for each patient; this shared decision-making (SDM) is designed to benefit both HCPs and patients. Among the 54% (n = 108/200) of respondents who were involved in SDM, 29% (n = 31/108) indicated that their opinion had been considered, 27% (n = 29/108) indicated that it had helped their HCPs to develop an informed action plan, and 21% (n = 23/108) to better support them in their asthma management. Among the 21% (n = 41/200) of respondents who were not involved in SDM, 15 patients thought it would help them to discuss more detailed information with their HCP, while 7 patients did not know SDM existed, but would feel comfortable asking. Patients from North America tended to be more involved in SDM compared to patients living in Europe [67% (n = 67/100) vs. 41% (n = 41/100), respectively], as well as men compared to women [64% (n = 67/105) vs. 43% (n = 41/95), respectively]. Moreover, the younger the patients were, the more often they were involved in SDM [61% (n = 31/51) for 18–30 years old vs. 31% (n = 13/42) for ≥ 51 years old]. Also, 48% (n = 10/21) of patients who were not confident to control their asthma over the long-term mentioned that engaging in SDM would help them feel more confident that they could achieve long-term control of their asthma.
Respondents reported that they had a good knowledge of their medical condition: 62% (n = 124/200) knew “a lot” about severe asthma, while only 6% (n = 12/200) knew “only a little”. Nevertheless, patients living in North America tended to know more about severe asthma than European patients [71% (n = 71/100) vs. 53% (n = 53/100), respectively].
The two most helpful tools mentioned by patients to support them feeling more confident in achieving long-term control of their asthma were focused on learning: either practical tips on how to control asthma (76%, n = 16/21), or more generally information on asthma and its causes (67%, n = 14/21) (Fig. 6). Additionally, 62% (n = 13/21) reported that accessing ongoing support services might also be helpful.
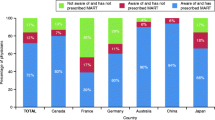
The preferred and most persuasive sources of information to change asthma management are detailed in Supplementary Fig. 1.
Regardless of the services offered to manage asthma, available resources were considered useful by more than 65% (n = 130/200) of patients, and were accessible to at least 44% (n = 88/200) of them (Fig. 7). Most available services offered to manage asthma were only accessible by 64% (n = 128/200) of patients. Technologies to better manage asthma—like smartphone apps or dedicated websites—were the main services that patients felt should be developed, as they were found useful by almost 80% of patients, but accessible to less than half of patients. An asthma action plan was the main service offered to patients (64%, n = 128/200), followed by patient education on asthma (62%, n = 124/200), and lifestyle and diet programs specific to asthma (60%, n = 120/200). An asthma education program was still not as accessible as it should be; indeed, it was offered to 44% (n = 88/200) of respondents, while 74% (n = 148/200) would have found it useful.
Services offered to manage asthma; n = 200 patients for all items. a Participation in an asthma education program; b technologies to better manage my asthma; c support from other people who live with asthma; d wellness programs; e lifestyle and diet programs specific to asthma; f patient education on the disease; g asthma action plan. Utility indicates how useful this
Discussion
Several key observations can be drawn from this online survey of 200 patients living with uncontrolled severe asthma in Europe and North America.
If affected patients reported good knowledge of their medical condition—especially North American respondents—and are in general confident in their ability to achieve long-term asthma control, they seem to need a better understanding of the practical side of the disease, e.g., advice on how to better manage and control their disease and its treatments.
For patients with severe or difficult-to-control-asthma, specialist referral is indicated [13]. Nevertheless, to support patients, HCPs and others should be engaged, such as policymakers or patient advocacy organizations (PAGs), with the aims of promoting patient-centric care, as well as identifying and remediating gaps in care [14]. Moreover, to improve patient care, PAGs are crucial in raising awareness and understanding for patients, caregivers, HCPs, and the public about the impact of uncontrolled severe asthma [15]. However, our analysis showed that PAGs were neither a preferred source of information on asthma management, nor a persuasive one among respondents with uncontrolled severe asthma. Several initiatives are dedicated to increase patients’ awareness of their medical condition and to encourage them to develop partnerships with their HCPs, as for instance the multidisciplinary working group named “Patient Understanding Leading to Assessment for a Severe Asthma Referral” (PULSAR) [16]. Better education regarding patients’ needs and conditions is essential for all caregivers and other stakeholders involved, especially in terms of improving patients’ education on asthma management; indeed, only 62% of people with uncontrolled severe asthma reported having been offered asthma education in our study. In this instance, building a more consistent, reliable documentation for patients and associated stakeholders might help. Telemedicine and e-health technologies might also be helpful as well enhancing in patients’ empowerment in the management of their condition, although disparities in access may be further exacerbated by these initiatives [12].
SDM encourages patients and families to take a more central and active role in their care by working with their HCP to participate in the choices regarding their treatments and medication options. SDM is evidence-based and balances risks and results with patient’s preferences and values. An important point that arose through our observational study is the lack of involvement of patients in the SDM process, as only 54% of them reported taking part in this practice, and only 29% of them indicated that their opinion had been considered. Our data show that most patients who were not involved in the therapeutic decision would like to discuss it in future with their HCP. This should be made as the default approach and be as inclusive as possible for caregivers when it is relevant. As an example, several publications describe the benefit in terms of meaningful outcomes of engaging patients with asthma, as well as advocacy group stakeholders, in the research team when planning for a case study in that field [17, 18].
Despite a large range of available therapeutic options, people with uncontrolled severe asthma still encounter unmet needs in the management of their disease; indeed, most of those patients have poorly or not well-controlled asthma, and strategies are needed to overcome this issue [12]. Of note, encouraging patients to achieve better asthma control may be of interest; indeed, respondents primarily mentioned that learning tips on how to manage asthma might help them feel more confident in reaching a better control of their severe condition, to learn more about their asthma and its causes, or to access ongoing support services.
This study, which is based on an online survey accessible to the Carenity asthma community only, presents several limitations inherent in its observational design: (1) overrepresentation of patients caring about their health status, while underrepresentation on Carenity communities of patients without online access (selection bias due to recruitment source); (2) high-technology and literacy bias, (3) self-reported perceptions of their asthma knowledge, control, and management; and (4) recall bias related to disease characteristics asked at the beginning of the survey (time elapsed since diagnosis, treatments received). In this study, we cannot estimate the extent of respondents’ participation in SDM with healthcare professionals; indeed, some participants mentioned this as still not having been taken into consideration, although they mentioned having been involved in SDM. However, the desirability bias was limited due to the direct answering of the questionnaire by the patients in the absence of their clinicians. Additionally, our findings should be considered cautiously, as the members of such patient community might not be poorly controlled, highly symptomatic, and heavily treated patients. The study population was selected from patients registered on the asthma Carenity platform in Europe and the USA; despite a homogeneous population of patients recruited, no generalizations of the study can be assumed. Finally, lack of control groups (for instance, non-severe patients) added to the study, selection of a small part of the asthma population (people with severe and uncontrolled asthma), and lack of clinical examination prior to inclusion are limitations of the study.
Conclusions
Most people with uncontrolled severe asthma believe they are well informed about their disease and have it under control. The urgent need concerns mostly education means to improve their knowledge about asthma management; all stakeholders should be implicated in this process. Involving the patients in the treatment decision—shared decision-making—should be implemented by all healthcare professionals concerned. In all, this aims to increase the patients’ self-confidence in achieving better asthma control and management, which may translate into improvements in the objective control of their disease.
References
Stridsman C, Axelsson M, Warm K, Backman H. Uncontrolled asthma occurs in all GINA treatment steps and is associated with worse physical health—a report from the OLIN adult asthma cohort. J Asthma. 2021;58(5):586–95.
Global initative for asthma: global strategy for asthma management and prevention. 2020. https://ginasthma.org/. Accessed 27 Feb 2020.
Padem N, Saltoun C. Classification of asthma. Allergy Asthma Proc. 2019;40(6):385–8.
Schoettler N, Strek ME. Recent advances in severe asthma: from phenotypes to personalized medicine. Chest. 2020;157(3):516–28.
Subbarao P, Mandhane PJ, Sears MR. Asthma: epidemiology, etiology and risk factors. CMAJ. 2009;181(9):E181-190.
Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343–73.
Ilmarinen P, Juboori H, Tuomisto LE, Niemelä O, Sintonen H, Kankaanranta H. Effect of asthma control on general health-related quality of life in patients diagnosed with adult-onset asthma. Sci Rep. 2019;9(1):16107.
Hsu J, Qin X, Beavers SF, Mirabelli MC. Asthma-related school absenteeism, morbidity, and modifiable factors. Am J Prev Med. 2016;51(1):23–32.
Aaron SD, Boulet LP, Reddel HK, Gershon AS. Underdiagnosis and overdiagnosis of asthma. Am J Respir Crit Care Med. 2018;198(8):1012–20.
Jones TL, Neville DM, Chauhan AJ. Diagnosis and treatment of severe asthma: a phenotype-based approach. Clin Med (Lond). 2018;18(Suppl 2):s36–40.
Price D, Fletcher M, van der Molen T. Asthma control and management in 8,000 European patients: the REcognise Asthma and LInk to Symptoms and Experience (REALISE) survey. NPJ Prim Care Respir Med. 2014;24:14009.
Caminati M, Vaia R, Furci F, Guarnieri G, Senna G. Uncontrolled Asthma: Unmet Needs in the Management of Patients. J Asthma Allergy. 2021;14:457–66.
Wu TD, Brigham EP, McCormack MC. Asthma in the primary care setting. Med Clin North Am. 2019;103(3):435–52.
Haughney J, Winders TA, Holmes S, et al. Global quality standard for identification and management of severe asthma. Adv Ther. 2020;37(9):3645–59.
Menzies-Gow A, Canonica GW, Winders TA, Correia-de-Sousa J, Upham JW, Fink-Wagner AH. A charter to improve patient care in severe asthma. Adv Ther. 2018;35(10):1485–96.
Winders TA, Wilson AM, Fletcher MJ, McGuinness A, Price DB. A patient-centered description of severe asthma: patient understanding leading to assessment for a severe asthma referral (PULSAR). Patient. 2019;12(5):539–49.
George M, Bruzzese JM, Sommers MLS, et al. Group-randomized trial of tailored brief shared decision-making to improve asthma control in urban black adults. J Adv Nurs. 2021;77(3):1501–17.
Tapp H, Derkowski D, Calvert M, Welch M, Spencer S. Patient perspectives on engagement in shared decision-making for asthma care. Fam Pract. 2017;34(3):353–7.
Acknowledgements
Funding
Sponsorship for this study and Rapid Service Fee were funded by Sanofi and Regeneron.
Medical Writing and Editorial Assistance
Medical writing assistance was provided by Dr. Florence Boulmé on behalf of Carenity.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Emilie Pain, Alexis Bombezin—Domino and Camille Graff. The first draft of the manuscript was written by Florence Boulmé, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. Authors want to thank all the study participant(s) for their involvement in the study.
Disclosures
Emilie Pain, Alexis Bombezin--Domino and Camille Graff are employees of Carenity. Maureen George has been a consultant/speaker for AstraZeneca, Genentech, and Teva, and a consultant for Sanofi Genzyme and Regeneron.
Compliance with Ethics Guidelines
As the aim of the study was to determine patient perception of their asthma control and how to gain better asthma control, the survey was considered as a Market Research or “patient satisfaction survey”. The study was conducted online and no healthcare practitioners were involved in the patient’s recruitment. The survey falls under the scope of market research and does not fall under the scope of regulations regarding observational studies nor research implying human beings. For this reason, submission to an ethical committee was neither required nor sought. Study was performed in accordance with the Helsinki Declaration of 1964, and its later amendments. Informed consent regarding participation and publication of outcomes were obtained from all individual participants included in the study. The participants’ privacy and confidentiality were guaranteed following health care personal data protection laws and regulations (GDPR, General Data Protection Regulation).
Data Availability
The datasets generated during and/or analyzed during the current study (except personal data) are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
George, M., Graff, C., Bombezin–Domino, A. et al. Patients with Severe Uncontrolled Asthma: Perception of Asthma Control and its Management. Pulm Ther 8, 209–223 (2022). https://doi.org/10.1007/s41030-022-00190-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-022-00190-z