Abstract
Introduction
The Respimat® Soft Mist™ Inhaler (SMI) is a hand-held device that generates an aerosol with a high fine-particle fraction, enabling efficient lung deposition. Inhalation therapy for children should be safe and effective. This study aimed to assess the success and the quality of inhalation maneuvers among children using the Respimat SMI.
Methods
This single-center study was conducted at Mainz University Hospital, Germany, between March 2006 and August 2006. Ninety-nine children, aged 4–12 years, with asthma bronchiale or other atopic diseases, and their healthy siblings were included. Children with serious respiratory conditions such as cystic fibrosis or any chronic destructive or severe lung disease were excluded. Each child performed three inhalation maneuvers using the Respimat SMI. Inspiratory flow rate, inhaled volume, and timing of actuation for each inhalation maneuver were recorded using a pneumotachograph. Successful use and quality of inhalation maneuvers (inspiratory flow rate, theoretical inhaled dose fraction, and estimated lung deposition of the aerosol cloud) were assessed. Results were compared with respect to prior experience of inhaler use and between two age groups (4–8 years and 9–12 years).
Results
Ninety of 99 children achieved one or more successful maneuver. Overall, 75.1 % of inhalation maneuvers performed with the Respimat SMI were successful; the greatest success was seen in older versus younger children. Overall median estimated lung deposition was 67 %. Median inspiratory flow was 41.5 L/min, with slower rates noted in the younger children. Fifty-two percent of children inhaled faster than 40.0 L/min. Prior inhaler experience imparted no benefit in terms of success of inhalation maneuvers, overall, but was associated with some group differences in inhalation flow rate.
Conclusion
Children can perform a successful inhalation maneuver with the Respimat SMI, with the greatest success rate in children aged >5 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inhalation therapy is a cornerstone in the management of chronic respiratory diseases. Direct drug delivery to the lung maximizes therapeutic outcome at the lowest possible dose while minimizing unwanted systemic side effects [1–3]. Treatment success relies on efficient operation of inhalation devices [4]. For children, achieving effective inhaler use can be challenging because of their different physiological characteristics and comparatively limited coordination [4].
The Respimat® Soft Mist™ inhaler (SMI) is a novel, hand-held, propellant-free, multidose inhalation device that generates a slow-moving, long-lasting aerosol cloud containing a high fine-particle fraction that enables efficient drug delivery to the lungs [5–10]. For optimal use of the Respimat SMI, the patient is directed to breathe out slowly and deeply. After exhalation the patient is asked to close his or her lips around the end of the mouthpiece [5]. The dose-release button is then pressed while the patient takes a slow, deep inhalation through the mouth; it is recommended that the patient hold this breath in for 10 s [5]. Although the Respimat SMI requires some degree of hand–breath synchronization, it may offer enhanced drug delivery in patients who have difficulties in actuating and coordinating inhalation when using a pressurized metered dose inhaler (MDI) [5].
A number of studies have shown that patients may find it easier to inhale with the Respimat because of the slow release of the aerosol—approximately 1.5 s, compared with approximately 0.2 s for a chlorofluorocarbon MDI, and 0.3 s for a hydrofluoroalkane MDI—and low cloud velocity (<0.8 m/s) with the Respimat [7, 11, 12]. However, it is possible that longer spray duration could also lead to a certain “loss” of aerosol, if inspiration stops before the end of the aerosol release.
A clinical study confirmed that the design and operative features of the Respimat SMI allows successful use in the pediatric population (children aged 6–15 years) and enabled a twofold reduction in the nominal dose for the treatment of asthma compared with inhalation from an MDI with a spacer [9]. The aim of the current study was to evaluate the use of the Respimat SMI in children aged 4–12 years.
Materials and Methods
Study Design
This single-center study was conducted at Mainz University Hospital, Germany, between March 2006 and August 2006. The objective was to assess the success and quality of inhalation maneuvers among children using the Respimat® SMI (Boehringer Ingelheim Pharma GmbH & Co KG, Ingelheim, Germany) in two age groups (4–8 years and 9–12 years), and the influence of prior inhaler experience. The exclusion of children with serious respiratory conditions eliminated functional restrictions and was in line with the study objective to investigate potential age-related handling issues with a new SMI. The study was conducted in accordance with Good Clinical Practice and applicable regulatory requirements. This was not a “clinical trial” according to the German Drug or Medical Devices Act as no medication was administered. Institutional review board approval was obtained. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients for being included in the study.
Study Participants
Children aged 4–12 years, of either sex, with asthma bronchiale or atopic diseases, and their healthy siblings were enrolled into the study at the Pediatric Pulmonology and Allergology Outpatient Clinic, Mainz University Hospital. Children with or without previous inhaler experience were included, and any devices used in the past 12 months were documented. Children with serious respiratory conditions such as cystic fibrosis or any chronic destructive or severe lung disease were excluded.
Device and Training
A Respimat SMI training kit that delivered an aerosol cloud containing no active medication was used. All children received standardized training on how to achieve a slow and deep inhalation maneuver using the training kit. During the training, the investigator gave three demonstrations of optimal inhaler technique (or two demonstrations for children aged 9–12 years). Next, the child was allowed three trial inhalations (or two trial inhalations for children aged 9–12 years) during which the investigator gave instructions on how to improve his or her technique, if required. Training was concluded by a demonstration of the measurement equipment plus one further test inhalation. The children were not given any help using the inhaler from parents or caregivers, and no accessory devices such as spacers were used.
Assessments
Maneuver assessment was based on inhalation flow profiles, recorded using a pneumotachograph (JAEGER® MasterScope, CareFusion Corporation, Germany) which was connected to the Respimat SMI. The profiles included inspiratory flow rate, inhaled volume, and timing of actuation for each inhalation maneuver. Three consecutive inhalation maneuvers, after the training maneuvers, were recorded and analyzed for each patient during a single visit.
Maneuver failure was defined as Respimat SMI actuation errors (i.e., no actuation, actuation ≥3 s before inhalation, actuation after inhalation), exhalation during the inhalation maneuver (including possible coughing triggered by inhalation), or inhalation volume <0.5 L (Fig. 1). If none of these errors occurred, the inhalation maneuver was defined as successful.
For each successful maneuver, three inhalation quality parameters were determined: the inspiratory flow rate (L/min), the theoretical inhaled fraction (%), and the estimated lung deposition (%) that would have been achieved. The theoretical inhaled fraction (i.e., the percentage of the placebo fine aerosol cloud inhaled by the patient) was calculated according to spray duration, actuation time point, and inhalation duration (See Appendix Fig. A1).
Estimated lung deposition of the placebo aerosol cloud was calculated by subtracting the extrathoracic deposition (approximately proportional to inspiratory flow rate [13]) from the theoretical inhaled fraction (See Appendix Fig. A2).
Statistical Analyses
Median values for the three inhalation quality parameters were recorded for each child who managed one or more successful inhalation maneuver. Statistical analyses were carried out using SPSS (IBM, Armonk, NY, USA [used at University of Mainz]) and SAS (SAS Institute, Inc., Cary, NC, USA [used at Boehringer Ingelheim]). Error rates were calculated for all inhalation maneuvers combined. Differences in the frequency of error rates between groups were analyzed using the Mann–Whitney U test and logistic regression. Differences in quality parameters between groups were analyzed using the Mann–Whitney U test. Linear regression was used for the analyses of dependency of the quality parameters and age.
Results
Study Participants
A total of 99 children were enrolled into the study (n = 59 aged 4–8 years; n = 40 aged 9–12 years). Of these 99 children, 15 had no previous experience with inhalation devices because they had not been diagnosed as having any lung disease, and were hence described as “healthy.” Demographics and prior inhaler experience are shown in Table 1.
Inhalation Success
Overall, 223/297 (75.1 %) of the inhalation maneuvers in 99 children were successful. Of the 74 unsuccessful maneuvers, 14 (18.9 %) were due to more than one type of user error. Actuation error occurred in 33/297 (11.1 %) maneuvers (3/297 [1.0 %] maneuvers with actuation after inhalation and 30/297 [10.1 %] maneuvers with missing actuation), exhalation occurred in 25/297 (8.4 %) maneuvers, and inhalation <0.5 L occurred in 33/297 (11.1 %) maneuvers. The rates of maneuvers with only one error were actuation error only 27/297 (9.1 %), inhalation volume <0.5 L only 19/297 (6.4 %), and exhalation error only 14/297 (4.7 %).
The frequency of successful maneuvers was numerically higher in the older group of children than in the younger group (99/120 [82.5 %] vs. 124/177 [70.1 %]); however, there was no significant difference in error type between groups (p > 0.05). The most frequent error in children aged 4–8 years was an inhalation volume <0.5 L, whereas poor coordination of the dose release with inhalation was most common in children aged 9–12 years (Fig. 2). None of the children aged 4 years (n = 3 children, nine maneuvers) were able to perform a successful inhalation, mainly because of coordination problems. In contrast, 5/12 (41.7 %) maneuvers of children aged 5 years (n = 4) and 24/27 (88.9 %) maneuvers of those aged 6 years (n = 9) had successful maneuvers (Appendix Table A1).
Inhalation Quality
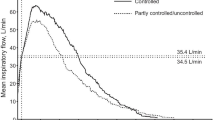
Overall, 90 of 99 children managed one or more successful inhalation maneuvers and only those children with successful maneuvers were included in the calculation of inhalation quality parameters (inspiratory flow rate, the theoretical inhaled fraction, and the estimated lung deposition). The median estimated lung deposition in this group was 66.9 % (Appendix Fig. A3). A difference in lung deposition was seen between age groups: children aged 4–8 years (n = 51) achieved a higher median estimated lung deposition (74.2 %) than children aged 9–12 years (n = 39) (61.7 %) (Fig. 3a). The linear regression shows a linear dependency between age and estimated lung deposition: the older the child, the lower the estimated lung deposition (p < 0.01) (Fig. 3b). Median inspiratory flow rate in all 90 children was 41.5 L/min (range, 7.9–113.5 L/min). Flow rate was >40.0 L/min in 52.2 % of children (Appendix Fig. A4). Inspiratory flow rate was slower in children aged 4–8 years than in the older group (median 30.6 L/min versus 49.9 L/min) (Fig. 4a). There is a linear trend between age and inspiratory flow: the older the child, the higher the flow (p < 0.01) (Fig. 4b). Total inhaled volumes increased with the age of the children (Appendix Fig. A5).
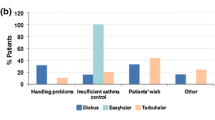
Effect of Prior Inhaler Experience
The percentage of successful maneuvers in children with no previous experience using inhalation devices was similar to that in experienced children (73.3 % [33/45] vs. 75.0 % [189/252], p > 0.5). Examination of data according to the type of inhaler previously used revealed some group differences: children who had previously used dry powder inhalers (DPIs), Autohaler® (Teva Deutschland, Ulm, Germany), or MDIs had the highest success rates (Appendix Fig. A6; Table 2); the lowest success rate was seen in children with prior experience using inhalers with spacer devices (65.7 % [71/108]).
Concerning the inhalation quality (determined from the 90 children with at least one successful maneuver), median estimated lung deposition was comparable in the nonexperienced and experienced subgroups (69 vs. 67 %, p > 0.1), but was lower in the group of children experienced with DPIs relative to those not experienced with DPIs (61 vs. 72 %, p < 0.01). Estimated lung deposition was also lower in children experienced with the Autohaler versus those with no prior use (60 vs. 71 %, p < 0.01). For those who have used an MDI versus those with no prior use of any MDI (60 vs. 69 %, p > 0.1) there was no influence on the estimated lung deposition. The highest level of lung deposition was seen in children with experience using nebulizers with spacers (72 %).
The median inspiratory flow rate in nonexperienced children was lower than in experienced children (29.7 vs. 44.0 L/min). High median flow rates of 49.9 L/min were recorded in children who had used a DPI or Autohaler previously, and of 50.0 L/min in those experienced with the MDI. A relatively low mean inspiratory flow rate (39 L/min) was seen among children with experience using nebulizers or MDIs with spacers.
Of interest, in 42 of 297 (14.1 %) inhalations, the children momentarily caught their breath during the test inhalations, causing a sudden drop in airflow during the inhalation maneuver. This phenomenon was more common in the 4–8-year-olds (affecting 36/177 [20.3 %] inhalations) than in the older group (6/120 [5.0 %] inhalations, p < 0.05). Since there was no associated exhalation during these instances, the maneuvers were classified as successful unless any of the other two failure criteria occurred.
Discussion
Efficient respiratory drug delivery to the lungs relies on the quality of the inhalation maneuver, which is in turn influenced by device design characteristics. The Respimat SMI generates a slow-moving aerosol cloud that is independent of inspiratory flow rate [7, 13, 14].
The objective of the current study was to assess the success of inhalation maneuvers and the quality of inhalation breathing patterns among children aged 4–12 years using Respimat SMI; other aspects of device handling were not evaluated. The high percentage of successful inhalation maneuvers (≈75 %) in children aged ≥5 years suggests that these children are able to use the Respimat SMI correctly without adult assistance or breathing aids (e.g., spacer). Conversely, children aged below 5 years are less able to perform a successful inhalation maneuver with the Respimat SMI; however, information is limited, as only three children aged 4 years were included. These younger children had problems coordinating actuation and inspiration, inhaling slowly and continuously, and holding their breath after inhaling. However, in these children, successful inhalation can be achieved using a spacer and with parental/caregiver help, as appropriate to their age [15].
In a previous study of children aged 4–14 years using other devices, the rate of correct inhalation maneuvers achieved after training was 88.5 % with the Diskus® (GlaxoSmithKline GmbH & Co. KG, Munich, Germany), 65.4 % with the Turbohaler® (AstraZeneca GmbH, Wedel, Germany), and 42.3 % with the Autohaler [16]. The rate of successful inhalation maneuvers in this study was 75.1 % overall, and 82.5 % in children aged 9–12 years. Although it is necessary to be cautious when comparing across studies, these results suggest that the ease of operating the Respimat SMI compares favorably with the Turbohaler and the Diskus DPI, both of which, unlike the Respimat SMI, require active inspiratory effort to overcome device resistance and achieve adequate drug delivery to the airways. The delivery of drug by the Respimat SMI is independent of inspiratory flow rate and efforts, in contrast to other devices, including DPIs such as the Turbohaler and the Diskus DPI, which require breath actuation, involving inspiratory effort and a need for a certain flow rate [2, 4, 17, 18].
In this study, only a small proportion of the errors recorded were device related (i.e., errors in coordinating dose release with inhalation, which occur with all manually operated devices, or exhalation errors caused by coughing in response to inhalation). The rate of device-related errors (11 %) is comparable to that associated with other devices [19]. The rate of inhalation maneuver success with the Respimat SMI was 73 % in children with no prior experience using inhalers, suggesting that those naïve to such devices can operate the Respimat SMI without difficulty. Children naïve to inhalers and those in the younger age group did appear to be more susceptible to the “breath-catching phenomenon” in response to inhalation; however, this response alone did not determine inhalation maneuver failure.
Children who had previously used DPIs, Autohaler, or pressurized MDIs achieved the highest percentages of successful maneuvers with the Respimat SMI, indicating that some device experience of this kind supports Respimat SMI operation. In contrast, prior experience using nebulizers or a pressurized MDI with a spacer provided no benefit in terms of ensuring correct inhalation via Respimat SMI. This may be because subjects are taking multiple breaths (tidal breathing) rather than a single deep breath or it may be influenced by the likely prior use of nebulizers and spacers in children with low levels of coordination (e.g., because of their young age).
The median estimated lung deposition recorded in the group of children aged 9–12 years was lower than in those aged 4–8 years. This is explained by higher inspiratory flow rates during inhalation maneuvers in older children, since the higher the inspiratory flow rate, the greater the deposition of drug in the oropharyngeal region rather than in the lungs [13, 20]. Only 48 % of children in the total group inhaled within the optimal flow range of <40 L/min, and in some children the inhalation flow rate reached beyond 100 L/min. In contrast to the Respimat SMI, DPIs in particular require a high inspiratory flow rate for effective drug delivery and users need to overcome a trigger threshold; children with experience using DPI were, therefore, trained to inhale as quickly and deeply as possible. In the current study, children with experience using DPIs inhaled faster than those without such background.
Although overall maneuver success rates were lowest in the subgroup of children who had previously used spacers, the median inspiratory flow rate from successful inhalations was <40 L/min, which led to a higher median estimated lung deposition than in children who had used other inhaler devices, and was similar to those without prior inhaler experience.
The interpretation of the results from this study is limited by a number of factors, among which are the number of participants and the pneumotachograph, which was added to the inhaler and made handling more difficult. Furthermore, estimated lung deposition was a calculated value and, therefore, only partially comparable with scintigraphic data, and did not take into account device deposition or losses due to re-exhaled aerosol. Pitcairn et al. [8] showed in a scintigraphic study a lung deposition of 51.6 % after an ideal inhalation maneuver. However, the loss due to device deposition and re-exhaled aerosol accounts for the loss of ≈27 % of the dose, predicting a median estimated lung deposition of 73 % [8] and supporting the plausibility of the results. In this study, a corresponding maneuver (i.e., ideal coordination and inspiratory flow 26 L/min) shows an estimated lung deposition of 83 %, thus somewhat overestimating the results from scintigraphic studies. A strength of this study is that estimated data in children were obtained, which circumvented the need for actual drug deposition scintigraphic studies.
Conclusion
These findings demonstrate that children aged 5 years and older can use the Respimat SMI and perform a successful inhalation maneuver; while children aged 4 years did not meet the success criteria. Children aged 5–8 years achieved higher estimated lung deposition values than children aged 9–12 years, possibly owing to a higher inspiratory flow rate (and, therefore, greater extrathoracic deposition) in the older group.
References
Barnes PJ. Pulmonary pharmacology. In: Brunton L, Chabner B, Knollman B, editors. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw Hill; 2010. p. 1031–66.
Chrystyn H. The Diskus: a review of its position among dry powder inhaler devices. Int J Clin Pract. 2007;61(6):1022–36.
Dolovich MB, Ahrens RC, Hess DR, et al. Device selection and outcomes of aerosol therapy: evidence-based guidelines: American College of Chest Physicians/American College of Asthma, Allergy, and Immunology. Chest. 2005;127(1):335–71.
Ari A, Fink JB. Guidelines for aerosol devices in infants, children and adults: which to choose, why and how to achieve effective aerosol therapy. Expert Rev Respir Med. 2011;5(4):561–72.
Anderson P. Use of Respimat Soft Mist inhaler in COPD patients. Int J Chron Obstruct Pulmon Dis. 2006;1(3):251–9.
Dalby RN, Eicher J, Zierenberg B. Development of Respimat((R)) Soft Mist Inhaler and its clinical utility in respiratory disorders. Med Devices (Auckl). 2011;4:145–55.
Hochrainer D, Holz H, Kreher C, Scaffidi L, Spallek M, Wachtel H. Comparison of the aerosol velocity and spray duration of Respimat Soft Mist inhaler and pressurized metered dose inhalers. J Aerosol Med. 2005;18(3):273–82.
Pitcairn G, Reader S, Pavia D, Newman S. Deposition of corticosteroid aerosol in the human lung by Respimat Soft Mist inhaler compared to deposition by metered dose inhaler or by Turbuhaler dry powder inhaler. J Aerosol Med. 2005;18(3):264–72.
von Berg A, Jeena PM, Soemantri PA, et al. Efficacy and safety of ipratropium bromide plus fenoterol inhaled via Respimat Soft Mist Inhaler versus a conventional metered dose inhaler plus spacer in children with asthma. Pediatr Pulmonol. 2004;37(3):264–72.
Brand P, Hederer B, Austen G, Dewberry H, Meyer T. Higher lung deposition with Respimat Soft Mist inhaler than HFA-MDI in COPD patients with poor technique. Int J Chron Obstruct Pulm Dis. 2008;3(4):763–70.
Kassner F, Hodder R, Bateman ED. A review of ipratropium bromide/fenoterol hydrobromide (Berodual) delivered via Respimat Soft Mist Inhaler in patients with asthma and chronic obstructive pulmonary disease. Drugs. 2004;64(15):1671–82.
Leach CL, Davidson PJ, Boudreau RJ. Improved airway targeting with the CFC-free HFA-beclomethasone metered-dose inhaler compared with CFC-beclomethasone. Eur Respir J. 1998;12(6):1346–53.
Wachtel H, Bickmann D, Langguth P. Impact of the respiratory pattern on aerosol deposition in mouth and pharynx. 11th German Aerosol Therapy Seminar. Marburg, Germany. 10-11 Nov 2006. [abstract]. Pneumologie. 2007;61:133. Abstract 14.
Krackhardt D, Stanko C, Kamin W. Use of the Respimat® Soft Mist™ Inhaler in children: an evaluation based on airflow profiles. Report to Boehinger Ingelheim. Poster presented at the 16th International Congress of the International Society for Aerosols in Medicine (ISAM), 16–20 June 2007; Tours, France.
Bickmann D, Kamin W, Sharma A, Wachtel H, Moroni-Zentgraf P, Zielen S. In vitro determination of Respimat dose delivery in children: an evaluation based on inhalation flow profiles and mouth-throat models. J Aerosol Med Pulm Drug Deliv. 2015 Jun 22 [Epub ahead of print].
Kamin W, Kreplin A. Teaching the inhalation manoeuvre to asthmatic children by means of visual feedback. Pneumologie. 2007;61(3):150–6.
Mahler DA, Waterman LA, Gifford AH. Prevalence and COPD phenotype for a suboptimal peak inspiratory flow rate against the simulated resistance of the Diskus® dry powder inhaler. J Aerosol Med Pulm Drug Deliv. 2013;26(3):174–9.
Vincken W, Dekhuijzen PR, Barnes P. The ADMIT series—issues in inhalation therapy. (4) How to choose inhaler devices for the treatment of COPD. Prim Care Respir J. 2010;19(1):10–20.
Molimard M. How to achieve good compliance and adherence with inhalation therapy. Curr Med Res Opin. 2005;21(Suppl 4):S33–7.
Brand P, Hederer B, Lowe L, Herprich C, Häussermann S, Sommerer K. Flow-dependence of lung deposition after inhalation using an HFA-aerosol or Respimat Soft Mist Inhaler in COPD patients. 11th German Aerosol Therapy Seminar. Marburg, Germany. November 10-11, 2006 [abstract]. Pneumologie. 2007;61:127. Abstract 1.
Acknowledgments
The study was partially sponsored by Boehringer Ingelheim. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis. The authors thank the children who participated in this study, and gratefully acknowledge Christine Stanko, who trained some of the children and performed flow measurements. Editorial assistance was provided by Carol A. Richter from PAREXEL, and was funded by Boehringer Ingelheim. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. Preliminary results of this study were presented in a poster at the 16th International Congress of the International Society for Aerosols in Medicine (ISAM), Tours, France, June 16–20, 2007.
Disclosures
Herbert Wachtel confirms that he has provided technical support on behalf of Boehringer Ingelheim without introducing any bias. Wolfgang Kamin received study material and financial support from Boehringer Ingelheim. Rüdiger Goessl is an employee of Boehringer Ingelheim. Sabine Kattenbeck is an employee of Boehringer Ingelheim. Paul Koker is an employee of Boehringer Ingelheim. Petra Moroni-Zentgraf is an employee of Boehringer Ingelheim. Herbert Wachtel is an employee of Boehringer Ingelheim. David Krackhardt has no disclosures to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was conducted in accordance with Good Clinical Practice and applicable regulatory requirements. This was not a “clinical trial” according to the German Drug or Medical Devices Act as no medication was administered. Institutional review board approval was obtained. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013.
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kamin, W., Krackhardt, D., Gössl, R. et al. A Handling Study to Assess the Use of the Respimat® Soft Mist™ Inhaler in Children Aged 4–12 Years. Pulm Ther 1, 53–63 (2015). https://doi.org/10.1007/s41030-015-0002-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-015-0002-y