Abstract
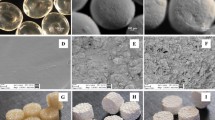
Tissue engineering scaffolds are intended as a replacement for conventional bone grafts used in the treatment of bone damages. One of the challenges in bone tissue engineering is to fabricate scaffolds with large pores, high porosity, and at the mean time proper mechanical properties suitable for bone applications. The elastic properties Young’s modulus and yield strength) of these scaffolds have been mostly considered but since bone is a viscoelastic material it is necessary to evaluate this behavior of the scaffolds as well. In the current study the novel method of microsphere sintering as a bottom-up approach was used to fabricate porous three dimensional (3D) bone scaffolds made of poly(ε-caprolactone) with controlled properties. Different variables effective on the mechanical and architectural properties of the scaffold (including time and temperature of the sintering process) were investigated and the optimum conditions (100 min and 64.5 °C) to fabricate scaffolds with the highest possible mechanical properties and porosity were determined (Young’s modulus = 33.61 MPa, yield strength = 2.2 MPa, with 44.5% porosity). Then the viscoelastic properties of this scaffold was evaluated and studied using stress relaxation test (25% stress relaxation) and generalized Maxwell model and compared to bone. Based on these results, the highly interconnected scaffold showed proper mechanical properties, pore size and structure proper for bone tissue engineering.







Similar content being viewed by others
References
Langer, R., & Vacanti, J. P. (1993). Tissue engineering. Science, 260(5110), 920–926.
Stock, U. A., & Vacanti, J. P. (2001). Tissue engineering: Current state and prospects. Annual Review of Medicine, 52, 443–451.
Place, E. S., Evans, N. D., & Stevens, M. M. (2009). Complexity in biomaterials for tissue engineering. Nature Materials, 8(6), 457–470.
Dawson, E., Mapili, G., Erickson, K., Taqvi, S., & Roy, K. (2008). Biomaterials for stem cell differentiation. Advanced Drug Delivery Reviews, 60(2), 215–228.
Doblaré, M., García, J. M., & Gómez, M. J. (2004). Modelling bone tissue fracture and healing: A review. Engineering Fracture Mechanics, 71(13), 1809–1840.
Laurencin, C. T., Ambrosio, A. M., Borden, M. D., & Cooper, J. A. (1999). Tissue engineering: Orthopedic applications. Annual Review of Biomedical Engineering, 1, 19–46.
Thomson, R. C., Yaszemski, M. J., Powers, J. M., & Mikos, A. G. (1998). Hydroxyapatite fiber reinforced poly(alpha-hydroxy ester) foams for bone regeneration. Biomaterials, 19(21), 1935–1943.
Mikos, A. G., Sarakinos, G., Lyman, M. D., Ingber, D. E., Vacanti, J. P., & Langer, R. (1993). Prevascularization of porous biodegradable polymers. Biotechnology and Bioengineering, 42(6), 716–723.
Hutmacher, D. W. (2001). Scaffold design and fabrication technologies for engineering tissues-state of the art and future perspectives. Journal of Biomaterials Science, 12(1), 107–124.
Wu, G. H., & Hsu, S. H. (2015). Polymeric-based 3D printing for tissue engineering. Journal of Medical and Biological Engineering, 35(3), 285–292.
Schmelzer, E., Over, P., Gridelli, B., & Gerlach, J. C. (2016). Response of primary human bone marrow mesenchymal stromal cells and dermal keratinocytes to thermal printer materials in vitro. Journal of Medical and Biological Engineering, 36(2), 153–167.
Devin, J. E., Attawia, M. A., & Laurencin, C. T. (1996). Three-dimensional degradable porous polymer-ceramic matrices for use in bone repair. Journal of Biomaterials Science, 7(8), 661–669.
Luciani, A., Coccoli, V., Orsi, S., Ambrosio, L., & Netti, P. A. (2008). PCL microspheres based functional scaffolds by bottom-up approach with predefined microstructural properties and release profiles. Biomaterials, 29(36), 4800–4807.
Ungaro, F., Nair, L. S., & Laurencin, C. T. (2006). Microsphere-integrated collagen scaffolds for tissue engineering: effect of microsphere formulation and scaffold properties on protein release kinetics. Journal of controlled Release, 113(2), 128–136.
Borden, M., Attawia, M., Khan, Y., & Laurencin, C. T. (2002). Tissue engineered microsphere-based matrices for bone repair: design and evaluation. Biomaterials, 23(2), 551–559.
Boyan, B. D., Hummert, T. W., Dean, D. D., & Schwartz, Z. (1996). Role of material surfaces in regulating bone and cartilage cell response. Biomaterials, 17(2), 137–146.
Hench, L. L., & Polak, J. M. (2002). Third-generation biomedical materials. Science, 295(5557), 1014–1017.
Hutmacher, D. W. (2000). Scaffolds in tissue engineering bone and cartilage. Biomaterials, 21(24), 2529–2543.
Marra, K. G., Szem, J. W., Kumta, P. N., DiMilla, P. A., & Weiss, L. E. (1999). In vitro analysis of biodegradable polymer blend/hydroxyapatite composites for bone tissue engineering. Journal of Biomedical Materials Research, 47(3), 324–335.
Ulery, B. D., Nair, L. S., & Laurencin, C. T. (2011). Biomedical Applications of Biodegradable Polymers. Journal of Polymer Science Part, 49(12), 832–864.
Dee, K.C., Puleo, D.A., & Bizios, R. (2003). Biomaterials. An introduction to tissue-biomaterial interactions (pp. 1–13). Wiley.
Discher, D. E., Janmey, P., & Wang, Y. L. (2005). Tissue cells feel and respond to the stiffness of their substrate. Science, 310(5751), 1139–1143.
Nazarov, R., Jin, H. J., & Kaplan, D. L. (2004). Porous 3-D scaffolds from regenerated silk fibroin. Biomacromolecules, 5(3), 718–726.
Matsuoka, S. (1992). Relaxation phenomena in polymers (p. 322). Munich: Hanser Gardner Publications.
Tschoegl, N. W. (2012). The phenomenological theory of linear viscoelastic behavior: an introduction. Berlin: Springer.
Troyer, K. L., Estep, D. J., & Puttlitz, C. M. (2012). Viscoelastic effects during loading play an integral role in soft tissue mechanics. Acta Biomaterialia, 8(1), 234–243.
Troyer, K. L., & Puttlitz, C. M. (2011). Human cervical spine ligaments exhibit fully nonlinear viscoelastic behavior. Acta Biomaterialia, 7(2), 700–709.
Troyer, K. L., & Puttlitz, C. M. (2012). Nonlinear viscoelasticty plays an essential role in the functional behavior of spinal ligaments. Journal of Biomechanics, 45(4), 684–691.
Zhang, X., & Gan, R. Z. (2014). Dynamic properties of human stapedial annular ligament measured with frequency-temperature superposition. Journal of Biomechanical Engineering, 136(8), 081004.
Boal, D. H. (2012). Mechanics of the cell (p 608). New York: Cambridge University Press.
Mayergoyz, I. D. (2003). Mathematical models of hysteresis and their applications (2nd ed.). New York: Elsevier Science.
Lakes, R. S. (2009). Viscoelastic materials (p. 461). New York: Cambridge University Press.
Jameela, S. R., Suma, N., & Jayakrishnan, A. (1997). Protein release from poly(epsilon-caprolactone) microspheres prepared by melt encapsulation and solvent evaporation techniques: A comparative study. Journal of Biomaterials Science, 8(6), 457–466.
Murphy, C. M., & O’Brien, F. J. (2010). Understanding the effect of mean pore size on cell activity in collagen-glycosaminoglycan scaffolds. Cell Adhesion and Migration, 4(3), 377–381.
Karageorgiou, V., & Kaplan, D. (2005). Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials, 26(27), 5474–5491.
Kweon, H., Yoo, M. K., Park, I. K., Kim, T. H., Lee, H. C., Lee, H. S., et al. (2003). A novel degradable polycaprolactone networks for tissue engineering. Biomaterials, 24(5), 801–808.
Gloria, A., Russo, T., D’Amora, U., Zeppetelli, S., D’Alessandro, T., Sandri, M., et al. (2013). Magnetic poly(ε-caprolactone)/iron-doped hydroxyapatite nanocomposite substrates for advanced bone tissue engineering. Journal of the Royal Society Interface, 10(80), 20120833.
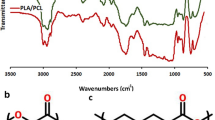
Elzein, T., Nasser-Eddine, M., Delaite, C., Bistac, S., & Dumas, P. (2004). FTIR study of polycaprolactone chain organization at interfaces. Journal of Colloid and Interface Science, 273(2), 381–387.
Tahriri, M., & Moztarzadeh, F. (2014). Preparation, characterization, and in vitro biological evaluation of PLGA/nano-fluorohydroxyapatite (FHA) microsphere-sintered scaffolds for biomedical applications. Applied Biochemistry and Biotechnology, 172(5), 2465–2479.
Wang, Y., Rodriguez-Perez, M. A., Reis, R. L., & Mano, J. F. (2005). Thermal and thermomechanical behaviour of polycaprolactone and starch/polycaprolactone blends for biomedical applications. Macromolecular Materials and Engineering, 290(8), 792–801.
Alvarez, K., & Nakajima, H. (2009). Metallic scaffolds for bone regeneration. Materials, 2(3), 790–832.
Borden, M., El-Amin, S. F., Attawia, M., & Laurencin, C. T. (2003). Structural and human cellular assessment of a novel microsphere-based tissue engineered scaffold for bone repair. Biomaterials, 24(4), 597–609.
Deligianni, D. D., Maris, A., & Missirlis, Y. F. (1994). Stress relaxation behaviour of trabecular bone specimens. Journal of Biomechanics, 27(12), 1469–1476.
Goto, T., Sasaki, N., & Hikichi, K. (1999). Early stage-stress relaxation in compact bone. Journal of Biomechanics, 32(1), 93–97.
Sethuraman, V., Makornkaewkeyoon, K., Khalf, A., & Madihally, S. V. (2013). Influence of scaffold forming techniques on stress relaxation behavior of polycaprolactone scaffolds. Journal of Applied Polymer Science, 130(6), 4237–4244.
Oskui, I. Z., & Hashemi, A. (2016). Dynamic tensile properties of bovine periodontal ligament. Journal of Biomechanics, 49(5), 756–764.
Rho, J. Y., Ashman, R. B., & Turner, C. H. (1993). Young’s modulus of trabecular and cortical bone material: ultrasonic and microtensile measurements. Journal of Biomechanics, 26(2), 111–119.
Reilly, D. T., Burstein, A. H., & Frankel, V. H. (1974). The elastic modulus for bone. Journal of Biomechanics, 7(3), 271–275.
Garner, E., Lakes, R., Lee, T., Swan, C., & Brand, R. (2000). Viscoelastic dissipation in compact bone: implications for stress-induced fluid flow in bone. Journal of Biomechanical Engineering, 122(2), 166–172.
Donnelly, E., Williams, R. M., Downs, S. A., Dickinson, M. E., Baker, S. P., & van der Meulen, M. C. H. (2006). Quasistatic and dynamic nanomechanical properties of cancellous bone tissue relate to collagen content and organization. Journal of Materials Research, 21(08), 2106–2117.
Boccaccini, A. R., & Maquet, V. (2003). Bioresorbable and bioactive polymer/Bioglass® composites with tailored pore structure for tissue engineering applications. Composites Science and Technology, 63(16), 2417–2429.
Lam, C. X. F., Teoh, S. H., & Hutmacher, D. W. (2007). Comparison of the degradation of polycaprolactone and polycaprolactone–(β-tricalcium phosphate) scaffolds in alkaline medium. Polymer International, 56(6), 718–728.
Lebourg, M., Sabater Serra, R., Mas Estelles, J., Hernandez Sanchez, F., Gomez Ribelles, J. L., & Suay Anton, J. (2008). Biodegradable polycaprolactone scaffold with controlled porosity obtained by modified particle-leaching technique. Journal of Materials Science, 19(5), 2047–2053.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
There is no funding or support.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Shahin-Shamsabadi, A., Hashemi, A. & Tahriri, M. A Viscoelastic Study of Poly(ε-Caprolactone) Microsphere Sintered Bone Tissue Engineering Scaffold. J. Med. Biol. Eng. 38, 359–369 (2018). https://doi.org/10.1007/s40846-017-0325-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-017-0325-2