Abstract
Background
Coronary heart disease (CHD)-related mortality is high in the southern United States. A five-drug pharmacotherapy regimen for acute coronary syndromes (ACS), defined as optimal medical therapy (OMT), can decrease CHD-related mortality. Studies have indicated that OMT is prescribed 50–60% of the time. Assessment of prescribing could provide insight into the potential etiology of disparate mortality.
Objective
The aim was to evaluate prescribing of OMT at discharge in patients presenting with an ACS event at an academic medical center and identify patients at risk of not receiving OMT.
Methods
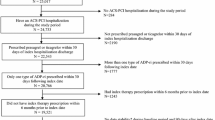
A single-center, retrospective cohort of patients with ACS diagnosis between July 2013 and July 2015 was investigated, and a multivariable regression analysis conducted to identify populations at risk of not receiving OMT.
Results
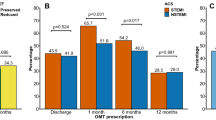
A total of 864 patients were identified by International Classification of Diseases, Ninth Revision (ICD-9) codes, with 533 excluded and 331 analyzed. OMT was prescribed in 69.79%. Patients ≥ 75 years of age [p = 0.003; odds ratio (OR) 0.30; 95% confidence interval (CI) 0.136–0.673], unstable angina presentation (p = 0.042; OR 0.55; 95% CI 0.307–0.977), and surgical management (p = 0.001; OR 0.22; 95% CI 0.095–0.519) were less likely to receive OMT.
Conclusions
The percentage of patients prescribed OMT exceeded the reported global percentage of prescribed OMT. However, disparities exist among specific populations.

Similar content being viewed by others
References
Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137:e67–492.
Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–98.
Gillum RF, Mehari A, Curry B, Obisesan TO. Racial and geographic variation in coronary heart disease mortality trends. BMC Public Health. 2012;12:410.
Pereira M, Araujo C, Dias P, et al. Age and sex inequalities in the prescription of evidence-based pharmacological therapy following an acute coronary syndrome in Portugal: the EURHOBOP study. Eur J Prev Cardiol. 2014;21:1401–8.
Sheikh-Taha M, Hijazi Z. Evaluation of proper prescribing of cardiac medications at hospital discharge for patients with acute coronary syndromes (ACS) in two Lebanese hospitals. SpringerPlus. 2014;3:159.
Yan AT, Yan RT, Tan M, et al. Optimal medical therapy at discharge in patients with acute coronary sydromes: temporal changes, characteristics, and 1-year outcome. Am Heart J. 2007;154:1108–15.
Yusuf S, Sleight P, Pogue J, et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000;342(3):145–53.
Skrepnek GH. Regression methods in the empirical analysis of health care data. J Manag Care Pharm. 2005;11(3):240–51.
Skrepnek GH, Olvey EL, Sahai A. Econometric approaches in evaluating cost and utilization within pharmacoeconomic analyses. Pharm Policy Law. 2012;14(1):105–22.
Amsterdam EA, Wenger NK, Brindis RB, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report from the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;130(25):2354–94.
O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:e78–140.
Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S1–45.
Cannon CP, Braunwald E, McCabe CH, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350(15):1495–504.
Heidenreich PA, Lewis WR, Labresh KA, Schwamm LH, Fonarow GC. Hospital performance recognition with the Get with the Guidelines program and mortality for acute myocardial infarction and heart failure. Am Heart J. 2009;158(4):546–53.
Basoor A, Doshi NC, Cotant JF, et al. Decreased readmissions and improved quality of care with the use of an inexpensive checklist in heart failure. Congest Heart Fail. 2013;19(4):200–6.
Wai A, Pulver L, Oliver K, Thompson A. Current discharge management of acute coronary syndromes: baseline results from a national quality improvement initiative. Intern Med J. 2012;42:e53–9.
Bi Y, Gao R, Patel A, et al. Evidence-based medication use among Chinese patients with acute coronary syndromes at the time of hospital discharge and 1 year after hospitalization: results from the Clinical Pathways for Acute Coronary Syndromes in China (CPACS) study. Am Heart J. 2009;157:509–16.
Al-Zakwani I, Zubaid M, Panduranga P, et al. Medication use pattern and predictors for optimal therapy at discharge in 8176 patients with acute coronary syndromes from 6 Middle Eastern countries: data from the gulf registry of acute coronary events. Angiology. 2011;62(6):447–54.
Pfeffer MA, Braunwald E, Moye LA, The SAVE Investigators, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. N Engl J Med. 1992;327(10):669–77.
Davis AM, Vinci LM, Okwuosa TM, Chase AR, Huang ES. Cardiovascular health disparities: a systematic review of health care interventions. MCRR. 2007;64:29s–100s.
Scirica BM, Cannon CP, Antman EM, et al. Validation of the thrombolysis in myocardial infarction (TIMI) risk score for unstable angina pectoris and non-ST-elevation myocardial infarction in the TIMI III registry. Am J Cardiol. 2002;90(3):303–5.
Hwang IC, Jeon JY, Kim Y, et al. Association between aspirin therapy and clinical outcomes in patients with non-obstructive coronary artery disease: a cohort study. PLoS One. 2015;10(6):e0129584.
Hwang IC, Jeon JY, Kim Y, et al. Statin therapy is associated with lower all-cause mortality in patients with non-obstructive coronary artery disease. Atherosclerosis. 2015;239(2):335–42.
Tam LM, Fonarow GC, Bhatt DL, et al. Achievement of guideline-concordant care and in-hospital outcomes in patients with coronary artery disease in teaching and nonteaching hospitals: results from get with the guidelines—coronary artery disease program. Circ Cardiovasc Qual Outcomes. 2013;6(1):58–65.
Faridi KF, Peterson ED, McCoy LA, et al. Timing of first postdischarge follow-up and medication adherence after acute myocardial infarction. JAMA Cardiol. 2016;1(2):147–55.
Lauffenburger JC, Robinson JG, Oramasionwu C, Fang G. Racial/ethnic and gender gaps in the use of and adherence to evidence-based preventative therapies among elderly Medicare Part D beneficiaries after acute myocardial infarction. Cirrculation. 2014;129(7):754–63.
Rassi AN, Cavender MA, Fonarow GC, et al. Temporal trends and predictors in the use of aldosterone antagonists post-acute myocardial infarction. J Am Coll Cardiol. 2013;61(1):35–40.
Acknowledgements
We would like to acknowledge Chelsea LaPreze, Pharm.D., for her contributions to data collection for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors Fox, Miller, Skrepnek, Schwier, and Ripley declare they have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Funding
No external funding was used in the preparation of this manuscript. None of the authors received grant support or other types of extramural funding for the writing of this manuscript.
Rights and permissions
About this article
Cite this article
Fox, A.N., Skrepnek, G.H., Miller, J.L. et al. Optimal Medical Therapy Prescribing Patterns and Disparities Identified in Patients with Acute Coronary Syndromes at an Academic Medical Center in an Area with High Coronary Heart Disease-Related Mortality. Am J Cardiovasc Drugs 19, 185–193 (2019). https://doi.org/10.1007/s40256-018-0308-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-018-0308-x