Abstract
Background
The coronavirus disease 2019 (COVID-19) pandemic has led to disruptions of healthcare delivery and may thus have impacted patterns of prescription opioid use, including risk factors for long-term use.
Objective
We aimed to describe changes in patterns of prescription opioid use due to the COVID-19 pandemic in community-dwelling adults without a cancer diagnosis.
Methods
Using administrative claims data of the province of Quebec, Canada, a random sample of adults (aged ≥18 years) was selected. These were members of the public drug plan without a cancer diagnosis who initiated a prescription opioid in the outpatient setting between 1 January, 2018 and 28 December, 2020. We assessed the daily dose of initial prescription opioids, the number of days’ supply of initial dispensing, and the total duration of opioid use over the first 6 months following initiation. We applied interrupted autoregressive integrated moving average models to examine weekly patterns of prescription opioids before and during the pandemic (starting at the lockdown). Our models included a step intervention function (immediate change) and a ramp intervention function (slope change).
Results
There were 112,650 and 34,261 patients who initiated opioid therapy, respectively, in the 115-week pre-pandemic period and in the 41-week pandemic period. At the start of the lockdown, there was a significant immediate decrease in opioid treatment initiation (−326; 95% confidence interval [CI] −419 to −234) and initial daily dose (−1.7 morphine milligram equivalents; 95% CI −2.7 to −0.7). Conversely, there was a significant immediate increase in the number of days’ supply of initial dispensing (1.4 days; 95% CI 1.0 to 1.8) and the total duration of opioid use over 6 months (5.7 days; 95% CI 4.6 to 6.8). All these weekly measures returned to values close to those of the pre-pandemic period 10 weeks after the start of lockdown.
Conclusions
Our findings showed that the COVID-19 lockdown had an impact on initial number of days’ supply, which is a risk factor for long-term use and ultimately opioid-related harm. However, over time, prescription practices and use reverted to those observed in the pre-pandemic period.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A decrease in opioid treatment initiation and initial daily dose, paralleled by an increase in opioid initial number of days’ supply and total duration of therapy were observed during the lockdown period. |
Ten weeks after the start of lockdown, the patterns of prescription opioid use reverted to those observed before the lockdown. |
1 Introduction
The coronavirus disease 2019 (COVID-19) pandemic has disrupted healthcare delivery worldwide. In the province of Quebec, Canada, a state of health emergency was declared on 13 March, 2020, in response to the increasing number of COVID-19 cases. On 16 March, 2020, several mitigation measures were enforced to slow the spread of the virus [1]. People were urged to stay at home, while healthcare professionals restricted patient interactions to urgent and essential services. These restrictions were maintained for several weeks and led to the interruption of elective procedures, a decrease in physician and emergency department visits, and a shift to telemedicine across Canada [3]. Some of the pharmacists’ legal activities were also relaxed, and included, among others, the prolongation of prescriptions for periods extending beyond the maximum periods provided for by law, the prescription of drugs for all minor conditions (under certain restrictions), and the substitution of drugs for those from another therapeutic subclass.
Previous studies have assessed changes in medication prescribing resulting from the COVID-19 pandemic. In Texas, USA, patients with chronic low back pain used less nonsteroidal anti-inflammatory drugs, whereas opioid use remained unchanged [4]. In the province of Ontario, Canada, more nursing home residents were dispensed opioids, antipsychotics, and antidepressants during the pandemic [5].
Another impact of the COVID-19 pandemic has been the exacerbation of the opioid-related overdose crisis in North America. In Kentucky, USA, the number of emergency department visits for opioid overdoses increased by 17% compared with the period of January–February 2020 [6]. The province of British Columbia, Canada reported a growing number of opioid-related deaths in the month of June 2020 in contrast to June 2019 [7].
Long-term opioid use is a known predictor of opioid-related harm [8,9,10,11,12,13,14]. Previous studies have shown that the number of days’ supply of the initial dispensing beyond 7 days [15] or 15 days [16] increases the risk of progressing to long-term opioid use. As an attempt to curb the opioid epidemic in Canada, which was officially declared on 14 April, 2016 [17], several policies and risk minimization activities have been implemented over the past decade, such as drug scheduling to increase the accessibility to naloxone, communication to healthcare professionals and/or patients, as well as interventions at the point of care (e.g., opioid stickers in pharmacies, triplicate prescriptions, prescription monitoring programs Goyer et al.,2). In the context of the Canadian Specific Opioid targeted Risk Management Plan [18], we ought to know whether the COVID-19 pandemic has modified the effectiveness of risk minimization efforts, including those that aim at optimizing opioid prescribing.
Owing to a decreased potential for monitoring practices, we hypothesized that reduced access to prescribers during the COVID-19 pandemic has altered patterns of prescription opioid use, including those that are risk factors for opioid-related harm such as an increase in the number of tablets dispensed. In this retrospective cohort study, conducted in the community-dwelling adult population without a cancer diagnosis who initiated a prescription opioid in Quebec, Canada, we aimed at describing changes in the patterns of use before and during the COVID-19 pandemic.
2 Methods
2.1 Design
We conducted a retrospective cohort study of adults (aged ≥18 years) without a cancer diagnosis who initiated a prescription opioid (new user design) in the outpatient setting in the province of Quebec, Canada. Using administrative claims data, we assessed the distribution over time of patients who initiated a prescription opioid and the patterns of opioid use (product dispensed, daily dose expressed in morphine milligram equivalent, initial number of days’ supply, total duration of opioid use over the first 6 months after initiation). We compared patterns observed during the period prior to the start of the COVID-19 pandemic (1 January, 2018 to 15 March, 2020) to those during the pandemic (16 March, 2020 [start of the lockdown in Quebec] to 28 December, 2020). As an attempt to identify subpopulations most affected by the pandemic, we performed comparisons within each potential indication for opioid initiation (acute pain including surgery, chronic pain, or other).
2.2 Data Sources
We used three administrative claims databases (drug dispensing database, medical database, and beneficiary database), managed by the public healthcare program of Quebec (Régie de l’assurance maladie du Québec, RAMQ), via a deterministic linkage using the patient health insurance number. In Quebec, there is universal coverage of medical services regardless of a patient’s socio-economic status. However, the public drug plan covers the majority (94%) of elderly people (aged ≥65 years), welfare recipients, and residents whose medication costs are not covered by private insurance (about 43% of residents aged <65 years). The beneficiary database includes sociodemographic characteristics (age group, sex, region of residence), level of copay, and coverage periods. The drug dispensing database contains dispensing date, drug code, number of units, dose per unit, number of days’ supply, and prescriber’s specialty related to drugs covered by the plan. There is no information on in-hospital and over-the-counter medications, nor on indication. The medical services database records inpatient, outpatient, and emergency department services that are billed on a fee-for-service. These include medical visits and related diagnoses coded using the International Classification of Diseases, Ninth Revision as well as procedures and laboratory tests (although no results are available).
2.3 Study Population
The study population was that of community-dwelling adults (aged ≥18 years) initiating a prescription opioid (butorphanol, codeine, fentanyl, hydromorphone, meperidine, morphine, oxycodone, or pentazocine, in monotherapy or in combination) in the outpatient setting between 1 January, 2018 and 28 December, 2020. We selected the start date of 1 January, 2018 to provide a baseline of approximately 2 years prior to the start of the lockdown due to COVID-19 (16 March, 2020 in Quebec) and the end date of 28 December, 2020 to keep only complete weeks in the analyses. We required that individuals had continuous enrollment in the Quebec public drug plan for at least 12 months before opioid initiation (index date) and until 28 December, 2020. Therefore, patients who died during the study period were excluded in order to avoid right censoring of the data on opioid duration. We excluded patients with a cancer diagnosis (International Classification of Diseases, Ninth Revision, codes 140-239.9) recorded in medical services claims at any time during the whole study period. In accordance with the new user design, we only included patients who initiated a prescription opioid treatment and excluded all users who received an opioid dispensing during the 12 months before the index date. As per the data-sharing agreement, the RAMQ selected a random sample of the eligible population, as it was not possible for data privacy purposes to analyze the entire population. Because the eligibility assessment was conducted by the RAMQ, it is not possible to describe the flow of patients through all stages of the selection process. Patients who initiated a prescription opioid more than once during the study period were only included once in the cohort (at the first eligible index date).
2.4 Variables
We assessed patterns of opioid use at the index date and over the 6 months following treatment initiation. At the index date, we determined the product dispensed (including concomitant opioid use), mode of action (short-acting or long-acting, or both), potential indication for opioid initiation (acute pain, chronic pain, other), initial number of days’ supply, prescribed daily dose, as well as total duration over 6 months following treatment initiation. Because indication is not available in the drug dispensing database, we derived the potential indication for opioid initiation using a diagnosis-based and procedure-based algorithm [16]. We defined three mutually exclusive categories: (i) diagnosis or procedure associated with acute pain (presence of a billing code for surgical procedure, accident, or fracture) in the 7 or 30 days prior to the index date, depending on diagnosis/procedure, or index opioid prescribed by a dentist; (ii) none of the above and medical visits with a diagnosis associated with chronic pain (arthritis, spinal stenosis, fibromyalgia, osteoporosis, spinal deformity, neuropathy, abscess, or limb, neck, abdominal, thoracic, tendon, renal colic, or digestive system pain) in the 12 months prior to the index date; (iii) none of the above and an inpatient visit billed within 7 days prior to the index date or no records of events potentially associated with opioid initiation. We derived the daily dose of prescription opioids from dispensing claims using dose per unit, number of units dispensed, and initial number of days’ supply. It was expressed as morphine milligram equivalents using conversion factors described in a previous study [16]. Over the 6 months following opioid initiation, we calculated the total duration of opioid use (for patients with at least 6 months of follow-up) using opioid refill dates and the number of days’ supply. When the same product was renewed during the follow-up period, the total duration of use was the sum of the individual number of days’ supply, up to a maximum of 6 months. If a hospitalization occurred during an active opioid prescribing period, without any opioid dispensing after discharge, the patient was assumed not to have taken the opioid during hospitalization. Conversely, a patient who was hospitalized during a period of opioid treatment and received another dispensation after discharge (at any time) was assumed to have continued treatment during hospitalization and the hospital length of stay was added to the total duration of use.
At the index date, we assessed the following patient characteristics as covariables: age group (18–44, 45–54, 55–64, 65–74, 75–84, ≥85 years), sex, region of residence (urban, semi-urban, rural), and socioeconomic status (using the level of copay as a proxy for income, categorized into: beneficiary of drug program (<65 years), low income (≥65 years), medium income (≥65 years), high income (≥65 years), welfare recipient). We calculated the Charlson Comorbidity Index (CCI) using medical claims recorded in the 12 months prior to the index date as an indicator of overall health status given that the CCI is a predictor of the risk of dying in the following year [19]. The CCI was categorized into 0, 1, 2, 3, and ≥4.
2.5 Statistical Analysis
We performed descriptive analyses of patient baseline characteristics (age group, sex, region of residence, socioeconomic status, CCI) and patterns of opioid use (index opioid, mode of action, potential indication for opioid) stratified by period (pre-pandemic and pandemic). We calculated standardized differences, which measure the effect size between two groups, to compare these characteristics between periods. A standardized difference <0.10 indicated a negligible difference in characteristics between periods [20]. We assessed prescription opioid patterns using the following measures: (i) prescription rate (number of patients initiating prescription opioids); (ii) opioid dispensed at the index date; (iii) prescribed daily dose of index opioid; (iv) number of days’ supply of index opioid; and (v) total duration of opioid use over the first 6 months following opioid initiation (for patients with at least 6 months of follow-up).
To measure trends over time in prescription practices, we used interrupted autoregressive integrated moving average (ARIMA) models to examine the association of the pandemic with patterns of prescription opioids. As we received a random sample of the eligible population, the distribution of the weekly number of patients initiating a prescription opioid was an accurate estimator of prescription rate. The number of patients initiating prescription opioids was examined for all opioids combined and separately for hydromorphone, morphine, and oxycodone (the three most frequently used index opioids). Because long-acting opioids only accounted for approximately 1% of the dispensed opioids, it was not feasible to stratify by long-acting versus short-acting. We also determined trends over time in the prescribed daily dose of index opioids, number of days’ supply of index opioids, and total duration of opioid use over 6 months, measured as mean per week. The ARIMA models allowed an examination of changes in patterns of prescription opioids while accounting for autocorrelation between consecutive weekly observations and seasonality [21]. The pre-pandemic period covered 115 weeks, while the pandemic period, starting on 16 March, 2020, covered 41 weeks.
To estimate the immediate and long-term impacts of the pandemic on patterns of prescription opioids, our models included a step intervention function (immediate change) and a ramp intervention function (slope change) [22]. We used an automated algorithm in the forecast package for R, to identify the ARIMA model terms [23]. This algorithm iteratively searches over a series of potential ARIMA models for the one with the lowest Akaike information criterion or Bayesian information criterion, with several constraints applied to avoid convergence problems. We examined the fit of the model using autocorrelation function and partial autocorrelation function plots, normality plots of the model residuals, and Ljung–Box tests for stationarity.
We then fit those ARIMA models to the pre-pandemic period in order to forecast weekly patterns of prescription opioids during the pandemic period. Therefore, we could compare observed outcomes during the pandemic period with the projected outcomes in the hypothetical absence of a pandemic.
We also stratified the analyses by potential indication for opioid initiation (acute versus chronic pain) and age group (18–64 years and ≥65 years) for all outcomes. The cohort was programmed using SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA) and the R package was used for the ARIMA analyses [24].
3 Results
Out of the 294,633 individuals who met the inclusion and exclusion criteria, a random sample of 146,911 new users of prescription opioids was available. A total of 112,650 individuals initiated therapy over the 115-week pre-pandemic period and 34,261 over the 41-week pandemic period. As shown in Table 1, all sociodemographic characteristics and the CCI were below the threshold of a 0.10 standardized difference, meaning that there were no differences in the characteristics of patients who initiated treatment before and during the pandemic.
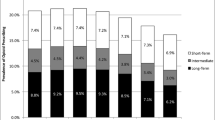
The characteristics of opioid prescriptions dispensed at treatment initiation are summarized in Table 2. In both the pre-pandemic and pandemic periods, the most frequent opioid prescriptions dispensed were hydromorphone (47.6% and 52.3%), morphine (33.2% and 33.8%), and oxycodone (11.7% and 10.5%), and patients were mostly dispensed short-acting opioids (98.9% and 98.8%). Codeine prescriptions decreased from 6.6% in the pre-pandemic period to 2.8% during the pandemic period, with a standardized difference of 0.18. Potential indication for chronic pain, which decreased from 40.0% to 34.9%, and other potential indications, which increased from 37.2% to 45.7%, were above the threshold of a 0.10 standardized difference.
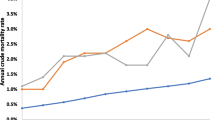
Figures 1 and 2 illustrate weekly measures for all outcomes, and forecasts in the absence of a pandemic. The frequency of an initial prescription opioid presented seasonal fluctuations over the pre-pandemic period (Fig. 1). At the onset of the pandemic, there was a significant immediate decrease of 326 weekly treatment initiations (95% confidence interval [CI] −419 to −234), while the slope change further represented an increase of 8 weekly treatment initiations (95% CI 4 to 12) (Fig. 1a, Table 3). There was a relative difference of −49.5% in the observed versus forecasted number of opioid treatment initiations in the first week of the pandemic (Table 3). Initiation of hydromorphone, morphine, and oxycodone followed similar trends during the pandemic period (Fig. 1b–d, Table 3).
The daily dose of the index opioid significantly decreased by 1.7 morphine milligram equivalents (95% CI −2.7 to −0.7) at the beginning of the pandemic (Fig. 2a, Table 3). In contrast, the mean number of initial days’ supply significantly increased as demonstrated by the step change of 1.4 days (95% CI 1.0 to 1.8) (Fig. 2b, Table 3). A similar trend was observed for the total duration of opioid use over 6 months, with an immediate increase of 5.7 days (95% CI 4.6 to 6.8) (Fig. 2c, Table 3). The initial decrease in initial daily dose reverted and over time, actually increased by 0.05 weekly. Conversely, the initial increase in the number of initial days’ supply and in the total duration of opioid use over 6 months reverted and over time decreased by 0.03 and 0.3 weekly, respectively (Table 3). Of note, the initial number of days’ supply and total duration presented a decline tendency over the pre-pandemic period (Fig. 2b, c).
Approximately 10 weeks after the start of the pandemic, all weekly measures returned to values close to the pre-pandemic period and did not differ from the forecasted values (Figs. 1, 2). The results of the stratified analyses by potential indication and by age groups for all measures were consistent with the main analyses. Notably, for the strata of chronic pain (potential indication) and age ≥65 years, the mean number of initial days’ supply was 7 days in the first week of the pandemic (Tables S1–4 in the Electronic Supplementary Material).
4 Discussion
In this retrospective cohort study, the COVID-19 pandemic was significantly associated with an immediate decrease in both the number of patients initiating a prescription opioid and the initial opioid daily dose. Lower morphine milligram equivalents prescribed may be because of less opportunity for monitoring during a period where access to a healthcare professional was impaired. Conversely, there was a significant immediate increase in the number of days supply dispensed at the index date and in the total duration of opioid use over 6 months after opioid initiation, which is consistent with our hypothesis that reduced access to healthcare may result in larger prescription fills. These were shown to be risk factors for long-term opioid use and ultimately, opioid-related harm [16]. The magnitude of the slope change was small for the measures of prescription opioid patterns and the observed and forecasted values did not differ approximately 10 weeks after the start of the pandemic. In Quebec, as the incidence of COVID-19 cases started to drop in June 2020 (until the start of the second wave in September–October 2020), some mitigation measures were lifted by the authorities [1]. Therefore, the healthcare system might have been able to accommodate the demand of patients other than those with COVID-19, which might explain the minor long-term impact of the pandemic in the initiation of prescription opioids in our study.
Our findings corroborate estimates from Ontario where the rate of individuals receiving at least one claim for prescription opioids decreased from March to April 2020 (from 8.15 to 7.23 per 1000 persons) and then increased in July 2020 (to 8.07 per 1000 persons) [25]. Conversely, in nursing homes in the same province, the impact of the pandemic was noticeable after June 2020 when 1% more residents were dispensed an opioid [5]. These divergent findings may be explained by differences in populations, namely that nursing home residents were older and frailer than the population covered by the public drug plan in Quebec included in our study.
Our study may reveal some concerns related to therapy duration as the mean number of initial opioid days’ supply increased to approximately 7 days during the early stage of the pandemic period, particularly for the elderly and for patients with a potential indication of chronic pain. Previous studies suggest that initial opioid prescriptions should not exceed 7 days [15, 16]. However, the increase of initial number of days’ supply observed at the beginning of the pandemic was temporary and offset by a decrease in initial daily dose. Moreover, the total duration of opioid use over a 6-month period was 18 days at its peak, which does not indicate a tendency for long-term opioid use (i.e., treatment for more than 3 months) [26].
Additionally, we observed the trends of prescription opioid patterns during the pre-pandemic period. First, there was a seasonal effect in opioid initiation, with lower numbers around end-of-year holidays and summer (likely because of vacation time in Canada). Second, the number of initial days’ supply decreased over time, possibly owing to changes in prescription practices and as a response to the implementation in Canada of opioid drug policies and regulatory measures, such as the Canadian Specific Opioid targeted Risk Management Plan.
The main strengths of our study are the analysis of a large cohort of individuals and the long time period before the pandemic (115 weeks) in the ARIMA model to predict the patterns of prescription opioids in the hypothetical absence of a pandemic. Our study also has some potential limitations. First, the use of pharmacy claims to measure medication utilization may not reflect the real medication use by the individuals. Second, we could not determine the actual indication for opioid therapy. However, we applied a comprehensive algorithm to identify diagnoses and procedures related to acute and chronic pain as well as other potential indications [16]. Finally, our study population represents residents of Quebec covered by the public drug plan (the vast majority of the elderly and close to half of the population aged 18–64 years), and our findings may not be generalizable to others without these benefits.
5 Conclusions
The COVID-19 pandemic has placed pressure on healthcare systems and resources, including prescription drugs. For high-risk drugs, such as opioids, which are currently under increased scrutiny, we found that patterns of prescription opioids were temporally affected by the pandemic; however, we did not detect a critical long-term impact. Further investigations should continue to evaluate the effect of a pandemic on factors associated with opioid-related harm and death. Monitoring changes in prescribing behaviors during the pandemic is crucial to tailor health programs aimed at reducing morbidity and mortality associated with prescription opioid usage.
References
Institut National de Santé Publique du Québec (INSPQ). Ligne du temps COVID-19 au Québec. https://www.inspq.qc.ca/covid-19/donnees/ligne-du-temps. Accessed 21 Sep 2021.
Goyer C, Castillon G, Moride Y. Implementation of interventions and policies on opioids and awareness of opioid-related harms in Canada: a multistage mixed methods descriptive study. Int J Environ Res Public Health. 2022;19(9):5122.
Canadian Institute for Health Information (CIHI). Impact of COVID-19 on Canada’s health care systems. https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems. Accessed 17 Jun 2022.
Licciardone JC. Impact of COVID-19 on utilization of nonpharmacological and pharmacological treatments for chronic low back pain and clinical outcomes. J Osteopath Med. 2021;121(7):625–33. https://doi.org/10.1515/jom-2020-0334.
Campitelli MA, Bronskill SE, Maclagan LC, et al. Comparison of medication prescribing before and after the COVID-19 pandemic among nursing home residents in Ontario, Canada. JAMA Netw Open. 2021;4(8): e2118441. https://doi.org/10.1001/jamanetworkopen.2021.18441.
Slavova S, Rock P, Bush HM, Quesinberry D, Walsh SL. Signal of increased opioid overdose during COVID-19 from emergency medical services data. Drug Alcohol Depend. 2020;214: 108176. https://doi.org/10.1016/j.drugalcdep.2020.108176.
Norton A, Kerr T. Applying the lessons of COVID-19 response to Canada’s worsening opioid epidemic. EClinicalMedicine. 2020;29: 100633. https://doi.org/10.1016/j.eclinm.2020.100633.
Duarte R, Raphael J. The pros and cons of long-term opioid therapy. J Pain Palliat Care Pharmacother. 2014;28:308–10.
Ballantyne JC. “Safe and effective when used as directed”: the case of chronic use of opioid analgesics. J Med Toxicol. 2012;8:417–23.
Burgess HJ, Siddiqui A, Burgess FW. Long-term opioid therapy for chronic pain and the risk of opioid addiction. R I Med J. 2013;2014(97):25–8.
Häuser W, Bock F, Engeser P, et al. Long-term opioid use in non-cancer pain. Dtsch Arztebl Int. 2014;111:732–40.
Noble M, Tregear SJ, Treadwell JR, et al. Long-term opioid therapy for chronic noncancer pain: a systematic review and meta-analysis of efficacy and safety. J Pain Symptom Manage. 2008;35:214–28.
Special Advisory Committee on the Epidemic of Opioid Overdoses. National report: apparent opioid-related deaths in Canada January 2016 to June 2017 [web-based report] (Public Health Agency of Canada, Ottawa). 2018. www.canada.ca/en/public-health/services/publications/healthy-living/national-report-apparent-opioid-related-deaths-released-march-2018.html. Accessed 13 Jun 2022.
Institut national de santé publique du Québec. Décès attribuables aux intoxications par opioïdes au Québec, 2000 à 2012: mise à jour 2013–2016. https://www.inspq.qc.ca/sites/default/files/publications/2298_deces_attribuables_opioides.pdf. Accessed 17 Jun 2022.
Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long-term opioid use: United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):265–9.
Béliveau A, Castilloux AM, Tannenbaum C, et al. Predictors of long-term use of prescription opioids in the community-dwelling population of adults without a cancer diagnosis: a retrospective cohort study. CMAJ Open. 2021;9(1):E96-106. https://doi.org/10.9778/cmajo.20200076.
House of Commons. Standing Committee on Health. Report and recommendations on the opioid crisis in Canada (December 2016). https://www.ourcommons.ca/Content/Committee/421/HESA/Reports/RP8685723/hesarp06/hesarp06-e.pdf. Accessed 17 Jun 2022.
Health Canada. Submission of targeted risk management plans and follow-up commitments for prescription opioid-containing products: guidance for industry. 2018. https://www.canada.ca/en/health-canada/services/drugs-health-products/reports-publications/medeffect-canada/submission-targeted-rm-plans-commitments-prescription-opioid-containing-products-guidance-industry/document.html. Accessed 17 Jun 2022.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–107. https://doi.org/10.1002/sim.3697.
Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46:348–55.
Helfenstein U. The use of transfer function models, intervention analysis and related time series methods in epidemiology. Int J Epidemiol. 1991;20(3):808–15. https://doi.org/10.1093/ije/20.3.808.
Hyndman RJ, Khandakar Y. Automatic time series forecasting: the forecast package for R. J Stat Softw. 2008;27:1–22.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2021. https://www.R-project.org/. Accessed 17 Jun 2022.
Ontario Drug Policy Research Network. COVID-19 Ontario prescription drug utilization tool. Toronto, ON; October 2020. https://odprn.ca/covid19-ontario-prescription-drug-utilization-tool/. Accessed 17 Jun 2022.
Busse JW, Craigie S, Juurlink DN, et al. Guideline for opioid therapy and chronic noncancer pain. CMAJ. 2017;189(18):E659–66. https://doi.org/10.1503/cmaj.170363.
Acknowledgments
We thank Sandrine Henri for her contribution to the design of the study and Marina Amaral de Avila Machado for assisting with the preparation of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no grant from any funding agency in the public, commercial, or not-for-profit sectors. YolaRX Consultants funded the open access.
Conflicts of interest/competing interests
All authors are employees of YolaRX Consultants, a research organization that provides consultancy services to pharmaceutical companies on topics unrelated to the work presented in this article.
Ethics approval
This study used existing anonymous data and thus no ethics approval was required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The data that support the findings of this study are not publicly available because of a data-sharing agreement with the data custodians.
Code availability
The code produced for the data analyses is not publicly available.
Author contributions
YM and AMC contributed to the concept and design of the study as well as to the acquisition of the data. AMC conducted all data management activities and produced all statistical analyses. All authors developed and revised the manuscript for important intellectual content, approved the final version for publication, and agreed to be accountable for the work. YM was the principal investigator and supervised all components of the study.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Castilloux, AM., Castillon, G. & Moride, Y. Impact of the COVID-19 Pandemic on Patterns of Prescription Opioid Use: A Retrospective Cohort Study of Adults Without a Cancer Diagnosis Initiating Opioids Using Administrative Claims Data. Drugs - Real World Outcomes 10, 31–39 (2023). https://doi.org/10.1007/s40801-022-00329-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-022-00329-z