Abstract
Disadvantaged adolescents such as those of low socioeconomic and geographically remote backgrounds experience disproportionate chronic disease burden and tend to engage in greater risk behaviors including poor diet, alcohol use, tobacco smoking, and vaping. The social, structural, and economical barriers to health that uniquely affect adolescents of low socioeconomic and geographically remote backgrounds, such as stigma, access to and affordability of services, may partially explain their disadvantage in attaining health equity. Universal eHealth interventions can provide effective prevention, however, it is unclear whether they benefit disadvantaged adolescents, including those from low socioeconomic and geographically remote contexts. This study systematically reviewed the effectiveness of eHealth interventions targeting disadvantaged adolescents in preventing poor diet, alcohol use, tobacco smoking and vaping. Of 3278 identified records, 15 publications assessing 14 interventions were included, comprising 7170 youth (aged 9–18 years, 50.1% female, 56% low-mid SES, 33% remote). Nine interventions targeted poor diet, three targeted alcohol, one targeted tobacco, and one targeted alcohol and tobacco. No interventions targeted vaping. eHealth interventions significantly increased fruit and vegetable intake and percentage energy of nutrient-rich food, decreased sugar-sweetened beverage consumption, total energy intake, nutrient-poor food percentage energy consumption, and were associated with reduced binge drinking at 1-month follow-up among intervention completers. The findings of this study highlight that eHealth interventions can be effective in targeting poor diet and alcohol use among disadvantaged adolescents. However, due to the limited number of studies meeting inclusion criteria for this study, it is critical future research focus on developing and evaluating effective eHealth interventions targeting disadvantaged adolescents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disadvantaged adolescent populations, including those from low socioeconomic and geographical remote contexts, experience exponentially greater chronic disease burden than their counterparts and report higher rates of engagement in modifiable risk behaviors such as poor diet, alcohol use, tobacco smoking and vaping (Australian Institute of Health & Welfare, 2019a). Chronic diseases detrimentally affect an individual’s health and wellbeing, and are associated with significant social and economic costs; this effect is exacerbated with multimorbidity (Australian Institute of Health & Welfare, 2020b). There is an opportunity to alleviate disadvantaged adolescents’ vulnerability to experiencing chronic disease burden across their lifetime in a cost-effective way by focusing on the prevention of key lifestyle risk behaviors prior to their establishment in adulthood (Solar & Irwin, 2010). There is growing evidence to support the use of electronic health (eHealth) interventions in delaying or preventing the onset of modifiable lifestyle risk behaviors among the general population (Newton et al., 2022; Qiu et al., 2022), however, their effect on disadvantaged adolescents has not yet been synthesized. Therefore, the purpose of this study is to systematically synthesize the literature on eHealth interventions among disadvantaged adolescents in preventing poor diet, alcohol use, tobacco smoking and vaping.
Disadvantage and Modifiable Lifestyle Risk Behaviors
Socioeconomic status refers to an individual’s or group’s social and economic position in relation to others in society (described as low, middle, and high), that affects access to resources and health outcomes (Australian Bureau of Statistics, 2011). In a country like Australia that covers 7 692 024 km2, there are large geographic differences in where people live with long distances between major cities and rural and remote areas. As remoteness increases, accessibility to services and health outcomes decrease. For instance, according to 2018 figures populations living in remote and very remote areas experience 1.4 times greater burden of disease than those living in major cities (Australian Institute of Health & Welfare, 2022).
Although low socioeconomic status and geographic remote backgrounds represent unique contexts, they share similar disadvantages to achieving health equity. It is for this reason the term ‘disadvantaged’ is used to describe low socioeconomic and geographically remote in this study. Disadvantaged adolescent populations face a multitude of social, structural, and economical barriers to health, such as stigma (Robards et al., 2018), less social support (World Health Organization, 2016), access to and affordability of services, employment prospects and educational opportunities (Australian Institute of Health & Welfare, 2019c); and these may partly explain health inequity between population groups.
Importantly, lifestyle risk behaviors, such as poor diet, alcohol use, and tobacco smoking, are modifiable (GBD, 2019 Diseases & Injuries Collaborators, 2020). Preventing the uptake or reducing engagement in these behaviors can lessen global disease, illness, and morbidity. However, engagement with these behaviors differs across socioeconomic positions and between geographical areas; generally, more disadvantaged populations are faring worse. Australian children and adolescents living in the lowest socioeconomic area compared to the highest socioeconomic area report: lower fruit intake, higher consumption of sugar-sweetened beverages (SSBs), and an increased likelihood of risky alcohol consumption and smoking (Australian Institute of Health & Welfare, 2020a). Similar trends have been reported among disadvantaged adolescents overseas (Palakshappa et al., 2020; Shackleton et al., 2019). Vaping (electronic cigarette or “e-cigarette” use), however, emerged relatively recently, and is becoming increasingly more common among adolescents across the world (Tarasenko et al., 2021), despite growing evidence of the harmful health effects (Banks et al., 2022). The UK Household Longitudinal Study reported greater e-cigarette use among socioeconomically disadvantaged youth, particularly among never-smokers (Green et al., 2020), and the 2018–2019 Kansas Communities That Care Student Survey reported a higher prevalence of current e-cigarette use among adolescents from rural areas compared to urban areas (Dai et al., 2021).
Adolescence as a Key Stage for Prevention
Prevention interventions targeted at adolescents provide a unique opportunity to prevent key lifestyle risk behaviors as they are ideally delivered prior to the onset and entrenchment of such behaviors. This is on account of adolescence marking a critical period of growth and development where patterns for current and future life behaviors start to take form, often accompanied by increased risk-taking behavior that can positively (e.g. competitive team sport) or negatively (e.g. substance use) influence health (Duell & Steinberg, 2019). The initiation of vaping, alcohol and tobacco use typically increases during adolescence (Degenhardt et al., 2016; Hammond et al., 2019), and dietary habits characteristically include greater consumption of nutrient-poor food (Murakami & Livingstone, 2016) including junk food (Australian Institute of Health & Welfare, 2018) and SSBs (Australian Institute of Health & Welfare, 2019b). These behaviors commonly cluster together (Gardner et al., 2022) and have been regarded as “consumption behaviors” (Thornton, 2022), suggesting that consuming food, alcohol, or tobacco requires active participation. Short-term consequences associated with these behaviors include obesity (Bleich & Vercammen, 2018), diminished quality of life (Hoare et al., 2019a, 2019b), and behavioral and mental health problems (Hoare et al., 2019a, 2019b). Many of these behaviors may persist into adulthood (Degenhardt et al., 2008), increasing chronic disease risk, particularly when they co-occur (Ding et al., 2015). Preventing these behaviors in adolescence is critical for safeguarding future health outcomes of disadvantaged populations, and engaging in health-promoting behaviors in adolescence shows promise in improving adolescent and adult health outcomes (Liu et al., 2012).
Viability of eHealth Interventions and Existing Systematic Reviews
Pertinent to the design of prevention interventions is consideration of the unique barriers experienced by disadvantaged adolescent populations. Electronic health (eHealth) interventions (e.g., computer-, web-, mobile-, or telephone-based) may be a viable option as they can be accessed remotely, at little cost to the end-user, and provide increased implementation fidelity and student engagement (Newton et al., 2017). As adolescents are high users of technology (Patton et al., 2016), eHealth provides an opportunity to connect with disadvantaged adolescents who may otherwise miss out on receiving interventions due to the aforementioned barriers. Several systematic reviews of eHealth interventions targeting poor diet, alcohol use, and/or tobacco smoking among adolescents have reported their effectiveness in: improving dietary behaviors (e.g. less unhealthy food and total fat and saturated fat consumption, and increased daily fruit and vegetable intake) (Kemp et al., 2021); reducing alcohol use (Hutton et al., 2020; Kazemi et al., 2021); and reducing the number of cigarettes and smoking frequency (Taylor et al., 2017). These reviews, however, focused on adolescents in the general population, and reviews on vaping are lacking. To date, no existing systematic review has focused specifically on eHealth interventions among adolescents living in geographically remote areas and/or of lower socioeconomic contexts targeting poor diet, alcohol use, tobacco smoking and vaping.
The Current Study
Due to the disproportionate chronic disease burden experienced by disadvantaged adolescents, innovative, effective and accessible prevention approaches are needed. Universal eHealth interventions among adolescents can provide effective prevention, therefore may be a practical option for preventing lifestyle risk behaviors such as poor diet, alcohol use, tobacco smoking and vaping among disadvantaged adolescents. However, the research on the effect of eHealth interventions among disadvantaged adolescents has yet to be systematically synthesized. This study aimed to address gaps in the literature by systematically reviewing the evidence on the effectiveness of eHealth interventions targeting adolescents (aged 10–19 years) from disadvantaged backgrounds in preventing poor diet, alcohol use, tobacco smoking, and vaping. It was hypothesized that eHealth interventions targeting these risk behaviors among disadvantaged adolescents would be limited in number and effect, especially those targeting vaping due to its relatively recent emergence among adolescents and the paucity of research focused on vaping.
Methods
This systematic review was prospectively registered with PROPSERO (CRD42021294119) and was written as outlined in the published review protocol (Egan et al., 2022) and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols guidelines (Moher et al., 2015).
Search Strategy and Selection Criteria
A systematic search of seven electronic databases (Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials, PROSPERO, MEDLINE [Ovid], Embase [Ovid], Scopus, and PsycInfo [Ovid]) was conducted December 19, 2022. An example search for MEDLINE [Ovid] is provided in the appendix (p 20). The search strategy was developed in consultation with a research librarian, and search terms were guided by the population, interventions, comparators, and outcomes (PICO) approach (Shamseer et al., 2015). Eligible studies were those that evaluated an eHealth intervention targeting poor diet, alcohol use, tobacco smoking, or vaping among adolescents aged 10–19 years (in line with the World Health Organization’s definition for “adolescents” (World Health Organization, 2021)) of low socioeconomic or from geographically remote backgrounds. The comparator groups included participants in a control group (e.g. no intervention) or assessed outcomes based on changes over time. Randomized controlled trials and quasi-experimental studies, with no language or publish date restrictions were included. Studies were excluded if there was no clear eHealth intervention component or if interventions were targeted at the general population without specific sub-group analysis among disadvantaged adolescents.
Data Extraction
All identified articles were imported into EndNote software (Clarivate) for removal of duplicates, and subsequently uploaded to Covidence software (Covidence) for screening. The reference lists of eligible studies were also searched to identify additional studies. Study titles and abstracts were independently reviewed by one author, and a subset (25%) of articles were double screened by the remaining study authors. Any disagreements were resolved through consultation. Data were extracted by one author using a standardized extraction form guided by the Template for Intervention Description and Replication checklist (Hoffmann et al., 2014), and reviewed by a second author.
Data Analysis
The primary outcome of interest was the prevention or reduction of alcohol (any consumption, total weekly-monthly alcohol consumption, heavy drinking, and frequency of binge drinking), tobacco (current vs non-smoker), and e-cigarette use, and improvements in dietary behaviors, including intake of fruit and vegetable, SSBs and nutrient-poor foods (junk food). Secondary outcomes included knowledge, intentions, and other health behaviors including physical activity, sleep and recreational screen time. Two authors independently assessed the risk of bias of included studies using the Cochrane Revised Risk of Bias Tool (Sterne et al., 2019). Any discrepancies between assessors were resolved through consultation. Study findings were summarized qualitatively following the UK Economic and Social Research Council guidance for narrative synthesis in systematic reviews (Popay et al., 2006).
Results
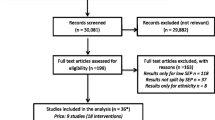
An overview of the study selection process is shown in a PRISMA flow diagram (Fig. 1). A total of 3601 articles were identified, with 15 articles (covering 14 trials) included for extraction. There was substantial inter-relater reliability present at full-text screening (Cohen’s K 0.625; 81% agreement). A summary of study characteristics is shown in Table 1.
Study Characteristics
Across the 14 trials, 7170 youth aged between 9 and 18 years took part, with an average of 50.1% female (for studies reporting sex), and 56% low-mid SES, and 33% remote. Trials predominantly included both males and females, with the exception of two trials that evaluated solely a male population (Lubans et al., 2016; Smith et al., 2014) and female population (Nollen et al., 2014). Studies were predominantly conducted in the USA (n = 8; 57%), and study designs included cluster randomized controlled trials (n = 6; 43%), randomized controlled trials (n = 4; 29%) and quasi-experimental studies (n = 4; 29%). Sample sizes ranged from 46 to 3213 adolescents, with intervention length varying between 20 min to 25-months and follow up periods ranging from one month to 25-months. Comparators were most commonly education as usual (n = 4; 29%) or waitlist control (n = 4; 29%), however, two studies (14%) did not have a control group, and instead examined between group comparisons.
Nine trials (Cremers et al., 2015; Frenn et al., 2003, 2005; Lubans et al., 2016; Martinez-Montilla et al., 2020; Nollen et al., 2014; Smith et al., 2014; Tripicchio et al., 2017; Voogt et al., 2013; Wright et al., 2013) were conducted among adolescents of low socioeconomic status, four (Chai et al., 2021; Davis et al., 2016; Gustafson et al., 2019; Hongthong & Areesantichai, 2016) were among adolescents living in geographically remote areas, and one focused on adolescents of both low socioeconomic and geographically remote backgrounds (Murry et al., 2019).
Nine trials (Chai et al., 2021; Davis et al., 2016; Frenn et al., 2003, 2005; Gustafson et al., 2019; Lubans et al., 2016; Nollen et al., 2014; Smith et al., 2014; Tripicchio et al., 2017; Wright et al., 2013) targeted diet, three (Hongthong & Areesantichai, 2016; Martinez-Montilla et al., 2020; Voogt et al., 2013) targeted alcohol, one (Cremers et al., 2015) targeted tobacco, and one (Murry et al., 2019) targeted both alcohol and tobacco. No studies targeted vaping.
Intervention Characteristics
Most interventions were either standalone eHealth (n = 11 Chai et al., 2021; Cremers et al., 2015; Davis et al., 2016; Frenn et al., 2005; Gustafson et al., 2019; Hongthong & Areesantichai, 2016; Martinez-Montilla et al., 2020; Murry et al., 2019; Nollen et al., 2014; Voogt et al., 2013; Wright et al., 2013)) or mainly eHealth (n = 1 (Frenn et al., 2003)) interventions, and primarily used computer-based methods (e.g., websites) to deliver the intervention, followed by telephone (including SMS), and telemedicine (e.g., Skype).
Twelve studies cited theoretical underpinnings for their interventions, most commonly Social Cognitive Theory (n = 3; 21%) and the I-Change Model (n = 3; 21%). Eight studies (Chai et al., 2021; Cremers et al., 2015; Davis et al., 2016; Gustafson et al., 2019; Hongthong & Areesantichai, 2016; Martinez-Montilla et al., 2020; Murry et al., 2019; Nollen et al., 2014) (57%) evaluated an intervention that was co-designed with end users and key stakeholders (including at least one of the following groups: adolescents; teachers; parents; community members; health care professionals).
Primary Outcomes
Primary outcome data relating to poor diet, alcohol use and tobacco smoking for each trial is shown in Table 1.
Dietary Intake
Of the eight trials assessing dietary outcomes, compared to a control group three eHealth interventions were significantly associated with: increased fruit and vegetable intake (Gustafson et al., 2019) at post-intervention; decreased SSB consumption at post-intervention (8-months) but not 18-month follow-up (Lubans et al., 2016; Smith et al., 2014); reduced total energy intake in a telehealth only-based intervention group, and percentage energy increase of nutrient-rich food e.g. fruit and decrease of nutrient-poor food in a telehealth plus SMS group (Chai et al., 2021).
Three trials reported non-significant between group differences on: fruit and vegetable consumption and SSB intake compared to control (Nollen et al., 2014); daily intake of calories, percent calories from fat, fruit and vegetables, SSBs, and nutrient-poor foods between a telephone-based to telemedicine-based intervention (Davis et al., 2016); and adolescents total consumption of kilocalories (kcal/wk), fat, fruits and vegetables (servings/day) compared to control (Wright et al., 2013).
Finally, two trials (Frenn et al., 2003, 2005) assessed intervention effects on percentage dietary fat, with one reporting no significant difference between intervention and control groups at post-intervention (1-year) (Frenn et al., 2003).
Alcohol and Tobacco Use
Of the three trials assessing alcohol consumption and tobacco smoking, one trial (Martinez-Montilla et al., 2020) reported a reduction in heavy episodic drinking at 4-months post-baseline among the whole study sample. Compared to participants of high family affluence, those of medium family affluence were significantly more likely to binge drink, and those of low family affluence were more likely to have consumed any alcohol (although results were not significant p = 0.6).
Two trials (Martinez-Montilla et al., 2020; Voogt et al., 2013) found no significant intervention effects on binge drinking, any or weekly alcohol consumption,—although one (Voogt et al., 2013) conducted analysis on participants that completed the intervention only and reported a significant reduction in binge drinking at 1-month follow-up compared to control –, and another (Cremers et al., 2015) found no intervention effects on smoking behavior.
Secondary Outcomes
Secondary outcomes data reported in each trial is presented in Table 1. Five trials assessed intervention effects on moderate to vigorous physical activity (MVPA) (Chai et al., 2021; Davis et al., 2016; Frenn et al., 2003, 2005; Lubans et al., 2016; Smith et al., 2014), however, only one trial reported a significant increase in MVPA (Frenn et al., 2005). Three trials assessed intervention effects on screen-time (Lubans et al., 2016; Nollen et al., 2014; Smith et al., 2014; Wright et al., 2013), with two reporting significant reductions (between -30 min/day to -2 h/day) in screen-time (Lubans et al., 2016; Smith et al., 2014; Wright et al., 2013).
One trial (Murry et al., 2019) conceptualized adolescent risk behaviors (substance use and sexual risk) as a composite risk score and found the computer-based intervention was associated with a significant decrease in risk behaviors and intentions to engage in risk behaviors (including alcohol and tobacco use) over time. Contrastingly, another trial (Cremers et al., 2015), reported no significant reduction in tobacco smoking intentions.
In the one trial (Hongthong & Areesantichai, 2016) that assessed intervention effects on alcohol knowledge, it reported significantly increased alcohol knowledge scores in the intervention group compared to control group at 6-month follow-up after adjusting for peer drinking and GPA.
Finally, seven trials (Chai et al., 2021; Davis et al., 2016; Gustafson et al., 2019; Lubans et al., 2016; Nollen et al., 2014; Smith et al., 2014; Tripicchio et al., 2017; Wright et al., 2013) assessed intervention effects on BMI, however, only one trial (Tripicchio et al., 2017) was associated with reduced BMI-z scores at post-intervention (12-weeks) among a app and telemedicine-based intervention group. However, between group differences were not significant.
Factors Associated with Intervention Effectiveness
For studies with significant intervention effects on primary outcomes (Chai et al., 2021; Gustafson et al., 2019; Lubans et al., 2016; Martinez-Montilla et al., 2020; Smith et al., 2014; Voogt et al., 2013), intervention length ranged from one 20-min session to 8-months, included personalized feedback to participants, and Social Cognitive Theory was most common when targeting poor diet, and I-Change Model was most common when targeting alcohol use.
Generally, studies reporting non-significant intervention effects on primary outcomes (Cremers et al., 2015; Davis et al., 2016; Frenn et al., 2003; Nollen et al., 2014; Wright et al., 2013) were either delivered via telephone or telemedicine, or did not provide personalized feedback, with intervention length ranging from 12-weeks to 1-year. There were no clear differences in intervention effects on primary outcomes when comparing programs that were co-designed (Chai et al., 2021; Cremers et al., 2015; Davis et al., 2016; Gustafson et al., 2019; Martinez-Montilla et al., 2020; Nollen et al., 2014) versus those that were not (Frenn et al., 2003, 2005; Lubans et al., 2016; Smith et al., 2014; Voogt et al., 2013; Wright et al., 2013).
Intervention effects on primary outcomes for trials specifically designed for disadvantaged adolescents (Chai et al., 2021; Davis et al., 2016; Frenn et al., 2003; Gustafson et al., 2019; Lubans et al., 2016; Nollen et al., 2014; Smith et al., 2014; Voogt et al., 2013) versus those that conducted sub-group analyses (Cremers et al., 2015; Frenn et al., 2005; Martinez-Montilla et al., 2020; Wright et al., 2013) were similar, with four (Chai et al., 2021; Gustafson et al., 2019; Lubans et al., 2016; Smith et al., 2014; Voogt et al., 2013) of ten trials, and one (Martinez-Montilla et al., 2020) of four, reporting significant intervention effects, respectively.
Three trials reported participants’ participation in the intervention was associated with higher reductions in dietary fat and increased physical activity (Frenn et al., 2005), decreased BMI-z scores (Tripicchio et al., 2017) and SSB consumption (Nollen et al., 2014). Of the six trials (Davis et al., 2016; Lubans et al., 2016; Martinez-Montilla et al., 2020; Nollen et al., 2014; Tripicchio et al., 2017; Wright et al., 2013) that assessed participant satisfaction with the intervention, generally interventions were rated highly. Participant retention did not appear meaningfully different between interventions reporting significant results versus those that did not, and only two studies (Cremers et al., 2015; Martinez-Montilla et al., 2020) reported participant retention below 50% at post-intervention follow-up.
Risk of Bias
A summary of the overall risk of bias assessment for included papers is shown in Fig. 2. Of the 15 included articles, seven studies were rated as having high risk of overall bias for at least one outcome (Chai et al., 2021; Cremers et al., 2015; Frenn et al., 2003; Martinez-Montilla et al., 2020; Nollen et al., 2014; Smith et al., 2014; Tripicchio et al., 2017), and several studies were rated as having unclear overall risk of bias for at least one outcome (Chai et al., 2021; Davis et al., 2016; Frenn et al., 2005; Gustafson et al., 2019; Hongthong & Areesantichai, 2016; Lubans et al., 2016; Murry et al., 2019; Smith et al., 2014; Voogt et al., 2013; Wright et al., 2013). These ratings were predominantly driven by missing outcome data (i.e. not examining differences between participants lost to follow-up and those that completed follow-up assessments) and deviations from intended interventions (i.e. blinding often was not possible and in some studies intention-to-treat analysis was not employed). Furthermore, most studies failed to reference a published protocol, and were therefore rated has having an unclear risk of selective reporting of the result.
Discussion
Chronic disease burden disproportionately affects disadvantaged adolescents including those from low socioeconomic and geographically remote backgrounds. A critical and cost-effective approach towards reducing the risk of experiencing chronic disease burden across the lifetime, is preventing lifestyle risk behaviors such as poor diet, alcohol use, tobacco smoking and vaping in adolescence, that is ideally prior to their onset and entrenchment. There is considerable evidence to support the efficacy of universal eHealth interventions among adolescents in delaying or preventing modifiable risk behaviors. This is the first study, however, to systematically review the effectiveness of eHealth interventions targeting adolescents living in geographically remote and/or of lower socioeconomic contexts in preventing poor diet, alcohol use, tobacco smoking and vaping.
As adolescence is a key formative period of development that can have lasting effects on future health, it is critical prevention interventions are delivered prior to the initiation and uptake of lifestyle risk behaviors that may lead to subsequent development of chronic disease in adulthood. Interestingly, this study found that although the age range of adolescents from disadvantaged backgrounds in included studies varied from 9 to 17 years, generally adolescents were older (average 14 years) in studies reporting significant intervention effects related to poor diet, alcohol and tobacco use (Chai et al., 2021; Gustafson et al., 2019; Hongthong & Areesantichai, 2016; Lubans et al., 2016; Martinez-Montilla et al., 2020; Murry et al., 2019; Smith et al., 2014; Voogt et al., 2013), compared to those that were not (average 11 years) (Cremers et al., 2015; Davis et al., 2016; Frenn et al., 2003, 2005; Nollen et al., 2014; Tripicchio et al., 2017; Wright et al., 2013). It appears that older adolescents are more receptive to eHealth interventions, which may be reflective of developing greater autonomy over their life (Spear & Kulbok, 2004). However, it is important that future longitudinal studies assess the long-term effects of eHealth interventions across adolescence.
Another key point to consider with regard to interventions aimed at preventing lifestyle risk behaviors among disadvantaged adolescents, is delivering interventions that pay attention to contextual factors including socioeconomic status and geographic location as they may potentially influence the efficacy of programs. In this study, the distribution of studies was largely skewed towards focusing on adolescents of low socioeconomic backgrounds, and were predominantly aimed at preventing poor diet, followed by alcohol use and tobacco smoking. Relatively fewer studies targeted adolescents living in geographically remote areas. Only one study targeted adolescents of both low socioeconomic and geographically remote contexts in preventing alcohol use and tobacco smoking. No studies targeted vaping. Of the 15 articles that were analyzed in this study, five (Chai et al., 2021; Gustafson et al., 2019; Lubans et al., 2016; Martinez-Montilla et al., 2020; Smith et al., 2014; Voogt et al., 2013) reported significant intervention effects relating to improved dietary behaviors, and reduced alcohol use and tobacco smoking.
Of the six studies targeting adolescents of low socioeconomic backgrounds in preventing poor diet, only one was associated with decreased SSB consumption immediately post-intervention, however, intervention effects were short-lived with non-significant results at longer-term follow-up (Lubans et al., 2016; Smith et al., 2014). This finding is consistent with a recent review (Champion et al., 2019) of eHealth multiple health behavior change interventions. Although a smaller number of studies targeted adolescents living in geographically remote areas, two of the three were associated with improved dietary outcomes at post-intervention. Specifically, they reported significant intervention effects on increasing fruit and vegetable intake and percentage energy increase of nutrient-rich food, and decreasing total energy intake, energy-dense, nutrient-poor food percentage energy consumption (Chai et al., 2021; Gustafson et al., 2019). Considering these three studies together, they were most commonly guided by Social Cognitive Theory, were specifically designed for disadvantaged adolescents, and included personalized feedback to participants.
For studies not associated with improved dietary outcomes, it is possible that the lack of personalized feedback to participants hindered significant intervention effects in two studies (Davis et al., 2016; Nollen et al., 2014) or the study length and/or intervention dose was not sufficient to achieve larger effect sizes. For instance, in one study (Frenn et al., 2003) four 50-min internet-based lessons and one 50-min peer-led healthy snack session were delivered over one year. As the only assessment was conducted at post-intervention (1-year), there is the potential that intermediary intervention effects may have been missed, or lessons were too infrequent for participants to consolidate and apply learning. Given two of these studies found participation was associated with decreased percentage dietary fat (Frenn et al., 2003) and a larger reduction in SSB consumption (Nollen et al., 2014), this suggests additional modules were required. This is in line with a previous review of eHealth interventions targeting diet and physical activity, reporting greater intervention dose and utilization tended to improve health behavior change (Norman et al., 2007). Together these study components may have enhanced the effectiveness of the interventions. The overall risk of bias ratings for studies targeting poor diet included four studies as having high risk of overall bias on at least one outcome (Chai et al., 2021; Frenn et al., 2003; Nollen et al., 2014; Smith et al., 2014), and seven studies as having unclear overall bias on at least one outcome (Chai et al., 2021; Davis et al., 2016; Frenn et al., 2005; Gustafson et al., 2019; Lubans et al., 2016; Smith et al., 2014; Wright et al., 2013). Key domains contributing to these ratings included high risk of bias on deviations from intended interventions (due to blinding of intervention groups often not being possible) and missing outcome data, and unclear risk of bias for selective reporting of result.
Turning to studies that targeted alcohol use only, only two were included in this study and both were among adolescents of low socioeconomic backgrounds (Martinez-Montilla et al., 2020; Voogt et al., 2013). The first (Martinez-Montilla et al., 2020) found adolescents of lower family affluence were more likely to report consumption of any alcohol (although not significant p = 0.6), and a significant association between family affluence and binge drinking at 4-months post-baseline among the whole study sample. The other (Voogt et al., 2013) reported significant intervention effects on binge drinking at 1-month follow-up among completers only. Although both studies were guided by the I-Change Model and included personalized messaging or feedback to participants, they differed in intervention dose and specific tailoring to disadvantaged adolescents. The first consisted of six one-hour sessions and conducted a sub-group analysis by family affluence. The second included one twenty-minute session and was specifically tailored to adolescents of low socioeconomic backgrounds. Interestingly, other universal studies have only found positive outcomes relating to the frequency of binge drinking at longer-term follow-up timepoints (i.e. 6- to 12-months, rather than immediately post-intervention) (Newton et al., 2010; Vogl et al., 2009) suggesting specifically tailored programs may yield more immediate enhanced program efficacy. The overall risk of bias was high for one (Martinez-Montilla et al., 2020) of these studies mainly due to missing outcome data (i.e. no sensitivity analysis) and measurement of the outcome (i.e. self-report), and unclear for the other (Voogt et al., 2013) largely due to measurement of the outcome (i.e. self-report). As no studies targeted adolescents living in geographically remote backgrounds, these findings underscore a crucial need for future research, particularly as consumption of alcohol at risky levels tends to be higher among adolescents living in geographically remote areas (Marqués-Sánchez et al., 2020).
Considering interventions targeting tobacco use, none were targeted at adolescents living in geographically remote areas. This is concerning given tobacco smoking is generally higher among adolescents living in geographically remote areas than their counterparts (Warren et al., 2017). Unlike the abovementioned interventions targeting alcohol use reporting significant intervention effects that were also underpinned by the I-Change Model, the one study (Cremers et al., 2015) that targeted tobacco use only was not associated with a reduction of smoking behavior or intentions. Additionally, participant retention was less than 50% at post-intervention follow-up. This study (Cremers et al., 2015) was rated as having high overall risk of bias predominantly due to missing outcome data (i.e. significant differences in participants lost to follow-up). In view of these findings, consideration of alternative theories for tobacco use prevention interventions is warranted. For instance, eHealth interventions grounded in Social Cognitive Theory show promise in reducing tobacco smoking among adolescents with higher retention rates (Champion et al., 2013; Skov-Ettrup et al., 2014).
Concerningly, no studies targeted vaping. Although the proportion of adolescents initiating tobacco use is generally declining, the same cannot be said for vaping, and suggests the motivators for tobacco smoking and vaping are dissimilar among adolescents (Dutra & Glantz, 2014; Wills et al., 2016). Effective theories for interventions targeting tobacco use may not translate to those targeting vaping. Indeed, findings from a recent review recommended the delivery of prevention strategies targeting vaping be set-apart from tobacco use and underpinned by behavior change theories (Liu et al., 2020). Nevertheless, as no study has specifically targeted vaping among disadvantaged adolescents, future research is needed to examine the mechanisms of change in these behaviors.
Despite relatively few studies reporting significant intervention effects on primary outcomes, this review found positive effects on secondary outcomes in six studies including increased alcohol knowledge (Hongthong & Areesantichai, 2016) and MVPA (Frenn et al., 2005), decreased screen-time (Lubans et al., 2016; Smith et al., 2014; Wright et al., 2013), BMI-z scores (Tripicchio et al., 2017), and engagement and intentions to engage in risk behaviors (including alcohol and tobacco use) (Murry et al., 2019). These behaviors are important protective factors for chronic disease risk (Ezzati & Riboli, 2013), thus make a substantial contribution to supporting disadvantaged adolescents achieve improved future health outcomes. Moreover, several factors associated with intervention effectiveness (e.g. most effective theories for targeting specific health behaviors, delivery method and frequency, inclusion of personalized feedback) were identified in this review. However, it is worth highlighting that although effectiveness in intervention outcomes appeared similar between studies incorporating co-design versus those that did not, previous research has found interventions that have not been tailored to disadvantaged populations are associated with poor engagement and impact, and may contribute to greater health inequalities (Coupe et al., 2018). Co-design facilitates incorporation of the intended audience’s experiences and perspectives into an intervention, and informs the type of content, delivery method, and key components to ensure its accessibility (Holly et al., 2022; World Health Organization, 2020). The importance of incorporating co-design into future interventions should be considered to adequately address the unique barriers disadvantaged adolescents experience and deliver effective and appropriate interventions.
The results indicate the need for future research on effective eHealth interventions among disadvantaged adolescents due to the paucity of studies identified and intervention effects on primary outcomes limited to those targeting poor diet and alcohol use only.
There are several strengths to this study. First, this study has provided a more up-to-date review of the literature on eHealth interventions, which is a rapidly developing area of research. For instance, compared to the Champion et al., (2019) systematic review that looked at eHealth interventions targeting poor diet, alcohol use and tobacco smoking, this systematic review differed in that it: utilized a targeted search to capture adolescents living in geographically remote and/or lower socioeconomic areas rather than focusing on the general population; included vaping as one of the target behaviors which is not included in the Champion et al., (2019) review; and includes research published up until 2022, with no date limits (Champion et al., 2019 included studies published from 2000 to 2017). Second, a team of experts in eHealth prevention interventions for young people contributed to this study by helping review, minimize bias and strengthening the analysis of findings. Third, a thorough, reproducible, and robust search strategy was employed to identify relevant studies. Fourth, this review provides critical information and analysis of important components of effective interventions, which has implications for the design and delivery of future eHealth interventions on this topic.
However, consideration of several limitations in this review is warranted. First, this study did not conduct a systematic search of grey literature, which may have limited the diversity of relevant research studies included in this study as negative results are less likely to be published in peer-reviewed journals. However, grey literature may be prone to high risk of bias (e.g., conflict of interest when the same researcher conducts and evaluates a study) and is not restricted to the same reporting standards of peer-reviewed literature thus may omit important publication information (e.g. publication date, contributors). Second, any interventions framed as treatment rather than prevention were not eligible. As disadvantaged youth are ‘higher risk’, interventions aimed at helping adolescents who were already experiencing unhealthy behaviors (e.g. alcohol use disorder) and insight into alternative methods to reach disadvantaged adolescents may not have been identified in this study’s analysis. Third, the overall risk of bias of included studies was unclear largely owing to authors failing to reference a published protocol, employing self-report as measurement for the outcome, missing outcome data for all participants, and deviations from the intended interventions. Fourth, despite the comprehensive search strategy, no studies targeting vaping met inclusion criteria. However, this is not unexpected considering vaping is a relatively newer behavior and the limited eHealth trials targeting vaping in the general population. Nevertheless, the potential of vaping exacerbating public health impact among disadvantaged adolescents, posits this is an important area for future research.
Conclusion
To address the disproportionately higher risk of chronic disease burden among disadvantaged adolescents including those of low socioeconomic or geographically remote backgrounds, prevention of lifestyle risk behaviors such as poor diet, alcohol use, tobacco smoking and vaping is critical. Despite evidence supporting the effectiveness of universal eHealth interventions in targeting these behaviors, there are gaps in the literature on whether eHealth interventions adequately serve disadvantaged adolescents. This is the first study to systematically examine and synthesize evidence on eHealth interventions targeting adolescents (aged 10–19 years) from disadvantaged backgrounds in preventing poor diet, alcohol use, tobacco smoking, and vaping. This study revealed that although eHealth interventions can be effective in targeting poor diet and alcohol use among disadvantaged adolescents, limited research in this area has been conducted with only 15 articles assessing 14 interventions included in this study’s analysis. Ultimately, this represents a missed opportunity to meaningfully improve chronic disease risk profiles of disadvantaged adolescents, especially considering the growing evidence for the effectiveness of universal eHealth interventions that may delay or prevent the onset of lifestyle risk behaviors. Challenges remain in developing, delivering, and disseminating findings on effective evidence-based programs for the prevention of chronic diseases among disadvantage adolescents. More research on developing and evaluating effective eHealth interventions specific to adolescents from lower socioeconomic and geographically remote contexts is needed.
References
Australian Bureau of Statistics. (2011). Measures of Socioeconomic Status, (Catalogue no. 1244.0.55.001). Canberra: ABS; Retrieved October 11, 2021, from https://www.ausstats.abs.gov.au/ausstats/subscriber.nsf/0/367D3800605DB064CA2578B60013445C/$File/1244055001_2011.pdf
Australian Institute of Health and Welfare. (2018). Nutrition across the life stages. Cat. no. PHE 227. Canberra: AIHW Retrieved October 11, 2021, from https://www.aihw.gov.au/getmedia/fc5ad42e-08f5-4f9a-9ca4-723cacaa510d/aihw-phe-227.pdf.aspx?inline=true
Australian Institute of Health and Welfare. (2019a). Australian Burden of Disease Study: Impact and causes of illness and death in Australia 2015. Australian Burden of Disease series no. 19. Cat. no. BOD 22. Canberra: AIHW Retrieved October 11, 2021, from https://www.aihw.gov.au/getmedia/c076f42f-61ea-4348-9c0a-d996353e838f/aihw-bod-22.pdf.aspx?inline=true
Australian Institute of Health and Welfare. (2019b). Poor diet. Cat. no: PHE 249. Canberra: AIHW Retrieved October 11, 2021, from https://www.aihw.gov.au/getmedia/f30d2eb2-b6e7-43cc-aba4-74802ad78f6a/Poor-diet.pdf.aspx?inline=true
Australian Institute of Health and Welfare. (2019c). Rural & remote health. Cat. no. PHE 255. Canberra: AIHW Retrieved April 01, 2022, from https://www.aihw.gov.au/getmedia/838d92d0-6d34-4821-b5da-39e4a47a3d80/Rural-remote-health.pdf.aspx?inline=true
Australian Institute of Health and Welfare. (2020a). Australia's children. Cat. no. CWS 69. Canberra: AIHW Retrieved October 11, 2021, from https://www.aihw.gov.au/getmedia/6af928d6-692e-4449-b915-cf2ca946982f/aihw-cws-69-print-report.pdf.aspx?inline=true
Australian Institute of Health and Welfare. (2020b). Australia’s health snapshots 2020b. Canberra: AIHW Retrieved October 11, 2021, from https://www.aihw.gov.au/reports-data/australias-health/australias-health-snapshots
Australian Institute of Health and Welfare. (2022). Rural and remote health. Canberra: AIHW Retrieved March 13, 2023, from https://www.aihw.gov.au/reports/rural-remote-australians/rural-and-remote-health
Banks, E., Yazidjoglou, A., Brown, S., Nguyen, M., Melonie Martin, Beckwith, K., Daluwatta, A., Campbell, S., & Joshy, G. (2022). Electronic cigarettes and health outcomes: systematic review of global evidence. Retrieved August 26, 2022, from https://openresearch-repository.anu.edu.au/bitstream/1885/262914/1/Electronic%20cigarettes%20health%20outcomes%20review_2022_WCAG.pdf
Bleich, S. N., & Vercammen, K. A. (2018). The negative impact of sugar-sweetened beverages on children’s health: An update of the literature. BMC Obesity, 5, 6. https://doi.org/10.1186/s40608-017-0178-9
Chai, L. K., Collins, C. E., May, C., Ashman, A., Holder, C., Brown, L. J., & Burrows, T. L. (2021). Feasibility and efficacy of a web-based family telehealth nutrition intervention to improve child weight status and dietary intake: A pilot randomised controlled trial. Journal of Telemedicine and Telecare, 27(3), 146–158. https://doi.org/10.1177/1357633X19865855
Champion, K. E., Newton, N. C., Barrett, E. L., & Teesson, M. (2013). A systematic review of school-based alcohol and other drug prevention programs facilitated by computers or the Internet. Drug and Alcohol Review, 32(2), 115–123. https://doi.org/10.1111/j.1465-3362.2012.00517.x
Champion, K. E., Parmenter, B., McGowan, C., Spring, B., Wafford, Q. E., Gardner, L. A., Thornton, L., McBride, N., Barrett, E. L., Teesson, M., & Newton, N. C. (2019). Effectiveness of school-based eHealth interventions to prevent multiple lifestyle risk behaviours among adolescents: A systematic review and meta-analysis. The Lancet Digital Health, 1(5), e206–e221. https://doi.org/10.1016/S2589-7500(19)30088-3
Coupe, N., Cotterill, S., & Peters, S. (2018). Tailoring lifestyle interventions to low socio-economic populations: A qualitative study. BMC Public Health, 18(1), 967. https://doi.org/10.1186/s12889-018-5877-8
Cremers, H.-P., Mercken, L., Candel, M., de Vries, H., & Oenema, A. (2015). A Web-based, computer-tailored smoking prevention program to prevent children from starting to smoke after transferring to secondary school: Randomized controlled trial. Journal of Medical Internet Research, 17(3), e59. https://doi.org/10.2196/jmir.3794
Dai, H., Chaney, L., Ellerbeck, E., Friggeri, R., White, N., & Catley, D. (2021). Rural-urban differences in changes and effects of tobacco 21 in youth e-cigarette use. Pediatrics, 147(5), e2020020651. https://doi.org/10.1542/peds.2020-020651
Davis, A. M., Sampilo, M., Gallagher, K. S., Dean, K., Saroja, M. B., Yu, Q., He, J., & Sporn, N. (2016). Treating rural paediatric obesity through telemedicine vs. telephone: Outcomes from a cluster randomized controlled trial. Journal of Telemedicine and Telecare, 22(2), 86–95. https://doi.org/10.1177/1357633X15586642
Degenhardt, L., Chiu, W. T., Sampson, N., Kessler, R. C., Anthony, J. C., Angermeyer, M., Bruffaerts, R., de Girolamo, G., Gureje, O., Huang, Y., Karam, A., Kostyuchenko, S., Lepine, J. P., Mora, M. E., Neumark, Y., Ormel, J. H., Pinto-Meza, A., Posada-Villa, J., Stein, D. J., et al. (2008). Toward a global view of alcohol, tobacco, cannabis, and cocaine use: Findings from the WHO World Mental Health Surveys. PLOS Medicine, 5(7), e141. https://doi.org/10.1371/journal.pmed.0050141
Degenhardt, L., Stockings, E., Patton, G., Hall, W. D., & Lynskey, M. (2016). The increasing global health priority of substance use in young people. Lancet Psychiatry, 3(3), 251–264. https://doi.org/10.1016/S2215-0366(15)00508-8
Ding, D., Rogers, K., van der Ploeg, H., Stamatakis, E., & Bauman, A. E. (2015). Traditional and emerging lifestyle risk behaviors and all-cause mortality in middle-aged and older adults: Evidence from a large population-based australian cohort. PLOS Medicine, 12(12), e1001917. https://doi.org/10.1371/journal.pmed.1001917
Duell, N., & Steinberg, L. (2019). Positive risk taking in adolescence. Child Development Perspectives, 13(1), 48–52. https://doi.org/10.1111/cdep.12310
Dutra, L. M., & Glantz, S. A. (2014). High international electronic cigarette use among never smoker adolescents. Journal of Adolescent Health, 55(5), 595–597. https://doi.org/10.1016/j.jadohealth.2014.08.010
Egan, L., Gardner, L. A., Newton, N., & Champion, K. (2022). eHealth interventions targeting poor diet, alcohol use, tobacco smoking, and vaping among disadvantaged youth: protocol for a systematic review. JMIR Research Protocols, 11(5), e35408. https://doi.org/10.2196/35408
Ezzati, M., & Riboli, E. (2013). Behavioral and dietary risk factors for noncommunicable diseases. The New England Journal of Medicine, 369(10), 954–964. https://doi.org/10.1056/NEJMra1203528
Frenn, M., Malin, S., Bansal, N., Delgado, M., Greer, Y., Havice, M., Ho, M., & Schweizer, H. (2003). Addressing health disparities in middle school students’ nutrition and exercise. Journal of Community Health Nursing, 20(1), 1–14. https://doi.org/10.1207/S15327655JCHN2001_01
Frenn, M., Malin, S., Brown, R. L., Greer, Y., Fox, J., Greer, J., & Smyczek, S. (2005). Changing the tide: An Internet/video exercise and low-fat diet intervention with middle-school students. Applied Nursing Research, 18(1), 13–21. https://doi.org/10.1016/j.apnr.2004.04.003
Gardner, L. A., Champion, K. E., Chapman, C., Newton, N. C., Slade, T., Smout, S., Teesson, M., & Sunderland, M. (2022). Multiple lifestyle risk behaviours and hierarchical dimensions of psychopathology in 6640 Australian adolescents. Australian and New Zealand Journal of Psychiatry. https://doi.org/10.1177/00048674221080406
GBD 2019 Diseases and Injuries Collaborators. (2020). Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet, 396(10258), 1204–1222. https://doi.org/10.1016/S0140-6736(20)30925-9
Green, M. J., Gray, L., Sweeting, H., & Benzeval, M. (2020). Socioeconomic patterning of vaping by smoking status among UK adults and youth. BMC Public Health, 20(1), 183. https://doi.org/10.1186/s12889-020-8270-3
Gustafson, A., Pitts, S. B. J., McQuerry, K., Babtunde, O., & Mullins, J. (2019). A mentor-led text-messaging intervention increases intake of fruits and vegetables and goal setting for healthier dietary consumption among rural adolescents in Kentucky and North Carolina, 2017. Nutrients, 11(3), 593. https://doi.org/10.3390/nu11030593
Hammond, D., Reid, J. L., Rynard, V. L., Fong, G. T., Cummings, K. M., McNeill, A., Hitchman, S., Thrasher, J. F., Goniewicz, M. L., Bansal-Travers, M., O'Connor, R., Levy, D., Borland, R., & White, C. M. (2019). Prevalence of vaping and smoking among adolescents in Canada, England, and the United States: repeat national cross sectional surveys. BMJ, 365, l2219. https://doi.org/10.1136/bmj.l2219
Hoare, E., Crooks, N., Hayward, J., Allender, S., & Strugnell, C. (2019a). Associations between combined overweight and obesity, lifestyle behavioural risk and quality of life among Australian regional school children: Baseline findings of the Goulburn Valley health behaviours monitoring study. Health and Quality of Life Outcomes, 17(1), 16. https://doi.org/10.1186/s12955-019-1086-0
Hoare, E., Marx, W., Firth, J., McLeod, S., Jacka, F., Chrousos, G. P., Manios, Y., & Moschonis, G. (2019b). Lifestyle behavioural risk factors and emotional functioning among schoolchildren: The Healthy Growth Study. European Psychiatry, 61, 79–84. https://doi.org/10.1016/j.eurpsy.2019.07.002
Hoffmann, T. C., Glasziou, P. P., Boutron, I., Milne, R., Perera, R., Moher, D., Altman, D. G., Barbour, V., Macdonald, H., Johnston, M., Lamb, S. E., Dixon-Woods, M., McCulloch, P., Wyatt, J. C., Chan, A.-W., & Michie, S. (2014). Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ, 348, g1687. https://doi.org/10.1136/bmj.g1687
Holly, L., Smith, R. D., Ndili, N., Franz, C., & Stevens, E. A. G. (2022). A review of digital health strategies in 10 countries with young populations: Do they serve the health and wellbeing of children and youth in a digital age? Frontiers in Digital Health, 4, 817810. https://doi.org/10.3389/fdgth.2022.817810
Hongthong, D., & Areesantichai, C. (2016). The effect of the PALMSS alcohol prevention program among high school students in a rural area of Thailand. Journal of Substance Use, 21(5), 460–465. https://doi.org/10.3109/14659891.2015.1063716
Hutton, A., Prichard, I., Whitehead, D., Thomas, S., Rubin, M., Sloand, E., Powell, T. W., Frisch, K., Newman, P., & Goodwin Veenema, T. (2020). mHealth interventions to reduce alcohol use in young people: a systematic review of the literature. Comprehensive Child and Adolescent Nursing, 43(3), 171–202. https://doi.org/10.1080/24694193.2019.1616008
Kazemi, D. M., Li, S., Levine, M. J., Auten, B., & Granson, M. (2021). Systematic review of smartphone apps as a mHealth intervention to address substance abuse in adolescents and adults. Journal of Addictions Nursing, 32(3), 180–187. https://doi.org/10.1097/JAN.0000000000000416
Kemp, B. J., Thompson, D. R., Watson, C. J., McGuigan, K., Woodside, J. V., & Ski, C. F. (2021). Effectiveness of family-based eHealth interventions in cardiovascular disease risk reduction: A systematic review. Preventive Medicine, 149, 106608. https://doi.org/10.1016/j.ypmed.2021.106608
Liu, J., Gaiha, S. M., & Halpern-Felsher, B. (2020). A breath of knowledge: Overview of current adolescent e-cigarette prevention and cessation programs. Current Addiction Reports, 7(4), 520–532. https://doi.org/10.1007/s40429-020-00345-5
Liu, K., Daviglus, M. L., Loria, C. M., Colangelo, L. A., Spring, B., Moller, A. C., & Lloyd-Jones, D. M. (2012). Healthy lifestyle through young adulthood and the presence of low cardiovascular disease risk profile in middle age: The Coronary Artery Risk Development in (Young) Adults (CARDIA) study. Circulation, 125(8), 996–1004. https://doi.org/10.1161/CIRCULATIONAHA.111.060681
Lubans, D. R., Smith, J. J., Plotnikoff, R. C., Dally, K. A., Okely, A. D., Salmon, J., & Morgan, P. J. (2016). Assessing the sustained impact of a school-based obesity prevention program for adolescent boys: The ATLAS cluster randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity, 13(1), 1–12. https://doi.org/10.1186/s12966-016-0420-8
Marqués-Sánchez, P., Quiroga Sánchez, E., Liébana-Presa, C., Fernández-Martínez, E., García-Rodríguez, I., Benítez- Andrades, J.A. The consumption of alcohol by adolescent schoolchildren: Differences in the triadic relationship pattern between rural and urban environments. PLoS ONE. 2020;15(11):e0241135. https://doi.org/10.1371/journal.pone.0241135
Martinez-Montilla, J. M., Mercken, L., de Vries, H., Candel, M., Lima-Rodríguez, J. S., & Lima-Serrano, M. (2020). A web-based, computer-tailored intervention to reduce alcohol consumption and binge drinking among spanish adolescents: Cluster randomized controlled trial. Journal of Medical Internet Research, 22(1), e15438. https://doi.org/10.2196/15438
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P., Stewart, L. A., & Group, P.-P. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4(1), 1. https://doi.org/10.1186/2046-4053-4-1
Murakami, K., & Livingstone, M. B. (2016). Decreasing the number of small eating occasions (<15 % of total energy intake) regardless of the time of day may be important to improve diet quality but not adiposity: A cross-sectional study in British children and adolescents. British Journal of Nutrition, 115(2), 332–341. https://doi.org/10.1017/S0007114515004420
Murry, V. M., Berkel, C., Inniss-Thompson, M. N., & Debreaux, M. L. (2019). Pathways for African American success: Results of three-arm randomized trial to test the effects of technology-based delivery for rural African American families. Journal of Pediatric Psychology, 44(3), 375–387. https://doi.org/10.1093/jpepsy/jsz001
Newton, N. C., Champion, K. E., Slade, T., Chapman, C., Stapinski, L., Koning, I., Tonks, Z., & Teesson, M. (2017). A systematic review of combined student- and parent-based programs to prevent alcohol and other drug use among adolescents. Drug and Alcohol Review, 36(3), 337–351. https://doi.org/10.1111/dar.12497
Newton, N. C., Stapinski, L. A., Slade, T., Sunderland, M., Barrett, E. L., Champion, K. E., Chapman, C., Smout, A., Lawler, S. M., Mather, M., Debenham, J., Castellanos-Ryan, N., Conrod, P. J., & Teesson, M. (2022). The 7-year effectiveness of school-based alcohol use prevention from adolescence to early adulthood: A randomized controlled trial of universal, selective, and combined interventions. Journal of the American Academy of Child and Adolescent Psychiatry, 61(4), 520–532. https://doi.org/10.1016/j.jaac.2021.10.023
Newton, N. C., Teesson, M., Vogl, L. E., & Andrews, G. (2010). Internet-based prevention for alcohol and cannabis use: Final results of the Climate Schools course. Addiction, 105(4), 749–759. https://doi.org/10.1111/j.1360-0443.2009.02853.x
Nollen, N. L., Mayo, M. S., Carlson, S. E., Rapoff, M. A., Goggin, K. J., & Ellerbeck, E. F. (2014). Mobile technology for obesity prevention: A randomized pilot study in racial- and ethnic-minority girls. American Journal of Preventive Medicine, 46(4), 404–408. https://doi.org/10.1016/j.amepre.2013.12.011
Norman, G. J., Zabinski, M. F., Adams, M. A., Rosenberg, D. E., Yaroch, A. L., & Atienza, A. A. (2007). A review of eHealth interventions for physical activity and dietary behavior change. American Journal of Preventive Medicine, 33(4), 336–345. https://doi.org/10.1016/j.amepre.2007.05.007
Palakshappa, D., Lenoir, K., Brown, C. L., Skelton, J. A., Block, J. P., Taveras, E. M., & Lewis, K. H. (2020). Identifying geographic differences in children's sugar-sweetened beverage and 100% fruit juice intake using health system data. Pediatric Obesity, 15(11), e12663. https://doi.org/10.1111/ijpo.12663
Patton, G. C., Sawyer, S. M., Santelli, J. S., Ross, D. A., Afifi, R., Allen, N. B., Arora, M., Azzopardi, P., Baldwin, W., Bonell, C., Kakuma, R., Kennedy, E., Mahon, J., McGovern, T., Mokdad, A. H., Patel, V., Petroni, S., Reavley, N., Taiwo, K., et al. (2016). Our future: a Lancet commission on adolescent health and wellbeing. The Lancet, 387(10036), 2423–2478. https://doi.org/10.1016/S0140-6736(16)00579-1
Popay, J., Roberts, H., Sowden, A., Petticrew, M., Arai, L., Rodgers, M., Britten, N., Roen, K., & Duffy, S. (2006). Guidance on the Conduct of Narrative Synthesis in Systematic Reviews: A Product from the ESRC Methods Programme. Retrieved February 09, 2022, from https://www.academia.edu/download/39246301/02e7e5231e8f3a6183000000.pdf
Qiu, L.-T., Sun, G.-X., Li, L., Zhang, J.-D., Wang, D., & Fan, B.-Y. (2022). Effectiveness of multiple eHealth-delivered lifestyle strategies for preventing or intervening overweight/obesity among children and adolescents: A systematic review and meta-analysis. Frontiers in Endocrinology, 13, 999702. https://doi.org/10.3389/fendo.2022.999702
Robards, F., Kang, M., Usherwood, T., & Sanci, L. (2018). How marginalized young people access, engage with, and navigate health-care systems in the digital age: Systematic review. Journal of Adolescent Health, 62(4), 365–381. https://doi.org/10.1016/j.jadohealth.2017.10.018
Shackleton, N., Milne, B. J., & Jerrim, J. (2019). Socioeconomic inequalities in adolescent substance use: Evidence from twenty-four European countries. Substance Use & Misuse, 54(6), 1044–1049. https://doi.org/10.1080/10826084.2018.1549080
Shamseer, L., Moher, D., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., Shekelle, P., Stewart, L. A., & PRISMA-P Group. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. Bmj, 350, g7647. https://doi.org/10.1136/bmj.g7647
Skov-Ettrup, L. S., Ringgaard, L. W., Dalum, P., Flensborg-Madsen, T., Thygesen, L. C., & Tolstrup, J. S. (2014). Comparing tailored and untailored text messages for smoking cessation: A randomized controlled trial among adolescent and young adult smokers. Health Education Research, 29(2), 195–205. https://doi.org/10.1093/her/cyt112
Smith, J. J., Morgan, P. J., Plotnikoff, R. C., Dally, K. A., Salmon, J., Okely, A. D., Finn, T. L., & Lubans, D. R. (2014). Smart-phone obesity prevention trial for adolescent boys in low-income communities: The ATLAS RCT. Pediatrics, 134(3), e723–e731. https://doi.org/10.1542/peds.2014-1012
Solar, O., & Irwin, A. (2010). A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2 (Policy and Practice). Retrieved October 11, 2021, from https://www.who.int/social_determinants/corner/SDHDP2.pdf
Spear, H. J., & Kulbok, P. (2004). Autonomy and adolescence: A concept analysis. Public Health Nursing, 21(2), 144–152. https://doi.org/10.1111/j.0737-1209.2004.021208.x
Sterne, J. A. C., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., Cates, C. J., Cheng, H.-Y., Corbett, M. S., Eldridge, S. M., Emberson, J. R., Hernán, M. A., Hopewell, S., Hróbjartsson, A., Junqueira, D. R., Jüni, P., Kirkham, J. J., Lasserson, T., Li, T., et al. (2019). RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ, 366, l4898. https://doi.org/10.1136/bmj.l4898
Tarasenko, Y., Ciobanu, A., Fayokun, R., Lebedeva, E., Commar, A., & Mauer-Stender, K. (2021). Electronic cigarette use among adolescents in 17 European study sites: findings from the Global Youth Tobacco Survey. European Journal of Public Health. https://doi.org/10.1093/eurpub/ckab180
Taylor, G. M. J., Dalili, M. N., Semwal, M., Civljak, M., Sheikh, A., & Car, J. (2017). Internet‐based interventions for smoking cessation. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD007078.pub5
Thornton, L. (2022). Measurement properties of smartphone approaches to assess diet, alcohol use, and tobacco use: Systematic review. JMIR mHealth and uHealth, 10(2), e27337. https://doi.org/10.2196/27337
Tripicchio, G. L., Ammerman, A. S., Neshteruk, C., Faith, M. S., Dean, K., Befort, C., Ward, D. S., Truesdale, K. P., Burger, K. S., & Davis, A. (2017). Technology components as adjuncts to family-based pediatric obesity treatment in low-income minority youth. Childhood Obesity, 13(6), 433–442. https://doi.org/10.1089/chi.2017.0021
Vogl, L., Teesson, M., Andrews, G., Bird, K., Steadman, B., & Dillon, P. (2009). A computerized harm minimization prevention program for alcohol misuse and related harms: Randomized controlled trial. Addiction, 104(4), 564–575. https://doi.org/10.1111/j.1360-0443.2009.02510.x
Voogt, C. V., Kleinjan, M., Poelen, E. A. P., Lemmers, L. A. C. J., & Engels, R. C. M. E. (2013). The effectiveness of a web-based brief alcohol intervention in reducing heavy drinking among adolescents aged 15–20 years with a low educational background: A two-arm parallel group cluster randomized controlled trial. BMC Public Health, 13(1), 1–11. https://doi.org/10.1186/1471-2458-13-694
Warren, J. C., Smalley, K. B., & Barefoot, K. N. (2017). Recent alcohol, tobacco, and substance use variations between rural and urban middle and high school students. Journal of Child & Adolescent Substance Abuse, 26(1), 60–65. https://doi.org/10.1080/1067828X.2016.1210550
Wills, T. A., Sargent, J. D., Gibbons, F. X., Pagano, I., & Schweitzer, R. (2016). E-cigarette use is differentially related to smoking onset among lower risk adolescents. Tobacco Control, 26(5), 534–539. https://doi.org/10.1136/tobaccocontrol-2016-053116
World Health Organization. (2016). Growing up unequal: gender and socioeconomic differences in young people's health and well-being. World Health Organization. Regional Office for Europe. Retrieved August 26, 2022, from https://apps.who.int/iris/handle/10665/326320
World Health Organization. (2020). Youth-centred digital health interventions: a framework for planning, developing and implementing solutions with and for young people. WHO. Retrieved October 13, 2022, from https://apps.who.int/iris/bitstream/handle/10665/336223/9789240011717-eng.pdf
World Health Organization. (2021). Adolescent Health. Retrieved October 11, 2021, from https://www.who.int/health-topics/adolescent-health#tab=tab_1
Wright, J. A., Phillips, B. D., Watson, B. L., Newby, P. K., Norman, G. J., & Adams, W. G. (2013). Randomized trial of a family-based, automated, conversational obesity treatment program for underserved populations. Obesity, 21(9), e369–e378. https://doi.org/10.1002/oby.20388
Acknowledgements
The authors are grateful to Tess Aitkin, Academic Liaison Librarian at the University of Sydney, for contributing to the design of search strategies used in this study.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. Lyra Egan is supported by a Paul Ramsay Foundation PhD Scholarship. Nicola Newton is funded by an NHMRC Career Development Fellowship. The Paul Ramsay Foundation and NHMRC had no role in study design, data collection, data analysis, data interpretation or writing of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors (LE, LAG, NN and KC) designed the study protocol; LE completed all database searches, article screening, data extraction, risk of bias assessments, interpretation of results and drafted the initial manuscript; LAG contributed to screening a subset (approximately 9%) of included studies and resolved disagreements through consultation with all authors; NN contributed to screening a subset (approximately 9%) of included studies and resolved disagreements through consultation with all authors; KC contributed to screening a subset (approximately 9%) of included studies and resolved disagreements through consultation with all authors, reviewed the data extraction sheet and conducted independent risk of bias assessments. All authors reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Preregistration
The study design, target analyses and synthesis of findings of this systematic review were prospectively registered with PROPSERO (CRD42021294119). Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021294119
Data Sharing
All data collected for this study were obtained from published peer-review literature. Data extracted to inform this review are available on reasonable request from the corresponding author.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1: Example Search Strategy
Appendix 1: Example Search Strategy
Database(s): MEDLINE (Ovid) search strategy from 1946 to Present.
Search Strategy: December 19, 2022.
Number | Search term |
|---|---|
1 | (eHealth or mhealth or electronic health or mobile health or telemedicine or telehealth).mp |
2 | Telemedicine/ |
3 | 1 or 2 |
4 | Teen*.mp |
5 | Adolescen*.mp. or Adolescent/ |
6 | Child*.mp. or Child/ |
7 | Young adult*.mp. or Young Adult/ |
8 | 4 or 5 or 6 or 7 |
9 | Diet*.mp. or Diet/ |
10 | Nutrition.mp |
11 | Alcohol.mp |
12 | Alcoholic Beverages/ |
13 | Smoking.mp. or Smoking/ |
14 | Cigarette.mp. or Tobacco Products/ |
15 | Vaping.mp. or Vaping/ |
16 | 9 or 10 or 11 or 12 or 13 or 14 or 15 |
17 | Socioeconomic status.mp. or Social Class/ |
18 | Socioeconomic Factors/ or low socioeconomic.mp |
19 | Poor.mp. or Working Poor/ |
20 | Low income.mp |
21 | Rural.mp. or Rural Health/ or Rural Population/ |
22 | (Regional or remote).mp |
23 | 17 or 18 or 19 or 20 or 21 or 22 |
24 | 3 and 8 and 16 and 23 |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Egan, L., Gardner, L.A., Newton, N. et al. A Systematic Review of eHealth Interventions Among Adolescents of Low Socioeconomic and Geographically Remote Backgrounds in Preventing Poor Diet, Alcohol Use, Tobacco Smoking and Vaping. Adolescent Res Rev 9, 1–32 (2024). https://doi.org/10.1007/s40894-023-00210-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40894-023-00210-2