Abstract
Introduction
The PROOF registry is a prospective, observational study that aimed to monitor disease progression in a real-world cohort of patients with idiopathic pulmonary fibrosis (IPF). Here, longitudinal quality-of-life (QoL) outcomes, healthcare resource use (HCRU), and the association between QoL and mortality in patients enrolled in the PROOF registry are presented.
Methods
QoL outcomes (St. George’s Respiratory Questionnaire [SGRQ], EuroQoL-5 dimensions-5 levels Health Questionnaire [EQ-5D-5L], EuroQoL-5 dimensions Health Questionnaire [EQ-5D] visual analogue scale [VAS] and cough VAS) and HCRU were collected for all patients. Associations between baseline QoL and mortality were assessed using univariate and multivariate analyses. During multivariate analyses, individual QoL measures were adjusted for the following covariates: age, sex, percent predicted forced vital capacity, percent predicted diffusing capacity of the lungs for carbon monoxide, smoking status, and supplementary oxygen use at registry inclusion.
Results
In total, 277 patients were enrolled in the PROOF registry. During the follow-up period, worsening in cough VAS score, SGRQ symptom score, and SGRQ activity score was observed, while EQ-5D VAS, SGRQ total score, and SGRQ impact score remained stable. During univariate analyses, EQ-5D VAS and all SGRQ sub-scores and total score at baseline were associated with mortality; however, during multivariate analyses, only the SGRQ total score, SGRQ impact score, and SGRQ symptom score at baseline were associated with mortality. During the follow-up period, 261 (94.2%) patients required an outpatient consultation (IPF- or non-IPF-related) and there were 182 hospitalizations in total, most of which were respiratory related (66.5%).
Conclusions
The PROOF registry provided valuable, real-world data on the association between baseline QoL and mortality, and longitudinal HCRU and QoL outcomes in patients with IPF over 24 months and identified that SGRQ may be an independent prognostic factor in IPF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The symptoms of idiopathic pulmonary fibrosis (IPF), which is a rare, fatal, fibrosing lung disease, can be debilitating and greatly impact the quality of life (QoL) of patients as well as healthcare resource use (HCRU). |
Previous registry-based studies have examined the relationship between QoL and clinical outcomes, including mortality, in IPF; however, longitudinal HCRU and QoL data for patients with IPF enrolled in prospective, real-world registries are limited. |
The PROOF registry was a prospective, observational study initiated in October 2013, and the analyses presented in this manuscript aimed to provide important insights into QoL and the burden of disease in IPF, as well as the relationship between baseline QoL and mortality in patients with IPF enrolled in the PROOF registry. |
What was learned from this study? |
Data from the PROOF registry highlighted the high HCRU burden for patients with IPF and identified that the St. George’s Respiratory Questionnaire (SGRQ) may be an independent prognostic factor in IPF. |
The findings reported in this manuscript are generally in line with existing registry-based literature regarding the relationship between QoL and mortality; however, some conflicting results were reported in the PROOF registry versus other IPF registries such as differences in the association between SGRQ sub-scores and mortality, which may be due to factors such as study design. |
Introduction
Idiopathic pulmonary fibrosis (IPF) is a progressive, irreversible, fatal, fibrosing lung disease that is associated with survival rates lower than those reported for many cancers [1,2,3]. Patients with IPF experience debilitating symptoms, including cough and shortness of breath that lead to increasing limitations on daily activities, a deterioration in emotional well-being, and a growing dependence on family or caregivers [4,5,6,7]. Indeed, the psychosocial impact of IPF and related comorbidities is substantial, and greatly influences patients’ quality of life (QoL) [8,9,10].
While the current antifibrotic therapies approved for patients with IPF slow disease progression [11,12,13], the impact of IPF symptoms on patients’ QoL remains extensive [14]. Several patient-reported outcomes (PROs), including the St. George’s Respiratory Questionnaire (SGRQ), EuroQoL-5 dimensions-5 levels (EQ-5D-5L) Health Questionnaire, and EuroQoL-5 dimensions Health Questionnaire (EQ-5D) visual analogue scale (VAS), have been shown to be effective measures of health-related QoL in patients with IPF and interstitial lung disease (ILD) [15, 16]. Other PROs such as cough VAS have been used to measure health-related QoL in patients with IPF and ILD; however, this PRO has not yet been validated in this patient population [9, 17]. Moreover, the role of these PROs in predicting clinical outcomes, including mortality, has also been explored [9, 10, 18,19,20,21,22,23,24,25,26,27]. Previous reports have highlighted a weak association between QoL and forced vital capacity (FVC) and the 6-minute walk test [26, 27], whereas more recent studies have reported a close relationship between QoL, disease severity, and clinical outcomes, such as changes in pulmonary function in patients with IPF [10, 18,19,20, 24]. Furthermore, several studies have identified an association between QoL and mortality in IPF [10, 22, 23, 25], and in particular, it has been suggested that SGRQ may be an independent prognostic factor in patients with IPF [22, 23]. However, it is important to note that not all studies have uncovered an association between QoL and mortality in IPF. Indeed, the results of a retrospective study and data from the Australian IPF registry did not reveal a significant association between SGRQ scores and mortality based on multivariate analyses [9, 21].
While PROs are used to assess the impact on patients’ QoL, data collected on healthcare resource use (HCRU) are critical to understanding the burden of disease in patients with IPF. HCRU and costs for patients with interstitial lung disease, in particular IPF, have been retrospectively examined [28,29,30,31], and recently it has been reported that patients with IPF have increased HCRU, which may be a reflection of the higher rates of diagnostic procedures and healthcare visits compared to controls [29]. However, longitudinal HCRU and QoL data for patients with IPF enrolled in a prospective, real-world registry are limited.
The PROOF registry was a prospective, observational study set up in October 2013 that aimed to monitor disease progression in a real-world cohort of patients with IPF [32, 33]. The baseline characteristics and longitudinal clinical outcomes of patients enrolled in the PROOF registry have been reported previously [32, 33]. The analyses presented here aimed to add to the existing registry-based literature on the relationship between QoL and mortality in IPF by examining the association between baseline QoL and mortality in patients enrolled in the PROOF registry. Furthermore, these analyses also looked to provide important insights into QoL and the burden of disease in IPF by reporting longitudinal QoL and HCRU data from the PROOF registry from October 2013 to July 2017.
Methods
Registry Design
Patients were enrolled across seven centers in Belgium and one center in Luxembourg during the period of October 2013 to January 2016. Patients eligible for inclusion in the PROOF registry were over 18 years of age and had a definite or probable IPF diagnosis confirmed by a multidisciplinary team, according to the 2011 American Thoracic Society/European Respiratory Society guidelines [2]. As the registry was set up to collect data on standard of care, patients were excluded if they were enrolled in a clinical trial at the time of inclusion in the PROOF registry.
The PROOF registry was conducted in accordance with the International Council on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use, Guidelines for Good Clinical Practice, and local legal and regulatory requirements. Patients were required to provide informed consent prior to inclusion. PROOF is registered with the relevant authorities in Belgium and Luxembourg, and received ethics approval from Comité National d'Éthique et de Recherche (CNER) N201309/03-12 September 2013 and Comité National de Protection des Données (CNDP) for Luxembourg.
Analysis Population and Patient Demographics
The PROOF registry closed in July 2017 and therefore analyses were performed at this cut-off date. QoL outcomes, QoL associations with mortality, and HCRU were assessed in all patients with IPF included in the PROOF registry. Demographic data, including age, sex, race, smoking status, supplemental oxygen use, and previous treatment for IPF other than pirfenidone, were collected upon enrollment in the PROOF registry. The comorbidities and co-medication use at baseline are described in the PROOF baseline manuscript [27]. Pirfenidone treatment patterns and longitudinal changes in pulmonary function at 3, 6, 12, and 24 months post-registry inclusion (post-inclusion) have also been reported previously [28]. Data for patients treated with nintedanib were not assessed due to low patient numbers, as patient enrollment into the PROOF registry began prior to the introduction of nintedanib.
QoL Outcomes
For all patients enrolled in the PROOF registry, PROs were used to evaluate QoL at baseline and at regular intervals throughout the follow-up period. Cough VAS is a linear visual scale on which patients are asked to indicate the severity of their cough, with 0 mm representing ‘no cough’ and 100 mm representing ‘worst cough ever’ [34]. The SGRQ sub-scores measure QoL in patients with IPF across three domains: activity, symptoms, and impact. Both the SGRQ total score and sub-scores are weighted to give a total score from 0 to 100, with higher scores indicating greater impairment [35,36,37]. The EQ-5D-5L measures impairment across five dimensions related to health status: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression, where patients rate their impairment on a categorical scale (no problems, slight problems, moderate problems, severe problems, extreme problems) [38]. EQ-5D VAS allows patients to rate their overall health status on a linear visual scale, with 0 mm representing ‘worst health imaginable’ and 100 mm representing ‘best health imaginable’ [38]. In this study, cough VAS was assessed at baseline and at months 3, 6, 12, and 24 post-inclusion. The SGRQ total score and sub-scores, and EQ-5D-5L and EQ-5D VAS scores, were evaluated at baseline and at Months 12 and 24 post-inclusion. All QoL scores are presented as mean (standard deviation [SD]).
Baseline QoL Associations with Mortality in all Patients Enrolled in the PROOF Registry
Univariate associations between baseline covariates (age, sex, percent predicted FVC, percent predicted diffusing capacity of the lungs for carbon monoxide [DLco], smoking status, and supplementary oxygen use at registry inclusion) and mortality were assessed in patients enrolled in the PROOF registry. The association between baseline QoL outcomes in all patients and mortality was assessed using univariate Cox modeling. Baseline QoL outcomes in all patients were then adjusted for covariates and the association with mortality was assessed using adjusted Cox proportional hazards models. To account for missing data in univariate and multivariate analyses, multiple imputation was performed, and missing data were considered missing at random; however, to contextualize the impact of imputation, analyses without multiple imputations were also performed. In univariate and multivariate analyses, lung transplant was not treated as a mortality event and these patients were included in the analyses.
HCRU
During the follow-up period, the number of outpatient consultations, reason for consultation (IPF- or non-IPF-related), type of care provider and the site of care were recorded for all patients enrolled in the PROOF registry. The proportion of respiratory-related and non-respiratory-related hospitalizations, duration of hospital stay, reason for hospital stay and type of care provider required during all hospitalizations were also collected during the follow-up period for all patients enrolled in the PROOF registry. Use of supplemental oxygen and pulmonary rehabilitation were also monitored during the follow-up period.
Data Analysis
Chi-square tests were used to compare baseline characteristics in patients who survived versus patients who died. All other QoL outcomes and HCRU were summarized descriptively. For the summary statistics of QoL outcomes, patients were included in the calculation if they had a QoL score available for the specified time point, regardless of whether they had a baseline score. For mean changes in QoL from Month 0, patients were included in the calculation for a time point if they had a QoL score available for that time point and a corresponding score at Month 0. For longitudinal QoL scores and HCRU, missing data were considered missing at random and were not imputed.
Cox proportional hazards models were used to assess associations of baseline covariates with mortality during the follow-up period using a univariate model. Cox proportional hazard models were also used to assess associations of QoL measures at baseline with mortality in all patients during the follow-up period using univariate and multivariate models. The proportional hazards assumption was assessed using a Schoenfeld residual test. During univariate analyses, individual baseline covariates or QoL measures were included separately as the only predictor per model. During multivariate analyses, individual QoL measures were modeled separately and adjusted for covariates [39]. In model covariates that had a maximum of 25% of data missing, multiple imputation was used, and missing data were considered missing at random. Five complete datasets were generated and analyzed using Cox proportional hazard models, and the results of the five analyses were then combined to generate the final result. To contextualize the impact of imputation, univariate and multivariate analyses without multiple imputations were also performed. Results of all univariate and multivariate analyses were presented using hazard ratios, 95% confidence intervals, and p values. A p value < 0.05 was considered significant.
Data in this study were collected using the electronic case report forms (eCRF) and end-of-study registration forms. A programmed database received all information collected in the eCRF and automated edit checks were performed. A contract research organization was responsible for the management of data, including data-quality checks, and was also required to produce a data review strategy to highlight the quality-check method performed on the data. An extensive quality-control audit was conducted to ensure data quality. The software analysis programs used for these analyses were Python 2.7 (Python Software Foundation, USA) and R version 3.6.1 (R Foundation for Statistical Computing, Austria).
Results
Patient Demographics
Between October 2013 and January 2016, 277 patients with IPF were enrolled in the PROOF registry. The mean (SD) age of the overall PROOF cohort was 69.6 (8.6) years, and the majority of patients enrolled were male (76.9%), white (92.1%), and were former or current smokers (66.8 and 6.5%, respectively; Table S1). At baseline, mean (SD) percent predicted FVC was 80.6% (19.9) and mean (SD) percent predicted DLco was 46.9% (13.8; Table S1). Patients had mean (SD) 2.5 (1.8) comorbidities at enrollment and the mean (SD) time since diagnosis to the end of enrollment was 1284.1 (921.3) days. Supplemental oxygen was used by 24.2% of all patients enrolled in the PROOF registry at any point throughout the study (Table S1), and 14 patients (5.1%) received a lung transplant during the follow-up period. Of the 277 patients enrolled in the PROOF registry, 233 patients received pirfenidone treatment at any time during the follow-up period and the mean (SD) duration of pirfenidone treatment was 635 (465) days. Previous treatment for IPF other than pirfenidone is presented in Table S1 in the Supplementary Material. Further details on the demographic and baseline characteristics of this patient population have been previously reported [32].
QoL Outcomes in all Patients
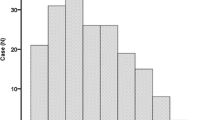
The percentage of patients who experienced problems in each of the EQ-5D-5L categories over 24 months is presented in Fig. 1. Mean cough VAS (1.4% of patient data missing at baseline), EQ-5D VAS (5.0% of patient data missing at baseline), and SGRQ total and sub-scores (24.5% of patient data missing at baseline) over 24 months are presented in Fig. 2. The mean (SD) change from baseline in cough VAS scores at Months 12 and 24 post-inclusion were 3.8 (26.6) mm and 8.4 (20.9) mm, respectively (Table 1). The mean change from baseline at Months 12 and 24 post-inclusion for EQ-5D VAS, and SGRQ total and sub-scores are also presented in Table 1.
QoL outcomesa over 24 months in all patients enrolled in the PROOF registry. EQ-5D EuroQoL-5 dimensions Health Questionnaire, EQ-5D-5L EuroQoL-5 dimensions-5 levels Health Questionnaire, QoL quality of life, SD standard deviation, SGRQ St. George’s Respiratory Questionnaire, VAS visual analogue scale. aFor EQ-5D scores, a higher score indicates better QoL. For cough VAS, a higher score indicates worse cough. For SGRQ total and all sub-scores, a higher score indicates worse impairments. bData were considered missing at random and were not imputed
QoL Associations with Mortality for all Patients Enrolled in the Registry
Among all patients enrolled in the PROOF registry, 64 (23.1%) deaths were recorded during the 24-month follow-up period; 70.3% (n = 45) of deaths were considered IPF-related, no deaths were considered treatment-related, 20.3% (n = 13) of deaths were neither IPF- nor treatment-related and an explanation was not provided for 9.4% (n = 6) of deaths. Patients who died during the 24-month follow-up period had lower mean percent predicted FVC (p = 0.006), mean percent predicted DLco (p < 0.001), and mean EQ-5D VAS score (p = 0.005), and greater mean SGRQ total score (p < 0.001) and mean SGRQ symptoms (p = 0.001), activity (p = 0.003) and impact (p = 0.001) sub-scores at baseline compared with patients who survived.
Analyses of univariate associations between covariates revealed that age, percent predicted FVC, percent predicted DLco, smoking status, and supplementary oxygen use at registry inclusion were significantly associated with mortality (p = 0.04, p < 0.005, p < 0.005, p = 0.03 and p = 0.03, respectively); however, sex was not significantly associated with mortality (p = 0.72).
In univariate analyses, EQ-5D VAS score, SGRQ total score, and all SGRQ sub-scores at baseline were significantly associated with mortality (p < 0.005 for all). However, there was no significant association between cough VAS at baseline and mortality (p = 0.3999; Table 2). In multivariate analyses adjusted for covariates, SGRQ total score and SGRQ impact and symptoms sub-scores were significantly associated with mortality (p = 0.0042, p = 0.0115 and p = 0.0037, respectively; Table 2).
Results from univariate and multivariate models without multiple imputation are presented in Table S2 in the Supplementary Material. Briefly, in univariate analyses without multiple imputation, EQ-5D VAS and SGRQ total score and sub-scores were significantly associated with mortality (p < 0.005 for all), whereas cough VAS was not. In multivariate analyses, without multiple imputation, adjusted for covariates, only SGRQ total score and SGRQ impact sub-score were significantly associated with mortality (p < 0.05 for both; Table S2).
HCRU for All Patients Enrolled in the Registry
During the follow-up period, a total of 3514 outpatient consultations were required by 261 (94.2%) of the 277 patients enrolled in the PROOF registry, and the mean (SD) number of outpatient consultations (IPF- or non-IPF-related) per patient was 13.5 (9.6) consultations (Table S3). The majority of outpatient consultations were with general practitioners (43.1%), followed by other medical specialists (24.4%) and pulmonologists (21.7%; Table S3). Most of these consultations took place at the caregiver’s office/outpatient department (87.2%) and were IPF-related (81.8%; Table S3).
A total of 103 patients experienced a total of 182 hospitalizations during the follow-up period, and of those patients, 27 (26%) died. Moreover, of the 103 patients who experienced a hospitalization, 64 experienced a respiratory hospitalization related to IPF, of whom 21 (33%) died during the follow-up period. The mean (SD) duration of hospitalization was similar for non-respiratory and respiratory-related hospitalization at 7.2 (9.6) days and 7.5 (9.1) days, respectively (Table S4). In cases of respiratory-related hospitalization, pulmonologists were the most common care provider (81.0%), while in non-respiratory-related hospitalization cases, other medical specialists were the most common care provider (93.4%; Table S4). Overall, 67 (24.2%) patients received supplemental oxygen and 76 (27.4%) patients received pulmonary rehabilitation.
Discussion
The PROOF registry provides valuable evidence and insights on longitudinal QoL outcomes and their baseline association with mortality from a real-world population of patients with IPF in Europe. Unlike clinical trials, which have strict inclusion and exclusion criteria, patients included in the PROOF registry were not excluded on the basis of disease severity, comorbidities, or prescribed medications. Furthermore, the follow-up period for the PROOF registry and other real-world registries is generally longer than that observed in clinical trials and, as a result, data collected from registries may be considered to be more representative of clinical practice than data from clinical trials.
In this study, univariate and multivariate analyses of data from patients enrolled in the PROOF registry suggested that baseline QoL may be associated with mortality in patients with IPF. Indeed, univariate analyses identified that EQ-5D VAS score, SGRQ total score and all sub-scores at baseline were significantly associated with mortality; however, during multivariate analyses adjusted for covariates, only SGRQ total score, SGRQ impact score and SGRQ symptom score at baseline were associated with mortality. During the follow-up period, EQ-5D VAS, SGRQ total scores and SGRQ impact scores remained generally stable, whereas slight worsening in cough VAS, SGRQ symptoms score and SGRQ activities score were observed in all patients. Patients also frequently reported moderate, severe or extreme impairments in mobility and usual activity on the EQ-5D-5L. When considered in combination with the SGRQ activity sub-scores, the EQ-5D-5L scores highlight that the main impairments reported by patients with IPF enrolled in the PROOF registry were related to mobility and activity.
The longitudinal QoL findings from the PROOF registry add to existing longitudinal QoL data previously reported by other real-world registries including the German INSIGHTS-IPF registry (N = 424; continuously enrolling from November 2012) [10] and the Australian IPF registry (N = 516; conducted from February 2012 to August 2014) [9]. Longitudinal data from patients enrolled in the INSIGHTS-IPF and Australian IPF registries showed a significant worsening of SGRQ total scores over time [9, 10], in contrast to PROOF, where SGRQ total score remained stable during the follow-up period. Furthermore, the INSIGHTS-IPF registry reported a significant worsening of EQ-5D VAS [10], whereas the PROOF registry reported minimal changes in EQ-5D VAS during the follow-up period. Therefore, whilst many patients report a decline in QoL over time, differences in data reported from each registry may be dependent on many factors including disease severity, treatment use, study population, study duration and healthy survivor bias.
The PROOF registry is not the first registry to report data on the association between QoL and mortality in patients with IPF. Univariate analyses from the INSIGHTS-IPF registry and the IPF-PRO registry (N = 662; patients enrolled from June 2014 to October 2017; 54.0% of patients receiving pirfenidone or nintedanib) have identified an association between EQ-5D VAS and mortality [10, 22]. However, during multivariate analyses adjusted for clinical characteristics, EQ-5D VAS was not associated with mortality in the PROOF registry and IPF-PRO registry [22]. Furthermore, univariate and multivariate analyses from the INSIGHTS-IPF registry found that mortality was significantly associated with a worse SGRQ score at last available follow-up [10]. Similar to the PROOF and INSIGHTS-IPF registries, univariate analyses from the IPF-PRO registry also reported an association between SGRQ total score and all sub-scores, and mortality or lung transplant [10, 22]. However, when adjusted for clinical characteristics, the IPF-PRO registry found that only SGRQ total score, and activity and symptom sub-scores were associated with mortality or lung transplant, whereas the PROOF registry reported an association between SGRQ total score, and impact and symptoms sub-scores. Additionally, univariate analyses from the Australian IPF registry reported an association between baseline SGRQ total scores and mortality; however, during multivariate analyses no significant relationship between baseline SGRQ total scores and mortality was identified [9]. It is important to note that when performing multivariate analyses adjusted for clinical characteristics, the INSIGHTS-IPF registry, the IPF-PRO registry, the Australian IPF registry and the PROOF registry did not adjust for an identical group of clinical characteristics. In general, the PROOF registry adjusted for a larger number of clinical characteristics compared with the other registries, and was the only registry to adjust for smoking status [10, 22].
Despite some differences in the association between SGRQ sub-scores and mortality across the PROOF, INSIGHTS-IPF and IPF-PRO registries, an association between SGRQ total score and mortality has consistently been reported in all three real-world registries. Furthermore, a recent analysis of data from the IPF-PRO registry that used adjusted regression models found that worsening SGRQ total score was associated with disease severity [24]. Additionally, univariate analyses from a single-center Japanese cohort identified that SGRQ total score and sub-scores were predictive of mortality, and during multivariate analyses, SGRQ total score was found to be an independent predictor of mortality [23].
The HCRU data collected highlights the high HCRU burden for patients with IPF enrolled in the PROOF registry. HRCU data have also been reported during previous longitudinal studies of patients with IPF. A recent study (conducted from 2000 to 2015) including patients with IPF (n = 691) and age- and gender-matched controls (n = 3452) reported that patients with IPF had an increased HCRU compared with control patients. This observed increase in HCRU in patients with IPF was sustained over 5 years, and may have resulted from higher rates of diagnostic procedures and healthcare visits post-diagnosis, compared with control patients [29]. Additionally, during a 5-year population-level longitudinal study (from 2008 to 2013), based on data from the French hospital discharge database, 43.7% of patients with IPF were hospitalized due to respiratory infections, and 36.5% were hospitalized due to acute respiratory worsening [40]. These reports are lower than the number of respiratory-related hospitalizations in the PROOF registry; however, this database was not developed for epidemiological purposes, which may, in part, explain any differences in the number of hospitalizations, and it is also possible that patients included in the PROOF registry may have had a more progressive phenotype in comparison with patients included in the French database. The IPF-PRO registry reported supplemental oxygen use at baseline, with 19.6% of patients enrolled in the registry using supplemental oxygen at rest [39], similar to the levels of supplemental oxygen use reported in the PROOF registry.
There are several limitations of the PROOF registry that should be considered when interpreting longitudinal QoL and healthcare use data from this analysis. Many forms of bias or confounding factors can exist in real-world registries and as such, these factors may have impacted data collected in the PROOF registry. As the majority of patients enrolled in the PROOF registry were diagnosed with IPF prior to their inclusion in the registry, it is possible that selection bias may have affected the study enrollment process. Enrollment and survival in the registry may also have been biased by the exclusion of patients who were enrolled in a clinical trial, as these patients would be expected to have less severe disease and fewer comorbidities compared with those patients who were not eligible for a clinical trial, and therefore eligible to enroll in the PROOF registry. It is also feasible that no significant worsening of SGRQ total score was observed as a result of patients with longer follow-up periods being healthier and experiencing a better QoL versus patients with shorter follow-up periods. Consequently, the longitudinal QoL data collected in the PROOF registry may have been impacted by a healthy survivor bias. Additionally, it is possible that differences in longitudinal QoL between individual patients may be hidden by relatively minor overall changes to QoL over time. Due to limited patient numbers, it was not possible to perform any subgroup analyses to identify if such differences existed in the data from the PROOF registry. Furthermore, the registry included a relatively small population of patients from a limited geographical area, and the use of antifibrotics in Belgium is limited to centers with experience in diagnosis and treatment of IPF. As the different types of healthcare systems used in many countries could impact HCRU, it is possible that the HCRU in other countries may differ from the HCRU data collected in the PROOF registry. Therefore, the PROOF patient population may not be fully representative of populations of patients with IPF in different countries. Finally, as the number of patients who had not been treated with pirfenidone was low, it is not possible to compare with the pirfenidone-treated population.
Conclusions
In conclusion, the PROOF registry provided valuable, real-world data on the association between baseline QoL and mortality, and longitudinal HCRU and QoL outcomes in patients with IPF over 24 months. In general, EQ-5D VAS, SGRQ total scores and SGRQ impact scores remained stable during the follow-up period; however, cough VAS, SGRQ activity scores and SGRQ symptom scores increased in all patients. Univariate and multivariate analyses, the latter of which were adjusted for a wide range of clinical characteristics, identified that SGRQ may be an independent prognostic factor in patients with IPF. The HCRU data reported in this manuscript provided an important insight into the high HCRU burden for patients with IPF enrolled in the PROOF registry. Overall, these findings are aligned with existing registry-based literature regarding the association between QoL and mortality; however, there are differences in the results reported in the PROOF registry versus other IPF registries, which may be due to use of different methodologies when analyzing data from each registry.
References
Ley B, Collard HR, King TE Jr. Clinical course and prediction of survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011;183:431–40.
Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824.
American Cancer Society. Cancer Facts & Figures 2019. 2019. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf. Accessed 14 Dec 2021.
Belkin A, Albright K, Swigris JJ. A qualitative study of informal caregivers’ perspectives on the effects of idiopathic pulmonary fibrosis. BMJ Open Respir Res. 2014;1:e000007.
Overgaard D, Kaldan G, Marsaa K, Nielsen TL, Shaker SB, Egerod I. The lived experience with idiopathic pulmonary fibrosis: a qualitative study. Eur Respir J. 2016;47:1472–80.
Russell AM, Ripamonti E, Vancheri C. Qualitative European survey of patients with idiopathic pulmonary fibrosis: patients’ perspectives of the disease and treatment. BMC Pulm Med. 2016;16:10.
van Manen MJ, Birring SS, Vancheri C, et al. Cough in idiopathic pulmonary fibrosis. Eur Respir Rev. 2016;25:278–86.
Kreuter M, Swigris J, Pittrow D, et al. Health related quality of life in patients with idiopathic pulmonary fibrosis in clinical practice: insights-IPF registry. Respir Res. 2017;18:139.
Glaspole IN, Chapman SA, Cooper WA, et al. Health-related quality of life in idiopathic pulmonary fibrosis: Data from the Australian IPF Registry. Respirology. 2017;22:950–6.
Kreuter M, Swigris J, Pittrow D, et al. The clinical course of idiopathic pulmonary fibrosis and its association to quality of life over time: longitudinal data from the INSIGHTS-IPF registry. Respir Res. 2019;20:59.
Noble PW, Albera C, Bradford WZ, et al. Pirfenidone in patients with idiopathic pulmonary fibrosis (CAPACITY): two randomised trials. Lancet. 2011;377:1760–9.
King TE Jr, Bradford WZ, Castro-Bernardini S, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2083–92.
Richeldi L, du Bois RM, Raghu G, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2071–82.
Kreuter M, Bendstrup E, Russell AM, et al. Palliative care in interstitial lung disease: living well. Lancet Respir Med. 2017;5:968–80.
Swigris JJ, Brown KK, Behr J, et al. The SF-36 and SGRQ: validity and first look at minimum important differences in IPF. Respir Med. 2010;104:296–304.
Tsai APY, Hur SA, Wong A, et al. Minimum important difference of the EQ-5D-5L and EQ-VAS in fibrotic interstitial lung disease. Thorax. 2020;76:37–43.
Yates H, Adamali HI, Maskell N, Barratt S, Sharp C. Visual analogue scales for interstitial lung disease: a prospective validation study. QJM. 2018;111:531–9.
Belkin A, Swigris JJ. Health-related quality of life in idiopathic pulmonary fibrosis: where are we now? Curr Opin Pulm Med. 2013;19:474–9.
Kreuter M, Wuyts WA, Wijsenbeek M, et al. Health-related quality of life and symptoms in patients with IPF treated with nintedanib: analyses of patient-reported outcomes from the INPULSIS ® trials. Respir Res. 2020;21:36.
Cheng JZ, Wilcox PG, Glaspole I, et al. Cough is less common and less severe in systemic sclerosis-associated interstitial lung disease compared to other fibrotic interstitial lung diseases. Respirology. 2017;22:1592–7.
Nishiyama O, Taniguchi H, Kondoh Y, et al. Health-related quality of life does not predict mortality in idiopathic pulmonary fibrosis. Sarcoidosis Vasc Diffuse Lung Dis. 2012;29:113–8.
Case AH, Hellkamp AS, Neely ML, et al. Associations between patient-reported outcomes and death or lung transplant in idiopathic pulmonary fibrosis. Data from the idiopathic pulmonary fibrosis prospective outcomes registry. Ann Am Thorac Soc. 2020;17:699–705.
Furukawa T, Taniguchi H, Ando M, et al. The St George’s Respiratory Questionnaire as a prognostic factor in IPF. Respir Res. 2017;18:18.
O’Brien EC, Hellkamp AS, Neely ML, et al. Disease severity and quality of life in patients with idiopathic pulmonary fibrosis: a cross-sectional analysis of the IPF-PRO registry. Chest. 2020;157:1188–98.
Gao J, Kalafatis D, Carlson L, et al. Baseline characteristics and survival of patients of idiopathic pulmonary fibrosis: a longitudinal analysis of the Swedish IPF Registry. Respir Res. 2021;22:40.
du Bois RM, Weycker D, Albera C, et al. Forced vital capacity in patients with idiopathic pulmonary fibrosis: test properties and minimal clinically important difference. Am J Respir Crit Care Med. 2011;184:1382–9.
du Bois RM, Weycker D, Albera C, et al. Six-minute-walk test in idiopathic pulmonary fibrosis: test validation and minimal clinically important difference. Am J Respir Crit Care Med. 2011;183:1231–7.
Corral M, DeYoung K, Kong AM. Treatment patterns, healthcare resource utilization, and costs among patients with idiopathic pulmonary fibrosis treated with antifibrotic medications in US-based commercial and Medicare Supplemental claims databases: a retrospective cohort study. BMC Pulm Med. 2020;20:188.
Farrand E, Iribarren C, Vittinghoff E, et al. Impact of idiopathic pulmonary fibrosis on longitudinal healthcare utilization in a community-based cohort of patients. Chest. 2021;159:219–27.
Lassenius MI, Toppila I, Pontynen N, et al. Forced Vital Capacity (FVC) decline, mortality and healthcare resource utilization in idiopathic pulmonary fibrosis. Eur Clin Respir J. 2019;7:1702618.
Olson AL, Maher TM, Acciai V, et al. Healthcare resources utilization and costs of patients with non-IPF progressive fibrosing interstitial lung disease based on insurance claims in the USA. Adv Ther. 2020;37:3292–8.
Wuyts WA, Dahlqvist C, Slabbynck H, et al. Baseline clinical characteristics, comorbidities and prescribed medication in a real-world population of patients with idiopathic pulmonary fibrosis: the PROOF registry. BMJ Open Respir Res. 2018;5:e000331.
Wuyts WA, Dahlqvist C, Slabbynck H, et al. Longitudinal clinical outcomes in a real-world population of patients with idiopathic pulmonary fibrosis: the PROOF registry. Respir Res. 2019;20:231.
Morice AH, Fontana GA, Belvisi MG, et al. ERS guidelines on the assessment of cough. Eur Respir J. 2007;29:1256–76.
Ferrer M, Villasante C, Alonso J, et al. Interpretation of quality of life scores from the St George’s Respiratory Questionnaire. Eur Respir J. 2002;19:405–13.
Swigris JJ, Esser D, Wilson H, et al. Psychometric properties of the St George’s Respiratory Questionnaire in patients with idiopathic pulmonary fibrosis. Eur Respir J. 2017;49:1601788.
Yorke J, Jones PW, Swigris JJ. Development and validity testing of an IPF-specific version of the St George’s Respiratory Questionnaire. Thorax. 2010;65:921–6.
van Reenen M. EQ-5D-5L User Guide: Basic information on how to use the EQ-5D-5L instrument. EuroQol Research Foundation. 2015. https://euroqol.org/publications/user-guides/. Accessed 14 Dec 2021.
Snyder L, Neely ML, Hellkamp AS, et al. Predictors of death or lung transplant after a diagnosis of idiopathic pulmonary fibrosis: insights from the IPF-PRO Registry. Respir Res. 2019;20:105.
Cottin V, Schmidt A, Catella L, et al. Burden of idiopathic pulmonary fibrosis progression: a 5-year longitudinal follow-up study. PLoS ONE. 2017;12:e0166462.
Acknowledgments
Funding
This study, and the Pulmonary Therapy Rapid Service Fee, was sponsored by F. Hoffmann-La Roche, Ltd.
Medical Writing and/or Editorial Assistance
Medical writing support was provided by Ceilidh McConnachie, MSc, and Leigh Clements, PhD, of CMC AFFINITY, McCann Health Medical Communications, and was funded by F. Hoffmann-La Roche, Ltd.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole and have given their approval for this version to be published.
Author Contributions
Wim A. Wuyts, Caroline Dahlqvist, Hans Slabbynck, Marc Schlesser and Benjamin Bondue were involved in the conception and design of the PROOF registry. Data collection was conducted by Wim A. Wuyts, Caroline Dahlqvist, Hans Slabbynck, Marc Schlesser and Benjamin Bondue. Data analysis was conducted by Karen Bartley and Shemra Rizzo. All authors contributed towards the interpretation of the results, and actively participated in drafting and revising this manuscript. All authors were involved in the final approval of the manuscript version to be published and agree to be accountable for all aspects of the work.
Disclosures
Wim A. Wuyts, Caroline Dahlqvist, Hans Slabbynck and Benjamin Bondue have received consulting and/or lecture fees from F. Hoffman-La Roche, Ltd. and Boehringer Ingelheim. Marc Schlesser, Natacha Gusbin, Christophe Compere and Sofie Maddens have nothing to disclose. Klaus-Uwe Kirchgaessler and Shemra Rizzo are employees of Roche-Genentech and hold shares. Karen Bartley is a former employee of Roche-Genentech and holds shares.
Compliance with Ethics Guidelines
The PROOF registry was conducted in accordance with the International Council on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use, Guidelines for Good Clinical Practice, and local legal and regulatory requirements. Patients were required to provide informed consent prior to inclusion. PROOF is registered with the relevant authorities in Belgium and Luxembourg, and received ethics approval from Comité National d'Éthique et de Recherche (CNER) N201309/03-12 September 2013 and Comité National de Protection des Données (CNDP) for Luxembourg.
Data Availability
Qualified researchers may request access to individual patient-level data through the clinical study data request platform (https://vivli.org/). Further details on Roche's criteria for eligible studies are available here: https://vivli.org/members/ourmembers/). For further details on Roche's Global Policy on the Sharing of Clinical Information and how to request access to related clinical study documents, see here: (https://www.roche.com/research_and_development/who_we_are_how_we_work/clinical_trials/our_commitment_to_data_sharing.htm)
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wuyts, W.A., Dahlqvist, C., Slabbynck, H. et al. Quality of Life and Healthcare Resource Use in a Real-world Patient Population with Idiopathic Pulmonary Fibrosis: The PROOF Registry. Pulm Ther 8, 181–194 (2022). https://doi.org/10.1007/s41030-022-00187-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-022-00187-8