Abstract
Background
Gabapentinoids (GBP) and benzodiazepines (BZ) are commonly prescribed in older adults and their package inserts list edema and vertigo as adverse drug reactions. These adverse drug reactions may be treated with symptomatic drug therapies without discontinuing the culprit drugs or decreasing their dose, thereby initiating a prescribing cascade and often resulting in polypharmacy. Whether prescribing cascades occur in the treatment of edema and dizziness among Japanese patients treated with GBP and BZ has not been investigated, including treatment with mirogabalin, a class drug of GBP marketed in Japan.
Objective
We aimed to investigate prescribing cascades with GBP-induced and BZ-induced edema and dizziness treated with loop diuretics (LD) and anti-vertigo drugs (AVD), respectively, among older adults.
Methods
A prescription sequence symmetry analysis design was used to detect signals of prescribing cascades associated with edema and dizziness induced by GBP and BZ (exposure drugs). Loop diuretics and AVD were the outcome drugs used to identify prescribing cascades following the initiation of exposure drugs. The study population consisted of enrollees of a large-scale health claims database provided by DeSC Healthcare, Inc., between April 2014 and March 2021. Subjects eligible for a prescription sequence symmetry analysis were patients aged ≥ 65 years prescribed an outcome drug within 90 days before and after exposure drug initiation. A signal of a prescribing cascade was detected if secular trend-adjusted sequence ratios were statistically significant on comparison of the frequencies of outcome drug initiation before and after exposure drug initiation.
Results
We identified 2671 patients with prescriptions of a GBP-LD combination, 4009 with a GBP-AVD combination, 8675 with a BZ-LD combination, and 9462 with a BZ-AVD combination. The adjusted sequence ratios for GBP-LD and BZ-LD cascades were significantly larger than one (adjusted sequence ratio [95% confidence interval], 1.69 [1.56–1.83]; 1.35 [1.29–1.41], respectively), indicating positive signals of prescribing cascades. No signal was detected for the GBP-AVD or BZ-AVD cascade (0.89 [0.83–0.94]; 0.90 [0.87–0.94], respectively). The adjusted sequence ratio for the mirogabalin cascade was higher than that for pregabalin (2.23 [1.84–2.71] vs 1.59 [1.46–1.73]).
Conclusions
Our study provides good evidence that LD-prescribing cascades associated with edema would be a class effect of GBP and BZ. Edema emerging around 1 month after GBP initiation should be carefully differentiated from pathological edema, and undue LD prescription as a prescribing cascade should be avoided.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Adverse drug reactions may be mistakenly treated as the presentation of new conditions with additional drugs but without discontinuing the culprit drugs or decreasing their doses, constituting a prescribing cascade, a cause of polypharmacy. |
Prescription sequence symmetry analysis indicated that excessive use of loop diuretics occurred among older adult patients after initiation of benzodiazepines and gabapentinoids, confirming loop diuretic-prescribing cascades as representing potential class effects due to these drugs. |
The observed higher risk of a loop diuretic-prescribing cascade with mirogabalin, a newly marketed gabapentinoid class drug in Japan, compared with pregabalin warrants more attention. |
1 Introduction
Polypharmacy, commonly defined as the concomitant use of five or more drugs, has been associated with several healthcare problems, particularly in older adults. These include an increased risk of adverse drug reactions (ADRs), loss of efficacy due to reduced adherence to medication, and higher medical costs [1,2,3]. The Statistics of Medical Care Activities in Public Health Insurance issued by the government of Japan reported that 27.0% of older adults aged 65 years and older and 40.7% aged 75 years and older were taking five or more concomitant medications, and accordingly met the definition of polypharmacy [4, 5].
Prescribing cascades (PC), a known cause of polypharmacy [6], occur when a putative ADR emerging after the initiation of a drug is misinterpreted as a newly developed condition and treated with another medication, instead of by discontinuation or dose reduction of the culprit drug [7, 8]. More than 20 types of PC have been identified related to drugs used for chronic conditions, including heart disease, hypertension, obstructive pulmonary disease, diabetes mellitus, dementia, Parkinson’s disease, epilepsy, schizophrenia, major depression, and chronic pain [8,9,10,11]. Increased awareness of PCs among practitioners via the provision of evidence derived from research is crucial to prevention [7, 9, 12]. The risk of PCs appears high in older adults because they are more likely to receive multiple drug therapies for multiple chronic conditions, and because conditions associated with general aging processes can mask potential relationships between culprit drugs and ADRs [9].
A study among Japanese patients aged 65 years and older reported that the most frequently prescribed potentially inappropriate medications were analgesics and benzodiazepines (BZ) [13]. Gabapentinoids (GBP) are first-line drugs for neuropathic pain and have been increasingly prescribed worldwide, including off-label treatment for low back pain [14, 15]. Benzodiazepines are the most used hypnotic sedatives in Japan. [16] Dizziness and edema are listed as ADRs in the Japanese package inserts of GBP and BZ products [17,18,19]. These symptoms are common in older adults, however, and it is difficult to determine whether their occurrence is due to aging or ADRs. The risk of overlooking potential PCs associated with these symptoms is accordingly high.
A potential PC involving treatment drugs for dizziness after sedatives including BZ and GBP have been reported [20,21,22]. The PC of GBP-induced edema treated with loop diuretics (LD) has been well documented, whereas that of BZ has not [15, 22,23,24]. To date, mirogabalin, a newly marketed drug in the GBP class, has not been tested for PCs since its marketing authorization was granted recently in 2019, with the sole indication of neuropathy pain in Japan. The incidence of PCs may be influenced by a number of regional factors, including the national medical care system, available medical products and guidelines, awareness of side effects, and the intervention of pharmacists [24, 25]. However, studies on PCs in Japan remain scarce. Here, we investigated PCs initiated by GBP and BZ that prompted subsequent treatment of edema with LD and of dizziness with anti-vertigo drugs (AVD) among older patients using a large-scale claims database in Japan.
2 Materials and Methods
2.1 Design
The study was conducted using the prescription sequence symmetry analysis (PSSA) design to assess GBP-initiated and BZ-initiated PCs. The PSSA is a case-only design that includes only individuals who experience the outcome of interest, and has been used in many studies evaluating the presence of PCs and in pharmacovigilance activities [23, 26,27,28,29]. Its advantages include its simple design, efficient computation, and robustness against time-invariant confounding factors [30]. The PSSA assesses the relative timing of exposure drug initiation (denoting a medication suspected of causing an ADR) to outcome drug initiation (denoting a medication potentially used to treat the ADR) in a patient receiving incident prescription of both medications. The null hypothesis of PSSA is that there is no association between exposure and outcome drugs. When a PC occurs, the null hypothesis of PSSA is rejected, meaning that it is more (or less) likely that the outcome drug is prescribed after the exposure drug than before.
2.2 Data Source
We used a large-scale claims database provided by DeSC Healthcare Inc. (Tokyo, Japan). This database contains records of health insurance claims of inpatients and outpatients, pharmacy dispensing claims, and medical check-up data, and as of May 2021 covered 6.2 million individuals of all ages, curated from the following three types of public and private health insurance plans: corporate health insurance societies for employees and their dependents; the National Health Insurance for individuals aged < 75 years who are not covered by other public insurance plans; and the Latter-Stage Elderly Healthcare System for older adults aged 75 years and older. Claims data are irreversibly anonymized when retrieved from the insurers and transferred to the DeSC claims database. Individuals in the database can be tracked by a unique identifier annotated before anonymization, allowing their total healthcare utilization to be comprehensively followed, except for self-medication and self-care, unless they withdraw from their health insurance plan. Study data were available from 1 April, 2014 to 31 May, 2021. The following information was available and provided from the DeSC claims database to the study team via secure cloud transfer: patient demographics, including sex and date of birth; diagnoses coded according to the International Classification of Diseases, 10th Edition, and the domestic standard disease name master compatible with the International Classification of Diseases, 10th Edition; prescribed drugs coded according to the National Health Insurance Drug List; and medical procedures coded according to the Japanese national insurance fee schedule. This study was conducted for non-commercial purposes by an academic research organization, and individual consent to the collection and secondary use of existing personal health data was accordingly waived in accordance with the Japanese Privacy Protection Law. The study protocol was approved by the Ethics Committee for Research Involving Humans of Keio University Faculty of Pharmacy (No. 220406-2), and followed local ethical guidelines for biological and medical research involving human subjects.
2.3 Study Drugs
Gabapentinoids and BZ were the exposure drugs, and LD and AVD were the outcome drugs as proxies for the incidence of edema and dizziness, respectively. Gabapentinoids included pregabalin and mirogabalin, which have been marketed in Japan with the sole indication of neuropathic pain (Electronic Supplementary Material [ESM]). Gabapentin is not indicated for neuropathic pain but has been used only for the treatment of seizure in Japan and was therefore excluded from the study drugs because the characteristics and care of patients with seizure treated with gabapentin are completely different from those of patients treated with pregabalin and mirogabalin. Benzodiazepines under the study included all BZ hypnotics and sedatives, including oral and parenteral formulations indicated for insomnia and anesthesia in Japan (ESM). Loop diuretics included furosemide, azosemide, bumetanide, torsemide, and piretamide (ESM). Anti-vertigo drugs, the drugs indicated for dizziness, were selected from the drug database of the Japanese regulatory agency, the Pharmaceuticals and Medical Devices Agency [31], after excluding those antiemetics and sedatives that are not specific to the treatment of dizziness (ESM). All medications of interest were available to the insured under the universal national insurance scheme in Japan and are subsidized. With a few exceptions (ESM), the study medications were available in the market throughout the entire study period.
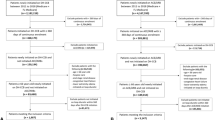
2.4 Study Population
The study cohort consisted of patients prescribed both an exposure drug and an incident outcome drug. We identified patients aged 65 years and older having continuous enrollment of 360 days or more in the study database before the date of first claim of the exposure drug. The date of first claim of the exposure drug defined cohort entry. A preceding 180-day look-back period was used to identify new users of the exposure drug by verifying the absence of preceding prescription claims of the exposure drug. A prescription claim for outcome drugs had to be found within a detection time window set before and after cohort entry (Fig. 1). In addition, a 180-day period without prescription records of an outcome drug prior to the detection time window for the outcome drugs was used to ensure incident prescription of the outcome drugs [28]. The 90-day period was primarily used for the detection time window of prescription claims of outcome drugs on the ground that outcome drugs prescribed beyond this window were unlikely to be related to ADRs caused by the exposure drug [32,33,34], and that time-varying confounders (e.g., worsening condition with aging) may generate false-positive signals if the detection window for outcome drug prescriptions were longer [35]. Patients who were prescribed both exposure and outcome drugs on the same date were excluded.
Tested drug pairs and observation days for detecting prescribing cascades. Exposure drug (e): an initial medication that potentially causes an adverse drug event (a) including gabapentinoid (GBP) and a benzodiazepine (BZ). Outcome drug (o): a new medication to treat effects caused by the first medication, including loop diuretics (LD) and anti-vertigo drugs (AVD). Bars represent days of detection time windows, which are set to detect prescriptions of outcome drugs (o) before and after the initiation date of exposure drug (e)
2.5 Statistical Analysis
The following patient characteristics were summarized with descriptive statistics: age, sex, major complications for which LD were indicated, including congestive heart failure (HF) and chronic kidney disease (CKD, ESM) [27, 36], and hospitalization in the month of cohort entry. There were no missing data in patient characteristics. No record of a prescription claim or a disease code in the study database was regarded as the absence of a drug prescription and a disease, respectively. Given that the PSSA requires patient use of both exposure and outcome drugs, the study patients for analysis possibly differed from the whole population of exposure drug initiators [27]. We therefore compared the characteristics of the study patients to the whole population of exposure drug initiators. We submitted all combinations of exposure and outcome drugs to PSSA, namely the four combinations of GBP-LD, GBP-AVD, BZ-LD, and BZ-AVD. Crude sequence ratios were calculated by dividing the number of outcome drug initiators after cohort entry by the number of outcome drug initiators before cohort entry. We calculated null-effect sequence ratios (NSRs) to adjust for secular trends in prescribing for the medication of interest (i.e., increase or decrease in prescriptions of exposure and outcome drugs during the study period; ESM) [35]. Adjusted sequence ratios (ASR) with 95% confidence intervals (CIs) were derived by dividing the crude sequence ratio by the NSR [37]. A lower limit of the 95% CI of ASR ≥1 indicated a positive signal of PCs with statistical significance.
Stratified analyses by the presence/absence of HF and CKD, and by drug of the exposure drug classes, were performed to assess the impact on the PC with a positive signal. Sensitivity analyses were performed to examine the robustness of the main results against different detection time windows, including 30 or 180 days. As this study was the first PSSA performed using the DeSC database, we preliminarily tested whether known PC signals and the absence of PC could be verified by PSSA in the study database. Specifically, the PC combinations of positive controls were angiotensin-converting enzyme inhibitors (ACEIs)-cough-antitussive, and calcium channel blockers (CCB)-edema-LD [27, 38]. Negative controls included angiotensin II receptor blockers (ARBs) or ACEIs-edema-LD, and CCB-cough-antitussives [27]. We also verified the combination of paracetamol (PRC)-AVD as a negative control for AVD cascade. Definitions of these drug codes are given in the ESM. All analyses were conducted using SAS Studio 3.8 (SAS 9.4; SAS Institute Inc., Cary, NC, USA).
3 Results
3.1 Validation of PSSA Using the DeSC Database
We identified 1273 ACEI-antitussive initiators and 5395 CCB-LD initiators eligible as PSSA-positive controls, and 6837 CCB-antitussive initiators, 6431 ACEI/ARB-LD initiators, and 15,925 PRC-AVD initiators eligible as negative controls. The patient groups of all combinations were aged around 80 years (mean age, 80.9 years for ACEI-antitussive; 82.3 years for CCB-LD; 78.4 years for CCB-antitussive; 81.9 for ACEI/ARB-LD; and 78.4 years for PRC-AVD), with more female individuals (ACEI-antitussive, 54.4%; CCB-LD, 56.4%; CCB-antitussive, 60.7%; ACEI/ARB-LD, 53.6%; and PRC-AVD, 61.1%) [ESM]. Using a 90-day time window, ASRs for all positive controls were significant whereas ASRs for all negative controls showed no signals (ESM). Sensitivity analyses using 30-day and 180-day time windows showed similar results, except for no signal for a 30-day ACEI-antitussive cascade.
3.2 Patient Characteristics for GBP and BZ Initiators
We identified 121,963 GBP initiators and 203,835 BZ initiators aged 65 years and older. Of these, 2671 GBP-LD initiators, 4009 GBP-AVD initiators, 8675 BZ-LD initiators, and 9462 BZ-AVD initiators were eligible for the PSSA (Figs. 2 and 3, Tables 1 and 2).
Compared with the whole GBP population, the GBP-LD initiators had a higher mean age (78.2 years vs 81.6 years, respectively), a higher percentage of inpatient prescriptions of GBP (7.2% vs 20.6%, respectively), and higher percentages of HF (32.9% vs 70.5%, respectively) and CKD (30.1% vs 48.4%, respectively) (Table 1). The GBP-AVD initiators had a higher percentage of inpatient prescriptions of GBP than the GBP whole population (7.2% vs 12.7%, respectively). Compared with the BZ whole population, the BZ-LD initiators had a higher mean age (78.7 years vs 81.4 years, respectively), fewer female individuals (55.9% vs 51.1%, respectively), a higher percentage of inpatient prescriptions of BZ (40.4% vs 77.0%, respectively), fewer prescriptions of midazolam (63.4% vs 56.6%, respectively), and higher percentages of HF (30.6% vs 76.1%, respectively) and CKD (23.9% vs 37.4%, respectively) (Table 2). The BZ-AVD initiators had a higher percentage of inpatient prescriptions of BZ than the BZ whole population (48.0% vs 40.4%, respectively).
3.3 PSSA
The results of PSSA are shown in Table 3. The NSRs were approximately 1.00 for all combinations. Significant positive signals of PCs were detected for GBP-LD and BZ-LD cascades, with ASRs of 1.69 (95% CI 1.56–1.83) and 1.35 (1.29–1.41), respectively. Loop diuretic prescriptions were most frequently found at 30 days after the GBP initiation and 10 days after the BZ initiation (Fig. 4a, c). No signal was detected for a GBP-AVD cascade (ASR [95% CI], 0.89 [0.83–0.94]) or a BZ-AVD cascade (0.90 [0.87–0.94]) (Table 3; Fig. 4b, d, respectively).
Frequency of outcome drug prescription relative to the exposure drug. The number of outcome drug initiators relative to the timing of exposure drug initiations for the 90-day time window is illustrated using a histogram with an x-axis in 10-day increments. AVD anti-vertigo drugs, BZ benzodiazepines, GBP gabapentinoids, LD loop diuretics
After the stratified analyses, the ASRs of the GBP-LD cascade were 1.62 (1.48–1.78) in patients with HF and 1.84 (1.58–2.13) in those without HF, and both remained significant. The ASRs were 1.57 (1.40–1.76) in patients with CKD and 1.81 (1.62–2.02) in those without CKD, and both again remained significant. The ASRs of the BZ-LD cascade stratified by the presence and absence of HF were 1.22 (1.16–1.28) and 1.90 (1.73–2.08), respectively, and both remained significant. The ASRs stratified by the presence and absence of CKD were 1.17 (1.10–1.26) and 1.47 (1.39–1.55), respectively, and both again remained significant.
A sensitivity analysis documented consistently positive signals with significantly elevated ASRs for the GBP-LD cascade against the changes in detection time windows for outcome drugs (ASR [95% CI], 1.66 [1.46–1.88] for 30 days; and 1.52 [1.43–1.61] for 180 days). Consistently positive significant signals were detected for the 30-day and 180-day detection time windows of the BZ-LD cascade (1.51 [1.43–1.60] for 30 days; and 1.32 [1.27–1.36] for 180 days). No signals were detected for the 30-day and 180-day time windows of the GBP-AVD cascade (0.97 [0.88–1.08] and 0.85 [0.81–0.89], respectively). Further, no signals were detected for the 30-day and 180-day time windows of the BZ-AVD cascade (0.82 [0.77–0.86] and 0.91 [0.88–0.94], respectively).
After stratification by GBP-class drugs, the ASR for the mirogabalin-LD cascade was significant and higher than that for pregabalin (2.23 [1.84–2.71] vs 1.59 [1.46–1.73], respectively) (Table 4). The proportion of outpatients among the patients with the mirogabalin-LD cascade was higher than the one among the patients with the pregabalin-LD cascade (92.9% and 76.4%, respectively). When the time window was extended to 180 days, the ASRs for both drugs decreased but remained significant (1.84 [1.59–2.12] for mirogabalin, and 1.45 [1.36–1.55] for pregabalin).
4 Discussion
We conducted a PSSA to investigate PCs of LD and AVD following the first prescription of GBP and BZ in Japanese older adults. We detected positive signals of GBP-LD and BZ-LD cascades, which potentially contribute to subsequent polypharmacy. In particular, a greater and significant ASR for the mirogabalin-LD cascade than for pregabalin was found in GBP class drugs, which may warrant consideration for an additional safety advisory. No signal was detected for AVD cascades.
The validity of this application of PSSA using the DeSC database was confirmed using both positive and negative controls. The sole failure in detecting the ACE-antitussive cascade in a 30-day time window may be explained by the prescribing practice in Japan. As patients typically make regular monthly visits to their doctor to obtain a new one-time prescription for a usual 28-day or 30-day supply of prescription drugs for chronic diseases, most ADRs occurring during visit intervals were likely to be recorded in medical records at the next visit, made after a 28-day or 30-day interval. Thus, a time window longer than 30 days appears to be optimal for capturing prescriptions issued at the next visit, considering an allowance of 2 or 3 days per visit interval, whereas a shorter window of less than 25 days may introduce considerable bias to PSSA results [39]. This finding is consistent with a previous finding that most prescriptions of antitussives were issued within 6 months after the initiation of ACEIs [38]. The finding of no signals for any of the negative control combinations suggests a minimal within-person time-varying bias [26].
The population included in the PSSA differed from the whole population initiating exposure drugs in several regards. The higher average age and higher percentage of inpatients among GBP and BZ initiators with LD cascades are consistent with the known risk factors of edema, which include older adults, female patients, and inpatients [40].
The present results provide good evidence for the GBP-LD cascade, as reported in a preceding study [23]. The NSR of 1.00 indicated that prescribing secular trends of GBP and LD did not change over the study period, suggesting that the impact of temporal changes in prescription trends throughout the whole study period were negligible. Sensitivity analyses using different detection time windows indicated the robustness of the positive signals for the GBP-LD cascade and a consistent increase in the risk of LD prescription after GBP initiation. Compared with those at 90 days, the ASRs of the GBP-LD cascade and the beta blocker-LD cascade in previous reports were decreased when longer detection time windows of 180 and 360 days were applied [23, 26]. The peak of LD initiations at 30 days after GBP is consistent with the results of a post-marketing surveillance study of pregabalin, in which edema and dizziness events were frequently observed within 1 month after the start of treatment [32]. Considering these findings together, a detection window longer than 90 days would bring about the possibility of less sensitivity because of increased LD prescriptions irrespective of drug-induced edema. The stratified analyses indicated that complications of HF and CKD would not alter positive signals for the GBP-LD cascade, suggesting that LD prescribed for the treatment of HF and CKD were irrelevant or had little impact on the PCs initiated by GBP. The mechanism of edema after GBP treatment remains to be elucidated, although several case reports suggest the hypothetical involvement of peripheral vasodilation via interaction with plasma membrane K-ATP channels [41, 42]. The use of LD may subsequently result in adverse outcomes such as an electrolyte imbalance (e.g., hyponatremia and hypokalemia) due to dehydration [43], and have been associated with an increased odds ratio of fall fractures [7, 44]. Further cascades involving potassium supplementation and AVD initiation for LD-induced hypokalemia and dizziness have also been reported [11, 20, 45]. To prevent a chain of PCs and resulting polypharmacy, drug-induced edema in older adults should be carefully differentiated from pathological edema, and undue LD prescriptions against PC should be avoided. In practice, discontinuation or a dose reduction of GBP is recommended as a first-choice treatment for drug-induced edema.
The present study added a new finding, namely the detection of a significant stronger signal of a LD cascade for mirogabalin. This finding makes this signal consistent across GBP-class drugs, as reported in preceding studies in Denmark and the USA [15, 23]. The higher ASR of the mirogabalin-LD cascade than for pregabalin is inconsistent with the results of multiple clinical trials reporting the lower incidence of edema for mirogabalin. A head-to-head randomized trial of patients with diabetic peripheral neuropathic pain found that the incidence of edema was as low as 5.1% in the mirogabalin groups, compared with 10% in the pregabalin group [46]. In addition, a pre-marketing clinical trial of mirogabalin in patients with postherpetic neuralgia consistently reported a lower incidence of peripheral edema than a separate trial of pregabalin [18, 19]. Mirogabalin has more potent and selective affinity for the target subunit of calcium channels than pregabalin [47]. Although mirogabalin is likely to present a preferable safety profile to pregabalin [48], a prospective single-site switching study of pregabalin-treated patients with chronic neuropathic pain found that the prevalences of patient-reported edema and dizziness did not decrease even at 24 weeks after switching to mirogabalin [49]. The perceived safety advantages of mirogabalin may have resulted in less watchful monitoring of outpatients treated with mirogabalin, given that most of patients experiencing a mirogabalin-LD cascade were outpatients. In addition, filling of a LD prescription at a different pharmacy or clinic without knowing that the outpatient was treated with mirogabalin might also have resulted in a mirogabalin-induced LD cascade. Although PCs may not always be possible to avoid, the elevated risk of a mirogabalin-LD cascade in our study seems to be non-negligible considering the possible chain of PCs. The guide for the rational use of mirogabalin issued by the supplier provides no guidance for differentiating and treating edema after the use of mirogabalin [50], and issuance of an additional safety advisory alerting prescribers and pharmacists to check for possible drug-induced edema before the initiation of LD to prevent subsequent PCs and polypharmacy may be warranted [43]. Following such issuance, real-world studies to test the effectiveness of the advisory, such as time trend studies, may be worthwhile. As clinical development of mirogabalin is still underway in Asia for the treatment of central neuropathic pain in patients with spinal cord injury [51], enhanced safety advisory and training for prescribers and community pharmacists to raise attention to the risk of mirogabalin-LD PC and its management before its label and geographical extension are warranted.
Among other findings, no signal of a GBP-AVD cascade was detected; this is despite the higher reported incidence of dizziness than edema for both pregabalin and mirogabalin in pre-marketing clinical trials (31.1% vs 11.7% for pregabalin, and 14.2% vs 7.1% for mirogabalin, respectively) [18, 19]. This result may be explained by the appropriate safety measures taken against the well-known GBP-induced dizziness in Japan. Several studies have reported that preventing PCs requires providing prescribers with guidelines on coping strategies, and improving communication among patients, caregivers, and healthcare providers [7, 9, 11]. In 2012, the Japanese regulatory agency alerted healthcare providers to GBP-induced dizziness and recommended that older adults should be started with a low dose [52]. The drug safety information for healthcare professionals and the patient leaflets provided by the marketing authorization holders, which emphasize caution against GBP-induced dizziness among older adults, may have helped successful communication and understanding of dizziness between patients and healthcare providers [50, 53, 54]. As the data period in the present study began in 2014, we were unable to examine the effect of the 2012 safety advisory on the rational use of pregabalin.
Positive signals of BZ-LD PCs were detected, in agreement with the Japanese package inserts. The mechanism of peripheral edema after BZ administration is likely to involve its vasodilation effects via several pathways [55,56,57]. In the present study, given that the percentage of inpatient prescriptions of the BZ-LD cascade was higher, the most frequently used parenteral drug, midazolam, is likely to have been administered in the in-hospital setting, where patients often receive more intensive care than ambulatory care and are therefore likely to be exposed to other risk factors of edema resulting from such care. Thus, hospitalization may have acted as a confounding factor; nevertheless, positive signals of the BZ-LD cascade with all detection time windows likely requires further caution in BZ use to prevent the LD-cascade in older adults. Most LD in the present study were prescribed within 10 days after BZ initiation, suggesting that the use of BZ during this period should be carefully monitored, especially in the hospital setting, and be limited to short-term administration to avoid consequential LD cascades and the subsequent chain of PC.
Hospitalization may also have functioned as a confounding factor for the ASRs significantly smaller than one in the BZ-AVD cascade. Hospitalization is a known risk factor for dizziness and insomnia and many patients were highly likely to have received both BZ and AVD during hospitalization, especially those receiving surgery under general anesthesia [58, 59]. In addition, BZ preparations are used to treat dizziness in Japanese practice. [60]. Contrary to the present results, a previous study in Australia reported a positive signal in the hypnotic sedative-prochlorperazine cascade [20]. In addition to the different definition of AVD between the studies, the inconsistent results may be attributable to a difference in study timing and clinical practice. The study period of the Australian study was from 2003 to 2006, which was shortly after recommendations restricting the long-term use of BZ were issued by the UK National Institute for Health and Care Excellence in 2004 [61].
There were a few limitations to our study. First, the underlying conditions of prescriptions were not available in the study database, and sequential combinations of exposure and outcome drugs may have been generated by chance. We were therefore unable to accurately determine the development of true PCs and causal exposure for outcome drug prescriptions. Second, we could not identify patients with dizziness or edema who sought care outside of the medical insurance system, such as over-the-counter drugs or self-care with compression stockings for edema. Given the varying and complex pathophysiology of dizziness, treatments for dizziness in Japanese practice are also highly variable. Dizziness could be also treated by several over-the-counter drugs such as motion sickness drugs and Chinese herbal medicines, especially in outpatients who accounted for the large fraction of GBP-treated patients. Some of the over-the-counter preparations contained the same active ingredients as the approved prescription preparations, including histamine H1 blockers (dimenhydrinate, diphenhydramine) and adenosine triphosphate disodium hydrate [60]. In addition, the off-label use of prescription preparations for treating patients with dizziness is widely accepted in Japan, including metoclopramide, promethazine injection, and psychotropic drugs including BZ. Our definition of AVD considered only the on-label use of medications approved in the national health insurance scheme. As the present results excluded these off-label prescriptions from the outcome drugs, results may have been biased towards null because of an increase in false negatives. Their inclusion probably largely increases the chance of counting unspecific prescriptions for conditions other than dizziness (and also edema) as positive (false positives) at the same time because of the large number of on-label uses for other indications of these medications.
5 Conclusions
This study presents evidence of GBP-initiated and BZ-initiated LD PC in older adults in Japan. A new GBP, mirogabalin, presented a higher risk of potential LD-PC than pregabalin, which warrants attention to prevent sequential PC and subsequent polypharmacy. Drug-induced edema in older adults should be carefully differentiated from pathological edema, and undue LD prescriptions should be avoided.
Abbreviations
- ACEI:
-
Angiotensin-converting enzyme inhibitor
- ADR:
-
Adverse drug reaction
- ARB:
-
Angiotensin II receptor blocker
- ASR:
-
Adjusted sequence ratio
- AVD:
-
Anti-vertigo drug
- BZ:
-
Benzodiazepine
- CCB:
-
Calcium channel blocker
- CI:
-
Confidence interval
- CKD:
-
Chronic kidney disease
- CSR:
-
Crude sequence ratio
- GBP:
-
Gabapentinoid
- HF:
-
Heart failure
- ICD:
-
International Classification of Disease
- LD:
-
Loop diuretic
- MGB:
-
Mirogabalin
- NSR:
-
Null-effect sequence ratio
- PC:
-
Prescribing cascade
- PRC:
-
Paracetamol
- PGB:
-
Pregabalin
- PSSA:
-
Prescription sequence symmetry analysis
- SD:
-
Standard deviation
References
Rodrigues MC, Oliveira C. Drug-drug interactions and adverse drug reactions in polypharmacy among older adults: an integrative review. Rev Lat Am Enfermagem. 2016;1(24): e2800.
Pasina L, Brucato AL, Falcone C, Cucchi E, Bresciani A, Sottocorno M, et al. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging. 2014;31(4):283–9.
Akazawa M, Imai H, Igarashi A, Tsutani K. Potentially inappropriate medication use in elderly Japanese patients. Am J Geriatr Pharmacother. 2010;8(2):146–60.
Ministry of Health, Labour and Welfare. Statistics of medical care activities in public health insurance 2021: outline of results: 2. Drug usage [in Japanese]. 2021 2021. Available from: https://www.mhlw.go.jp/toukei/saikin/hw/sinryo/tyosa21/dl/yakuzai.pdf. Accessed 6 Nov 2023.
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230.
Ministry of Health, Labour and Welfare. Guidelines for proper use of medicines in the elderly: an introduction [in Japanese]. 2018. Available from: https://www.mhlw.go.jp/content/11121000/kourei-tekisei_web.pdf. Accessed 6 Nov 2023.
Rochon PA, Gurwitz JH. Optimising drug treatment for elderly people: the prescribing cascade. BMJ. 1997;315(7115):1096–9.
Rochon PA. The prescribing cascade revisited. Lancet. 2017;389(10081):1778–80.
Brath H, Mehta N, Savage RD, Gill SS, Wu W, Bronskill SE, et al. What is known about preventing, detecting, and reversing prescribing cascades: a scoping review. J Am Geriatr Soc. 2018;66(11):2079–85.
Kalisch LM, Caughey GE, Roughead EE, Gilbert AL. The prescribing cascade. Austr Prescr. 2011;34(6):162–6.
Kwan D, Farrell B. Polypharmacy: optimizing medication use in elderly patients. CGS J CME. 2014;4(1):21–7.
Rochon PA, Sudeep SG, Gurwitz JH, et al. General principles of pharmacology and appropriate prescribing. In: Halter JB, Ouslander JG, Studenski S, High KP, Asthana S, Supiano MA, et al., editors. Hazzard’s geriatric medicine and gerontology. 7th ed. New York: McGraw Hill; 2017.
Suzuki Y, Sakakibara M, Shiraishi N, Hirose T, Akishita M, Kuzuya M. Prescription of potentially inappropriate medications to older adults: a nationwide survey at dispensing pharmacies in Japan. Arch Gerontol Geriatr. 2018;77:8–12.
Montastruc F, Loo SY, Renoux C. Trends in first gabapentin and pregabalin prescriptions in primary care in the United Kingdom, 1993–2017. JAMA. 2018;320(20):2149–51.
Read SH, Giannakeas V, Pop P, Bronskill SE, Herrmann N, Chen S, et al. Evidence of a gabapentinoid and diuretic prescribing cascade among older adults with lower back pain. J Am Geriatr Soc. 2021;69(10):2842–50.
Inada K, Enomoto M, Yamato K, Mishima K. Prescribing pattern of hypnotic medications in patients initiating treatment at Japanese hospitals: a nationwide, retrospective, longitudinal, observational study using a claims database. Drugs Real World Outcomes. 2021;8(3):277–88.
Mitsubishi Tanabe Pharma Co. The interview form Depas (etizoram tablets and fine granules) [in Japanese]. 2019. Available from: https://www.pmda.go.jp/PmdaSearch/iyakuDetail/ResultDataSetPDF/400315_1179025C1054_2_18. Accessed 6 Nov 2022.
Viatris Inc. Lyrica® (pregabalin) [package insert]. 2023. Available from: https://www.info.pmda.go.jp/go/pack/1190017F1029_3_03/. Accessed 6 Nov 2023.
Daiichi sankyo Co. Ltd. Tarlige® (mirogabalin) [package insert] [in Japanese]. 2023. Available from: https://www.info.pmda.go.jp/go/pack/1190026F1028_1_10. Accessed 6 Nov 2023.
Caughey GE, Roughead EE, Pratt N, Shakib S, Vitry AI, Gilbert AL. Increased risk of hip fracture in the elderly associated with prochlorperazine: is a prescribing cascade contributing? Pharmacoepidemiol Drug Saf. 2010;19(9):977–82.
Kobayashi M. Drug-induced dizziness with delayed identification of the culprit drug due to polypharmacy [in Japanese]. Yakuji [The Pharmaceuticals]. 2020; p. 1772–5.
Shahid F, Doherty A, Wallace E, Schmiedl S, Alexander GC, Dreischulte T. Prescribing cascades in ambulatory care: a structured synthesis of evidence. Pharmacotherapy. 2024;44(1):87–96.
Vouri SM, Morris EJ, Wang GH, Hashim Jaber Bilal A, Hallas J, Henriksen DP. Association between gabapentinoids and oedema treated with loop diuretics: a pooled sequence symmetry analysis from the USA and Denmark. Br J Clin Pharmacol. 2022;88(12):5269–94.
Doherty AS, Shahid F, Moriarty F, Boland F, Clyne B, Dreischulte T, et al. Prescribing cascades in community-dwelling adults: a systematic review. Pharmacol Res Perspect. 2022;10(5): e01008.
Pratt N, Andersen M, Bergman U, Choi NK, Gerhard T, Huang C, et al. Multi-country rapid adverse drug event assessment: the Asian Pharmacoepidemiology Network (AsPEN) antipsychotic and acute hyperglycaemia study. Pharmacoepidemiol Drug Saf. 2013;22(9):915–24.
Vouri SM, Morris EJ, Jiang X, Hofer AK, Schmidt S, Pepine C, et al. Evaluation of a beta-blocker-edema-loop diuretic prescribing cascade: a prescription sequence symmetry analysis. Am J Hypertens. 2022;35(7):601–9.
Vouri SM, Jiang X, Manini TM, Solberg LM, Pepine C, Malone DC, et al. Magnitude of and characteristics associated with the treatment of calcium channel blocker-induced lower-extremity edema with loop diuretics. JAMA Netw Open. 2019;2(12): e1918425.
Vouri SM, Morris EJ, Usmani SA, Reise R, Jiang X, Pepine CJ, et al. Evaluation of the key prescription sequence symmetry analysis assumption using the calcium channel blocker: loop diuretic prescribing cascade. Pharmacoepidemiol Drug Saf. 2022;31(1):72–81.
King CE, Pratt NL, Craig N, Thai L, Wilson M, Nandapalan N, et al. Detecting medicine safety signals using prescription sequence symmetry analysis of a national prescribing data set. Drug Saf. 2020;43(8):787–95.
Lai EC, Pratt N, Hsieh CY, Lin SJ, Pottegard A, Roughead EE, et al. Sequence symmetry analysis in pharmacovigilance and pharmacoepidemiologic studies. Eur J Epidemiol. 2017;32(7):567–82.
Pharmaceuticals and Medical Devices Agency. Drug information search [in Japanese]. Available from: https://www.pmda.go.jp/PmdaSearch/iyakuSearch/. Accessed 6 Nov 2022.
Nozawa K, Matui M, Yoshiyama T, Fuzii K. Safety and efficacy of pregabalin (Lyrica capsules) in patients with neuropathic pain under practical conditions [in Japanese]. Prog Med. 2018;38(9):1009–18.
Kato J, Baba M, Kuroha M, Kakehi Y, Murayama E, Wasaki Y, et al. Safety and efficacy of mirogabalin for peripheral neuropathic pain: pooled analysis of two pivotal phase III studies. Clin Ther. 2021;43(5):822-35.e16.
Kaiser Permanente. Benzodiazepine and Z-drug safety guideline. 2014. Available from: https://wa.kaiserpermanente.org/static/pdf/public/guidelines/benzo-zdrug.pdf. Accessed 6 Nov 2023.
Tsiropoulos I, Andersen M, Hallas J. Adverse events with use of antiepileptic drugs: a prescription and event symmetry analysis. Pharmacoepidemiol Drug Saf. 2009;18(6):483–91.
Australian Institute of Health and Welfare. Acute kidney injury in Australia: a first national snapshot. 2015. Available from: https://www.aihw.gov.au/getmedia/7e0f5313-d61d-4de3-ad8d-389dcc7a03dc/19380.pdf. Accessed 5 Dec 2023.
Japan Pharmaceutical Manufacturers Association. Real world data analysis in practice: let’s try RWD analysis [in Japanese]. 2017. Available from: https://www.jpma.or.jp/information/evaluation/results/allotment/lofurc00000083es-att/real_world_data.pdf. Accessed 20 Dec 2022.
Vegter S, de Jong-van den Berg LT. Misdiagnosis and mistreatment of a common side-effect: angiotensin-converting enzyme inhibitor-induced cough. Br J Clin Pharmacol. 2010;69(2):200–3.
Takeuchi Y, Shinozaki T, Matsuyama Y. A comparison of estimators from self-controlled case series, case-crossover design, and sequence symmetry analysis for pharmacoepidemiological studies. BMC Med Res Methodol. 2018;18(1):4.
Besharat S, Grol-Prokopczyk H, Gao S, Feng C, Akwaa F, Gewandter JS. Peripheral edema: a common and persistent health problem for older Americans. PLoS ONE. 2021;16(12): e0260742.
Kruger S, Lindstaedt M. Pregabalin and edema in young women suffering from premenstrual syndrome. Pharmacopsychiatry. 2010;43(5):202–3.
Wustmann T, Piro J, Gutmann P. Metabolic considerations in a case of pregabalin-induced edema. Pharmacopsychiatry. 2009;42(2):75–6.
Sica DA. Diuretic-related side effects: development and treatment. J Clin Hypertens (Greenwich). 2004;6(9):532–40.
Berry SD, Mittleman MA, Zhang Y, Solomon DH, Lipsitz LA, Mostofsky E, et al. New loop diuretic prescriptions may be an acute risk factor for falls in the nursing home. Pharmacoepidemiol Drug Saf. 2012;21(5):560–3.
Wang GH, Morris EJ, Smith SM, Hallas J, Vouri SM. Continued potassium supplementation use following loop diuretic discontinuation in older adults: an evaluation of a prescribing cascade relic. J Am Geriatr Soc. 2023;71:505–15.
Vinik A, Rosenstock J, Sharma U, Feins K, Hsu C, Merante D, et al. Efficacy and safety of mirogabalin (DS-5565) for the treatment of diabetic peripheral neuropathic pain: a randomized, double-blind, placebo- and active comparator-controlled, adaptive proof-of-concept phase 2 study. Diabetes Care. 2014;37(12):3253–61.
Domon Y, Arakawa N, Inoue T, Matsuda F, Takahashi M, Yamamura N, et al. Binding characteristics and analgesic effects of mirogabalin, a novel ligand for the alpha(2)delta subunit of voltage-gated calcium channels. J Pharmacol Exp Ther. 2018;365(3):573–82.
Mendell J, Levy-Cooperman N, Sellers E, Vince B, Kelsh D, Lee J, et al. Abuse potential of mirogabalin in recreational polydrug users. Ther Adv Drug Saf. 2019;10:2042098619836032.
Hagihara S, Nakagawa M, Kamijima K, Kuwahara S, Hayashi M, Abe Y. Assessment of clinical adverse events of mirogabalin switching from pregabalin in choronic pain management [in Japanese]. J Japan Soc Pain Clinicians. 2021;28(4):43–8.
Daiichi sankyo Co. Ltd. Tarlige: guideline for property use [in Japanese]. 2018. Available from: https://www.medicalcommunity.jp/filedsp/products$druginfo$tarlige$safety_rmp_m$TLG7RM01/field_file_pdf. Accessed 6 Nov 2022.
Ushida T, Katayama Y, Hiasa Y, Nishihara M, Tajima F, Katoh S, et al. Mirogabalin for central neuropathic pain after spinal cord injury. Neurology. 2023;100(11):e1193–206.
Ministry of Health, Labour and Welfare. Pharmaceuticals and medical devices safety information No. 293. 2012. Available from: https://www.pmda.go.jp/files/000144665.pdf#page=7. Accessed 6 Nov 2023.
Pfizer Japan Inc. Lyrica capsule: proper use information: dizziness, somnolence, and loss of consciousness in the elderly [in Japanese]. 2012. Available from: https://www.pmda.go.jp/files/000144302.pdf. Accessed 6 Nov 2022.
Daiichi sankyo Co. Ltd. Tarlige for patients receiving treatment with Tarlige [in Japanese]. 2018. Available from: https://www.medicalcommunity.jp/filedsp/products$druginfo$tarlige$safety_rmp_p$TLG1P001/field_file_pdf. Accessed 6 Nov 2022.
Veenman L, Gavish M. The peripheral-type benzodiazepine receptor and the cardiovascular system: implications for drug development. Pharmacol Ther. 2006;110(3):503–4.
Cho S, Atwood JE. Peripheral edema. Am J Med. 2002;113(7):580–6.
Kagota S, Morikawa K, Ishida H, Chimoto J, Maruyama-Fumoto K, Yamada S, et al. Vasorelaxant effects of benzodiazepines, non-benzodiazepine sedative-hypnotics, and tandospirone on isolated rat arteries. Eur J Pharmacol. 2021;892: 173744.
Badr AF, Kurdi S, Alshehri S, McManus C, Lee J. Pharmacists’ interventions to reduce sedative/hypnotic use for insomnia in hospitalized patients. Saudi Pharm J. 2018;26(8):1204–7.
Frighetto L, Marra C, Bandali S, Wilbur K, Naumann T, Jewesson P. An assessment of quality of sleep and the use of drugs with sedating properties in hospitalized adult patients. Health Qual Life Outcomes. 2004;24(2):17.
Yasuyuki N. Recently introduced anti-dizziness/vertigo drugs in Japan [in Japanese]. Equil Res. 2019;78(1):7–15.
National Institute for Health and Care Excellence. Guidance on the use of zaleplon, zolpidem and zopiclone for the short-term management of insomnia. 2004 . Available from: https://www.nice.org.uk/guidance/ta77/informationforpublic. Accessed 6 Nov 2022.
Acknowledgments
We are in debt to DeSC Healthcare Inc. for providing the DeSC database. We are grateful to Dr. Guy Harris of Dmed (Tokyo, Japan; https://dmed.co.jp) for English editing and proofreading.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors did not receive support from any organization for the submitted work.
Conflicts of Interest/Competing Interests
Hisashi Urushihara has received research funds from Daiichi Sankyo Co. Ltd., outside of the present work and bearing no role in it. Rina Omata, Akane Asami, and Azusa Hara have no relevant financial or non-financial interests to disclose.
Ethics Approval
The study protocol was approved by the Ethics Committee for Research Involving Humans of Keio University Faculty of Pharmacy (No. 220406-2), according to the local ethical guidelines for biological and medical research involving human subjects. This study was conducted for non-commercial purposes by an academic research organization, and the requirement for individual consent to the collection and secondary use of existing personal health data was therefore waived according to the Japanese Privacy Protection Law.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
All data generated or analyzed during this study are included in this published article.
Code Availability
Not applicable.
Authors’ Contributions
Conceptualization, RO and HU; methodology, RO and HU; formal analysis, RO and HU; validation, AA; resources, HU; writing - original draft preparation; RO; writing - review and editing; AA, AH, and HU; supervision, AH and HU. All authors gave final approval of the version to be published, and agreed on the journal to which the article has been submitted. Further, all authors agree to take responsibility and be accountable for the contents of the article. All authors read and approved the final version.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Omata, R., Asami, A., Hara, A. et al. Prescribing Cascades of Loop Diuretics and Anti-vertigo Drugs Following Treatment with Gabapentinoids and Benzodiazepines: Prescription Sequence Symmetry Analysis of a Large-Scale Claims Database Including Japanese Older Adults. Drugs - Real World Outcomes 11, 529–540 (2024). https://doi.org/10.1007/s40801-024-00446-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-024-00446-x