Abstract
Background
Disease-modifying anti-rheumatic drugs (DMARDs), since their introduction in 1990, have revolutionized the management of rheumatoid arthritis. Newer DMARDs have recently been approved, influencing treatment patterns and clinical guidelines.
Objective
To update the current prescribing patterns of DMARDs in the pharmacotherapy of rheumatoid arthritis (RA) to include the pandemic era.
Methods
This was a retrospective cross-sectional multi-year study. Using Optum’s Clinformatics® Data Mart Database, we summarized trends in the prevalence of DMARD use in the USA from 2016 to 2021 by year for adult patients ≥ 18 years old with at least one medical RA claim and one pharmacy/medical claim of a DMARD medication. Trends included type of DMARD, class of DMARD (conventional (csDMARDs), biologics [tumor necrosis factor (TNFi) and Non-TNFi), and Janus kinase inhibitors (JAKs)], and triple therapy [methotrexate (MTX), hydroxychloroquine (HCQ), sulfasalazine (SUL)] used.
Results
The total sample from 2016 to 2021 was 670,679 commercially insured patients. The average age was 63.7 years (SD 13.6), and 76.7% were female and 70% were White. csDMARDs remain the most prescribed (ranging from 77.2 to 79.2%). Although JAKs were the least prescribed DMARD class, their proportion more than doubled from 2016 (1.5%) to 2021 (4%). MTX utilization declined from 40% in 2016 to 34% in 2021. In contrast, HCQ use increased during the pandemic era from < 25% in 2018 to 30% in 2021. Although there is evidence of the therapeutic benefit of triple therapy, its use was very low (~ 1%) compared to biologics only (~ 17%) or biologics+MTX (~ 10%).
Conclusion
About half of patients with RA were on DMARDs. As expected, csDMARDs were highly used consistently. The COVID-19 pandemic might have influenced the use of HCQ and infusion DMARDs. Triple therapy use remains low.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Although the overall rate of disease-modifying anti-rheumatic drug (DMARD) use has not changed in the past 5 years, biologic DMARD use increased while conventional DMARDs use decreased. |
The COVID pandemic appears to have influenced the use of hydroxychloroquine and infusion DMARDs in patients with rheumatoid arthritis. |
Although triple therapy is recommended by clinical guidelines because of low cost and equivalent effectiveness, its use remains low. |
1 Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory autoimmune disorder with primary clinical manifestations of symmetrical inflammatory polyarthritis, starting often with the small joints of the hands and feet, and spreading to other larger joints [1]. The prevalence of RA is low (~ 0.5% in the USA), but the most common form of inflammatory arthritis [2]. The economic cost of RA is substantial: from direct medical cost/patient of US $12,509 for those using any treatment to US $36,053 for those using biologic disease-modifying antirheumatic drugs (DMARDs) in the USA [3].
DMARDs are immunosuppressive and immunomodulatory drugs indicated for multiple conditions including inflammatory arthritis and connective tissue diseases such as systemic lupus erythematosus [4]. Medications such as non-steroidal anti-inflammatory drugs (NSAIDs) are useful for symptomatic treatment; however, DMARDs have revolutionized RA management since they are disease modifying (suppress autoimmune activity and delay or prevent joint degeneration) and have the potential for remission or low disease activity [1, 5]. Since the inception of the use of DMARDs in the late 1990s, newer forms have emerged with substantial cost. Treatment patterns and clinical guidelines have recognized DMARDs as the cornerstone of RA management, including the use of “treat-to-target” (T2T) as a disease-management strategy. T2T is a prescriber-patient treatment plan to achieve a specific clinical goal or target, and it could involve mono, dual, or multi- RA medications [5]. A 2004–2015 trend analysis of biologic use in RA showed a significant shift to newer biologics from the older approved biologics such as infliximab, as first agent of choice [6]. Additionally, the COVID-19 pandemic impacted healthcare delivery, especially in-person care, and the controversies surrounding the role of hydroxychloroquine for COVID-19 treatment/prevention may have impacted RA treatment patterns [7]. For example, there was a significant uptake of telehealth care, self-reported discontinuation of DMARDs, and drug shortages, especially those used in COVID-19 management for sedation, analgesia, and paralysis [8,9,10].
Consequently, the complexity of RA, medical improvements in diagnosis, newer DMARDs, efficacy and safety concerns, and financial costs are some of the issues that have impacted the management of RA recently [1].
It is therefore important to objectively periodically evaluate contemporary medication management approaches and trends to inform prescribers of changes in medication use as well as uptake of newer medications, which has the potential to inform third-party payers, health systems, and other decision makers of strategies to anticipate expected pipeline innovations, and unexpected disruptions such as pandemics on care delivery.
2 Methods
This was a retrospective, observational administrative claims data, annual cross-sectional trend analysis of patients diagnosed with RA with claims for a DMARD. The study was deemed exempt by the University of Pittsburgh Institutional Review Board. The dataset, Optum’s de-identified Clinformatics® Data Mart Database (CDM), is derived from a database of administrative health claims from members of large commercial and Medicare Advantage health plans. The database includes approximately 17–19 million annual covered lives, for a total of over 65 million unique lives over January 2007 through December 2021. CDM is statistically de-identified under the Expert Determination method consistent with HIPAA and managed according to Optum customer data use agreements. CDM administrative claims submitted for payment by providers and pharmacies are verified, adjudicated, and de-identified prior to inclusion. These data, including patient-level enrollment information, are derived from claims submitted for all medical and pharmacy healthcare services with information related to healthcare costs and resource utilization, therefore informed consent was not needed. The population is geographically diverse, spanning all 50 states [11].
Study patients were defined as those with ≥ one RA-related medical claim (inpatient and/or outpatient identified with the international classification of disease (ICD-10) ‘M05’ and ‘M06’), and either a medical claim of a RA-related DMARD (using J-codes such as J0129 and J0135) or a pharmacy claim for a DMARD (using NDCs such as 00054455015 and 000740067020). New users of DMARD were defined as those with DMARD and RA medical claims in a year, who had RA medical claims, but no DMARD claims in the previous year.
The number of DMARD claims at the patient level were summarized as 30-day equivalent claims per year (2016–2021 had full year data but 2021 had only 9 months available data at the time of the study). A 30-day supply of medications is one 30-day equivalent claim, a 60-day supply is two 30-day equivalent claims, and a 90-day supply is three 30-day equivalent claims. The sum of the number of 30-day equivalent claims per patient of each specific DMARD, divided by the total number of 30-day equivalent claims of all DMARDs in each year, was defined as the proportion of the specific DMARD for that year. DMARDs were summarized at the individual drug level, as a class (conventional (csDMARDs)), biologic (bDMARDs), which include (tumor necrosis factor inhibitors (TNFis) and Non-TNFis), and Janus kinase inhibitors (JAKs) (Table 3) [12]. We also compared triple therapy (defined as the overlap use of MTX, SUL, and HCQ) with overlap use of a biologic and MTX. We defined the pandemic era in this analysis as the years covering 2020 and 2021. All comparative categorical analyses, including descriptive statistics, were performed using chi-square tests.
3 Results
The total sample from 2016 to 2021 included a DMARD prevalence group of 670,679 and 37,907 new DMARD users (2017–2021) (Table 1).
There was an approximately 40% increase in unique patients/year from 2016 (88,826) to 2021 (123,278), with duplicates in multiple years in the prevalence group (Table 2).
The new DMARD group average was 7600/year (see Online Supplemental Material (OSM) Table 1). On average, there were 48.5% of patients with RA medical claims who also had a prescription-claim DMARD (46%) and/or medical-claim DMARD (5%). The proportion prescribed DMARDs increased from 46% in 2019 to 51% in 2020 and 2021.
The average age was 63.7 years (SD 13.6); 53.6% were ≥ 65 years old, 76.7% were female, 70% were White, and almost half of the patients came from the south (Table 2). These demographics from the prevalence cohort were similar to the new DMARD users (OSM Table 1).
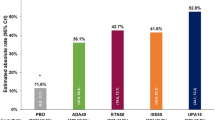
csDMARDs remain the most prescribed DMARD (ranging from 77.2% to 79.2%) followed by biologic TNFis (ranging from 13.2% to 19.5%). Although the JAKs were the least prescribed DMARD class, their proportion doubled from 2016 (1.5%) to 2021 (4%) (Fig. 1).
The patterns of use for prevalent DMARD use and new DMARD use were dramatically different (Fig. 1). Prevalent DMARDs were mainly more than 75% csDMARDs and 20% bDMARDs for all years, while new DMARD use was almost split between csDMARDs and bDMARDs. For new users of DMARDs, in 2019 and 2020, there were significant reductions in csDMARDs use (47% and 49%) compared to 56% in 2017 and 2018; and an increase in the use of bDMARDs (42% in 2017 and 2018 to 50% in 2019 and 47% in 2020), driven mainly by the newer biologics (tofacitinib1.5–2.7%, tocilizumab 0.2–0.5%, upadacitinib 0–1.2%, baricitinib 0–0.2%, and sarilumab 0–0.2%) (Fig. 1). Of note, three of the DMARDs were approved within the study period (two of the three JAKs (upadacitinib: August 2019, baricitinib: May 2018) and the non-TNFi sarilumab: May 2017) (Table 3).
MTX was the most prescribed DMARD followed by HCQ and LEF; however, there was a steady decline in MTX utilization from 40% in 2016 to about 33% in 2021. On the contrary, HCQ use increased from < 25% in 2018 to 30% in 2021, consistent with an increased use during the pandemic era (Fig. 2).
Among new users of DMARDs, the most prescribed DMARD was infliximab, followed by MTX, HCQ, and rituximab. However, unlike MTX and HCQ, there was a significant decrease in infliximab (22% in 2019 to 15% in 2021) and rituximab (17% in 2019 to 12% in 2021) claims, indicating a significant decrease in use of infusion DMARDs in the pandemic era (Fig. 3).
Triple therapy use, across the 6 years, was very low (~ 1%) compared to that of biologics monotherapy (~ 17%) or biologics+MTX (~ 10%) (OSM Fig. 1). Among new users of DMARDs, the proportion using biologics monotherapy was even higher, 43% in 2017 to 47% in 2021, biologic+MTX 5.6% in 2017 to 10% in 2021, and triple therapy use was ≤ 0.5% (OSM Fig. 2).
4 Discussion
The goal of this study was to update trends in type of DMARDs utilization for patients with RA including the pandemic era. The proportion of patients with RA who had DMARD claims (~ 50%) was consistent with previous studies on prevalence or newly diagnosed patients [13]. Similarly, females continue to dominate RA medical or DMARD claims. There were 76.7% females in our analysis, compared to 72.7% in an analysis of newly diagnosed commercially insured patients in a study by Kern et al. [14], three- to fivefold higher prevalence in a global review study by Radu et al. [1], and 76% among the commercially insured subgroup in the Komodo CMS report [15]. A previous trend analysis of RA medications from 2006 to 2014 found that almost half of patients diagnosed with RA were not given a DMARD as recommended by the American College of Rheumatology (ACR), similar to our findings almost 10 years later [14]. Another trend analysis from 2005 to 2016 found that 45% of patients had any use of a DMARD in the 12-year study period [16].
We found different mono, dual, and multi-therapy involving the various types of DMARDs reflective of the ACR and the European Alliance of Associations for Rheumatology (EULAR) recommendation to T2T [1]. This could mean that more prescribers are aiming for remission or low disease activity in their RA management. In 2021 ACR recommendations, MTX monotherapy was either strongly or conditionally recommended over other DMARDs for DMARD-naïve patients with moderate to severe disease [5]. The high prevalence of MTX over the years attests to its value among DMARDs for the treatment of RA. MTX remains the best combination of efficacy, safety, and cost among csDMARDs [17, 18]. However, the dramatic differences in prevalent and new users of csDMARDs versus bDMARDs indicates a shift in aggressiveness of initial RA DMARD therapy. The increase in bDMARD use, especially among non-TNFis, could explain the slight decline in use of MTX from 2018. The increase in csDMARD use in 2020 and 2021 could be a shift in prescribing influenced by the COVD-19 pandemic due to mode of administration and cost of bDMARDs relative to csDMARDs.
The proportion of triple therapy claims is low and surprising especially since there is evidence to suggest that their efficacy is equivalent to biologics+MTX. However, a recent systematic review and network meta-analysis reported that triple therapy had lower odds of achieving an ACR70 response rate at 6 months compared to TNF+MTX (odds ratio (OR) 0.35; 95% confidence interval (CI) 0.19–0.64) for patients naïve to MTX or without adequate response to MTX monotherapy [19]. Therefore, our findings could suggest that prescribers are choosing MTX+TNF over triple therapy as a secondary option.
Following limited anecdotal clinical data suggesting clinical benefit of the use of HCQ for preventing COVID-related hospitalization, the US Food and Drug Administration (FDA) issued an emergency use authorization on 28 March 2020 [20]. The increase in HCQ use in 2020 and 2021 in our analysis coincides with the authorization and could explain the increased use among RA patients.
Our findings of a reduction in MTX and an increase in HCQ use during the pandemic era are buttressed by a UK population-level cohort study using both primary-care and hospital data. The study, using data from April 2019 to March 2022, concluded, among others, that the proportion of DMARD use during the pandemic was similar to the year prior to the start of the pandemic. However, the rate of use of MTX and LEF reduced and HCQ and SUL use increased [21].
Given current treatment paradigms that emphasize treating to target symptoms, it is not apparent what an appropriate proportion of utilization of DMARDs is. The value of DMARDs in managing RA continues to grow given newer or different combination therapies, but these are often hobbled by well-documented adverse reactions, which include severe infections, hepatoxicity, gastrointestinal distress, alopecia, and peripheral neuropathy [4]. Although efficacy and safety are often the primary considerations of therapy, patient quality of life, which is associated with efficacy and safety, and could include ease and frequency of medication administration, is increasingly being addressed. A patient-reported outcomes meta-analysis of DMARDs supports the benefits of DMARDs in the domains of pain, fatigue, and activity limitation [22]. The authors had inadequate information to make conclusions on work absenteeism/productivity (only two papers that compared other DMARDs with MTX with comparable impact), but findings were favorable. JAK inhibitors, the newest approved FDA DMARDs, which are oral medications, are gradually gaining traction as an adjunct in most combination therapies and there is evidence that they were used to treat COVID-19, which could also explain the higher usage in the pandemic era [23]. Currently, only three JAK inhibitors have been approved by the FDA, but several more are in different phases in the approval process [1].
This is an observational cross-sectional study using administrative dataset, so it is subject to limitations such as miscoding and equating medication claims to actual patient use. Additionally, although our data source has broad national coverage, it was mainly about commercial covered lives and had a significant diversity limitation for broad external validity consideration. We do not have access to laboratory testing, and thus cannot evaluate rheumatoid factor (RF), and were not able to examine the influence of RF negative RA on prescribing trends.
5 Conclusions
In conclusion, trends in the proportion of patients with RA with any DMARD claims have not increased despite addition of newer products and recommendations from the ACR and EULAR. csDMARDs continue to play a significant role in the management of RA, and use of newer medications, such as JAKs, has doubled over the past 5 years. Triple therapy use is low, suggesting that prescribers prefer mono and dual therapies involving biologics.
References
Safiri S, Kolahi AA, Hoy D, et al. Global, regional and national burden of rheumatoid arthritis 1990–2017: a systematic analysis of the global burden of disease study 2017. Ann Rheum Dis. 2019;78:1463–71.
Holdsworth EA, Donaghy B, Fox KM, et al. Biologic and targeted synthetic DMARD utilization in the United States: Adelphi real world disease specific programme for rheumatoid arthritis. Rheumatol Ther. 2021;8(4):1637–49.
Hsieh P, Wu O, Geue C, et al. Economic burden of rheumatoid arthritis: a systematic review of literature in biologic era. Ann Rheum Dis. 2020;79(6):771–7.
Benjamin O, Goyal A., Lappin SL. 2022. Disease modifying anti-rheumatic drugs (DMARD). StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 4, 2022. Disease Modifying Anti-Rheumatic Drugs (DMARD) - StatPearls - NCBI Bookshelf (nih.gov)
Fraenkel L, Bathon JM, England BR, et al. 2021American College of Rheumatology guidelines for the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken). 2021;73(7):924–39.
Desai RJ, Solomon DH, Jin Y, et al. Temporal trends in use of biologics DMARDs for rheumatoid arthritis in the United States: a cohort study of publicly and privately insured patients. J Manag Care Spec Pharm. 2017;23(8):809–14.
Udapa A, Leverenz D, Balevic SJ, et al. Hydroxychloroquine and COVID-19: a Rheumatological’s take on the lessons learned. Curr Allergy Asthma Rep. 2021;21(1):5.
Ammar MA, Sacha GL, Welch SC, et al. Sedation, Analgesia, and Paralysis in COVID-19 patients in the setting of drug shortages. J Intensive Care Med. 2021;36(2):157–74.
Alipor J, Hayavi-Haghighi MH. Opportunities and challenges of telehealth in disease management during COVID-19 pandemic: A scoping review. Appl Clin Inform. 2021;12(4):864–76.
George MD, Venkatachalam S, Banerjee S, et al. Concerns, healthcare use, and treatment interruptions in patients with common autoimmune rheumatoid diseases during the COVID-19 pandemic. J Rheumatol. 2021;48(4):603–7.
Optum’s de-identified Clinformatics® Data Mart Database. Available at W377379_Clinformatics Data Mart collateral_Sept17.indd (optum.com). Accessed 18 Dec2023.
Arnold MJ. Management of rheumatoid arthritis: update from ACR. Am Fam Physician. 2022;106(3):340–2.
Ward MM. Trends in the use of disease modifying antirheumatic medications in rheumatoid arthritis, 1980–1955: results from the National Ambulatory Medical Care surveys. J Rheumatol. 1999;26(3):546–50.
Kern DM, Chang L, Sonawane K, et al. Treatment patterns of newly diagnosed rheumatoid arthritis patients from a commercially insured population. Rheumatology and Therapy. 2018;5:355–69.
Disease modifying anti-rheumatic drug (DMARD) therapy for rheumatoid arthritis: Patterns of utilization and actionable insights. Komodo Health. A public report on behalf of the Centers for Medicare & Medicaid Services Qualified Entity program. Accessed 02/05/2023. Available at https://www.komodohealth.com/hubfs/_2021_QE_Reports/Arthritis/KomodoHealth-QECP-Report-11-03-2021.pdf Accessed 17 Jan 2024.
Lee J, Chang C, Yung R, Bynum JPW. Provider specialty and the use of disease-modifying antirheumatic drugs for rheumatoid arthritis among older adults in the 2005–2016 national ambulatory medical care survey. ACR Open Rheumatol. 2022;4(4):332–7.
Yazici Y. Long-term safety of methotrexate in the treatment of rheumatoid arthritis. Clin Exp Rheumatol. 2010;28:65–7.
Alfaro-Lara R, Espinosa-Ortega HF, Arce-Salinas CA. Systematic review and meta-analysis of the efficacy and safety of leflunomide and methotrexate in the treatment of rheumatoid arthritis. Rheumatol Clin. 2019;15:133–9.
Fleischmann R, Tongbram V, van Vollenhoven R, et al. Systematic review and network meta-analysis of the efficacy and safety of tumor necrosis factor inhibitor-methotrexate combination therapy versus triple therapy in rheumatoid arthritis. RMD Open. 2017;3: e000371.
Lenzer J. COVID-19: US gives emergency approval to hydroxychloroquine despite lack of evidence. BMJ. 2020;369: m1335.
Russell MD, Galloway JB, Andrews CD, et al. Incidence and management of inflammatory arthritis in England before and during the COVID-19 pandemic: a population level cohort study using OpenSAFELY. The Lancet Rheumatology. 2022;4(12):e853–63.
Van den Dikkenberg M, Luurssen-Masurel N, Kuijper TM, et al. Meta-analyses on the effects of disease modifying anti-rheumatic drugs on the most relevant patient-reported outcome domains in rheumatoid arthritis. Arthritis care Res (Hoboken). 2023;75(8):1659–72.
Chen C, Wang J, Li H. JAK-inhibitors for coronavirus disease-2019 (COVID-19): a meta-analysis. Leukemia. 2021;35(9):2616–20.
Approval of Methotrexate. Available at Accumulating Evidence for a Drug–Drug Interaction Between Methotrexate and Proton Pump Inhibitors - PMC (nih.gov) Accessed 17 Jan 2024.
Approval of hydroxychloroquine. Available at Myth surrounding the FDA disapproval of hydroxychloroquine sulfate and chloroquine phosphate as drugs for coronavirus disease 2019 - PMC (nih.gov). Accessed 17 Jan 2024.
Approval of Sulfasalazine. Available at Exposure Data - Some Drugs and Herbal Products - NCBI Bookshelf (nih.gov). Accessed 17 Jan 2024.
Approval of Leflunomide. Available at Leflunomide for the treatment of rheumatoid arthritis - PMC (nih.gov). Accessed 17 Jan 2024.
Approval of Azathioprine. Available at Generic Imuran Availability - Drugs.com. Available at 01/17/24.
Approval of Humira. Available at Humira (adalimumab) FDA Approval History - Drugs.com. Accessed at 01/17/24.
Approval of Enbrel. Available at Enbrel (etanercept) FDA Approval History - Drugs.com. Accessed 17 Jan 2024.
Approval of Cimzia. Available at FDA Approves Cimzia to Treat Crohn's Disease - Gastroenterology (gastrojournal.org). Accessed 17 Jan 2024.
Approval of Simponi. Available at Simponi (golimumab) FDA Approval History - Drugs.com. Accessed 17 Jan 2024.
Approval of Remicade. Available at Remicade® (infliximab): 20 years of contributions to science and medicine - PMC (nih.gov). Accessed 17 Jan 2024.
Approval of Abatacept. Available at FDA APPROVED: Subcutaneous Abatacept for the Treatment of Rheumatoid Arthritis • Johns Hopkins Arthritis Center. Accessed 17 Jan 2024.
Approval of Tocilizumab. Available at FDA approves tocilizumab to treat rheumatoid arthritis | American Journal of Health-System Pharmacy | Oxford Academic (oup.com). Accessed 17 Jan 2024.
Approval of Sarilumab. Available at FDA Approves Sarilumab for the Treatment of Adults with Glucocorticoid-Resistant PMR - The Rheumatologist (the-rheumatologist.org). Accessed 17 Jan 2024.
Approval of Rituximab. Available at Rituximab: the first monoclonal antibody approved for the treatment of lymphoma - PubMed (nih.gov). Accessed 17 Jan 2024.
Approval of Anakinra. Available at FDA Expands Indication for Anakinra to Include Rare Autoinflammatory Disease (pharmacytimes.com). Accessed 17 Jan 2024.
Approval of Upadacitinib. Available at Upadacitinib: First Approval - PubMed (nih.gov). Accessed 17 Jan 2024.
Approval of Baricitinib. Available at FDA Approves Baricitinib Oral Tablets as First Systemic Alopecia Areata Treatment (drugtopics.com). Accessed 17 Jan 2024.
Approval of Tofacitinib. Available at FDA approves Boxed Warning about increased risk of blood clots and death with higher dose of arthritis and ulcerative colitis medicine tofacitinib (Xeljanz, Xeljanz XR) | FDA. Accessed 17 Jan 2024.
Acknowledgements
The authors acknowledge Ms. Kristie Max for providing support with the references and figures.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This project was deemed exempt by the University of Pittsburgh Institutional Review Board. The study did not use any interventions or experiments on humans or human tissues.
Availability of Data and Materials
The data that support the findings of this study are available from Optum Clinformatics, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of Optum, although there may be a fee from Optum should patient-level data be requested.
Competing Interests
The authors have no competing interests.
Funding
There was no funding for this project; authors are employees of the affiliations listed and there is a funded collaboration between the Center for Value-based Pharmacy Initiatives and Evernorth for projects of mutual interest.
Authors’ Contributions
CM, CBG, and UP conceived the study. SLG and AS provided access to data. SKP, YH, and CBG performed statistical analyses. ECS conducted the literature review, which was used by SKP for the initial draft of the manuscript. All authors contributed to data interpretation and review of the manuscript. All authors read and approved the final version.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Peasah, S.K., Swart, E.C.S., Huang, Y. et al. Disease-Modifying Medications in Patients with Rheumatoid Arthritis in the USA: Trends from 2016 to 2021. Drugs - Real World Outcomes 11, 241–249 (2024). https://doi.org/10.1007/s40801-024-00416-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-024-00416-3