Abstract
Background
Acute coronary syndrome (ACS)-related readmission is an important hospital quality measure. Medication management therapy, especially adherence to antiplatelet agents post discharge, could play an important role in reducing readmission rates. Newer agents such as ticagrelor and prasugrel have been shown, in randomized control trials, to have superior effectiveness to cardiovascular outcomes compared to clopidogrel, but they are more expensive and have more common adverse events such as bleeding and dyspnea.
Objective
We compared real-world readmission rates and adherence to antiplatelet agents among patients who initiated these agents post discharge.
Methods
This was a retrospective cohortstudy of patients with an index ACS-related hospitalization between 1 July 2017 and 31 December 2018. Using integrated pharmacy and medical claims data from a large national pharmacy benefits manager for commercially insured adults aged ≥ 18 years, we compared ACS-related readmission and medication adherence (as medication possession ratio (MPR)) among the three agents. ANOVA and logistic regression, controlling for demographics such as age, gender, and Charlson Comorbidity Index, were used to estimate any association between the agents and 365-day readmission rates.
Results
Of the 948 eligible patients, 86, 342, and 520 were initiated on prasugrel, ticagrelor, and clopidogrel (PTC), respectively. There were 4.7%, 5.3%, and 8.5% readmissions rates in the PTC cohorts, respectively, but these were not statistically significant in either the ANOVA or the logistic regression analyses. MPR was highest in the ticagrelor (88.1%) cohort, followed by the prasugrel (79.1%) and clopidogrel (76.4%) cohorts.
Conclusion
Ticagrelor cohort had the highest medication adherence. Clopidogrel cohort had the highest readmission rate but the difference with the other cohorts was statistically insignificant.
Similar content being viewed by others
Ticagrelor and prasugrel are recommended over clopidogrel in patients with acute coronary syndrome under certain conditions. |
Clopidogrel is preferred when cost, bleeding, and dyspnea are important considerations. |
In a cohort of 948 patients, we found ticagrelor to have the highest medication adherence rate (88%) compared to prasugrel (79%) and clopidogrel (76%). |
Although the clopidogrel cohort had the highest readmission rate, the differences among the three cohorts were not statistically significant in the multiple logistic regression model. |
1 Introduction
In the Study of Platelet Inhibition and Patient Outcomes (PLATO) and the Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel-Thrombolysis in Myocardial Infarction (TRITON-TIMI), ticagrelor and prasugrel, respectively, were shown to be superior to clopidogrel for reducing ischemic complication and stent thromboses. The American Heart Association/American College of Cardiology (AHA/ACC) in their 2016 guidelines, therefore, recommended their use over clopidogrel in patients with acute coronary syndrome (ACS) (Non-ST Elevation-Acute Coronary Syndrome (NSTE-ACS) or ST Segment Elevation Myocardial Infarction (STEMI)). Specifically, they recommended use of ticagrelor after coronary stent implantation without revascularization or prasugrel for those who are not at high risk for bleeding complications or without a history of stroke or transient ischemic attack [1,2,3]. Subsequent studies and meta-analyses show mixed results of either confirmatory superior effectiveness or no differences in effectiveness between clopidogrel and ticagrelor or prasugrel; however, a higher rate of bleeding and dyspnea in ticagrelor versus clopidogrel is well established [4,5,6].
Readmission rates of patients with ACS remain a concern and hence this metric is one of the measures tracked by the Centers for Medicare and Medicaid (CMS) Hospital Readmission Reduction Program and is a component in the Medicare star ratings [7, 8]. Dyspnea and bleeding, which may be more common with ticagrelor, are associated with higher readmission rates [3, 9]. Likewise, medication non-adherence, which may be greater for branded products with higher co-pays, is associated with higher readmissions [10].
Influenced by the paucity of real-world comparative effectiveness studies of the antiplatelet medications, in this study we retrospectively compared the medication adherence and ACS-related hospital readmissions of patients with ACS who initiated ticagrelor, prasugrel, or clopidogrel post discharge.
2 Methods
2.1 Data and Study Design
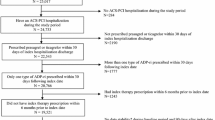
This was a retrospective cohort study designed to examine recurrence of inpatient hospitalizations for patients initiating antiplatelet treatment for ACS after an ACS-related index hospitalization. ACS-related hospitalizations included acute/chronic ischemic heart disease (I24.9, I25*, I24*), unstable angina (I20.0), and myocardial infarction (I21.0-4, I21.9, I21.A*, I22). Data were derived from de-identified, integrated member enrollment, pharmacy administrative and medical claims of a large national (USA) pharmacy benefits manager (PBM). The target population comprised patients who were continuously eligible between 1 January 2017 and 31 December 2019, aged ≥ 18 years as of 1 January 2017, and were hospitalized for an episode of ACS in the index period (Fig. 1). The index period spanned an 18-month period from 1 July 2017 through 31 December 2018. The first ACS-related hospitalization date in the index period was considered the index date. Outcomes were assessed within 365 days post index date. Patients were categorized into ticagrelor, clopidogrel, or prasugrel cohorts based on the study medication prescribed post index event. Patients were excluded from the analysis if they had a prior ACS-related hospitalization or prior antiplatelet medication claim in the pre-period (previous 180 days), or switched study medications in the post-index analysis period.
2.2 Variables
The outcomes of interest were the proportion of ACS-related inpatient readmissions and medication adherence measured as medication possession ratio (MPR) in each of the three patient cohorts. The MPR was computed as the sum of the days’ supply of the study medications divided by the length of the study period (365 days).
In addition to antiplatelet medication, other patient characteristics included in the study were age, gender, any inpatient hospitalization in the pre-period, history of bleeds, ischemic complications, coronary stent use, number of days between index date and first prescription of study medication, MPR (for study medications and other cardiovascular medications), and Charlson Comorbidity Index (CCI) (based on medical claims from the pre-period).
2.3 Statistical Analysis
Descriptive statistics were estimated and bivariate differences between the medication groups were tested using a Pearson chi-square test for categorical variables and ANOVA for continuous variables. Multivariate logistic regression analysis was performed to estimate the association of the type of study medication used with the odds of ACS-related inpatient readmissions, controlling for the confounding variables listed above. Everyone in the sample had continuous eligibility without censorship or switching of medication concerns, making logistic regression an appropriate model for analysis. We also analyzed patients who switched between antiplatelets for context. Statistical significance was set at p < 0.05. All analyses were conducted in SAS statistical software version 9.4 (SAS Institute, Cary, NC, USA).
3 Results
3.1 Patient Characteristics
Of the total 948 eligible patients who experienced an ACS-related inpatient hospitalization within the study index period, 86, 520, and 342 were initiated on PCT, respectively (Fig. 2). The average ages of patients initiated on PCT were 55.9, 55.8, and 54.1 years, respectively (Table 1; clopidogrel vs. ticagrelor p < 0.05). The percent male in the prasugrel, clopidogrel and ticagrelor cohorts were 81.4%, 68.8% and 77.8%, respectively (prasugrel vs. clopidogrel and clopidogrel vs. ticagrelor p < 0.05). Average CCI was 0.686, 1.031, and 0.602 in the PCT cohorts, respectively (prasugrel vs. clopidogrel, and clopidogrel vs. ticagrelor p < 0.05). The clopidogrel cohort had a history of a higher rate of ischemic complications (6.2%) than ticagrelor (2.6%) and prasugrel (3.5%), p = 0.0481. There were no significant differences in the proportion of patients with a history of bleeds or with coronary stent among the three cohorts (Table 1).
3.2 Medication and Health Services Outcomes
MPR was highest in the ticagrelor cohort at 88.1% compared to prasugrel (76.4%) and clopidogrel (79.1%). Of these, the proportion adherent (MPR ≥ 80%) were 81.3%, 61.6%, and 68.9% in the ticagrelor, prasugrel, and clopidogrel cohorts, respectively. The difference between prasugrel and clopidogrel MPRs was not statistically significant. There were no statistically significant differences in average number of inpatient hospitalizations in the pre-period or days to first prescribed study medication following ACS admission among the study cohorts.
The ACS-related inpatient readmission rates for the ticagrelor, clopidogrel, and prasugrel cohorts were 5.3%, 8.5%, and 4.7%, respectively (not shown). None of the readmission rate comparisons between cohorts were statistically significant.
In the multivariable logistic regression analysis, with the ticagrelor cohort as reference group, there were no statistically significant associations between the odds of ACS-related readmissions and use of clopidogrel (odds ratio (OR) 1.013; 95% confidence interval (CI) 0.956–1.073) or of prasugrel (OR 0.967; 95% CI 0.849–1.104) (Table 2).
4 Discussion
In this study, we compared the medication adherence of patients with ACS who initiated ticagrelor, prasugrel, or clopidogrel after an index ACS-related hospitalization and subsequent ACS-related readmissions within 365 days of discharge. We found ticagrelor to have the highest adherence (88%), followed by clopidogrel (79%) and prasugrel (76%). We also found that there were no statistically significant differences in readmission rates among the three study cohorts.
Medication adherence is associated with lower hospital re-admission [11] and hence several interventions pre- and post-discharge have been implemented at different care settings to improve medication adherence such as transitions-of-care with a care coordinator [10, 12, 13]. The mean MPR for prasugrel in our study was 76.4%, which was nearly identical to the 78.8% in the Nordstrom et al. study of patients with ACS after a percutaneous coronary intervention [14]. Similar to our findings, in a study comparing ticagrelor and clopidogrel on major adverse cardiovascular events, patients in the ticagrelor cohort had a higher adherence rate (MPR 81.6%) than those on clopidogrel (MPR 73.9%) [11]. The proportion of males in that study was comparable to ours (77.2% vs. 77.8%), and in their study, the mean age in the ticagrelor group was 60 years compared to 62 years in the clopidogrel group (54 years vs. 55.8 years, respectively, in our study). These findings in the literature and our study of the high ticagrelor adherence rate is surprising since the randomized control trials (RCTs) and meta-analysis found high ticagrelor discontinuation rates driven mainly by dyspnea or bleeding [5, 6]. Our study population was younger and most of these adverse events are more common in the elderly, which could explain the higher ticagrelor adherence rate. Furthermore, because clopidogrel is significantly less expensive than ticagrelor, and is dosed once daily rather than twice daily in the case of ticagrelor, it is counter-intuitive that medication adherence would be significantly greater with ticagrelor. This raises the possibility of other unmeasured differences among groups, such as lower socioeconomic status among users of clopidogrel. MPR for concomitant antihypertensive claims [(ticagrelor: 82.9% [adherent 72.4%]), (clopidogrel: 71.3% [adherent 71.1%]), (prasugrel: 62.2% [adherent 78.3%])] and statins [(ticagrelor: 86.4% [adherent 82.0%]), (clopidogrel: 75.8% [adherent 77.3%]), (prasugrel: 68.6% [adherent 91.7%])] show a similar pattern with better adherence among the ticagrelor cohort.
Most of the antiplatelet comparative effectiveness studies evaluated, as a primary outcome, a composite measure of all-cause mortality, myocardial infarction or strokes, and the findings are mixed [2,3,4,5,6]. The landmark RCTs PLATO and TRITON-TIMI clearly show superiority of ticagrelor and prasugrel in reducing the composite measures mentioned earlier and stent thrombosis; conversely, subsequent smaller controlled trials and the SWEDEHEART registry observational study [2, 4, 5] found no significant differences in effectiveness between these two medications and clopidogrel. Bergmark suggested that the difference between such landmark RCTs and a large real-world study like SWEDEHEART is reflected in the populations studied (well-defined vs. higher inclusivity). In real-world practice, patients may differ from clinical trial patients based on comorbidities, age, race, socioeconomic status, and insurance coverage (or lack thereof), making other considerations important, such as cost (and co-pays) of the medications, bleeding potential of patients, dosing frequency, and concerns for medication compliance [15]. Thus, real-world studies such as our study are useful to inform practice beyond RCTs.
There are few studies specifically comparing readmission rates among patients treated with antiplatelet agents for ACS. For example, Song et al. compared 90-day readmission rates of patients aged over 65 years on ticagrelor or prasugrel and reported no statistically significant difference in readmissions between them [16]. Our study of younger adults over a 365-day follow-up period reported higher readmission rates with clopidogrel (8.5%) than ticagrelor (5.3%) or prasugrel (4.7%); however, readmission rates were not statistically significant in the multivariate logistic regression analysis. The lack of differences in the logistic regression model could likely reflect the higher pre-study hospitalization rate and higher comorbidity index in the clopidogrel cohort compared to ticagrelor and prasugrel cohorts, as well as differences in medication adherence rates between agents.
4.1 Limitations and Strengths
Our study is subject to biases typical of observation studies such as selection bias and limitations of administrative claims datasets that are not collected primarily for research. Importantly, administrative data do not provide information on severity of coronary artery anatomy and many other clinical factors related to ACS. In addition, use of aspirin, which is an important variable, is often not recorded in claims data because aspirin is often purchased by patients over the counter, hence introducing information bias. Additionally, readmission is a multifactorial public health problem, and affected by many factors beyond choice of medication; many providers and health plans implement interventions aimed at improving clinical outcomes in patients discharged with ACS. As such, although our dataset represents many different health plans across the country, giving it a broad real-world practice appeal, it fails to account for the individual programs in place at hospitals, community pharmacies, and health plans to improve adherence and reduce readmissions. Medication adherence (such as MPR or proportion of days covered) calculated from claims data might not necessarily mean patients actually took the drug. But they have been widely used and validated as good measures with caveats. MPR is also believed to have the tendency to overestimate adherence because it does not account for early refills [17]. Finally, our study excluded antiplatelet switches, which do occur in general practice. However, when we analyzed the switchers (229), 30.3% switched from ticagrelor, 11% from clopidogrel, and 15.7% from prasugrel. Overall, the readmission rate of switchers was higher than non-switchers (10% vs. 7%). Readmissions from those who switched from ticagrelor were lowest (8.1%) compared to clopidogrel (14.1%) and prasugrel (15.4%).
Most studies that show superiority of ticagrelor and prasugrel over clopidogrel used a composite measure that includes deaths and stroke. Our findings are limited to only readmissions of non-switchers. Additionally, ticagrelor had the highest proportion of patients who were adherent, yet ticagrelor also had the highest number that switched (30.3%) compared to prasugrel (15.7%), and clopidogrel (11%). Prescribers therefore should be cognizant of the importance of adherence to antiplatelet efficacy in initiating therapy. Switching could be due to cost or adverse events including bleeding, and often requires de-escalation [18].
5 Conclusion
Although AHA and ACC recommend ticagrelor and prasugrel over clopidogrel because of their superior antiplatelet effectiveness as demonstrated in the PLATO and TRITON-TIMI studies, clopidogrel use remains popular among prescribers for several reasons. We found adherence to ticagrelor higher than clopidogrel and prasugrel, but no statistically significant association between the antiplatelet agent initiated after an index ACS-related hospitalization and hospital readmission one year post discharge.
References
Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease. Circulation. 2016;134(10):e123–55.
Sahlén A, Varenhorst C, Lagerqvist B, et al. Outcomes in patients treated with ticagrelor or clopidogrel after acute myocardial infarction: experiences from SWEDEHEART registry. Eur Heart J. 2016;37(44):3335–42.
Wallentin L, Becker RC, Budaj A, et al. PLATO Investigators. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045–57.
Yang H, Tang B, Xu CH, Ahmed A. Ticagrelor versus Prasugrel for the treatment of patients with type 2 diabetes mellitus following percutaneous coronary intervention: a systematic review and meta-analysis. Diabetes Ther. 2019;10(1):81–93.
Wang D, Yang XH, Zhang JD, Li RB, Jia M, Cui XR. Compared efficacy of clopidogrel and ticagrelor in treating acute coronary syndrome: a meta-analysis. BMC Cardiovasc Disord. 2018;18(1):217.
Gimble M, Qaderdan K, Willemsen L, Hermanides R, Bergmeijer T, De Very E, et al. Clopidogrel versus ticagrelor or prasugrel in patients aged 70 years or older with non-ST-elevation acute coronary syndrome (POPular AGE). The Randomized, open-label, non-inferior trial. Lancet. 2020;395:1374–81.
CMS: Hospital Quality Initiative-Outcomes Measures. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/OutcomeMeasures. Accessed 26 Feb 2021.
Prosser AE. Real-world incidence of patient-reported dyspnoea with ticagrelor. Ther Adv Drug Saf. 2018;9(10):577–84.
Wasfy JH, Hidrue MK, Ngo J, et al. Association of an acute myocardial infarction readmission reduction program with mortality and readmission. Circ Cardiovasc Quality Outcomes. 2020. https://doi.org/10.1161/CIRCOUTCOMES.120.007184.
Rosen OZ, Fridman R, Rosen BT, Shane R, Pevnick JM. Medication adherence as a predictor of 30-day hospital readmissions. Patient Prefer Adherence. 2017;11:801–10.
Turgeon RD, Koshman SL, Youngson E, et al. Association of ticagrelor vs clopidogrel with major adverse cooronary events in patients with acute coronary syndrome undergoing percutaneous coronary intervention. JAMA Intern Med. 2020;180:420.
Rupper TM, Cooper PS, Mahr D, et al. Medication adherence interventions improve heart failure mortality and readmission rates: systematic review and meta-analysis of controlled trials. J Am Heart Assoc. 2016. https://doi.org/10.1161/JAHA.115.002606.
Zhang Y, Kaplan CM, Baik SH, et al. Medication adherence and readmission in Medicare myocardial infarction. Am J Manag Care. 2014;20(11):e498–505.
Nordstrom BL, Simeone JC, Zhao Z, et al. Adherence and persistence with prasugrel following acute coronary syndrome with percutaneous coronary intervention. Am J Cardiovasc Drugs. 2013;13:263–71.
Bergmark BA. Real-world comparison of ticagrelor and clopidogrel: Rosetta Stone or lost in translation? JAHA. 2020. https://doi.org/10.1161/JAHA.120.017888.
Song C, Sukul D, Seth M, et al. Ninety-day readmission and long-term mortality in Medicare patients (>=65 years) treated with ticagrelor versus prasugrel after percutaneous coronary intervention (from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium. Am J Cardiol. 2017;120(11):1926–32.
Malo S, Aguilar-Palacio I, Feja C, et al. Different approaches to the assessment of adherence of adherence and persistence with cardiovascular-disease preventive medications. Curr Med Res Opin. 2017;33(7):1329–36.
Franch F, Rollini F, Rios JR, et al. Pharmacodynamic effects of switching from ticagrelor to clopidogrel in patients with coronary artery disease. Circulation. 2018;137(23):2450–62.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study is part of an ongoing collaboration between UPMC Value-Based Pharmacy Initiatives and Evernorth. Evernorth provides both funding and research personnel for this collaboration.
Conflicts of interest/competing interest
The authors report no conflicts of interest apart from being employees of UPMC or Evernorth.
Ethics approval
Data used for this study were de-identified and in full compliance with the Health Insurance Portability and Accountability Act (HIPPA); this project is deemed exempt by the University of Pittsburgh Institutional Review Board.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Data availability
Because of data use agreements with clients, individual-level data will not be available to share.
Code availability
Codes used are available upon request.
Author contributions
All authors contributed to the concept, design, review, and final approval of the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Peasah, S.K., Mager, D., Munshi, K.D. et al. Real-World Use and Outcomes of Oral Antiplatelets Among Patients with Acute Coronary Syndrome: A Retrospective Cohort Study. Drugs - Real World Outcomes 9, 121–127 (2022). https://doi.org/10.1007/s40801-021-00283-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-021-00283-2