Abstract
Background
Cardiac glycosides such as digoxin, digitoxin and ouabain are still used around the world to treat patients with chronic heart failure with reduced ejection fraction (HFrEF) and/or atrial fibrillation (AF). However, in the US, only digoxin is licensed for treating these illnesses, and the use of digoxin for this group of patients is increasingly being replaced in the US by a new standard of care with groups of more expensive drugs. However, ouabain and digitoxin, and less potently digoxin, have also recently been reported to inhibit SARS-CoV-2 virus penetration into human lung cells, thus blocking COVID-19 infection. COVID-19 is known to be a more aggressive disease in patients with cardiac comorbidities, including heart failure.
Objective
We therefore considered the possibility that digoxin might provide at least a measure of relief from COVID-19 in digoxin-treated heart failure patients. To this end, we hypothesized that treatment with digoxin rather than standard of care might equivalently protect heart failure patients with regard to diagnosis of COVID-19, hospitalization and death.
Methods
To test this hypothesis, we conducted a cross-sectional study by using the US Military Health System (MHS) Data Repository to identify all MHS TRICARE Prime and Plus beneficiaries aged 18–64 years with a heart failure (HF) diagnosis during the period April 2020 to August 2021. In the MHS, all patients receive equal, optimal care without regard to rank or ethnicity. Analyses included descriptive statistics on patient demographics and clinical characteristics, and logistic regressions to determine likelihood of digoxin use.
Results
We identified 14,044 beneficiaries with heart failure in the MHS during the study period. Of these, 496 were treated with digoxin. However, we found that both digoxin-treated and standard-of-care groups were equivalently protected from COVID-19. We also noted that younger active duty service members and their dependents with HF were less likely to receive digoxin compared with older, retired beneficiaries with more comorbidities.
Conclusion
The hypothesis of equivalent protection by digoxin treatment of HF patients in terms of susceptibility to COVID-19 infection appears to be supported by the data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Heart failure patients with a moderate or severe Charlson Comorbidity Index (CCI) score were more likely than those with a mild score to receive digoxin. |
The hypothesis of equivalent protection by digoxin treatment or standard of care of heart failure patients in terms of susceptibility to COVID-19 infection appears to be supported by the data. |
In the Military Health System (MHS, with ca. 9.6 million members), it cannot be excluded that digoxin and standard of care protect heart failure patients equivalently from COVID-19. |
1 Introduction
Cardiac glycosides such as digoxin, digitoxin, and ouabain are still used around the world to treat patients with chronic heart failure with reduced ejection fraction (HFrEF) and/or atrial fibrillation (AF) [1,2,3,4,5,6]. However, in the United States (US), only digoxin is licensed, and it has been increasingly replaced by a standard-of-care group of drugs which include renin-angiotensin aldosterone inhibitors (ARNI), β-blockers, mineralocorticoid receptor antagonists (MRA), and the SGLT2 inhibitor. However, a recent analysis using the Medical Expenditure Panel Survey (MEPS) showed that an increasing proportion of digoxin users in the US population at large are adults living at or below the federal poverty level [7]. Consistently, the yearly median out-of-pocket cost for standard of care is US$2217.00, whereas that for digoxin is only US$60.00. Other digoxin users in this category are those who self-identify as either Asian or Hispanic [7], and those with comorbidities which are inconsistent with standard of care [8, 9]. By contrast, the MEPS analysis also showed that digoxin use had declined among females and self-identified white adults [7].
Historically, because of the comorbidity problem, digoxin has been given, by design, both here in the US and elsewhere in the world, to the sickest patients who, by definition, have a higher mortality risk [6]. This strategy has caused previous clinical trials of digoxin to be subject to prescription bias, because digoxin was, by design, associated with lower overall survival [1, 6, 10]. However, current reexaminations of these older clinical trial data have led to the suggestion that use of digoxin may lead to overall survival outcomes “equal to or slightly better” than standard of care [3, 6, 11]. Consequently, digoxin may be experiencing a recurrence of interest as reexamination of old clinical trial data has revealed that negative conclusions for both digoxin and digitoxin needed to be reconsidered [11,12,13,14,15].
However, because the COVID-19 pandemic has impacted profoundly on those with concomitant cardiovascular comorbidities [16], we considered whether digoxin-treated patients might be more susceptible to COVID-19 than those treated with standard of care. The reason for this consideration was that increased comorbidities, as defined by the Charlson Comorbidity Index (CCI), have been widely seen to be associated with worse outcomes for COVID-19 [17,18,19,20]. By contrast, it has been reported that digitoxin and ouabain, and with lesser potency digoxin, interfere with penetration of the SARS-CoV-2 virus into human lung cells [21] and green monkey kidney cells [22]. We therefore hypothesized that treatment with digoxin rather than standard of care might equivalently protect heart failure patients with regard to diagnosis of COVID-19, hospitalization and death.
2 Methods
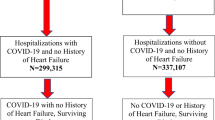
To test this hypothesis, we conducted a cross-sectional study using the US Military Health System (MHS) Data Repository (MDR) to identify all MHS TRICARE Prime and Plus beneficiaries ages 18–64 years with a heart failure (HF) diagnosis during the COVID-19 pandemic (April 1 2020 to August 31 2021). The MDR contains administrative and clinically comprehensive data for 9.6 million beneficiaries, including active duty personnel, retirees, and their family members. In the MHS, all patients receive care through universal health coverage irrespective of rank, gender, or ethnicity. Beneficiaries aged 65 years and older were excluded from analyses due to TRICARE becoming secondary payer to Medicare. Beneficiaries associated with—either as personnel or dependents—the National Guard or Reserves were also excluded due to their inconsistent access to care.
We subsequently identified all persons in our study population diagnosed with COVID-19 or COVID-19-related conditions, and who received digoxin, β-blockers, ACE inhibitors, and angiotensin receptor blockers during the study period, as well as those who were hospitalized or died during the study period. The CCI score was retrospectively calculated by the authors for each patient at the time of their HF diagnosis using International Classification of Diseases, 10th revision (ICD-10), diagnostic codes and used to account for comorbidities and increased risk of disease. The full list of diagnostic codes used to identify heart failure and COVID-19 or related conditions can be found in the electronic supplementary material.
Study analyses included descriptive statistics on patient demographic and clinical characteristics; chi-square tests for differences in demographics and clinical characteristics between those with and without COVID-19; and unadjusted and adjusted logistic regressions, with multiple imputations for missing race, which were used to assess any demographic and clinical associations of COVID-19 diagnosis in HF patients. Twenty iterations and all patient demographics, CCI score categories, and receipt of digoxin status were used in the imputation of race. Parameter estimates and Akaike information criterion (AIC) fit statistics from full and complete case analysis models were compared with imputed results to assess the quality and fit of regression analysis. All patient demographics, CCI scores, and receipt of digoxin were used as adjustment factors in the adjusted logistic regression models. Additional subset analyses stratified by patient demographics and clinical characteristics were performed to determine impact of digoxin on patients with heart failure. All analyses were performed using SAS 9.4. This research was reviewed and determined exempt from human subjects oversight by the Uniformed Services University of the Health Sciences Institutional Review Board.
3 Results
We identified 14,044 beneficiaries with HFrEF during the study period. Of these, 10.6% were diagnosed with COVID-19; 3.5% were treated with digoxin; 27.1% were hospitalized; and 1.9% died during the study period. Among the subset diagnosed with COVID-19, 3.4% were treated with digoxin; 44.8% were hospitalized; and 3.3% died (Table 1). In addition, COVID-19 patients had systematically higher values of comorbidity above mild scores compared with those without COVID-19. Chi-square tests found differences across demographic and clinical characteristics, excluding gender, service, receipt of digoxin, ACE inhibitors and receptors, and other systemic and connective-tissue–related conditions (Table 1). However, these differences in COVID-19 diagnosis were statistically insignificant (Table 2).
Nonetheless, multivariate logistic regressions with imputed race revealed statistically significant associations with age group, officer ranks, and mild CCI score category. For example, all age groups under the referent of 55–64 years were more likely to have COVID-19, with ages 18–24 years having the highest odds (OR 1.63; 95% CI 1.20–2.20). Those associated with Junior (OR 0.69, 95% CI 0.51–0.92) and Senior Officer ranks (OR 0.76, 95% CI 0.63–0.93) were less likely to have COVID-19 compared with those associated with a Senior Enlisted rank. However, patients with a mild CCI score (OR 0.57; 95% CI 0.47–0.71) were also less likely to receive digoxin when compared with patients with no score.
Descriptive and inferential statistics of data from patients prescribed digoxin can be found in Table 3. Use of Chi-square tests revealed statistically significant differences across age groups, beneficiary status, rank, and CCI score. In addition, multivariate logistic regression results found statistically significant associations among beneficiary status and CCI score only. Dependents of active duty personnel with HF were less likely to receive digoxin (OR 0.50, 95% CI 0.26–0.95) compared with retirees, and those with a moderate (OR 1.70, 95% CI 1.38–2.09) or severe CCI score (OR 1.60, 95% CI 1.18–2.18) were more likely than those with a mild score to receive digoxin.
4 Discussion
As hypothesized, these data indicate that digoxin, given to the HF patients with the most comorbidities, and standard of care given to those with the least comorbidities, equivalently protected against COVID-19. The hypothesis of equivalent protection by digoxin treatment of HF patients in terms of susceptibility to COVID-19 infection thus appears to be supported by the data. Whether the same can be said for digitoxin, which is a more potent inhibitor of viral penetration [21], may soon be known when analysis is completed for the DIGIT-HF trial [1]. We are also aware that ouabain, the most potent inhibitor of viral penetration, may eventually have a role to play in viral defense. However, to the best of our knowledge, no trial is ongoing.
An additional inference from this analysis, at least as it might inform regarding current digoxin treatment in the US population at large, is that the socioeconomic relegation of digoxin to the poor, to certain ethic groups, and to those with relevant comorbidities [7] does not necessarily carry with it a poor outcome for either HF treatment or resistance to COVID-19. However, an important caveat is that optimal care, as provided by the MHS to all patients, could be contributing to the equivalent outcome.
Indeed, in contrast to the US population at large, the MHS population of the youngest patients, as marked by their representation as service members and their dependents, and independent of ethnicity, race or gender, are less frequently prescribed digoxin than the older patients/beneficiaries (see Table 2). The older beneficiaries have larger numbers of comorbidities than the younger active duty service members and their families, and are therefore more likely to be prescribed digoxin. Thus, the rationale for who is prescribed digitoxin to treat HF in the US population at large is the inverse of the MHS population. In addition, we noted that HF patients treated with digoxin were also more likely to be prescribed β-blocker drugs (see Table 3).
There are limitations to this study. It is a limitation that there is a smaller number of digoxin-treated patients compared with those receiving standard of care. However, this is also generally the case for the comparison study of the US population at large [7]. Furthermore, it is a limitation that the MHS patients were all in the age range of 18–64 years. However, the racial/ethnic/gender demographics of our two groups were comparable, thus providing further support for our findings, regardless of the limitations [7]. It is also a limitation that it cannot be excluded that digoxin-dependent blockade of SARS-CoV-2 penetration into target cells [21,22,23] may have contributed to successful resistance to COVID-19 infection by HF patients receiving digoxin. However, further tests of this possibility will have to be left for future studies. Furthermore, the use of administrative claims data can lead to underestimation of prevalence and comorbidities, and there is the potential for unseen confounders or biases; both points are additional limitations of the study. Lastly, this cross-sectional study can only provide observed associations; other criteria such as experimental study designs, temporality, and repeatability from further studies are needed to prove or disprove causation.
5 Conclusion
The hypothesis of equivalent protection by digoxin treatment of HF patients in terms of susceptibility to COVID-19 infection appears to be supported by the data. In the MHS (which has ca. 9.5 million members), it cannot be excluded that digoxin and standard of care protect HF patients equivalently from COVID-19.
Data Availability Statement
The data that support the findings of this study are available from the United States Department of Defense, Defense Health Agency. Restrictions apply to the availability of these data, which were used under federal Data User Agreements for the current study, and so are not publically available.
References
Bavendiek U, Berliner D, Dávila LA, Schwab J, Maier L, Philipp SA, et al. Rationale and design of the DIGIT-HF trial (DIGitoxin to Improve ouTcomes in patients with advanced chronic Heart Failure): a randomized, double-blind, placebo-controlled study. Eur J Heart Fail. 2019;21(5):676–84. https://doi.org/10.1002/ejhf.1452.
Konstantinou DM, Karvounis H, Giannakoulas G. Digoxin in heart failure with a reduced ejection fraction: a risk factor or a risk marker. Cardiology. 2016;134(3):311–9. https://doi.org/10.1159/000444078.
Kotecha D, Bunting KV, Gill SK, Mehta S, Stanbury M, Jones JC, et al. Effect of digoxin vs bisoprolol for heart rate control in atrial fibrillation on patient-reported quality of life: the RATE-AF randomized clinical trial. JAMA. 2020;324(24):2497–508. https://doi.org/10.1001/jama.2020.23138.
Pervaiz MH, Dickinson MG, Yamani M. Is digoxin a drug of the past? Cleve Clin J Med. 2006;73(9):821–4. https://doi.org/10.3949/ccjm.73.9.821. (6, 9–32 passim).
Rosca CI, Kundnani NR, Tudor A, Rosca MS, Nicoras VA, Otiman G, et al. Benefits of prescribing low-dose digoxin in atrial fibrillation. Int J Immunopathol Pharmacol. 2021. https://doi.org/10.1177/20587384211051955.
Bavendiek U, Aguirre Davila L, Koch A, Bauersachs J. Assumption versus evidence: the case of digoxin in atrial fibrillation and heart failure. Eur Heart J. 2017;38(27):2095–9. https://doi.org/10.1093/eurheartj/ehw577.
Alahmed AA, Lauffenburger JC, Vaduganathan M, Aldemerdash A, Ting C, Fatani N, et al. Contemporary trends in the use of and expenditures on digoxin in the United States. Am J Cardiovasc Drugs. 2022. https://doi.org/10.1007/s40256-022-00540-x.
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136(6):e137–61. https://doi.org/10.1161/cir.0000000000000509.
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200. https://doi.org/10.1093/eurheartj/ehw128.
Friberg L, Hammar N, Rosenqvist M. Digoxin in atrial fibrillation: report from the Stockholm Cohort study of Atrial Fibrillation (SCAF). Heart. 2010;96(4):275–80. https://doi.org/10.1136/hrt.2009.175786.
Eichhorn EJ, Gheorghiade M. Digoxin–new perspective on an old drug. N Engl J Med. 2002;347(18):1394–5. https://doi.org/10.1056/NEJMp020118.
Gheorghiade M, Fonarow GC, van Veldhuisen DJ, Cleland JG, Butler J, Epstein AE, et al. Lack of evidence of increased mortality among patients with atrial fibrillation taking digoxin: findings from post hoc propensity-matched analysis of the AFFIRM trial. Eur Heart J. 2013;34(20):1489–97. https://doi.org/10.1093/eurheartj/eht120.
Patel NJ, Hoosien M, Deshmukh A, Badheka AO, Grover PM, Shah N, et al. Digoxin significantly improves all-cause mortality in atrial fibrillation patients with severely reduced left ventricular systolic function. Int J Cardiol. 2013;169(5):e84–6. https://doi.org/10.1016/j.ijcard.2013.10.040.
Mulder BA, Van Veldhuisen DJ, Crijns HJ, Tijssen JG, Hillege HL, Alings M, et al. Digoxin in patients with permanent atrial fibrillation: data from the RACE II study. Heart Rhythm. 2014;11(9):1543–50. https://doi.org/10.1016/j.hrthm.2014.06.007.
Rathore SS, Wang Y, Krumholz HM. Sex-based differences in the effect of digoxin for the treatment of heart failure. N Engl J Med. 2002;347(18):1403–11. https://doi.org/10.1056/NEJMoa021266.
Italia L, Tomasoni D, Bisegna S, Pancaldi E, Stretti L, Adamo M, et al. COVID-19 and heart failure: from epidemiology during the pandemic to myocardial injury, myocarditis, and heart failure sequelae. Front Cardiovasc Med. 2021;8: 713560. https://doi.org/10.3389/fcvm.2021.713560.
Kim DH, Park HC, Cho A, Kim J, Yun KS, Kim J, et al. Age-adjusted Charlson comorbidity index score is the best predictor for severe clinical outcome in the hospitalized patients with COVID-19 infection. Medicine (Baltimore). 2021;100(18): e25900. https://doi.org/10.1097/md.0000000000025900.
Salaffi F, Carotti M, Di Carlo M, Ceccarelli L, Galli M, Sarzi-Puttini P, et al. Predicting Severe/Critical Outcomes in Patients With SARS-CoV2 Pneumonia: development of the prediCtion seveRe/crItical ouTcome in COVID-19 (CRITIC) Model. Front Med (Lausanne). 2021;8: 695195. https://doi.org/10.3389/fmed.2021.695195.
Christensen DM, Strange JE, Gislason G, Torp-Pedersen C, Gerds T, Fosbøl E, et al. Charlson Comorbidity Index Score and Risk of Severe Outcome and Death in Danish COVID-19 Patients. J Gen Intern Med. 2020;35(9):2801–3. https://doi.org/10.1007/s11606-020-05991-z.
TutyKuswardhani RA, Henrina J, Pranata R, Anthonius Lim M, Lawrensia S, Suastika K. Charlson comorbidity index and a composite of poor outcomes in COVID-19 patients: a systematic review and meta-analysis. Diabetes Metab Syndr. 2020;14(6):2103–9. https://doi.org/10.1016/j.dsx.2020.10.022.
Caohuy H, Eidelman O, Chen T, Liu S, Yang Q, Bera A, et al. Common cardiac medications potently inhibit ACE2 binding to the SARS-CoV-2 Spike, and block virus penetration and infectivity in human lung cells. Sci Rep. 2021;11(1):22195. https://doi.org/10.1038/s41598-021-01690-9.
Cho J, Lee YJ, Kim JH, Kim SI, Kim SS, Choi BS, et al. Antiviral activity of digoxin and ouabain against SARS-CoV-2 infection and its implication for COVID-19. Sci Rep. 2020;10(1):16200. https://doi.org/10.1038/s41598-020-72879-7.
Caohuy H, Eidelman O, Chen T, Yang Q, Walton NI, Pollard HB. Inflammation in the COVID-19 airway is due to inhibition of CFTR signaling by the SARS-CoV-2 Spike protein. bioRxiv. 2022. https://doi.org/10.1101/2022.01.18.476803.
Acknowledgements
We gratefully acknowledge support for this work by the Center for Health Services Research (CHSR), Grant no. HU0001-20-20035 (PI: Koehlmoos TP); by the Consortium for Health and Military Performance (CHAMP), supported by Warfighter Readiness: Optimizing Human Performance (HU00011920047; MEM-91-10314 [PI: Deuster PA]); and by Intramural Research Program Award, Grant no. APG-70-12301 (PI: Pollard HB). We are grateful to Drs Mark Kortepeter and Patricia Deuster, and to Mr.Walter Tinling, and Bette S. Pollard for thoughtful suggestions at different stages of the analysis. The contents of this presentation are the sole responsibility of the authors and do not necessarily reflect the views, assertions, opinions or policies of the Uniformed Services University of the Health Sciences (USUHS), The Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc. (HJF), the Department of Defense (DoD), or the Departments of the Army, Navy, or Air Force. Mention of trade names, commercial products, or organizations does not imply endorsement by the US Government.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the final submitted manuscript, and agree to be accountable for the work. HBP, ALB and TPK planned the study. ALB performed statistical analysis. HBP, TPK and ALB analyzed the data and wrote the paper. All authors meet the four ICMJE criteria for authorship.
Corresponding author
Ethics declarations
Code availability
Not applicable.
Ethics Approval
This research was reviewed and determined exempt from human subjects oversight by the Uniformed Services University of the Health Science’s Institutional Review Board.
Funding
The study was funded by U.S. Department of Defense (Grant nos.: APG-70-12301, HU0001-20-20035).
Conflict of interest/competing of interest
There are no conflicts of interest.
Consent for publication
USU Publication Submission Approval number REQ0024590.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Banaag, A.L., Pollard, H.B. & Koehlmoos, T.P. Digoxin and Standard-of-Care Therapy for Heart Failure Patients with COVID-19: Analysis of Data from the US Military Health System (MHS) Data Repository. Drugs - Real World Outcomes 10, 299–307 (2023). https://doi.org/10.1007/s40801-023-00360-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-023-00360-8