Abstract
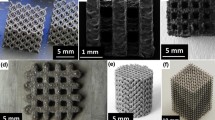
We elucidate here the process-structure-property relationships in three-dimensional (3D) implantable titanium alloy biomaterials processed by electron beam melting (EBM) that is based on the principle of additive manufacturing. The conventional methods for processing of biomedical devices including freeze casting and sintering are limited because of the difficulties in adaptation at the host site and difference in the micro/macrostructure, mechanical, and physical properties with the host tissue. In this regard, EBM has a unique advantage of processing patient-specific complex designs, which can be either obtained from the computed tomography (CT) scan of the defect site or through a computeraided design (CAD) program. This review introduces and summarizes the evolution and underlying reasons that have motivated 3D printing of scaffolds for tissue regeneration. The overview comprises of two parts for obtaining ultimate functionalities. The first part focuses on obtaining the ultimate functionalities in terms of mechanical properties of 3D titanium alloy scaffolds fabricated by EBM with different characteristics based on design, unit cell, processing parameters, scan speed, porosity, and heat treatment. The second part focuses on the advancement of enhancing biological responses of these 3D scaffolds and the influence of surface modification on cell-material interactions. The overview concludes with a discussion on the clinical trials of these 3D porous scaffolds illustrating their potential in meeting the current needs of the biomedical industry.
摘要
摘要本文综述了电子束增材制造法(EBM)制备医用钛合金多孔支架植入物的工艺-结构-性能之间关系. 传统加工多孔材料方法(如冷冻铸造及烧结法)制备的多孔植入器械由于很难匹配患病部位以及与人体组织在宏微观结构、 力学和物理性能存在差异等因素受到很多限制. 针对这一问题, EBM方法具有独特的优势. 它可以利用患病部位的CT扫描成像或者CAD程序设计制备出复杂个性化多孔植入器械. 本文概述了用于组织再生3D打印多孔支架的发展历程, 主要包含两部分: 第一部分介绍了EBM法制备的具有不同特征(设计、 结构单元、 加工参数、 扫描速率、 孔隙率及热处理)钛合金多孔支架的力学性能; 第二部分介绍了多孔支架生物响应的改进优化以及表面改性对细胞-材料交互作用的研究进展. 最后, 本文还讨论了三维多孔钛合金支架的临床试验结果, 并展望了其在生物医疗领域的应用前景.
Similar content being viewed by others
References
Kumar A, Nune KC, Murr LE, et al. Biocompatibility and mechanical behaviour of three-dimensional scaffolds for biomedical devices: process–structure–property paradigm. Int Mater Rev, 2016, 61: 20–45
Schubert C, van Langeveld MC, Donoso LA. Innovations in 3D printing: a 3D overview from optics to organs. Br J Ophthalmol, 2014, 98: 159–161
Simancik F. Introduction: the strange world of cellular metals. In: Degischer HP, Kriszt B (Eds). Handbook of cellular metals. Weinheim: Wiley-VCH Verlag, 2002, 1–4
Weber JN, White EW. Carbon-metal graded composites for permanent osseous attachment of non-porous metals. Mater Res Bull, 1972, 7: 1005–1016
Klawitter JJ, Weinstein AM. The status of porous materials to obtain direct skeletal attachment by tissue ingrowth. Acta Orthop Belg 1974, 40: 755–765
White EW, Weber JN, Roy DM, et al. Replamineform porous biomaterials for hard tissue implant applications. J Biomed Mater Res, 1975, 9: 23–27
Spector M, Michno MJ, Smarook WH, et al. A high-modulus polymer for porous orthopedic implants: Biomechanical compatibility of porous implants. J Biomed Mater Res, 1978, 12: 665–677
Klawitter JJ, Bagwell JG, Weinstein AM, et al. An evaluation of bone growth into porous high density polyethylene. J Biomed Mater Res, 1976, 10: 311–323
Cestero HJ, Salyer KE, Toranto IR. Bone growth into porous carbon, polyethylene, and polypropylene prostheses. J Biomed Mater Res, 1975, 9: 1–7
Homsy CA, Cain TE, Kessler FB, et al. Porous implant systems for prosthesis stabilization. Clin Orthop, 1972, 89: 220–235
Sauer BW, Weinstein AM, Klawitter JJ, et al. The role of porous polymeric materials in prosthesis attachment. J Biomed Mater Res, 1974, 8: 145–153
Hirschhorn J, McBeath A, Dustoor M. Porous titanium surgical implant materials. J Biomed Mater Res Symp, 1971, 2: 49–67
Galante J, Rostoker W, Lueck R, et al. Sintered fiber metal composites as a basis for attachment of implants to bone. J Bone Joint Surgery, 1971, 53: 101–114
Hahn H, Palich W. Preliminary evaluation of porous metal surfaced titanium for orthopedic implants. J Biomed Mater Res, 1970, 4: 571–577
Karagienes M. Porous metals as a hard tissue substitute. I. Biomedical aspects. Biomater Med Dev Artif Organs, 1973: 171–181
Ryan G, Pandit A, Apatsidis DP. Fabrication methods of porous metals for use in orthopaedic applications. Biomaterials, 2006, 27: 2651–2670
Brunette DM, Tengvall P, Textor M, et al. Titanium in medicine: materials science, surface science, engineering, biological responses and medical applications. Berlin: Springer, 2001
Karageorgiou V, Kaplan D. Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials, 2005, 26: 5474–5491
Bobyn JD, Stackpool GJ, Hacking SA, et al. Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surgery, 1999, 81: 907–914
Hacking SA, Bobyn JD, Toh KK, et al. Fibrous tissue ingrowth and attachment to porous tantalum. J Biomed Mater Res, 2000, 52: 631–638
Bobyn JD, Pilliar RM, Binnington AG, et al. The effect of proximally and fully porous-coated canine hip stem design on bone modeling. J Orthop Res, 1987, 5: 393–408
Bronzino JD (Ed), The Biomedical Engineering Handbook, Vol. 1, Boca Raton: CRC Press, 2000
Lemmons JE. Inorganic-organic combinations for bone repair. In: Christel P, Meumier A, Lee AJC (Eds). Biological and Biomechanical Performance of Biomaterials. Amsterdam: Elsevier, 1986, 51–57
Yang S, Leong KF, Du Z, et al. The design of scaffolds for use in tissue engineering. Part I. Traditional factors. Tissue Eng, 2001, 7: 679–689
Niinomi M. Mechanical biocompatibilities of titanium alloys for biomedical applications. J Mech Behav BioMed Mater, 2008, 1: 30–42
Heinl P, Müller L, Körner C, et al. Cellular Ti–6Al–4V structures with interconnected macro porosity for bone implants fabricated by selective electron beam melting. Acta Biomater, 2008, 4: 1536–1544
Murr LE, Gaytan SM, Medina F, et al. Additive layered manufacturing of reticulated Ti-6Al-4V biomedical mesh structures by electron beam melting. In: McGoron AJ, Li CZ, Lin WC (Eds). Proceedings of 25th Southern Biomedical Engineering Conference, ICFMBE Proceedings, Heidelberg: Springer, 2009, 24: 23–28
Murr LE, Gaytan SM, Martinez E, et al. Next generation orthopaedic implants by additive manufacturing using electron beam melting. Int J Biomater, 2012, 2012: 1–14
Coelho PG, Hollister SJ, Flanagan CL, et al. Bioresorbable scaffolds for bone tissue engineering: optimal design, fabrication, mechanical testing and scale-size effects analysis. Med Eng Phys, 2015, 37: 287–296
Klammert U, Gbureck U, Vorndran E, et al. 3D powder printed calcium phosphate implants for reconstruction of cranial and maxillofacial defects. J Cranio-Maxillofacial Surgery, 2010, 38: 565–570
Wang J, Yang M, Zhu Y, et al. Phage nanofibers induce vascularized osteogenesis in 3D printed bone scaffolds. Adv Mater, 2014, 26: 4961–4966
Zhao S, Zhu M, Zhang J, et al. Three dimensionally printed mesoporous bioactive glass and poly(3-hydroxybutyrate-co-3-hydroxyhexanoate) composite scaffolds for bone regeneration. J Mater Chem B, 2014, 2: 6106–6118
Jones AC, Milthorpe B, Averdunk H, et al. Analysis of 3D bone ingrowth into polymer scaffolds via micro-computed tomography imaging. Biomaterials, 2004, 25: 4947–4954
Silva GA, Coutinho OP, Ducheyne P, et al. Materials in particulate form for tissue engineering. 2. Applications in bone. J Tissue Eng Regen Med, 2007, 1: 97–109
Baker BM, Chen CS. Deconstructing the third dimension—how 3D culture microenvironments alter cellular cues. J Cell Sci, 2012, 125: 3015–3024
Guvendiren M, Burdick JA. Engineering synthetic hydrogel microenvironments to instruct stem cells. Curr Opin Biotech, 2013, 24: 841–846
Kraehenbuehl TP, Langer R, Ferreira LS. Three-dimensional biomaterials for the study of human pluripotent stem cells. Nat Meth, 2011, 8: 731–736
Hutmacher DW. Biomaterials offer cancer research the third dimension. Nat Mater, 2010, 9: 90–93
Guo B, Lei B, Li P, et al. Functionalized scaffolds to enhance tissue regeneration. Regenerative Biomaterials, 2015, 2: 47–57
Dawson JI, Oreffo ROC. Bridging the regeneration gap: stem cells, biomaterials and clinical translation in bone tissue engineering. Archives Biochem Biophys, 2008, 473: 124–131
Kolk A, Handschel J, Drescher W, et al. Current trends and future perspectives of bone substitute materials—From space holders to innovative biomaterials. J Cranio-Maxillofacial Surgery, 2012, 40: 706–718
Place ES, Evans ND, Stevens MM. Complexity in biomaterials for tissue engineering. Nat Mater, 2009, 8: 457–470
Ebrahimkhani MR, Young CL, Lauffenburger DA, et al. Approaches to in vitro tissue regeneration with application for human disease modeling and drug development. Drug Discovery Today, 2014, 19: 754–762
Engler AJ, Sen S, Sweeney HL, et al. Matrix elasticity directs stem cell lineage specification. Cell, 2006, 126: 677–689
Pelham RJ, Wang YL. Cell locomotion and focal adhesions are regulated by substrate flexibility. Proc Natl Acad Sci USA, 1997, 94: 13661–13665
Engelmayr GC, Cheng M, Bettinger CJ, et al. Accordion-like honeycombs for tissue engineering of cardiac anisotropy. Nat Mater, 2008, 7: 1003–1010
Roy TD, Simon JL, Ricci JL, et al. Performance of degradable composite bone repair products made via three-dimensional fabrication techniques. J Biomed Mater Res, 2003, 66A: 283–291
Chu TMG, Orton DG, Hollister SJ, et al. Mechanical and in vivo performance of hydroxyapatite implants with controlled architectures. Biomaterials, 2002, 23: 1283–1293
Kujala S, Ryhänen J, Danilov A, et al. Effect of porosity on the osteointegration and bone ingrowth of a weight-bearing nickel–titanium bone graft substitute. Biomaterials, 2003, 24: 4691–4697
Jin QM, Takita H, Kohgo T, et al. Effects of geometry of hydroxyapatite as a cell substratum in BMP-induced ectopic bone formation. J Biomed Mater Res, 2000, 52: 841–851
Koffler J, Kaufman-Francis K, Shandalov Y, et al. Improved vascular organization enhances functional integration of engineered skeletal muscle grafts. Proc Natl Acad Sci USA, 2011, 108: 14789–14794
Hollister SJ. Porous scaffold design for tissue engineering. Nat Mater, 2005, 4: 518–524
Hardy JG, Cornelison RC, Sukhavasi RC, et al. Electroactive tissue scaffolds with aligned pores as instructive platforms for biomimetic tissue engineering. Bioengineering, 2015, 2: 15–34
Kumar A, Nune KC, Misra R. Understanding the response of pulsed electric field on osteoblast functions in three-dimensional mesh structures. J Biomater Appl, 2016, 31: 594–605
Kumar A, Nune KC, Misra RDK. Electric field-mediated growth of osteoblasts—the significant impact of dynamic flow of medium. Biomater Sci, 2016, 4: 136–144
Pirvu T, Blanquer SBG, Benneker LM, et al. A combined biomaterial and cellular approach for annulus fibrosus rupture repair. Biomaterials, 2015, 42: 11–19
Kim DG, Huja SS, Tee BC, et al. Bone ingrowth and initial stability of titanium and porous tantalum dental implants. ImPlant Dentistry, 2013, 22: 399–405
Hutmacher DW. Scaffolds in tissue engineering bone and cartilage. Biomaterials, 2000, 21: 2529–2543
Kiran S, Nune KC, Misra RDK. The significance of grafting collagen on polycaprolactone composite scaffolds: processingstructure-functional property relationship. J Biomed Mater Res, 2015, 103: 2919–2931
Sachlos E, Czernuszka J. Making tissue engineering scaffolds work. Review: the application of solid freeform fabrication technology to the production of tissue engineering scaffolds. Euro Cell Mater, 2003, 5: 29–39
Liu YJ, Li SJ, Wang HL, et al. Microstructure, defects and mechanical behavior of beta-type titanium porous structures manufactured by electron beam melting and selective laser melting. Acta Mater, 2016, 113: 56–67
Murr LE, Quinones SA, Gaytan SM, et al. Microstructure and mechanical behavior of Ti–6Al–4V produced by rapid-layer manufacturing, for biomedical applications. J Mech Behav BioMed Mater, 2009, 2: 20–32
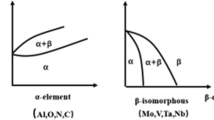
Hernandez J, Li SJ, Martinez E, et al. Microstructures and hardness properties for β-phase Ti–24Nb–4Zr–7.9Sn alloy fabricated by electron beam melting. J Mater Sci Tech, 2013, 29: 1011–1017
Gaytan SM, Murr LE, Martinez E, et al. Comparison of microstructures and mechanical properties for solid and mesh cobaltbase alloy prototypes fabricated by electron beam melting. Metall Mat Trans A, 2010, 41: 3216–3227
Hao YL, Li SJ, Yang R. Biomedical titanium alloys and their additive manufacturing. Rare Met, 2016, 35: 661–671
Leukers B, Gülkan H, Irsen SH, et al. Biocompatibility of ceramic scaffolds for bone replacement made by 3D printing. Mat-wiss u Werkstofftech, 2005, 36: 781–787
Oliveira JM, Rodrigues MT, Silva SS, et al. Novel hydroxyapatite/chitosan bilayered scaffold for osteochondral tissue-engineering applications: Scaffold design and its performance when seeded with goat bone marrow stromal cells. Biomaterials, 2006, 27: 6123–6137
Freed LE, Vunjak-Novakovic G, Biron RJ, et al. Biodegradable polymer scaffolds for tissue engineering. Nat Biotechnol, 1994, 12: 689–693
Hench L, Wilson J. An Introduction to Bioceramics. Singapore: World Scientific, 1993
Simske SJ, Ayers RA, Bateman TA. Porous materials for bone engineering. MSF, 1997, 250: 151–182
Liulan L, Aili T, Huicun Z, et al. The mechanical properties of bone tissue engineering scaffold fabricating via selective laser sintering. Life System Modeling and Simulation, 2007, 4689: 146–152
Bignon A, Chouteau J, Chevalier J, et al. Effect of micro-and macroporosity of bone substitutes on their mechanical properties and cellular response. J Mater Sci-Mater Med, 2003, 14: 1089–1097
Chantarapanich N, Puttawibul P, Sucharitpwatskul S, et al. Scaffold library for tissue engineering: a geometric evaluation. Comp Math Methods Med, 2012, 2012: 1–14
Richart O, Descamps M, Liebetrau A, et al. Preparation and mechanical characterization of hydroxyapatite monodispersed macroporous structure. Influence of interconnection and macropores diameters. KEM, 2002, 218–220: 9–12
Zhao S, Li SJ, Hou WT, et al. The influence of cell morphology on the compressive fatigue behavior of Ti-6Al-4V meshes fabricated by electron beam melting. J Mech Behav BioMed Mater, 2016, 59: 251–264
Liu YJ, Wang HL, Li SJ, et al. Compressive and fatigue behavior of beta-type titanium porous structures fabricated by electron beam melting. Acta Mater, 2017, 126: 58–66
Liu Y, Li S, Hou W, et al. Electron beam melted beta-type Ti–24Nb–4Zr–8Sn porous structures with high strength-to-modulus ratio. J Mater Sci Tech, 2016, 32: 505–508
Weibmann V, Drescher P, Bader R, et al. Comparison of single Ti6Al4V struts made using selective laser melting and electron beam melting subject to part orientation. Metals, 2017, 7: 91
Suard M, Martin G, Lhuissier P, et al. Mechanical equivalent diameter of single struts for the stiffness prediction of lattice structures produced by Electron Beam Melting. Additive Manufacturing, 2015, 8: 124–131
Pompe W, Worch H, Epple M, et al. Functionally graded materials for biomedical applications. Mater Sci Eng-A, 2003, 362: 40–60
Miao X, Sun D. Graded/gradient porous biomaterials. Materials, 2010, 3: 26–47
Li S, Zhao S, Hou W, et al. Functionally graded Ti-6Al-4V meshes with high strength and energy absorption. Adv Eng Mater, 2016, 18: 34–38
Hooreweder BV, Lietaert K, Neirinck B, et al. CoCr F75 scaffolds produced by additive manufacturing: Influence of chemical etching on powder removal and mechanical performance. J Mech Behav BioMed Mater, 2017, 70: 60–67
Van Hooreweder B, Apers Y, Lietaert K, et al. Improving the fatigue performance of porous metallic biomaterials produced by selective laser melting. Acta Biomater, 2017, 47: 193–202
Liu YJ, Li SJ, Wang HL, et al. Microstructure, defects and mechanical behavior of beta-type titanium porous structures manufactured by electron beam melting and selective laser melting. Acta Mater, 2016, 113: 56–67
Pyka G, Burakowski A, Kerckhofs G, et al. Surface modification of Ti6Al4V open porous structures produced by additive manufacturing. Adv Eng Mater, 2012, 14: 363–370
Liu X, Chu P, Ding C. Surface modification of titanium, titanium alloys, and related materials for biomedical applications. Mater Sci Eng-R-Rep, 2004, 47: 49–121
Mendes VC, Moineddin R, Davies JE. The effect of discrete calcium phosphate nanocrystals on bone-bonding to titanium surfaces. Biomaterials, 2007, 28: 4748–4755
Ajami E, Mahno E, Mendes VC, et al. Bone healing and the effect of implant surface topography on osteoconduction in hyperglycemia. Acta Biomater, 2014, 10: 394–405
Davies JE, Ajami E, Moineddin R, et al. The roles of different scale ranges of surface implant topography on the stability of the bone/implant interface. Biomaterials, 2013, 34: 3535–3546
Nune KC, Misra RDK, Li SJ, et al. The functional response of bioactive titania-modified three-dimensional Ti-6Al-4V mesh structure toward providing a favorable pathway for intercellular communication and osteoincorporation. J Biomed Mater Res, 2016, 104: 2488–2501
Nune KC, Misra RDK, Gai X, et al. The role of surface nanotopography on enhanced bioactivity and osteoconductive potential of anodized 3D printed Ti-6Al-4V alloy mesh structure. Coll Surf B: Biointerfaces, 2017. In press
Karaji ZG, Hedayati R, Pouran B, et al. Effects of plasma electrolytic oxidation process on the mechanical properties of additively manufactured porous biomaterials. Mat Sci Eng C, 2017, 76: 406–416
Amin Yavari S, Ahmadi SM, van der Stok J, et al. Effects of biofunctionalizing surface treatments on the mechanical behavior of open porous titanium biomaterials. J Mech Behav BioMed Mater, 2014, 36: 109–119
Nune KC, Misra RDK, Gaytan SM, et al. Biological response of next-generation of 3D Ti-6Al-4V biomedical devices using additive manufacturing of cellular and functional mesh structures. J Biomater Tissue Eng, 2014, 4: 755–771
Nune KC, Misra RDK, Gaytan SM, et al. Interplay between cellular activity and three-dimensional scaffold-cell constructs with different foam structure processed by electron beam melting. J Biomed Mater Res, 2015, 103: 1677–1692
Oh SH, Park IK, Kim JM, et al. In vitro and in vivo characteristics of PCL scaffolds with pore size gradient fabricated by a centrifugation method. Biomaterials, 2007, 28: 1664–1671
Klawitter JJ, Hulbert SF. Application of porous ceramics for the attachment of load bearing internal orthopedic applications. J Biomed Mater Res, 1971, 5: 161–229
Griffon DJ, Sedighi MR, Schaeffer DV, et al. Chitosan scaffolds: interconnective pore size and cartilage engineering. Acta Biomater, 2006, 2: 313–320
Zardiackas LD, Parsell DE, Dillon LD, et al. Structure, metallurgy, and mechanical properties of a porous tantalum foam. J Biomed Mater Res, 2001, 58: 180–187
Nune KC, Kumar A, Misra RDK, et al. Osteoblast functions in functionally graded Ti-6Al-4 V mesh structures. J Biomater Appl, 2016, 30: 1182–1204
Nune KC, Kumar A, Misra RDK, et al. Functional response of osteoblasts in functionally gradient titanium alloy mesh arrays processed by 3D additive manufacturing. Colloids Surfs BBiointerfaces, 2017, 150: 78–88
Ponader S, Vairaktaris E, Heinl P, et al. Effects of topographical surface modifications of electron beam melted Ti-6Al-4V titanium on human fetal osteoblasts. J Biomed Mater Res, 2008, 84A: 1111–1119
Rapuano BE, Lee JJE, MacDonald DE. Titanium alloy surface oxide modulates the conformation of adsorbed fibronectin to enhance its binding to α5β1 integrins in osteoblasts. Eur J Oral Sci, 2012, 120: 185–194
Trivedi P, gupta P, Srivastava S, et al. Characterization and in vitro biocompatibility study of Ti–Si–N nanocomposite coatings developed by using physical vapor deposition. Appl Surf Sci, 2014, 293: 143–150
Brammer KS, Oh S, Cobb CJ, et al. Improved bone-forming functionality on diameter-controlled TiO2 nanotube surface. Acta Biomater, 2009, 5: 3215–3223
Trivedi P, Patel AK, Maurya R, et al. Nanomechanical characterization and protein adsorption of cold-rolled zirconium alloy. JOM, 2015, 67: 726–732
Xu JY, Chen XS, Zhang CY, et al. Improved bioactivity of selective laser melting titanium: Surface modification with micro-/nano-textured hierarchical topography and bone regeneration performance evaluation. Mater Sci Eng-C, 2016, 68: 229–240
Tay CY, Irvine SA, Boey FYC, et al. Micro-/nano-engineered cellular responses for soft tissue engineering and biomedical applications. Small, 2011, 7: 1361–1378
Gittens RA, McLachlan T, Olivares-Navarrete R, et al. The effects of combined micron-/submicron-scale surface roughness and nanoscale features on cell proliferation and differentiation. Biomaterials, 2011, 32: 3395–3403
Zhao L, Mei S, Chu PK, et al. The influence of hierarchical hybrid micro/nano-textured titanium surface with titania nanotubes on osteoblast functions. Biomaterials, 2010, 31: 5072–5082
Zhao L, Liu L, Wu Z, et al. Effects of micropitted/nanotubular titania topographies on bone mesenchymal stem cell osteogenic differentiation. Biomaterials, 2012, 33: 2629–2641
Kubo K, Tsukimura N, Iwasa F, et al. Cellular behavior on TiO2 nanonodular structures in a micro-to-nanoscale hierarchy model. Biomaterials, 2009, 30: 5319–5329
Zhuang XM, Zhou B, Ouyang JL, et al. Enhanced MC3T3-E1 preosteoblast response and bone formation on the addition of nano-needle and nano-porous features to microtopographical titanium surfaces. Biomed Mater, 2014, 9: 045001
Wang W, Zhao L, Wu K, et al. The role of integrin-linked kinase/β-catenin pathway in the enhanced MG63 differentiation by micro/nano-textured topography. Biomaterials, 2013, 34: 631–640
Brammer KS, Frandsen CJ, Jin S. TiO2 nanotubes for bone regeneration. Trends Biotech, 2012, 30: 315–322
Liu XH, Wu L, Ai HJ, et al. Cytocompatibility and early osseointegration of nanoTiO2-modified Ti-24Nb-4Zr-7.9Sn surfaces. Mater Sci Eng-C, 2015, 48: 256–262
Ma XY, Feng YF, Ma ZS, et al. The promotion of osteointegration under diabetic conditions using chitosan/hydroxyapatite composite coating on porous titanium surfaces. Biomaterials, 2014, 35: 7259–7270
Wang L, Hu X, Ma X, et al. Promotion of osteointegration under diabetic conditions by tantalum coating-based surface modification on 3-dimensional printed porous titanium implants. Colloids Surfs B-Biointerfaces, 2016, 148: 440–452
Javed F, Romanos GE. Impact of diabetes mellitus and glycemic control on the osseointegration of dental implants: a systematic literature review. J Periodontology, 2009, 80: 1719–1730
Tamam E, Turkyilmaz I. Effects of pH and elevated glucose levels on the electrochemical behavior of dental implants. J Oral Im-Plantology, 2014, 40: 153–159
Maló P, de Araújo Nobre M, Gonçalves Y, et al. Long-term outcome of implant rehabilitations in patients with systemic disorders and smoking habits: a retrospective clinical study. Clinical ImPlant Dentistry Related Res, 2016, 18: 649–665
Feng YF, Wang L, Zhang Y, et al. Effect of reactive oxygen species overproduction on osteogenesis of porous titanium implant in the present of diabetes mellitus. Biomaterials, 2013, 34: 2234–2243
Trivedi P, Nune KC, Misra RDK. Grain structure dependent selfassembled bioactive coating on Mg-2Zn-2Gd alloy: Mechanism of degradation at biointerfaces. Surf Coatings Tech, 2017, 315: 250–257
Morscher EW, Hefti A, Aebi U. Severe osteolysis after third-body wear due to hydroxyapatite particles from acetabular cup coating. J Bone Joint Surgery, 1998, 80: 267–272
Røkkum M, Reigstad A, Johansson CB. HA particles can be released from well-fixed HA-coated stems. Acta Orthopaedica Scandinavica, 2002, 73: 298–306
Nune KC, Kumar A, Murr LE, et al. Interplay between self-assembled structure of bone morphogenetic protein-2 (BMP-2) and osteoblast functions in three-dimensional titanium alloy scaffolds: Stimulation of osteogenic activity. J Biomed Mater Res, 2016, 104: 517–532
Kumar A, Nune KC, Misra RDK. Biological functionality and mechanistic contribution of extracellular matrix-ornamented three dimensional Ti-6Al-4V mesh scaffolds. J Biomed Mater Res, 2016, 104: 2751–2763
Liu H, Li W, Liu C, et al. Incorporating simvastatin/poloxamer 407 hydrogel into 3D-printed porous Ti6Al4 V scaffolds for the promotion of angiogenesis, osseointegration and bone ingrowth. Biofabrication, 2016, 8: 045012
Murr LE, Gaytan SM, Medina F, et al. Next-generation biomedical implants using additive manufacturing of complex, cellular and functional mesh arrays. Philos Trans R Soc A-Math Phys Eng Sci, 2010, 368: 1999–2032
Torres J, Tamimi F, Alkhraisat MH, et al. Vertical bone augmentation with 3D-synthetic monetite blocks in the rabbit calvaria. J Clin Periodontol, 2011, 38: 1147–1153
Wu BM, Borland SW, Giordano RA, et al. Solid free-form fabrication of drug delivery devices. J Control Release, 1996, 40: 77–87
Katstra WE, Palazzolo RD, Rowe CW, et al. Oral dosage forms fabricated by Three Dimensional Printing™. J Control Release, 2000, 66: 1–9
Wu W, Zheng Q, Guo X, et al. The controlled-releasing drug implant based on the three dimensional printing technology: Fabrication and properties of drug releasing in vivo. J Wuhan Univ Technol-Mat Sci Edit, 2009, 24: 977–981
Yu DG, Zhu LM, Branford-White CJ, et al. Three-dimensional printing in pharmaceutics: promises and problems. J Pharmaceutical Sci, 2008, 97: 3666–3690
Kuboki Y, Jin Q, Takita H. Geometry of carriers controlling phenotypic expression in BMP-induced osteogenesis and chondrogenesis. J Bone Joint Surg, 2001, 83: S105–S115
Tsuruga E, Takita H, Itoh H, et al. Pore size of porous hydroxyapatite as the cell-substratum controls BMP-induced osteogenesis. J Biochem, 1997, 121: 317–324
Yarlagadda P, Chandrasekharan M, Shyan J. Recent advances and current developments in tissue scaffolding. Biomed Mater Eng, 2005, 15: 159–177
Carmeliet P. Mechanisms of angiogenesis and arteriogenesis.. Nat Med, 2000, 6: 389–395
Laschke MW, Harder Y, Amon M, et al. Angiogenesis in tissue engineering: breathing life into constructed tissue substitutes. Tissue Eng, 2006, 12: 2093–2104
Rouwkema J, Rivron NC, van Blitterswijk CA. Vascularization in tissue engineering. Trends Biotech, 2008, 26: 434–441
Malda J, Rouwkema J, Martens DE, et al. Oxygen gradients in tissue-engineered Pegt/Pbt cartilaginous constructs: Measurement and modeling. Biotechnol Bioeng, 2004, 86: 9–18
Folkman J. Self-regulation of growth in three dimensions. J Exp Med, 1973, 138: 745–753
Colton CK. Implantable biohybrid artificial organs. Cell Trans-Plantation, 1995, 4: 415–436
Carmeliet P, Jain RK. Angiogenesis in cancer and other diseases.. Nature, 2000, 407: 249–257
Kannan RY, Salacinski HJ, Sales K, et al. The roles of tissue engineering and vascularisation in the development of microvascular networks: a review. Biomaterials, 2005, 26: 1857–1875
Druecke D, Langer S, Lamme E, et al. Neovascularization of poly (ether ester) block-copolymer scaffolds in vivo: long-term investigations using intravital fluorescent microscopy. J Biomed Mater Res, 2004, 68A: 10–18
Hutmacher DW, Sittinger M, Risbud MV. Scaffold-based tissue engineering: rationale for computer-aided design and solid freeform fabrication systems. Trends Biotech, 2004, 22: 354–362
Novosel EC, Kleinhans C, Kluger PJ. Vascularization is the key challenge in tissue engineering. Adv Drug Deliver Rev, 2011, 63: 300–311
Liu WF, Chen CS. Engineering biomaterials to control cell function. Mater Today, 2005, 8: 28–35
Hutmacher DW. Scaffold design and fabrication technologies for engineering tissues—state of the art and future perspectives. J BioMater Sci Polymer Ed, 2001, 12: 107–124
Anderson CR, Ponce AM, Price RJ. Immunohistochemical identification of an extracellular matrix scaffold that microguides capillary sprouting in vivo. J Histochem Cytochem, 2004, 52: 1063–1072
Ochman S, Frey S, Raschke MJ, et al. Local application of VEGF compensates callus deficiency after acute soft tissue trauma-results using a limb-shortening distraction procedure in rabbit tibia. J Orthop Res, 2011, 29: 1093–1098
Trueta J, Little K. The vascular contribution to osteogenesis II. Studies with the electron microscope. J Bone Joint Surg Br, 1960, 42-B: 367–376
Bose S, Roy M, Bandyopadhyay A. Recent advances in bone tissue engineering scaffolds. Trends Biotech, 2012, 30: 546–554
Holder Jr. WD, Gruber HE, Roland WD, et al. Increased vascularization and heterogeneity of vascular structures occurring in polyglycolide matrices containing aortic endothelial cells implanted in the rat. Tissue Eng, 1997, 3: 149–160
Mooney DJ, Mikos AG. Growing new organs. Sci Am, 1999, 280: 60–65
Muller D, Chim H, Bader A, et al. Vascular guidance: microstructural scaffold patterning for inductive neovascularization. Stem Cells Int, 2011, 2011: 1–6
Prasad K, Bazaka O, Chua M, et al. Metallic biomaterials: current challenges and opportunities. Materials, 2017, 10: 884–917
Li S, Li X, Hou W, et al. Fabrication of open-cellular (porous) titanium alloy implants: osseointegration, vascularization and preliminary human trials. Sci China Mater, 2018, 61: 525–536
Fan H, Fu J, Li X, et al. Implantation of customized 3-D printed titanium prosthesis in limb salvage surgery: a case series and review of the literature. World J Surg Onc, 2015, 13: 308–317
Ponader S, von Wilmowsky C, Widenmayer M, et al. In vivo performance of selective electron beam-melted Ti-6Al-4V structures. J Biomed Mater Res, 2010, 92A: 56–62
Hollander DA, von Walter M, Wirtz T, et al. Structural, mechanical and in vitro characterization of individually structured Ti–6Al–4V produced by direct laser forming. Biomaterials, 2006, 27: 955–963
Van Bael S, Chai YC, Truscello S, et al. The effect of pore geometry on the in vitro biological behavior of human periosteumderived cells seeded on selective laser-melted Ti6Al4V bone scaffolds. Acta Biomater, 2012, 8: 2824–2834
Butscher A, Bohner M, Hofmann S, et al. Structural and material approaches to bone tissue engineering in powder-based threedimensional printing. Acta Biomater, 2011, 7: 907–920
Sobral JM, Caridade SG, Sousa RA, et al. Three-dimensional plotted scaffolds with controlled pore size gradients: effect of scaffold geometry on mechanical performance and cell seeding efficiency. Acta Biomater, 2011, 7: 1009–1018
Olivares-Navarrete R, Gittens RA, Schneider JM, et al. Osteoblasts exhibit a more differentiated phenotype and increased bone morphogenetic protein production on titanium alloy substrates than on poly-ether-ether-ketone. Spine J, 2012, 12: 265–272
Levchenko I, Ostrikov KK, Zheng J, et al. Scalable graphene production: perspectives and challenges of plasma applications. Nanoscale, 2016, 8: 10511–10527
Lethaus B, Kessler P, Boeckman R, et al. Reconstruction of a maxillary defect with a fibula graft and titanium mesh using CAD/CAM techniques. Head Face Med, 2010, 6: 16–19
Malhotra K, Sharma A, Giraddi G, et al. Versatility of titanium 3D plate in comparison with conventional titanium miniplate fixation for the management of mandibular fracture. J Maxillofac Oral Surg, 2012, 11: 284–290
Lee UL, Kwon JS, Woo SH, et al. Simultaneous bimaxillary surgery and mandibular reconstruction with a 3-dimensional printed titanium implant fabricated by electron beam melting: A preliminary mechanical testing of the printed mandible. J Oral Maxillofac Surg, 2016, 74: 1501
Acknowledgements
Nune KC and Misra RDK acknowledge support from the Department of Metallurgical, Materials and Biomedical Engineering, University of Texas at El Paso. All the authors acknowledge different reference sources that enabled the authors to prepare this overview article. The authors have done their best in citing all the relevant articles, however, inadvertently there may be situations where an article has not been appropriately cited. All figures adapted from different references and reference number is indicated in the figure caption. Li S greatly acknowledges support of the Key Research Program of Frontier Science, CAS (QYZDJ-SSW-JSC031-02)
Author information
Authors and Affiliations
Corresponding author
Additional information
Krishna Chaitanya Nune is a senior research scientist in the Department of Metallurgical, Materials and Biomedical Engineering, University of Texas at El Paso, USA. His research interests are in biomaterials.
Shujun Li is a tenured professor in Shenyang National Laboratory for Materials Science, Institute of Metal Research, Chinese Academy of Sciences. His current research interest focuses on additive manufacturing via electron beam melting technology, aiming to understand the structure-process-property relationship of 3D printable metallic materials and explore their practical applications in aerospace and biomedical components, etc.
R. Devesh Kumar Misra is a professor and Chair of the Department of Metallurgical, Materials and Biomedical Engineering, University of Texas at El Paso, USA. The research interests are in biomaterials, nanostructured materials, deformation and fracture, and additive manufacturing.
Rights and permissions
About this article
Cite this article
Nune, K.C., Li, S. & Misra, R.D.K. Advancements in three-dimensional titanium alloy mesh scaffolds fabricated by electron beam melting for biomedical devices: mechanical and biological aspects. Sci. China Mater. 61, 455–474 (2018). https://doi.org/10.1007/s40843-017-9134-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40843-017-9134-x