Abstract
Purpose
Skin injuries are a worldwide health issue that affects millions of people each year. Tissue engineering has the potential to provide an opportunity to resolve this challenge. For more than 40 decades, researchers have focused on different aspects of skin tissue engineering. The purpose of the present study was to provide a comprehensive overview of the critical factors in skin tissue engineering.
Methods
Recent studies were investigated to gather relevant studies about the basic aspects of skin tissue engineering.
Results
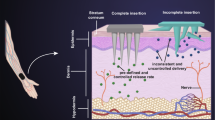
In the present review, the nature of the native skin and natural repair of the skin injuries is described. The knowledge of this part is a foundation for producing a tissue or organ that mimics the actual one. Then, the different essential elements in skin tissue engineering are underlined. In this regard, a variety of cells and scaffolds that create the main structure of the engineered constructs are emphasized. On the other hand, the application of critical signaling factors including biochemical, physicochemical, and physical factors in skin tissue engineering are reviewed.
Conclusion
A comprehensive review of these components clarifies critical points in the regenerative medicine of the skin and guides researchers to adopt optimized approaches to achieve a viable and functional construct.


Similar content being viewed by others
References
Wong, R., Geyer, S., Weninger, W., Guimberteau, J. C., & Wong, J. K. (2016). The dynamic anatomy and patterning of skin. Experimental Dermatology, 25(2), 92–98. https://doi.org/10.1111/exd.12832
White, S. D., & Yager, J. A. (1995). Resident dendritic cells in the epidermis: Langerhans cells, Merkel cells and melanocytes. Veterinary Dermatology, 6(1), 1–8. https://doi.org/10.1111/j.1365-3164.1995.tb00034.x
Zaidi, Z., & Lanigan, S. W. (2010). Skin: Structure and function. Dermatology in clinical practice. London: Springer.
Macefield, V. G. (2005). Physiological characteristics of low-threshold mechanoreceptors in joints, muscle and skin in human subjects. Clinical and Experimental Pharmacology and Physiology, 32(1–2), 135–144. https://doi.org/10.1111/j.1440-1681.2005.04143.x
Rittié, L. (2016). Cellular mechanisms of skin repair in humans and other mammals. Journal of Cell Communication and Signaling, 10(2), 103–120. https://doi.org/10.1007/s12079-016-0330-1
Ridiandries, A., Tan, J. T. M., & Bursill, C. A. (2018). The role of chemokines in wound healing. International Journal of Molecular Sciences, 19(10), 3217. https://doi.org/10.3390/ijms19103217
Clark, R. (1994). Wound repair. In R. A. F. Clark (Ed.), The molecular and cellular biology of wound repair. Boston: Springer.
Rheinwald, J., & Green, H. (1975). Serial cultivation of strains of human epidermal keratinocytes: the formation of keratinizing colonies from single cells. Cell, 6(3), 331–343.
Farhadihosseinabadi, B., Farahani, M., Tayebi, T., Jafari, A., Biniazan, F., Modaresifar, K., Moravvej, H., Bahrami, S., Redl, H., & Tayebi, L. (2018). Amniotic membrane and its epithelial and mesenchymal stem cells as an appropriate source for skin tissue engineering and regenerative medicine. Artificial Cells, Nanomedicine, and Biotechnology, 46(sup2), 431–440. https://doi.org/10.1080/21691401.2018.1458730
Keirouz, A., Zakharova, M., Kwon, J., Robert, C., Koutsos, V., Callanan, A., Chen, X., Fortunato, G., & Radacsi, N. (2020). High-throughput production of silk fibroin-based electrospun fibers as biomaterial for skin tissue engineering applications. Materials Science and Engineering: C, 112, 110939. https://doi.org/10.1016/j.msec.2020.110939
Rad, Z. P., Mokhtari, J., & Abbasi, M. (2018). Fabrication and characterization of PCL/zein/gum Arabic electrospun nanocomposite scaffold for skin tissue engineering. Materials Science and Engineering: C, 93, 356–366. https://doi.org/10.1016/j.msec.2018.08.010
Zelen, C. M., Serena, T. E., Gould, L., Le, L., Carter, M. J., Keller, J., & Li, W. W. (2016). Treatment of chronic diabetic lower extremity ulcers with advanced therapies: A prospective, randomised, controlled, multi-centre comparative study examining clinical efficacy and cost. International Wound Journal, 13(2), 272–282. https://doi.org/10.1111/iwj.12566
Nicholas, M. N., Jeschke, M. G., & Amini-Nik, S. (2016). Cellularized bilayer pullulan-gelatin hydrogel for skin regeneration. Tissue Engineering Part A, 22(9–10), 754–764. https://doi.org/10.1089/ten.TEA.2015.0536
Sabolinski, M. L., & Gibbons, G. (2018). Comparative effectiveness of a bilayered living cellular construct and an acellular fetal bovine collagen dressing in the treatment of venous leg ulcers. Journal of Comparative Effectiveness Research, 7(8), 797–805. https://doi.org/10.2217/cer-2018-0031
Baltazar, T., Merola, J., Catarino, C., Xie, C. B., Kirkiles-Smith, N. C., Lee, V., Hotta, S., Dai, G., Xu, X., Ferreira, F. C., Saltzman, W. M., Pober, J. S., & Karande, P. (2020). Three dimensional bioprinting of a vascularized and perfusable skin graft using human keratinocytes, fibroblasts, pericytes, and endothelial cells. Tissue Engineering Part A, 26(5–6), 227–238. https://doi.org/10.1089/ten.TEA.2019.0201
Barros, N. R., Kim, H. J., Gouidie, M. J., Lee, K., Bandaru, P., Banton, E. A., Sarikhani, E., Sun, W., Zhang, S., Cho, H. J., Hartel, M. C., Ostrovidov, S., Ahadian, S., Hussain, S. M., Ashammakhi, N., Dokmeci, M. R., Herculano, R. D., Lee, J., & Khademhosseini, A. (2021). Biofabrication of endothelial cell, dermal fibroblast, and multilayered keratinocyte layers for skin tissue engineering. Biofabrication, 13(3), 035030. https://doi.org/10.1088/1758-5090/aba503
Zhong, J., Wang, H., Yang, K., Wang, H., Duan, C., Ni, N., An, L., Luo, Y., Zhao, P., Gou, Y., Sheng, S., Shi, D., Chen, C., Wagstaff, W., Hendren-Santiago, B., Haydon, R. C., Luu, H. H., Reid, R. R., Ho, S. H., … Fan, J. (2022). Reversibly immortalized keratinocytes (iKera) facilitate re-epithelization and skin wound healing: Potential applications in cell-based skin tissue engineering. Bioactive Material, 9, 523–540. https://doi.org/10.1016/j.bioactmat.2021.07.022
Hashemi, S. S., Mohammadi, A. A., Moshirabadi, K., & Zardosht, M. (2021). Effect of dermal fibroblasts and mesenchymal stem cells seeded on an amniotic membrane scaffold in skin regeneration: A case series. Journal of Cosmetic Dermatology, 20(12), 4040–4047. https://doi.org/10.1111/jocd.14043
Loh, E. Y. X., Fauzi, M. B., Ng, M. H., Ng, P. Y., Ng, S. F., & Amin, M. C. I. M. (2020). Insight into delivery of dermal fibroblast by non-biodegradable bacterial nanocellulose composite hydrogel on wound healing. International Journal of Biological Macromolecules, 159, 497–509. https://doi.org/10.1016/j.ijbiomac.2020.05.011
Shera, S. S., & Banik, R. M. (2021). Development of tunable silk fibroin/xanthan biopolymeric scaffold for skin tissue engineering using L929 fibroblast cells. Journal of Bionic Engineering, 18(1), 103–117. https://doi.org/10.1007/s42235-021-0004-4
Sharif, S., Ai, J., Azami, M., Verdi, J., Atlasi, M. A., Shirian, S., & Samadikuchaksaraei, A. (2018). Collagen-coated nano-electrospun PCL seeded with human endometrial stem cells for skin tissue engineering applications. Journal of Biomedical Materials Research Part B, Applied Biomaterials, 106(4), 1578–1586. https://doi.org/10.1002/jbm.b.33966
Oryan, A., Alemzadeh, E., Mohammadi, A. A., & Moshiri, A. (2019). Healing potential of injectable Aloe vera hydrogel loaded by adipose-derived stem cell in skin tissue-engineering in a rat burn wound model. Cell and Tissue Research, 377(2), 215–227. https://doi.org/10.1007/s00441-019-03015-9
Ranjbarvan, P., Golchin, A., Azari, A., & Niknam, Z. (2021). The bilayer skin substitute based on human adipose-derived mesenchymal stem cells and neonate keratinocytes on the 3D nanofibrous PCL-platelet gel scaffold. Polymer Bulletin, 79, 4013–4030. https://doi.org/10.1007/s00289-021-03702-0
Zhang, Z., Li, Z., Li, Y., Wang, Y., Yao, M., Zhang, K., Chen, Z., Yue, H., Shi, J., Guan, F., & Ma, S. (2021). Sodium alginate/collagen hydrogel loaded with human umbilical cord mesenchymal stem cells promotes wound healing and skin remodeling. Cell and Tissue Research, 383(2), 809–821. https://doi.org/10.1007/s00441-020-03321-7
Cui, B., Zhang, C., Gan, B., Liu, W., Liang, J., Fan, Z., Wen, Y., Yang, Y., Peng, X., & Zhou, Y. (2020). Collagen-tussah silk fibroin hybrid scaffolds loaded with bone mesenchymal stem cells promote skin wound repair in rats. Materials Science & Engineering, C: Materials for Biological Applications, 109, 110611. https://doi.org/10.1016/j.msec.2019.110611
Kaviani, M., Geramizadeh, B., Rahsaz, M., & Marzban, S. (2015). Considerations in the improvement of human epidermal keratinocyte culture in vitro. Experimental and Clinical Transplantation, 13(Suppl 1), 366–370. https://doi.org/10.6002/ect.mesot2014.L4
Rahsaz, M., Geramizadeh, B., Kaviani, M., & Marzban, S. (2015). Gelatin for purification and proliferation of primary keratinocyte culture for use in chronic wounds and burns. Experimental and Clinical Transplantation, 13(1), 361–365. https://doi.org/10.6002/ect.mesot2014.L4
Luckett, L. R., & Gallucci, R. M. (2007). Interleukin-6 (IL-6) modulates migration and matrix metalloproteinase function in dermal fibroblasts from IL-6KO mice. British Journal of Dermatology, 156(6), 1163–1171. https://doi.org/10.1111/j.1365-2133.2007.07867.x
Nolte, S. V., Xu, W., Rennekampff, H.-O., & Rodemann, H. P. (2008). Diversity of fibroblasts–a review on implications for skin tissue engineering. Cells Tissues Organs, 187(3), 165–176. https://doi.org/10.1159/000111805
Zhao, X., Psarianos, P., Ghoraie, L. S., Yip, K., Goldstein, D., Gilbert, R., Witterick, I., Pang, H., Hussain, A., Lee, J. H., Williams, J., Bratman, S. V., Ailles, L., Haibe-Kains, B., & Liu, F. F. (2019). Metabolic regulation of dermal fibroblasts contributes to skin extracellular matrix homeostasis and fibrosis. Nature Metabolism, 1(1), 147–157. https://doi.org/10.1038/s42255-018-0008-5
Chopra, A., Murray, M. E., Byfield, F. J., Mendez, M. G., Halleluyan, R., Restle, D. J., Raz-Ben Aroush, D., Galie, P. A., Pogoda, K., Bucki, R., Marcinkiewicz, C., Prestwich, G. D., Zarembinski, T. I., Chen, C. S., Pure, E., Kresh, J. Y., & Janmey, P. A. (2014). Augmentation of integrin-mediated mechanotransduction by hyaluronic acid. Biomaterials, 35(1), 71–82. https://doi.org/10.1016/j.biomaterials.2013.09.066
Sasaki, M., Abe, R., Fujita, Y., Ando, S., Inokuma, D., & Shimizu, H. (2008). Mesenchymal stem cells are recruited into wounded skin and contribute to wound repair by transdifferentiation into multiple skin cell type. The Journal of Immunology, 180(4), 2581–2587. https://doi.org/10.4049/jimmunol.180.4.2581
Jin, G., Prabhakaran, M. P., & Ramakrishna, S. (2011). Stem cell differentiation to epidermal lineages on electrospun nanofibrous substrates for skin tissue engineering. Acta Biomaterialia, 7(8), 3113–3122. https://doi.org/10.1016/j.actbio.2011.04.017
Han, C. M., Zhang, L. P., Sun, J. Z., Shi, H. F., Zhou, J., & Gao, C. Y. (2010). Application of collagen-chitosan/fibrin glue asymmetric scaffolds in skin tissue engineering. Journal of Zhejiang University Science B, 11(7), 524–530. https://doi.org/10.1631/jzus.B0900400
Lee, J. J., Lee, S.-G., Park, J. C., Yang, Y. I., & Kim, J. K. (2007). Investigation on biodegradable PLGA scaffold with various pore size structure for skin tissue engineering. Current Applied Physics, 7, e37–e40. https://doi.org/10.1016/j.cap.2006.11.011
Liu, Y., Ma, L., & Gao, C. (2012). Facile fabrication of the glutaraldehyde cross-linked collagen/chitosan porous scaffold for skin tissue engineering. Materials Science and Engineering C, 32(8), 2361–2366. https://doi.org/10.1016/j.msec.2012.07.008
Ma, L., Gao, C., Mao, Z., Zhou, J., Shen, J., Hu, X., & Han, C. (2003). Collagen/chitosan porous scaffolds with improved biostability for skin tissue engineering. Biomaterials, 24(26), 4833–4841. https://doi.org/10.1016/s0142-9612(03)00374-0
Vázquez, J. J., & Martínez, E. S. M. (2019). Collagen and elastin scaffold by electrospinning for skin tissue engineering applications. Journal of Materials Research, 34(16), 2819–2827. https://doi.org/10.1557/jmr.2019.233
Zulkifli, F. H., Hussain, F. S. J., Rasad, M. S. B. A., & Yusoff, M. M. (2014). In vitro degradation study of novel HEC/PVA/collagen nanofibrous scaffold for skin tissue engineering applications. Polymer Degradation and Stability, 110, 473–481. https://doi.org/10.1016/j.polymdegradstab.2014.10.017
Gautam, S., Chou, C. F., Dinda, A. K., Potdar, P. D., & Mishra, N. C. (2014). Surface modification of nanofibrous polycaprolactone/gelatin composite scaffold by collagen type I grafting for skin tissue engineering. Materials Science & Engineering, C: Materials for Biological Applications, 34, 402–409. https://doi.org/10.1016/j.msec.2013.09.043
Gomes, S., Rodrigues, G., Martins, G., Henriques, C., & Silva, J. C. (2017). Evaluation of nanofibrous scaffolds obtained from blends of chitosan, gelatin and polycaprolactone for skin tissue engineering. International Journal of Biological Macromolecules, 102, 1174–1185. https://doi.org/10.1016/j.ijbiomac.2017.05.004
Han, F., Dong, Y., Su, Z., Yin, R., Song, A., & Li, S. (2014). Preparation, characteristics and assessment of a novel gelatin–chitosan sponge scaffold as skin tissue engineering material. International Journal of Pharmaceutics, 476(1–2), 124–133. https://doi.org/10.1016/j.ijpharm.2014.09.036
Pezeshki-Modaress, M., Mirzadeh, H., & Zandi, M. (2015). Gelatin–GAG electrospun nanofibrous scaffold for skin tissue engineering: fabrication and modeling of process parameters. Materials Science and Engineering: C, 48, 704–712. https://doi.org/10.1016/j.msec.2014.12.023
Pezeshki-Modaress, M., Zandi, M., & Rajabi, S. (2018). Tailoring the gelatin/chitosan electrospun scaffold for application in skin tissue engineering: An in vitro study. Progress in Biomaterials, 7(3), 207–218. https://doi.org/10.1007/s40204-018-0094-1
Bhardwaj, N., Sow, W. T., Devi, D., Ng, K. W., Mandal, B. B., & Cho, N.-J. (2015). Silk fibroin–keratin based 3D scaffolds as a dermal substitute for skin tissue engineering. Integrative Biology, 7(1), 53–63. https://doi.org/10.1039/C4IB00208C
Adekogbe, I., & Ghanem, A. (2005). Fabrication and characterization of DTBP-crosslinked chitosan scaffolds for skin tissue engineering. Biomaterials, 26(35), 7241–7250. https://doi.org/10.1016/j.biomaterials.2005.05.043
Shalumon, K. T., Anulekha, K. H., Chennazhi, K. P., Tamura, H., Nair, S. V., & Jayakumar, R. (2011). Fabrication of chitosan/poly(caprolactone) nanofibrous scaffold for bone and skin tissue engineering. International Journal of Biological Macromolecules, 48(4), 571–576. https://doi.org/10.1016/j.ijbiomac.2011.01.020
Zhu, T., Jiang, J., Zhao, J., Chen, S., & Yan, X. (2019). Regulating preparation of functional alginate-chitosan three-dimensional scaffold for skin tissue engineering. International Journal of Nanomedicine, 14, 8891–8903. https://doi.org/10.2147/IJN.S210329
Keskin, Z., Sendemir Urkmez, A., & Hames, E. E. (2017). Novel keratin modified bacterial cellulose nanocomposite production and characterization for skin tissue engineering. Materials Science & Engineering, C: Materials for Biological Applications, 75, 1144–1153. https://doi.org/10.1016/j.msec.2017.03.035
Monteiro, I. P., Shukla, A., Marques, A. P., Reis, R. L., & Hammond, P. T. (2015). Spray-assisted layer-by-layer assembly on hyaluronic acid scaffolds for skin tissue engineering. Journal of Biomedical Materials Research. Part A, 103(1), 330–340. https://doi.org/10.1002/jbm.a.35178
Solovieva, E. V., Fedotov, A. Y., Mamonov, V. E., Komlev, V. S., & Panteleyev, A. A. (2018). Fibrinogen-modified sodium alginate as a scaffold material for skin tissue engineering. Biomedical Materials, 13(2), 025007. https://doi.org/10.1088/1748-605X/aa9089
El Ghalbzouri, A., Lamme, E. N., van Blitterswijk, C., Koopman, J., & Ponec, M. (2004). The use of PEGT/PBT as a dermal scaffold for skin tissue engineering. Biomaterials, 25(15), 2987–2996. https://doi.org/10.1016/j.biomaterials.2003.09.098
Kumbar, S. G., Nukavarapu, S. P., James, R., Nair, L. S., & Laurencin, C. T. (2008). Electrospun poly(lactic acid-co-glycolic acid) scaffolds for skin tissue engineering. Biomaterials, 29(30), 4100–4107. https://doi.org/10.1016/j.biomaterials.2008.06.028
Ru, C., Wang, F., Pang, M., Sun, L., Chen, R., & Sun, Y. (2015). Suspended, shrinkage-free, electrospun PLGA nanofibrous scaffold for skin tissue engineering. ACS Applied Materials & Interfaces, 7(20), 10872–10877. https://doi.org/10.1021/acsami.5b01953
Zulkifli, F. H., Hussain, F. S. J., Zeyohannes, S. S., Rasad, M., & Yusuff, M. M. (2017). A facile synthesis method of hydroxyethyl cellulose-silver nanoparticle scaffolds for skin tissue engineering applications. Materials Science & Engineering, C: Materials for Biological Applications, 79, 151–160. https://doi.org/10.1016/j.msec.2017.05.028
Cui, W., Zhu, X., Yang, Y., Li, X., & Jin, Y. (2009). Evaluation of electrospun fibrous scaffolds of poly (dl-lactide) and poly (ethylene glycol) for skin tissue engineering. Materials Science and Engineering: C, 29(6), 1869–1876. https://doi.org/10.1016/j.msec.2009.02.013
Wolfe, P. S., Sell, S. A., & Bowlin, G. L. (2011). Natural and synthetic scaffolds. In N. Pallua & C. Suscheck (Eds.), Tissue engineering (pp. 41–67). Berlin: Springer.
Sundar, G., Joseph, J., John, A., & Abraham, A. (2021). Natural collagen bioscaffolds for skin tissue engineering strategies in burns: A critical review. International Journal of Polymeric Materials and Polymeric Biomaterials, 70(9), 593–604. https://doi.org/10.1080/00914037.2020.1740991
Willard, J. J., Drexler, J. W., Das, A., Roy, S., Shilo, S., Shoseyov, O., & Powell, H. M. (2013). Plant-derived human collagen scaffolds for skin tissue engineering. Tissue Engineering Part A, 19(13–14), 1507–1518. https://doi.org/10.1089/ten.TEA.2012.0338
Sarkar, S. D., Farrugia, B. L., Dargaville, T. R., & Dhara, S. (2013). Chitosan–collagen scaffolds with nano/microfibrous architecture for skin tissue engineering. Journal of Biomedical Materials Research Part A, 101(12), 3482–3492. https://doi.org/10.1002/jbm.a.34660
Ramanathan, G., Singaravelu, S., Muthukumar, T., Thyagarajan, S., Perumal, P. T., & Sivagnanam, U. T. (2017). Design and characterization of 3D hybrid collagen matrixes as a dermal substitute in skin tissue engineering. Materials Science and Engineering: C, 72, 359–370. https://doi.org/10.1016/j.msec.2016.11.095
Rnjak-Kovacina, J., Wise, S. G., Li, Z., Maitz, P. K., Young, C. J., Wang, Y., & Weiss, A. S. (2012). Electrospun synthetic human elastin: Collagen composite scaffolds for dermal tissue engineering. Acta Biomaterialia, 8(10), 3714–3722. https://doi.org/10.1016/j.actbio.2012.06.032
Buttafoco, L., Kolkman, N. G., Engbers-Buijtenhuijs, P., Poot, A. A., Dijkstra, P. J., Vermes, I., & Feijen, J. (2006). Electrospinning of collagen and elastin for tissue engineering applications. Biomaterials, 27(5), 724–734. https://doi.org/10.1016/j.biomaterials.2005.06.024
Gu, L. H., & Coulombe, P. A. (2007). Keratin function in skin epithelia: A broadening palette with surprising shades. Current Opinion in Cell Biology, 19(1), 13–23. https://doi.org/10.1016/j.ceb.2006.12.007
Madub, K., Goonoo, N., Gimie, F., Ait Arsa, I., Schonherr, H., & Bhaw-Luximon, A. (2021). Green seaweeds ulvan-cellulose scaffolds enhance in vitro cell growth and in vivo angiogenesis for skin tissue engineering. Carbohydrate Polymers, 251, 117025. https://doi.org/10.1016/j.carbpol.2020.117025
Shefa, A. A., Amirian, J., Kang, H. J., Bae, S. H., Jung, H. I., Choi, H. J., Lee, S. Y., & Lee, B. T. (2017). In vitro and in vivo evaluation of effectiveness of a novel TEMPO-oxidized cellulose nanofiber-silk fibroin scaffold in wound healing. Carbohydrate Polymers, 177, 284–296. https://doi.org/10.1016/j.carbpol.2017.08.130
Koh, L.-D., Cheng, Y., Teng, C.-P., Khin, Y.-W., Loh, X.-J., Tee, S.-Y., Low, M., Ye, E., Yu, H.-D., & Zhang, Y.-W. (2015). Structures, mechanical properties and applications of silk fibroin materials. Progress in Polymer Science, 46, 86–110. https://doi.org/10.1016/j.progpolymsci.2015.02.001
Hodgkinson, T., Yuan, X. F., & Bayat, A. (2014). Electrospun silk fibroin fiber diameter influences in vitro dermal fibroblast behavior and promotes healing of ex vivo wound models. Journal of Tissue Engineering, 5, 2041731414551661. https://doi.org/10.1177/2041731414551661
Chlapanidas, T., Tosca, M., Farago, S., Perteghella, S., Galuzzi, M., Lucconi, G., Antonioli, B., Ciancio, F., Rapisarda, V., & Vigo, D. (2013). Formulation and characterization of silk fibroin films as a scaffold for adipose-derived stem cells in skin tissue engineering. International Journal of Immunopathology and Pharmacology, 26(1_suppl), 43–49. https://doi.org/10.1177/03946320130260S106
Bacakova, M., Musilkova, J., Riedel, T., Stranska, D., Brynda, E., Zaloudkova, M., & Bacakova, L. (2016). The potential applications of fibrin-coated electrospun polylactide nanofibers in skin tissue engineering. International Journal of Nanomedicine, 11, 771–789. https://doi.org/10.2147/IJN.S99317
Bacakova, M., Pajorova, J., Stranska, D., Hadraba, D., Lopot, F., Riedel, T., Brynda, E., Zaloudkova, M., & Bacakova, L. (2017). Protein nanocoatings on synthetic polymeric nanofibrous membranes designed as carriers for skin cells. International Journal of Nanomedicine, 12, 1143. https://doi.org/10.2147/IJN.S121299
Bacakova, M., Pajorova, J., Sopuch, T., & Bacakova, L. (2018). Fibrin-modified cellulose as a promising dressing for accelerated wound healing. Materials, 11(11), 2314. https://doi.org/10.3390/ma11112314
Kenawy, E.-R., Abdel-Hay, F. I., El-Magd, A. A., & Mahmoud, Y. (2005). Biologically active polymers: Modification and anti-microbial activity of chitosan derivatives. Journal of Bioactive and Compatible Polymers, 20(1), 95–111. https://doi.org/10.1177/0883911505049655
Madni, A., Kousar, R., Naeem, N., & Wahid, F. (2021). Recent advancements in applications of chitosan-based biomaterials for skin tissue engineering. Journal of Bioresources and Bioproducts, 6(1), 11–25. https://doi.org/10.1016/j.jobab.2021.01.002
Asghari, F., Rabiei Faradonbeh, D., Malekshahi, Z. V., Nekounam, H., Ghaemi, B., Yousefpoor, Y., Ghanbari, H., & Faridi-Majidi, R. (2022). Hybrid PCL/chitosan-PEO nanofibrous scaffolds incorporated with A. euchroma extract for skin tissue engineering application. Carbohydrate Polymers, 278, 118926. https://doi.org/10.1016/j.carbpol.2021.118926
Liu, H., Mao, J., Yao, K., Yang, G., Cui, L., & Cao, Y. (2004). A study on a chitosan-gelatin-hyaluronic acid scaffold as artificial skin in vitro and its tissue engineering applications. Journal of Biomaterials Science, Polymer Edition, 15(1), 25–40. https://doi.org/10.1163/156856204322752219
Abatangelo, G., Vindigni, V., Avruscio, G., Pandis, L., & Brun, P. (2020). Hyaluronic acid: Redefining its role. Cells, 9(7), 1743. https://doi.org/10.3390/cells9071743
Wolf, K. J., & Kumar, S. (2019). Hyaluronic acid: incorporating the bio into the material. ACS Biomaterials Science & Engineering, 5(8), 3753–3765. https://doi.org/10.1021/acsbiomaterials.8b01268
Ehterami, A., Salehi, M., Farzamfar, S., Samadian, H., Vaez, A., Ghorbani, S., Ai, J., & Sahrapeyma, H. (2019). Chitosan/alginate hydrogels containing Alpha-tocopherol for wound healing in rat model. Journal of Drug Delivery Science and Technology, 51, 204–213. https://doi.org/10.1016/j.jddst.2019.02.032
Shi, L., Xiong, L., Hu, Y., Li, W., Chen, Z., Liu, K., & Zhang, X. (2018). Three-dimensional printing alginate/gelatin scaffolds as dermal substitutes for skin tissue engineering. Polymer Engineering & Science, 58(10), 1782–1790. https://doi.org/10.1002/pen.24779
Aderibigbe, B. A., & Buyana, B. (2018). Alginate in wound dressings. Pharmaceutics, 10(2), 42. https://doi.org/10.3390/pharmaceutics10020042
Yang, D., & Jones, K. S. (2009). Effect of alginate on innate immune activation of macrophages. Journal of Biomedical Materials Research. Part A, 90(2), 411–418. https://doi.org/10.1002/jbm.a.32096
Sadeghi, A., Nokhasteh, S., Molavi, A., Khorsand-Ghayeni, M., Naderi-Meshkin, H., & Mahdizadeh, A. (2016). Surface modification of electrospun PLGA scaffold with collagen for bioengineered skin substitutes. Materials Science and Engineering: C, 66, 130–137. https://doi.org/10.1016/j.msec.2016.04.073
Cipitria, A., Skelton, A., Dargaville, T., Dalton, P., & Hutmacher, D. (2011). Design, fabrication and characterization of PCL electrospun scaffolds—a review. Journal of Materials Chemistry, 21(26), 9419–9453. https://doi.org/10.1039/C0JM04502K
Wang, H. J., Bertrand-De Haas, M., Riesle, J., Lamme, E., & Van Blitterswijk, C. A. (2003). Tissue engineering of dermal substitutes based on porous PEGT/PBT copolymer scaffolds: Comparison of culture conditions. Journal of Materials Science. Materials in Medicine, 14(3), 235–240. https://doi.org/10.1023/a:1022880623151
Law, J. X., Liau, L. L., Saim, A., Yang, Y., & Idrus, R. (2017). Electrospun collagen nanofibers and their applications in skin tissue engineering. Tissue Engineering and Regenerative Medicine, 14(6), 699–718. https://doi.org/10.1007/s13770-017-0075-9
Ghafari, R., Jonoobi, M., Amirabad, L. M., Oksman, K., & Taheri, A. R. (2019). Fabrication and characterization of novel bilayer scaffold from nanocellulose based aerogel for skin tissue engineering applications. International Journal of Biological Macromolecules, 136, 796–803. https://doi.org/10.1016/j.ijbiomac.2019.06.104
Pereira, R. F., Barrias, C. C., Bartolo, P. J., & Granja, P. L. (2018). Cell-instructive pectin hydrogels crosslinked via thiol-norbornene photo-click chemistry for skin tissue engineering. Acta Biomaterialia, 66, 282–293. https://doi.org/10.1016/j.actbio.2017.11.016
Su, T., Zhang, M., Zeng, Q., Pan, W., Huang, Y., Qian, Y., Dong, W., Qi, X., & Shen, J. (2021). Mussel-inspired agarose hydrogel scaffolds for skin tissue engineering. Bioactive Materials, 6(3), 579–588. https://doi.org/10.1016/j.bioactmat.2020.09.004
Afghah, F., Ullah, M., Seyyed Monfared Zanjani, J., Akkus Sut, P., Sen, O., Emanet, M., Saner Okan, B., Culha, M., Menceloglu, Y., Yildiz, M., & Koc, B. (2020). 3D printing of silver-doped polycaprolactone-poly(propylene succinate) composite scaffolds for skin tissue engineering. Biomedical Materials, 15(3), 035015. https://doi.org/10.1088/1748-605X/ab7417
Daikuara, L. Y., Yue, Z., Skropeta, D., & Wallace, G. G. (2021). In vitro characterisation of 3D printed platelet lysate-based bioink for potential application in skin tissue engineering. Acta Biomaterialia, 123, 286–297. https://doi.org/10.1016/j.actbio.2021.01.021
Xue, J., Wu, T., Dai, Y., & Xia, Y. (2019). Electrospinning and electrospun nanofibers: Methods, materials, and applications. Chemical Reviews, 119(8), 5298–5415. https://doi.org/10.1021/acs.chemrev.8b00593
Keirouz, A., Chung, M., Kwon, J., Fortunato, G., & Radacsi, N. (2020). 2D and 3D electrospinning technologies for the fabrication of nanofibrous scaffolds for skin tissue engineering: A review. Wiley Interdisciplinary Reviews Nanomedicine and Nanobiotechnology, 12(4), e1626. https://doi.org/10.1002/wnan.1626
Park, Y. R., Ju, H. W., Lee, J. M., Kim, D. K., Lee, O. J., Moon, B. M., Park, H. J., Jeong, J. Y., Yeon, Y. K., & Park, C. H. (2016). Three-dimensional electrospun silk-fibroin nanofiber for skin tissue engineering. International Journal of Biological Macromolecules, 93(Pt B), 1567–1574. https://doi.org/10.1016/j.ijbiomac.2016.07.047
Iswariya, S., Bhanukeerthi, A., Velswamy, P., Uma, T., & Perumal, P. T. (2016). Design and development of a piscine collagen blended pullulan hydrogel for skin tissue engineering. RSC Advances, 6(63), 57863–57871. https://doi.org/10.1039/C6RA03578G
Derr, K., Zou, J., Luo, K., Song, M. J., Sittampalam, G. S., Zhou, C., Michael, S., Ferrer, M., & Derr, P. (2019). Fully three-dimensional bioprinted skin equivalent constructs with validated morphology and barrier function. Tissue Engineering. Part C, Methods, 25(6), 334–343. https://doi.org/10.1089/ten.TEC.2018.0318
Choi, K. Y., Ajiteru, O., Hong, H., Suh, Y. J., Sultan, M. T., Lee, H., Lee, J. S., Lee, Y. J., Lee, O. J., Kim, S. H., & Park, C. H. (2023). A digital light processing 3D-printed artificial skin model and full-thickness wound models using silk fibroin bioink. Acta Biomaterialia, 164, 159–174. https://doi.org/10.1016/j.actbio.2023.04.034
Park, U., & Kim, K. (2017). Multiple growth factor delivery for skin tissue engineering applications. Biotechnology and Bioprocess Engineering, 22(6), 659–670. https://doi.org/10.1007/s12257-017-0436-1
Colige, A., Nusgens, B., & Lapiere, C. (1988). Effect of EGF on human skin fibroblasts is modulated by the extracellular matrix. Archives of Dermatological Research, 280, S42–S46.
Yun, Y. R., Won, J. E., Jeon, E., Lee, S., Kang, W., Jo, H., Jang, J. H., Shin, U. S., & Kim, H. W. (2010). Fibroblast growth factors: Biology, function, and application for tissue regeneration. Journal of Tissue Engineering, 2010(1), 218142. https://doi.org/10.4061/2010/218142
Grazul-Bilska, A. T., Luthra, G., Reynolds, L. P., Bilski, J. J., Johnson, M. L., Adbullah, S. A., Redmer, D. A., & Abdullah, K. M. (2002). Effects of basic fibroblast growth factor (FGF-2) on proliferation of human skin fibroblasts in type II diabetes mellitus. Experimental and Clinical Endocrinology & Diabetes, 110(4), 176–181. https://doi.org/10.1055/s-2002-32149
Rinsch, C., Quinodoz, P., Pittet, B., Alizadeh, N., Baetens, D., Montandon, D., Aebischer, P., & Pepper, M. S. (2001). Delivery of FGF-2 but not VEGF by encapsulated genetically engineered myoblasts improves survival and vascularization in a model of acute skin flap ischemia. Gene Therapy, 8(7), 523–533. https://doi.org/10.1038/sj.gt.3301436
Qu, Y., Cao, C., Wu, Q., Huang, A., Song, Y., Li, H., Zuo, Y., Chu, C., Li, J., & Man, Y. (2018). The dual delivery of KGF and b FGF by collagen membrane to promote skin wound healing. Journal of Tissue Engineering and Regenerative Medicine, 12(6), 1508–1518. https://doi.org/10.1002/term.2691
Tan, J., Li, L., Wang, H., Wei, L., Gao, X., Zeng, Z., Liu, S., Fan, Y., Liu, T., & Chen, J. (2021). Biofunctionalized fibrin gel co-embedded with BMSCs and VEGF for accelerating skin injury repair. Materials Science & Engineering, C: Materials for Biological Applications, 121, 111749. https://doi.org/10.1016/j.msec.2020.111749
Li, P., Ruan, L., Wang, R., Liu, T., Song, G., Gao, X., Jiang, G., & Liu, X. (2021). Electrospun scaffold of collagen and polycaprolactone containing ZnO quantum dots for skin wound regeneration. Journal of Bionic Engineering, 18(6), 1378–1390. https://doi.org/10.1007/s42235-021-00115-7
Saik, J. E., Gould, D. J., Watkins, E. M., Dickinson, M. E., & West, J. L. (2011). Covalently immobilized platelet-derived growth factor-BB promotes angiogenesis in biomimetic poly(ethylene glycol) hydrogels. Acta Biomaterialia, 7(1), 133–143. https://doi.org/10.1016/j.actbio.2010.08.018
Judith, R., Nithya, M., Rose, C., & Mandal, A. B. (2010). Application of a PDGF-containing novel gel for cutaneous wound healing. Life Sciences, 87(1–2), 1–8. https://doi.org/10.1016/j.lfs.2010.05.003
Dearman, B. L., & Greenwood, J. E. (2021). Scale-up of a composite cultured skin using a novel bioreactor device in a porcine wound model. Journal of Burn Care & Research, 42(6), 1199–1209. https://doi.org/10.1093/jbcr/irab034
Sun, T., Norton, D., Haycock, J. W., Ryan, A. J., & MacNeil, S. (2005). Development of a closed bioreactor system for culture of tissue-engineered skin at an air–liquid interface. Tissue Engineering, 11(11–12), 1824–1831. https://doi.org/10.1089/ten.2005.11.1824
Wahlsten, A., Rutsche, D., Nanni, M., Giampietro, C., Biedermann, T., Reichmann, E., & Mazza, E. (2021). Mechanical stimulation induces rapid fibroblast proliferation and accelerates the early maturation of human skin substitutes. Biomaterials, 273, 120779. https://doi.org/10.1016/j.biomaterials.2021.120779
Kalyanaraman, B., & Boyce, S. T. (2009). Wound healing on athymic mice with engineered skin substitutes fabricated with keratinocytes harvested from an automated bioreactor. Journal of Surgical Research, 152(2), 296–302. https://doi.org/10.1016/j.jss.2008.04.001
Liu, J. Y., Hafner, J., Dragieva, G., & Burg, G. (2006). A novel bioreactor microcarrier cell culture system for high yields of proliferating autologous human keratinocytes. Cell Transplantation, 15(5), 435–443. https://doi.org/10.3727/000000006783981828
Kalyanaraman, B., & Boyce, S. (2007). Assessment of an automated bioreactor to propagate and harvest keratinocytes for fabrication of engineered skin substitutes. Tissue Engineering, 13(5), 983–993. https://doi.org/10.1089/ten.2006.0338
Norouzi, M., Shabani, I., Atyabi, F., & Soleimani, M. (2015). EGF-loaded nanofibrous scaffold for skin tissue engineering applications. Fibers and Polymers, 16(4), 782–787. https://doi.org/10.1007/s12221-015-0782-6
Golchin, A., & Nourani, M. R. (2020). Effects of bilayer nanofibrillar scaffolds containing epidermal growth factor on full-thickness wound healing. Polymers for Advanced Technologies, 31(11), 2443–2452. https://doi.org/10.1002/pat.4960
Mirdailami, O., Soleimani, M., Dinarvand, R., Khoshayand, M. R., Norouzi, M., Hajarizadeh, A., Dodel, M., & Atyabi, F. (2015). Controlled release of rh EGF and rhb FGF from electrospun scaffolds for skin regeneration. Journal of Biomedical Materials Research Part A, 103(10), 3374–3385. https://doi.org/10.1002/jbm.a.35479
Zhang, Z., Li, Z., Wang, Y., Wang, Q., Yao, M., Zhao, L., Shi, J., Guan, F., & Ma, S. (2021). PDGF-BB/SA/Dex injectable hydrogels accelerate BMSC-mediated functional full thickness skin wound repair by promoting angiogenesis. Journal of Materials Chemistry B, 9(31), 6176–6189. https://doi.org/10.1039/d1tb00952d
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
MK and BG were major contributors in the writing and critical edition of the manuscript. All authors contributed to the study conception and design. The first draft of the manuscript was written by [Maryam Kaviani] and Dr. Bita Geramizadeh commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kaviani, M., Geramizadeh, B. Basic Aspects of Skin Tissue Engineering: Cells, Biomaterials, Scaffold Fabrication Techniques, and Signaling Factors. J. Med. Biol. Eng. 43, 508–521 (2023). https://doi.org/10.1007/s40846-023-00822-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-023-00822-y