Abstract
Purpose
Intertrochanteric fractures are common among femoral fractures in the elderly population. The trochanteric nail is a standard internal fixator used in treating femoral intertrochanteric fractures. The technique of femoral fracture reduction affects the postoperative outcome. Here, we applied finite element analysis (FEA) to study mechanical effects of different reduction approaches using the trochanteric nail in treating both stable and unstable intertrochanteric fractures.
Methods
We combined FEA and in vitro experiments using a digital imaging correlation (DIC) technique to study effects of different alignment conditions after treating 4 cases of intertrochanteric fractures using the trochanteric nail system. A downward force of 2250 N was applied to the femoral head, and the distal end of the femur was fixed. The observed indicators were the femur displacement, together with the stress on the femur and trochanteric nail system. In addition, the displacement distribution was analyzed using DIC.
Results
In the case of space reduction, the force was transmitted by the trochanteric nail system, resulting in greater stress imposed on the femur or the trochanteric nail system. In the case of closed reduction, the stress was much smaller. In the case of unstable fracture reduction, closed reduction was associated with a smaller contact area at the fracture site, resulting in greater stress on both trochanter and the trochanteric nail system.
Conclusion
When the trochanteric nail system was used for fixation, the fracture site was well aligned, reducing the stress on the femur or the trochanteric nail.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
With an aging society, the elderly population, having relatively weak bones, is prone to femoral neck fractures and femoral intertrochanteric fractures due to falls and collisions [1]. Therefore, these bone fractures are their common problems with femurs. The classification of AO fractures is based on Müller [2]. The classification is conventionally used in clinical research. In order to analyze stable and unstable intertrochanteric fractures, A1 (stable) and A2 (unstable) are often used as analytical models [3].
The standard treatments for femoral intertrochanteric fractures are internal fixation of fracture and artificial hip replacement. Choice of treatment depends on the patient’s age, physical condition, fracture type, and degree of fracture displacement. Artificial hip replacement is often used for older or frail patients, with displaced fractures. Whereas internal fixation is used for stronger or younger patients, with slightly displaced fractures. Internal fixation methods include implanting multiple steel screws, a pair of crossed steel screws, a trochanteric nail internal fixator, or a dynamic hip screw [4]. Different styles of internal fixator are also developed to treat femoral intertrochanteric fractures as well as for various clinical conditions [4,5,6]. With developing science and technology, multiple medical devices for femoral fractures are available on the market (etc. trochanteric nail internal fixator, dynamic hip screw) for clinical practice along with more research on newly designed internal fixators. It is also important to study treatment techniques for femoral fractures. Several studies reported that reduction techniques for femoral fractures can affect postoperative outcomes [7, 8]. However, after implantation of the internal fixator, the reduction might result in poor alignment of the greater trochanter (misalignment or failure to fit). Therefore, if the femoral fracture is not properly reduced, surgical results and postoperative recovery are affected poorly.
Finite element analysis (FEA) is commonly used in orthopaedic research to evaluate biomechanical impact of implants. For example, FEA evaluations have been performed on the structure of trochanteric nails after implantation to the femur [9, 10]. Another study also compared implanted materials of trochanteric nails [11]. A biomechanical analysis was done comparing different trochanteric nails implanted for stable and unstable intertrochanteric fractures [12]. Therefore, FEA is suitable for analyzing trochanteric nail implants in the femur. However, no study has been made using FEA to analyze the effect of trochanteric fracture on alignment. FEA results are often compared with experimental results, but without adequate reference indicators. Digital imaging correlation (DIC) is a full-area strain/deformation measurement approach based on images. Selecting surface features of the tested object, or spraying a layer of randomly distributed speckles on the object surface, these speckles are displaced when the object is deformed. After the object is stressed, these displacements can be measured [13]. Therefore, DIC is also good at measuring implant deformations.
The elderly population suffer from femoral fractures caused by osteoporosis of the femur. After the reduction operation with the trochanteric nail internal fixator, the greater trochanter may not well-align, resulting in a failed reduction outcome. The main purpose of this study was to use FEA and DIC system to investigate the effects of different reduction situations for stable and unstable intertrochanteric fractures when fixed with a trochanteric nail system. Our results will provide clinical orthopaedic physicians with the preventive assessment of the displacement between different trochanteric femoral heads after trochanteric nail internal fixator surgery. Consequently patients can be treated with better surgical quality with a lower failure rate.
2 Materials and Methods
2.1 Building a Simulation Geometry Model
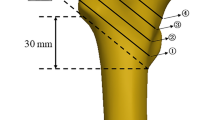
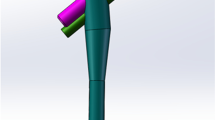
In this study, four stable and unstable femoral intertrochanteric fractures were treated with trochanteric nail implantation, and we aimed to analyze biomechanical effects of different contrapositions during surgery. The femur model we used was divided into five parts: cortical bone of femur, cancellous bone of femur, trochanteric nail, lag screw, and cortical screws. The femur model was established based on CT images (Visible Human Project) released by National Institutes of Health (NIH), using the medical imaging software Mimics (Mimics Medical 20.0, Materialise, Leuven, Belgium). The selected femur was divided into two parts: cortical bone and cancellous bone. The stable and unstable intertrochanteric fracture models we used followed the AO fracture classification (AO-OTA 31-A1 and AO-OTA 31-A2), and an inclined fracture site was established at the greater trochanter. For the trochanteric nail (Ø10 mm × 170 mm × 130°), lag screw (Ø10.5 mm × 90 mm) and cortical screw, we used a 3D CAD software (Solidworks, Dassault Systemes SolidWorks Corp, Waltham, MA, USA) for graphic presentation. The computer model of the trochanteric nail system is established with reference to the commercially available trochanteric nail system (Gamma3, Stryker, USA). In addition, the 3D CAD software Solidworks was further used to combine the femur, trochanteric nail, lag screw and cortical screw. They were divided into four groups (Fig. 1) as follows. Group 1: stable (AO-OTA 31-A1) fracture closed reduction. Group 2: Stable (AO-OTA 31-A1) fracture space reduction. Group 3: Unstable (AO-OTA 31-A2) fractures closed reduction. Group 4: Unstable (AO-OTA 31-A2) fracture space reduction. Models in which there was a space reduction, the intermediate spatial distance was set at 2 mm. The difference between stable and unstable femoral intertrochanteric fractures is whether the lesser trochanter of the femur is fractured. After establishing the 3D computer model, the model was imported into FEA software (ANSYS Workbench 18.0, ANSYS, Inc., Canonsburg, PA) for FEA.
2.2 Loading Conditions and Boundary Conditions
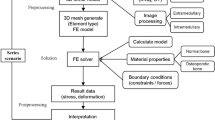
The femur’s simulated force is in accordance with the external force reported in the literature [14]. We gave a load condition and a boundary condition (Fig. 2a). The load condition is a downward external force at 2250 N applied on the femoral head [15]. In the boundary condition, the distal end of the femur is fixed. At this point, the X-, Y-, and Z-axes displacements are set to zero. Otherwise, the contact between the trochanteric nail and the lag screw is set to have no separation, and the contact between the implant and the femur is also set to have no separation. These settings simulate the lag screw which does not separate at the trochanteric nail connection, while allowing a small frictionless sliding [16]. In addition, the friction site contact surface of the inclined greater trochanter is set to frictional type, with a friction coefficient of 0.45 [17]. The intersections of other models are also set to bonded type. The mesh elements used in our FEA model are tetrahedral meshes (Fig. 2b). After the mesh passes the convergence test, the model reaches 5% stop criteria of the convergence test. We then used the mesh model to investigate whether trochanteric nail implantation of internal fixator devices is justified in different situations. The mesh size used in this study is 0.8 mm. The number of nodes and elements of the FEA model are shown in (Fig. 2b).
2.3 Material Properties of the Model
Our research model includes five parts: cortical bone of femur, cancellous bone of femur, trochanteric nail, lag screw, and cortical screws. We used the set material properties in accordance with the published data [14, 18, 19]. All materials are assumed to be homogeneous, isotropic, linear elastic. Therefore, Young’s modulus and Poisson’s ratio are used to represent the material properties. Material properties used for our simulations are shown in Table 1.
After FEA, we used the von Mises stress distribution as the observation index (von Mises stress is \({\upsigma }_{\mathrm{von}}\)=\(\sqrt{{\frac{1}{2}[({\upsigma }_{1}-{\upsigma }_{2})}^{2}+{{(\upsigma }_{1}-{\upsigma }_{3})}^{2}+{{(\upsigma }_{2}-{\upsigma }_{3})}^{2}]}\), where σ1, σ2, σ3 are principal stresses in the three axial directions). The main observation indicators are the von Mises stress on the femur, the von Mises stress on the trochanteric nail, the lag screw, and the cortical screw.
2.4 DIC Observation
Four artificial femurs (Sawbones femur (#3403), Pacific Research Laboratories, Vashon, USA) were trimmed with a cutting machine to generate AO-OTA intertrochanteric fractures of types 31-A1 and 31-A2. Among them, Group 1 and Group 2 are stable fractures (AO-OTA 31-A1), Group 3 and Group 4 are unstable fractures (AO-OTA 31-A2), and the intermediate fracture space of Group 2 and Group 4 is about 2 mm (Fig. 3a). The trochanteric nail (Gamma3, Stryker, USA) internal fixator was implanted into each artificial femur (the dimensions of trochanteric nail is Ø10 mm × 170 mm × 130° and the dimensions of lag screw is Ø10.5 mm × 90 mm). Speckles were sprayed as feature points on the surface of the artificial bone implanted with the trochanteric nail internal fixator. These feature points facilitated displacement observation by DIC. Embedding the femur with polyester resin (Poly), the femoral shaft was first set at 11° off vertical during embedding, consistent with the angle of the human femur [20]. The artificial femur was then fixed in the tensile testing machine (MTS 858 Mini Bionix Testing Machine; MTS Systems Corp., Eden Prairie, MN) (Fig. 3b). The DIC system (VIC, Correlated Solutions Inc., USA) was also used to evaluate the displacement when the femoral head was subjected to external force. The calibration plate was used to calibrate the position of the femur surface, with the light source adjusted during calibration, so that the spots on the calibration plate or the femoral surface were clearly visible (Fig. 3c). After calibrating the DIC system, the fixture position on the material test system (MTS) was adjusted so that the femoral head was under a preload of 10 N. After stabilization, a vertical downward displacement of 2 mm is delivered at a speed of 2 mm/min [9]. Afterwards, the DIC system was used with two 2.3 megapixel digital cameras to quantify displacements of feature spots on the femoral surface (Fig. 3b).
3 Results
After FEA, the distribution of von Mises stress in the entire femoral structure was obtained (Fig. 4). Figure 5 shows the von Mises stress distribution over the femur. We found the stress was higher on the femoral surface in Group 1 and Group 3. The stress on the fracture surface of Group 3 was greater than that of Group 1.
Figure 6 shows the von Mises stress distribution on the femur at the position of the trochanteric nail system. Figure 6a shows the von Mises stress distribution on the femur at the position of the trochanteric nail. We found that the stress on the femur was higher in Group 2 and Group 4. The stress on Group 4 was larger than Group 2. Figure 6b shows the von Mises stress distribution of the femur at the position of the lag screw. We found that the stress on the femur was higher in Group 2 and Group 4. The stress on Group 4 was larger than Group 2. Figure 6c shows the von Mises stress distribution of the femur at the position of cortical screws. We found that the stress on the femur was higher in Group 2 and Group 4. The stress in Group 4 was larger than Group 2.
Figure 7a shows the von Mises stress distribution on the trochanteric nail. We found that the stress on the femur was higher in Group 2 and Group 4. The stress on Group 4 was larger than Group 2. Figure 7b shows the von Mises stress distribution on the lag screw. We found that the stress on the femur was higher in Group 2 and Group 4. The stress on Group 4 was larger than Group 2. Figure 7c shows the von Mises stress distribution on cortical screws. We found that the stress on the femur was higher in Group 2 and Group 4. The stress on Group 4 was larger than Group 2.
Figure 8 shows the axial displacement distribution as revealed in the DIC system. We found that in Group 1 and Group 3, a downward displacement on the medial side of the femur, and an upward displacement on the lateral side of the femur. In addition, we found that in both Group 2 and Group 4, a downward displacement in the femur.
4 Discussion
In this study, we used FEA to investigate the effects of different reduction situations for stable and unstable intertrochanteric fractures when fixed with a trochanteric nail system. There were no detailed mechanical data on the postoperative impact of femoral fracture reduction in clinical practice. For orthopaedic surgeons, when performing trochanteric nail system femoral reduction surgery, the results of this study can be used as biomechanical reference to reduce postoperative failure.
The overall stress distribution of the femur was observed. We found minimal difference in the stress distribution among the various groups. However, regarding fracture site on the upper half of the femur, we found that during the two groups of space reduction (Groups 2 and 4), a higher stress at the position where the trochanteric nail was implanted. We also found that in the closed reduction groups (Groups 1 and 3), a higher stress on the surface of the femoral head, especially near the lesser trochanter abutting the fracture site. In addition, the unstable fracture reduction (Group 3) received a greater force on the femur because of the smaller contact cross-sectional area of the close reduction. Therefore, the results of FEA we found that the external force on the femur was transmitted from the greater trochanter during closed reduction. In the event of a gap present between the trochanters, the force was transmitted from the trochanteric nail system, resulting in a large deformation of the trochanteric nail system. The stress distribution on the femur in the implant area of the trochanteric nail system was observed, and results showed slightly higher stress on the bone in the area of the trochanteric nail and lag screw, when there was a gap in the reduction (Groups 2 and 4). However, at the position of the cortical screw, the stress distribution on the bone was similar. The main reason could be due to a large deformation in the trochanteric nail system and, therefore, also in the area of the femur that was in contact with the trochanteric nail system. According to Hooke’s law, there was also greater stress on the femur. As the cortical screw was far from the fracture site area, the influence was likely small. The position of high stress from the implanted trochanteric nail system on the femur was mostly in the area of cortical bone. That was because firstly, the femur received external force, which deformed the trochanteric nail system. And secondly the Young’s modulus of the cortical bone was larger compared with the cancellous bone. Therefore, according to Hooke’s law, because the stress is proportional to the Young’s modulus, the stress on the cortical bone is larger.
From the stress distribution on the trochanteric nail implant, we found that the trochanteric nail was subjected to a bending moment (one side was under compressive stress, and the other was under tensile stress). From the stress distribution on the lag screw, we found that the lag screw also received a bending moment. During reduction with a gap, there was a high stress on the trochanteric nail implant, especially in the area where the trochanteric nail was in contact with the lag screw. From the stress distribution of the cortical screws on the trochanteric nail system, we found that in the reduction group with a gap, a higher stress on the cortical screws. This is mainly because in such a group, the force was directly transmitted by the trochanteric nail implant. Thus, greater stress was generated on the trochanteric nail system. The material of the trochanteric nail was metal. It is known [21] that the ultimate strength of titanium alloy material is about 1250 MPa. In the case of reduction with a gap, it was more likely for the stress value on the trochanteric nail system to approach the ultimate strength and subsequently may causing a fracture. Therefore, it is recommended that when a trochanteric nail is used for fixation, the fracture site should have alignment as good as possible, reducing the stress on the trochanteric nail system and avoiding the failure of surgery. A previous study also reported that contact reduction of cortical bone is important in treating intertrochanteric fractures [22].
The biomechanical model of the artificial femur implanted with the trochanteric nail internal fixator was given a displacement by the tensile testing machine and it was observed with the DIC system. The DIC system used to outline the area of interest. Our area of interest was the trochanteric area. Because the fracture site of the femur under the action of external force has a great influence on the trochanter of the femur, this area was our main area of study. We found an axial displacement when the femur was subjected to external force. Regardless of a stable or an unstable fracture, the fracture site showed a downward displacement where the fracture site was in contact with the trochanter of the femur under the condition of closed reduction (Groups 1 and 3). The force was thus transmitted via the trochanteric fracture site. As the femur structure was subjected to an eccentric external force, the entire femur received a bending moment, with one side getting pressure and the other side getting tension. We also observed that the force was transmitted by the trochanteric nail in the case of reduction with a gap (Groups 2 and 4). Therefore, after the femur was subjected to an external force, the femoral trochanter showed an overall downward displacement. In addition, the DIC system revealed only the trend on the surface of the structure, and was unable to detect the inside deformation. Despite such a shortcoming, the DIC system has a much larger measurement range than the traditional single point measurement using the strain gauge.
There are several limitations in our present study. First, in our simulation experiment, all material properties were assumed to be homogeneous, isotropic, and linear elastic, as consistent with previous studies [23,24,25]. The reason was to limit the variability of the results of this study in using nonlinear materials. Although the mechanical response of cortical and cancellous bone is viscoelastic-plastic, the effect of loading rate on femur is a critical assessment. In homogeneous, isotropic and linear elastic models, the effect of time-dependent behavior is ignored in this study, leading to limitations of this work. Second, we only observed half of the femur (proximal end), in order to speed up simulation calculations. We argue that such assumptions may differ slightly from reality, but research trends do not change. In addition, we have tried to observe the principal stress in this study, but the magnitude of the principal stress depends on different directions. Therefore, if we want to discuss the influence of principal stress, we must consider the effect of different directions, and the results of discussion and analysis are complicated. Therefore, we used Von Mises stress as an observation index referring to other studies [23,24,25].
This study investigated the biomechanical analysis of different reduction situations of stable and unstable intertrochanteric fractures fixed by the trochanteric nail system through both in vitro experiments and FEA. Our results and experience can provide orthopaedic surgeons with a biomechanical reference, and provide tools for evaluating the reduction situation when performing trochanteric nail system surgery.
5 Conclusion
We found that in the case of space reduction, the force is transmitted by the trochanteric nail, resulting in a greater stress on the trochanteric nail system or femur. In the case of closed reduction, we found some smaller stress values on the trochanteric nail system or on the femur. In the case of unstable fracture reduction, the contact area of closed reduction at the fracture site is small. Consequently, the femur and the trochanteric nail system would receive a greater stress. Thus, we propose that when the trochanteric nail is used for fixation, good alignment on the fracture site can reduce the stress on the trochanteric nail system or femur.
Data Availability
Data and materials are available from the corresponding author under at a reasonable request.
Code Availability
Not applicable.
References
Napoli, N., Schwartz, A. V., Palermo, L., Jin, J. J., Wustrack, R., Cauley, J. A., Ensrud, K. E., Kelly, M., & Black, D. M. (2013). Risk factors for subtrochanteric and diaphyseal fractures: The study of osteoporotic fractures. The Journal of Clinical Endocrinology & Metabolism, 98(2), 659–667.
Müller, M. E., Nazarian, S., Koch, P., & Schatzker, J. (2012). The comprehensive classification of fractures of long bones. Springer Science & Business Media.
Schatzker, J., Tile, M., & Axelrod, T. S. (2005). The rationale of operative fracture care (Vol. 24). Springer.
Cooper, C., Cole, Z., Holroyd, C., Earl, S., Harvey, N. C., Dennison, E. M., Melton, L. J., Cummings, S. R., & Kanis, J. A. (2011). Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporosis International, 22(5), 1277–1288.
Melton, L. J., Kearns, A. E., Atkinson, E. J., Bolander, M. E., Achenbach, S. J., Huddleston, J. M., Therneau, T. M., & Leibson, C. L. (2009). Secular trends in hip fracture incidence and recurrence. Osteoporosis International, 20(5), 687–694.
Luthje, P., Santavirta, S., Nurmi, I., Honkanen, R., & Heiliovaaras, M. (1993). Increasing incidence of hip fractures in Finland. Archives of Orthopaedic and Trauma Surgery, 112(6), 280–282.
Davis, T., Sher, J., Horsman, A., Simpson, M., Porter, B., & Checketts, R. (1990). Intertrochanteric femoral fractures. Mechanical failure after internal fixation. The Journal of Bone and Joint Surgery, 72(1), 26–31.
Jensen, J. S., Sonne-Holm, S., & Tobndevold, E. (1980). Unstable trochanteric fractures: A comparative analysis of four methods of internal fixation. Acta Orthopaedica Scandinavica, 51(1–6), 949–962.
Kuan, F. C., Hsu, K. L., Lin, C. L., Hong, C. K., Yeh, M. L., & Su, W. R. (2019). Biomechanical properties of off-axis screw in Pauwels III femoral neck fracture fixation: Bicortical screw construct is superior to unicortical screw construct. Injury, 50(11), 1889–1894.
Kwak, D. K., Bang, S. H., Kim, W. H., Lee, S. J., Lee, S., & Yoo, J. H. (2021). Biomechanics of subtrochanteric fracture fixation using short cephalomedullary nails: A finite element analysis. PLoS ONE, 16(7), e0253862.
Wang, C., Li, X., Chen, W., Wang, C., Guo, Y., & Guo, H. (2021). Three-dimensional finite element analysis of intramedullary nail with different materials in the treatment of intertrochanteric fractures. Injury, 52(4), 705–712.
Ding, K., Zhu, Y., Li, Y., Wang, H., Cheng, X., Yang, W., Zhang, Y., Chen, W., & Zhang, Q. (2022). Triangular support intramedullary nail: A new internal fixation innovation for treating intertrochanteric fracture and its finite element analysis. Injury, 53(6), 1796–1804.
Palanca, M., Tozzi, G., & Cristofolini, L. (2016). The use of digital image correlation in the biomechanical area: A review. International Biomechanics, 3(1), 1–21.
Lee, C. H., Su, K. C., Chen, K. H., Pan, C. C., & Wu, Y. C. (2018). Impact of tip–apex distance and femoral head lag screw position on treatment outcomes of unstable intertrochanteric fractures using cephalomedullary nails. Journal of International Medical Research, 46(6), 2128–2140.
Helwig, P., Faust, G., Hindenlang, U., Hirschmüller, A., Konstantinidis, L., Bahrs, C., Südkamp, N., & Schneider, R. (2003). Finite element analysis of four different implants inserted in different positions to stabilize an idealized trochanteric femoral fracture. Injury, 40(3), 288–295.
Lee, H. H. (2014). Finite element simulations with ANSYS Workbench 15. Chuan Hwa Book Co.
Chen, Y. N., Chang, C. W., Lin, C. W., Wang, C. W., Peng, Y. T., Chang, C. H., & Li, C. T. (2017). Numerical investigation of fracture impaction in proximal humeral fracture fixation with locking plate and intramedullary nail. International Orthopaedics, 41(7), 1471–1480.
Hung, L. K., Su, K. C., Lu, W. H., & Lee, C. H. (2017). Biomechanical analysis of clavicle hook plate implantation with different hook angles in the acromioclavicular joint. International Orthopaedics, 41(8), 1663–1669.
Lee, C. H., Shih, C. M., Huang, K. C., Chen, K. H., Hung, L. K., & Su, K. C. (2016). Biomechanical analysis of implanted clavicle hook plates with different implant depths and materials in the acromioclavicular joint: A finite element analysis study. Artificial Organs, 40(11), 1062–1070.
Heiner, A. D., & Brown, T. D. (2001). Structural properties of a new design of composite replicate femurs and tibias. Journal of Biomechanics, 34(6), 773–781.
Enderle, J. (2012). Introduction to biomedical engineering. Academic Press.
Laros, G. S. (1983). Factors influencing the treatment of intertrochanteric fractures. The Iowa Orthopaedic Journal, 3, 62–64.
Tzeng, C. Y., Huang, K. C., Wu, Y. C., Chang, C. L., Lee, K. R., & Su, K. C. (2017). Biomechanical effect of different lag screw lengths with different barrel lengths in dynamic hip screw system: A finite element analysis study. Journal of Mechanics in Medicine and Biology, 17(01), 1750008.
Wang, C. C., Lee, C. H., Chin, N. C., Chen, K. H., Pan, C. C., & Su, K. C. (2020). Biomechanical analysis of the treatment of intertrochanteric hip fracture with different lengths of dynamic hip screw side plates. Technology and Health Care, 28(6), 593–602.
Wang, C. C., Lee, C. H., Chen, K. H., Pan, C. C., & Su, K. C. (2019). Effects of different lateral femoral wall thicknesses in intertrochanteric hip fracture treated with dynamic hip screw. Journal of Mechanics in Medicine and Biology, 19(02), 1940022.
Acknowledgements
The authors acknowledge the United States National Library of Medicine (NLM) and the Visible Human Project as the source of the image data used to create the finite element analysis model in this study. We would like to thank the Ministry of Science and Technology of Taiwan (MOST 110-2221-E-075A-001), Taichung Veterans General Hospital/HungKuang University Joint Research Program (TCVGH-HK1088001 and TCVGH-HK1098002), Taichung Veterans General Hospital (TCVGH-1057302B, TCVGH-1055105C, TCVGH-1095105C, TCVGH-1115101C and TCVGH-1117315C) in Taiwan and the 3D Printing Research and Development Group of Taichung Veterans General Hospital for building the simulation computer model of this study. The first authors Ming-Tzu Tsai and Cheng-Hung Lee have contributed equally to this work.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conception and design, MT Tsai, CH Lee, KH Chen and SP Wang; methodology, KC Su, YC Yen and CH Wang; data curation, KC Su and YC Yen; manuscript writing, MT Tsai, CH Lee and KC Su. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The article does not contain any studies with human participants or animals performed by any of the authors.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tsai, MT., Lee, CH., Chen, KH. et al. Trochanteric Nails for the Reduction of Intertrochanteric Fractures: A Biomechanical Analysis Based on Finite Element Analysis and DIC System. J. Med. Biol. Eng. 42, 459–468 (2022). https://doi.org/10.1007/s40846-022-00732-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-022-00732-5