Abstract
Background
The effectiveness of specialty medications in complicated clinical conditions depends on adherence to therapy. However, specialty medications pose unique barriers to adherence.
Objective
This study aims to determine whether pharmacist interventions improve specialty medication adherence.
Methods
This is a single-center, pragmatic, randomized controlled trial ongoing since 10 May 2019 at an integrated health system specialty pharmacy. This study evaluates usual care compared with usual care plus patient-tailored adherence interventions. Study design and procedures were informed by focus groups with patients and specialty pharmacists. Patients at Vanderbilt Specialty Pharmacy with a proportion of days covered (PDC) < 90% in the previous 4 months are identified by a daily query of the electronic pharmacy database. A pharmacist reviews these patients’ electronic health records to identify and exclude ineligible patients. Eligible patients are randomized evenly to the control or intervention arm and stratified by historical clinic nonadherence rates. Patients randomized to the intervention arm undergo a baseline assessment to clarify reasons for nonadherence and subsequently receive patient-tailored interventions based on their specific reasons. Interventions and follow-up are provided at the discretion of the intervening pharmacist. The primary outcome is PDC calculated at 8 months post-enrollment. Enrollment of 438 participants will provide 90% power to detect a 5% difference in PDC between the two arms within each nonadherence risk stratum.
Discussion
This trial will evaluate the effect of patient-tailored interventions on specialty medication adherence and will inform how often and why patients are misidentified as nonadherent.
Registration
The trial was deemed a quality improvement initiative by the Vanderbilt University Institutional Review Board. It was registered in ClinicalTrials.gov (NCT03709277) on 17 October 2018.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Specialty medications have unique challenges that may affect adherence, such as medication costs, administration technique, frequent monitoring requirements, challenging distribution networks, shipping and storage logistics, and intentional interruptions in therapy because of side effects or extenuating circumstances. |
Reasons for misidentified and true nonadherence to specialty medications, and pharmacist interventions to improve nonadherence, were identified based on patients’ and pharmacists’ feedback and by reviewing patients’ electronic health records. |
Increasing specialty medication adherence through patient-tailored pharmacist-led interventions may improve clinical outcomes, reduce direct and indirect remuneration fees, and improve outcomes-based contracts and accreditation standard performance by specialty pharmacies. |
1 Background
Medication nonadherence costs the USA healthcare system an estimated $US672.7 billion and results in 12 million hospitalizations and over 275,000 deaths annually [1]. The contribution of specialty medication nonadherence to these financial and clinical outcomes is unknown but likely high, as patients prescribed specialty medications are known to incur more healthcare costs than nonspecialty patients [2]. When used as directed, specialty medications can significantly reduce patient morbidity and mortality [3,4,5]. However, specialty medications have unique barriers to adherence, including high out-of-pocket costs, challenging administration methods (often self-injected), limited distribution and payor networks, unique shipping and storage considerations, and safety monitoring that requires frequent follow-up visits with providers. Additionally, patients on specialty therapies often struggle with multiple comorbidities such as pain, disability, and fatigue as a result of their diseases [6,7,8]. Measures to combat nonadherence in this population include direct and indirect remuneration fees posed by payors on pharmacies, accreditation standards for specialty pharmacies, and a growing number of outcomes-based contracts [9]. Health system specialty pharmacists are ideally positioned to identify and address barriers to specialty medication adherence as they are embedded within clinics and maintain frequent (often monthly) communication with patients on therapy. Little work has explored the rates of and reasons for nonadherence in a broad specialty population or patient-level pharmacist interventions for improving adherence in the specialty population.
Specialty pharmacies and payors most commonly use pharmacy claims to calculate adherence, producing a skewed view of true adherence behavior in a population that often requires intentional interruptions in therapy because of adverse effects, extenuating clinical circumstances, or the use of samples [10, 11]. Previous research, limited by a small retrospective study design, demonstrated high rates of misidentified nonadherence using pharmacy claims adherence calculations in specialty patients [11]. More data are needed to guide specialty pharmacies in improving methods to identify and reduce true medication nonadherence in all three stages of medication use (initiation, implementation, persistence) [12].
Herein, we describe the design and pilot data of a study to accomplish two aims: (1) to evaluate the effects of pharmacist-provided patient-tailored adherence interventions on adherence to specialty medications, and (2) to improve understanding of misidentified nonadherence by determining reasons for nonadherence. The methods undertaken to design the study and pilot results can provide significant insight into pharmacist- and patient-perceived reasons for nonadherence, potential interventions to improve adherence, and a detailed method of calculating adherence. The outcomes of this study will provide needed insight into rates of and reasons for nonadherence and the impact of pharmacist-led patient-tailored interventions. While we await the results of this study, the protocol description offers key learnings for specialty pharmacy practice.
2 Methods
This manuscript was prepared in accordance with Criteria for Reporting the Development and Evaluation of Complex Interventions in healthcare: revised guideline (CReDECI 2) [13].
2.1 Study Design
This is a single-center, pragmatic, randomized controlled trial being conducted since 10 May 2019 that continues to enroll at an integrated health system specialty pharmacy at Vanderbilt University Medical Center (VUMC). The study is evaluating usual care compared with usual care plus pharmacist-driven patient-specific adherence interventions. Patients with a prescription written by a VUMC provider and dispensed by Vanderbilt Specialty Pharmacy (VSP), who demonstrate suboptimal adherence based on both their previous 4-month proportion of days covered (PDC) and chart review for true (as opposed to misidentified) nonadherence are assessed for eligibility. Adherence interventions are performed by either of two specialty pharmacists, termed intervention pharmacists, with experience in multiple specialty clinics. The primary investigator has practiced within seven specialty clinics over the previous year and has experience in both inpatient and outpatient settings. Specific preparation to provide adherence interventions in this study included reviewing pertinent literature, participating in a community focus group regarding medication adherence, meeting with manufacturer adherence specialists, and conducting the pilot study. The primary investigator enrolled patients, determined reasons for nonadherence, and made recommendations for interventions that were conducted by either herself or a second intervention pharmacist. The second pharmacist was trained by the primary investigator and was primarily responsible for follow-up after the initial intervention. Study design and interventions are informed by focus groups with patients and specialty pharmacists as detailed below. Figure 1 provides a visual representation of our methods.
2.2 Pilot Study
We conducted a 4-week pilot study using the planned study design as described. Of 84 patients reviewed, 33 met inclusion criteria and were randomized. All screened patients fit one of the proposed categories of reasons for nonadherence. Based on the pilot study findings, the following changes were made to the study design.
2.2.1 Eligibility Criteria
Many patients had low PDC at the medication level because of switching therapy during the previous 4 months. To address this, we added a filter to the pharmacy adherence report to omit patients with two medications from the same clinic within the 4-month timeframe. We also encountered many patients who appeared nonadherent because of discontinuing therapy. Based on anecdotal and pilot study experience, patients with > 30 days beyond their anticipated refill date were highly likely to have either discontinued treatment or have excess medication because of previous overlapping refills. Therefore, an additional requirement of > 30 gap days in the previous 4 months was included to reduce the risk of excluding patients with a medication surplus because of early refills.
2.2.2 Patient Follow-Up Protocol
Prior to the pilot, we had a standardized protocol for post-intervention follow-up at specified time intervals. The pilot revealed our greatest hurdle would be contacting the patient. Therefore, we determined it best to leave the frequency of follow-up to the discretion of the intervention pharmacist. Most patients are contacted during their routine refill call.
2.2.3 Forgetfulness Adherence Intervention
The pilot also identified forgetfulness as a primary reason for nonadherence, often because of administration frequencies of two or four times per month. We explored several options for aiding memory and decided to use smartphone reminders. In the pilot experience, patients were willing to set up reminders on their phone. Therefore, we sent written instructions via post for how to set up reminders as a component of the intervention when memory was indicated as a reason for nonadherence and the patient reported using a smartphone.
2.2.4 Health System Determinants
We noted several patients missed refills because of inaccurate data input in the pharmacy management system. Examples included refill tasks that did not fire appropriately, new prescriptions required but not sent, or prescriptions sent to the incorrect pharmacy. To minimize the impact of health system determinants, the investigator ensures all refill requirements are met for each patient in the intervention arm prior to the date they will run out of their previous fill if taking as prescribed.
2.2.5 Defining Nonadherence
Adherence thresholds have been proposed by the Pharmacy Quality Alliance for noninfused biologic medications used to treat rheumatoid arthritis, noninfused disease-modifying therapy used to treat multiple sclerosis, and antiretrovirals (PDC of 80%, 80%, and 90%, respectively), and a medication possession ratio of < 86% in patients on adalimumab for inflammatory bowel disease demonstrated poorer outcomes [14, 15]. However, in most specialty diseases, data are insufficient to correlate an adherence threshold with negative clinical outcomes, and it is widely accepted that different medications require varying levels of adherence for effectiveness. Our pilot defined nonadherence as having a PDC < 80%; however, our proposed study population demonstrated high rates of baseline adherence. Therefore, we decided to define nonadherent as PDC < 90% to increase the number of eligible patients and set a high standard for adherence within our population. A PDC of < 90% applied to 365 days would mean ≥ 37 days without therapy. We consider this clinically significant given some specialty medications require re-titration or re-induction following multiple missed doses.
2.3 Sample
All patients who receive a specialty medication prescription from VSP and who meet the following criteria are included.
-
The same medication (at Generic Product Identifier level 14) was filled four or more times in the 12 months before date of import into the study database.
-
The prescription was generated from one of the following Vanderbilt outpatient specialty clinics: pediatric rheumatology, pediatric gastroenterology/inflammatory bowel disease, adult rheumatology clinics, dermatology, hematology, adult endocrinology, neurology, asthma sinus & allergy, idiopathic pulmonary fibrosis, pulmonary arterial hypertension, cystic fibrosis, multiple sclerosis, neurology, or a lipid clinic.
-
Patient PDC was < 90% over the previous 4 months.
Patients meeting the following criteria are excluded.
-
Prescription issued by a non-VUMC provider.
-
Deceased patients.
-
Planned treatment discontinuation in the subsequent 8 months (e.g., if the patient was > 16 months into a 24-month therapy or the planned course of treatment was < 8 months).
-
More than one unique specialty medication from the same clinic in the previous 4 months (to reduce including patients with gaps in claims data because of discontinuing one therapy to start another).
-
Patients with > 30 gap days in the previous 4 months and whose last fill was > 30 days from importing into the study database. This criterion was developed to better identify patients likely to have discontinued treatment and is further described in the Sect. 2.2.
-
Any reason for misidentified nonadherence (such as for provider-directed treatment holds or external pharmacy fills, samples, discontinuation, inaccurate days’ supply from claims data, lapse in financial assistance, no longer prescribed by a VUMC provider, or held for coronavirus disease 2019 [COVID-19] concerns) in the previous 4 months.
2.4 Screening, Enrollment, and Randomization
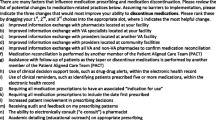
To identify eligible patients, we developed an automated structured query language-based report that calculates PDC, at Generic Product Identifier level 14, daily for all patients with specialty prescriptions. The report is stored in a shared protected folder for review and then securely transferred via secure file transfer protocol to VUMC’s server. Each day, patient and prescription data for patients meeting inclusion criteria automatically imports from this folder into the study database in Research Electronic Data Capture (REDCap), a web-based system for collecting and managing data that complies with the Health Insurance Portability and Accountability Act [16, 17]. Imported fields include medical record number, demographics, insurance type, specialty clinic, specialty medication, PDC rate over the previous 4 and 12 months, and gap days over the previous 4 months. An intervention pharmacist reviews the patients’ electronic health records (i.e., clinical notes, provider and patient communication) and the pharmacy patient management system (i.e., notes on shipment delays, pharmacist/pharmacy technician communications) for reasons for nonadherence. Reasons for nonadherence were informed by the pharmacists’ previous experience as well as patient and pharmacist feedback and are described in Table 1. Patients meeting exclusion criteria are not randomized.
We use a stratified randomization scheme to minimize baseline risk imbalance between arms. The strata are defined by the specialty outpatient clinic from which a prescription is generated, which has been characterized by risk for nonadherence based on historical data. Eligible patients are randomized between the intervention arm and control (usual care) arm with 1:1 allocation ratio within strata. The randomization sequence was generated by a study statistician and deployed through REDCap’s randomization module. If a patient is randomized to the intervention arm, but the pharmacist later determines, after speaking with the patient, that they met the exclusion criteria, the patient will not receive any intervention but will be included in the final analysis to maintain the balance of the randomized intervention allocation.
2.5 Measuring Adherence
PDC is often the preferred medication adherence calculation because it more accurately represents the supply of medication available [18, 19]. To determine PDC, a supply diary is generated for the time window of interest. A supply diary calculates the day-to-day tally of medication availability for each day in the window, where excess supply because of overlapping refills is shifted forward (but never backward) so that only 1 day’s supply is available each day, as seen in Fig. 2. Any oversupply at the end of the time period is truncated from the total supply.
Illustration of proportions of days covered (PDC) based on claims data demonstrating an example of a PDC supply diary. Blue bars correspond to the number of days’ supply received at each pharmacy claim. A surplus of medication (shown in red) occurs when a patient fills a prescription before the prior fill is exhausted, and thus the patient has excess supply during the overlapping days. According to the rules for calculating PDC, early refills are shifted forward to begin once the prior fill is exhausted (as shown in fill 4). The study period for all patients is the first 240 days after randomization. The observation window is the time from the date of the first fill to the date of the last fill within the study period and therefore varies by patient. To calculate PDC, the number of covered days is divided by the length of the observation window. In this example, there are 150 covered days in the observation window, and the time from the first to last fill can be calculated as 201 − 11 = 190 days. Thus, the PDC for the given example is 150/190 = 78.9%
2.6 Proportion of Days Covered Calculations
PDC will be used to calculate adherence for eligibility (< 90% over the previous 4 months), baseline characteristics (PDC over the previous 8 months), and for the primary analysis 8 months post-enrollment. We chose a 4-month PDC for eligibility screening to assess patients with recent nonadherence with the goal of identifying and addressing adherence challenges prior to longer gaps in therapy. A longer PDC timeframe may include patients with nonadherence several months prior to screening, reducing the potential for an actionable intervention at the time it is needed. However, a longer PDC timeframe likely provides better insight into sustained adherence behavior and we have therefore chosen an 8-month PDC for baseline and outcome analyses. Each of these PDC calculations measures the number of covered days in the supply diary divided by the number of days between the first fill in the time period of interest and either the enrollment date (eligibility and baseline) or the last fill in the study period (primary outcome) (Fig. 3). For the primary outcome analysis, confining PDC to the last fill date ensures that we are measuring adherence when patients in both arms are known to be on the medication. A fixed end date was not used as this method does not account for treatment discontinuation and can introduce bias by reducing PDC of patients known to not be on therapy [20,21,22].
Time periods used in calculations for the study. At enrollment, patients must have filled four or more prescriptions over the preceding 12 months. Proportion of days covered (PDC) will be calculated over two time periods at the time of enrollment: 4 months for eligibility and 8 months for baseline analysis, and once at the end of the 8-month study. Dark blue lines represent inclusion criteria. The green line represents baseline adherence analysis. The yellow line represents the primary outcome analysis
2.7 Intervention Design
To explore reasons for nonadherence that would inform intervention design, we calculated PDC over 12 months for all specialty areas. The average PDC was 91.8% from a sample of 7488 patients, with 14.1% (n = 1056) having a PDC < 80% [11]. We performed a manual chart review of 10% of patients with PDC < 80% to evaluate reasons for true and misidentified nonadherence. True nonadherence was defined as PDC < 80%, and no understandable reason for gaps in therapy were identified. We found six primary reasons for true nonadherence: unreachable (preventing medication dispensing), unresponsive (missed laboratory tests, missed appointments, failure to respond to financial documentation requirements), health literacy, financial, clinical, or memory. Misidentified nonadherence was defined as PDC < 80%, and an understandable reason for gaps in therapy were identified. We identified four reasons for misidentified nonadherence: clinically appropriate medication holds, external pharmacy fills, samples, or medication discontinuation. Misidentified nonadherence accounted for 40% of patients with PDC < 80%. These results motivated us to further explore challenges to medication adherence from the perspective of both patients and pharmacists.
2.8 Pharmacist Focus Group
We hosted a focus group of six clinic pharmacists (representing dermatology, pediatrics, multiple sclerosis, hematology, and rheumatology clinics) and three research pharmacists to better understand real-world reasons for and actions to address nonadherence among specialty patients. We presented our preliminary data and discussed perceived reasons for nonadherence among our population. Input from this group reinforced the previously developed categories of reasons for nonadherence and contributed to the list of categories of interventions used in this study (Table 1). From these discussions, we developed a working protocol for the intervention pharmacist to follow when true nonadherence is identified.
2.9 Patient and Public Involvement
To understand reasons for nonadherence from the patient perspective, we hosted a focus group of six adult patients from VUMC recruited through ResearchMatch, a platform for engaging community members [16]. Two strategies were used to guide our discussion: (1) summaries of previous community engagement groups were reviewed to identify previously reported barriers to medication adherence, and (2) a literature review was conducted for completeness and to provide a framework for discussion [23, 24]. Six members of the community participated and were compensated. Though we were unable to recruit patients receiving specialty medications for the focus group, all focus group participants were receiving prescription medication and voiced previous adherence challenges. Attendees were given a brief description of the project then asked a series of questions to gather feedback on reasons for nonadherence, study design, and proposed interventions. The questions and responses from this meeting can be found in the electronic supplementary material (ESM). A summary of the group’s recommendations and how they were used can be found in Table 2.
2.9.1 Control (Usual Care) Group
Most VSP pharmacists are physically embedded in clinics where they manage the selection, acquisition, and monitoring of specialty therapies [25]. They use clinic-specific protocols outlining disease state and therapeutic goals, clinical management guidelines, patient support services, and patient monitoring methods and frequency. Patient treatment response, adverse effects, healthcare utilization, and adherence behaviors are evaluated using refill questionnaires (typically performed monthly) and pharmacist assessments (frequency based on clinic protocols). Additional patient monitoring services and frequency are dependent on clinic protocols detailing longitudinal safety and effectiveness monitoring plans.
2.9.2 Intervention Group
Patients randomized to the intervention arm receive the usual care described plus adherence interventions performed remotely by an intervention pharmacist. Interventions are referred to as patient tailored because the intervention delivered is determined based on the patient’s specific reason(s) for nonadherence. Clinic pharmacists are consulted as needed to maximize the effectiveness of interventions and maintain continuity of care for the patient. When appropriate, a progress note is documented in the patient’s electronic health record listing the study inclusion PDC and barriers to adherence (if known) to allow other members of the healthcare team (anyone with access to the electronic health record) to intervene and provide accountability. Any intervention from the healthcare team that may be provided from the intervention pharmacist’s note is considered an extension of the pharmacist intervention given the direct correlation.
The intervention pharmacist contacts patients in the intervention group by phone and uses a semistructured script for a baseline assessment of potential causes for medication nonadherence. Information from this assessment is used to create patient-specific intervention(s) based on the determined reason(s) for nonadherence. For example, if a patient is nonadherent because of lack of memory and because they are unclear on what benefit the mediation provides, the pharmacist may provide instructions for setting up reminders on their smartphone and counsel on the benefits and risks of the medication. See Table 1 for a complete list of possible interventions. The intervening pharmacist will consider the patient’s nonadherence rate and the patient’s response to the intervention and decide when follow-up is appropriate. Follow-up calls will be combined with refill calls when possible and will be used to gauge the effectiveness of the intervention. If the pharmacist can provide a specific intervention based on patient responses, this is done during the call. Some barriers to adherence require investigation and follow-up with an additional call or email. The timing of the baseline assessment, the choice of intervention, and all follow-up is at the intervention pharmacist’s discretion. If a patient is unreachable by phone, the intervention pharmacist communicates through the secure My Health at Vanderbilt patient portal, a documented email address, or mailed letters as a last resort. These communications may include any recommendations, such as making an appointment or updating contact information, and may also include a baseline assessment survey. Attempts are made to reach the patient until either the patient responds or the 8-month follow-up date is reached. Unreachable patients will be included in the analyses.
2.9.3 Statistical Analysis
The primary outcome is PDC calculated at 8 months post-enrollment. As the distribution of PDC measures are typically skewed, an ordinal regression analysis will be performed to determine whether there is a difference in 8-month PDC between patients in the intervention arm versus the control arm, controlling for the following: 8-month PDC at the baseline, age, sex, race/ethnicity, insurance type, drug administration route, My Health at Vanderbilt enrollment status, time on therapy, distance from Vanderbilt (based on patient address), historical clinic nonadherence risk, and clinic type (i.e., rheumatology, endocrinology, etc.) as a surrogate for specialty conditions. The historical nonadherence risk for each clinic can be found in the ESM and will be used to adjust for varying nonadherence risk between disease states. In addition to the covariates selected a priori, inclusion of interactions as well as nonlinear relationship between the outcome and continuous covariates in the model will be also considered based on exploratory analysis. We will use an intention-to-treat analysis. Descriptive statistics will be used to describe our patient cohort and reasons for nonadherence by clinic.
We will report the rates of and reasons for misidentified nonadherence to assess the utility of quantifying data that are unavailable when utilizing pharmacy claims calculations alone. Hospitalizations between the intervention and usual care arms will be reported at the end of the study period. Though our study is not primarily designed to test the difference in this outcome between the arms, we anticipate an increase in adherence will result in a decrease in hospitalizations. In addition to our primary outcome, we will calculate PDC post enrollment at 6 and 12 months to evaluate the short-term effect of interventions and durability of intervention impact after they have ceased, respectively. We recognize that PDC is limited in measuring short-term adherence. Capturing PDC at three separate time intervals will demonstrate a time trend on the intervention effects on adherence. We do not anticipate any missing PDC data and < 5% of covariates, which will be imputed using predictive mean matching. However, we do expect 10% attrition because of death, treatment discontinuation, or transfer of care prior to 4 months post enrollment.
2.9.4 Sample Size Considerations
We calculated the sample size and power based on the preliminary data for raw PDC from patients who were nonadherent (61.5 ± 15.3%). Assuming a 5% difference in PDC between the intervention and control arms would be meaningful, we will enroll 438 patients (219 per arm), which provides 90% power to detect the difference at a type I error rate of 0.05, after accounting for 10% attrition rate. This sample size also allows sufficient precision in estimating the 95% confidence interval for the mean difference between the two arms such that the difference in mean raw PDC between the two arms could be estimated within ± 3% precision.
2.9.5 Learning Healthcare Partnership
This project was informed and supported by the Vanderbilt Institute for Clinical and Translational Research (VICTR) Learning Healthcare System. This platform partners clinical research and clinical operations to embed research questions within the context of routine care delivery. Consultation with clinical trialists, implementation scientists, and biostatisticians informed the design of this pragmatic trial.
3 Discussion
This prospective, randomized controlled study is designed to fill an existing gap in the literature to identify and address nonadherence to specialty medications. Patient and pharmacist input on the study design and planned interventions provide unique perspectives to the field even prior to study initiation. Preliminary work and a pilot study have affirmed the importance and utility of this study on garnering needed insights into improving the care delivery model for specialty patients.
3.1 Pragmatic Trial Design
The pragmatic nature of the trial enables delivery of high-touch standard of care to patients at VSP while performing a high-quality clinical trial. Enrolling a study population from several specialty clinics with limited exclusions supports generalizability towards improving adherence at other health system specialty pharmacies. Also, the intervention is customized to the patient as several study elements are left to the discretion of the pharmacist, including determining reasons for nonadherence, frequency of follow-up, and coordination of care with the clinic. The study protocol outlining potential reasons for nonadherence and subsequent interventions will allow others to replicate our approach.
3.2 Study Limitations
Though a blinded study design would be ideal, the clinic pharmacists and technicians providing usual care could not be blinded to the intervention. Patients remain unaware of their assignment, and randomization is masked until enrollment. The patient’s medical record does not contain any indicator of assignment. However, clinic pharmacists and other healthcare providers could become unblinded and able to identify patients randomized to the intervention group because adherence interventions can be documented in patient charts and pharmacy software, and the pharmacist providing the intervention may contact clinic pharmacists for assistance. However, there is no potential for a clinic pharmacist or other healthcare provider to identify control group patients as the intervention pharmacist does not make note of control group assignment in the patient’s record, nor do they contact clinic pharmacists concerning these patients, minimizing the risk for bias in this group. All pharmacists are aware of the study’s existence and were asked not to alter their usual workflow or interventions, but we cannot rule out that this occurred.
Prior to randomization, each patients’ electronic health records are reviewed to determine whether nonadherence has been misidentified by pharmacy claims. Given that not all possible reasons for nonadherence can be found in record review and the possibility that reasons are overlooked, some patients are erroneously enrolled in the study with the presumption of true nonadherence. Though these instances are not identifiable in the control arm, they will likely be identified in the intervention arm where a baseline assessment is utilized to identify reasons for nonadherence. We are not excluding patients based on such findings to prevent bias and to maintain the integrity of randomization.
This study targets patients established on specialty medications. Proactively identifying and addressing potential adherence barriers at the initiation of medication would be ideal to prevent future nonadherence. We hope to use learnings from this study, namely a better understanding of barriers and impact of various interventions, to inform future study designs targeted to patients starting specialty therapies. Additionally, if study results are positive, future research could utilize various implementation science methods to assess the process and outcomes of implementing the intervention into normal practice.
Our study is limited to the impact of a pharmacist on patients’ adherence to their specialty medications. In our embedded pharmacist model, most of our pharmacists work alongside the prescribers in their clinic and are often used by the prescriber to address medication-related issues. Despite this, we acknowledge that the prescriber plays an important role in identifying and addressing medication nonadherence. Our study does not address the role of the prescriber in our methods and cannot account for the impact of nonpharmacist providers on medication adherence.
3.3 Anticipated Learnings
Upon completion, this trial will answer the question of whether providing a complex, patient-tailored adherence intervention increases adherence to specialty medications. Additional questions that this study will inform include the following: How often are specialty patients misidentified as nonadherent when utilizing pharmacy claims alone? What are the reasons patients may be misidentified as nonadherent based on pharmacy claims? What are the reasons for true nonadherence in a variety of specialty disease states?
Given the growing evidence that reasons for nonadherence are multifactorial, this trial will evaluate the effectiveness of adherence interventions tailored to patient-specific reasons for nonadherence [3, 23, 26]. If the intervention is effective, specialty pharmacies may consider providing a focused adherence service similar to that which we describe. The descriptive analysis of rate of and reasons for misidentified nonadherence will inform a more accurate understanding of the shortcomings of calculating adherence based on pharmacy claims alone.
References
Watanabe JH, McInnis T, Hirsch JD. Cost of prescription drug-related morbidity and mortality. Ann Pharmacother. 2018;52(9):829–37. https://doi.org/10.1177/1060028018765159.
Express Scripts 2019 Drug Trend report: https://www.express-scripts.com/corporate/drug-trend-report#2019-by-the-numbers Accessed 3 Dec 20
Pascual-Ramos V, Contreras-Yanez I, Villa AR, Cabiedes J, Rull-Gabayet M. Medication persistence over 2 years of follow-up in a cohort of early rheumatoid arthritis patients: associated factors and relationship with disease activity and with disability. Arthritis Res Ther. 2009;11(1):R26. https://doi.org/10.1186/ar2620.
Carrat F, et al. Clinical outcomes in patients with chronic hepatitis C after direct-acting antiviral treatment: a prospective cohort study. Lancet. 2019;393(10179):1453–64. https://doi.org/10.1016/s0140-6736(18)32111-1.
Hoy SM. Elexacaftor/Ivacaftor/Tezacaftor: first approval. Drugs. 2019;79(18):2001–7. https://doi.org/10.1007/s40265-019-01233-7.
Roubille C, et al. Evidence-based recommendations for the management of comorbidities in rheumatoid arthritis, psoriasis, and psoriatic arthritis: expert opinion of the canadian dermatology-rheumatology comorbidity initiative. J Rheumatol. 2015;42(10):1767–80. https://doi.org/10.3899/jrheum.141112.
Moss BP, Rensel MR, Hersh CM. Wellness and the role of comorbidities in multiple sclerosis. Neurotherapeutics. 2017;14(4):999–1017. https://doi.org/10.1007/s13311-017-0563-6.
Ronan NJ, Elborn JS, Plant BJ. Current and emerging comorbidities in cystic fibrosis. Presse Med. 2017;46(6 Pt 2):e125–e138138. https://doi.org/10.1016/j.lpm.2017.05.011.
Duhig AM, Saha S, Smith S, Kaufman S, Hughes J. The current status of outcomes-based contracting for manufacturers and payers: an AMCP membership survey. J Manag Care Spec Pharm. 2018;24(5):410–5. https://doi.org/10.18553/jmcp.2017.16326.
Canfield SL, et al. Navigating the wild west of medication adherence reporting in specialty pharmacy. J Manag Care Spec Pharm. 2019;25(10):1073–7. https://doi.org/10.18553/jmcp.2019.25.10.1073.
Paolella D, Cherry E, Jolly JA, DeClercq J, Choi L, Zuckerman A. Closing the gap: identifying rates and reasons for nonadherence in a specialty population. J Manag Care Spec Pharm. 2019;25(11):1282–8. https://doi.org/10.18553/jmcp.2019.25.11.1282.
Vrijens B, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012;73(5):691–705. https://doi.org/10.1111/j.1365-2125.2012.04167.x.
Mohler R, Kopke S, Meyer G. Criteria for reporting the development and evaluation of complex interventions in healthcare: revised guideline (CReDECI 2. Trials. 2015;16:204. https://doi.org/10.1186/s13063-015-0709-y.
P. Q. Alliance, "PQA’s Specialty Core Measure’s Set," ed.
Govani SM, et al. Defining an optimal adherence threshold for patients taking subcutaneous anti-TNFs for inflammatory bowel diseases. Am J Gastroenterol. 2018;113(2):276–82. https://doi.org/10.1038/ajg.2017.438.
Harris PA, Scott KW, Lebo L, Hassan N, Lightner C, Pulley J. ResearchMatch: a national registry to recruit volunteers for clinical research. Acad Med. 2012;87(1):66–73. https://doi.org/10.1097/ACM.0b013e31823ab7d2.
Harris PA, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. https://doi.org/10.1016/j.jbi.2019.103208.
Martin BC, Wiley-Exley EK, Richards S, Domino ME, Carey TS, Sleath BL. Contrasting measures of adherence with simple drug use, medication switching, and therapeutic duplication. Ann Pharmacother. 2009;43(1):36–44. https://doi.org/10.1345/aph.1K671.
Nau DP (2012) Proportion of days covered (PDC) as a preferred method of measuring medication adherence. Pharm Qual Alliacne 1–3.
Garcia-Sempere A, Hurtado I, Sanfelix-Genoves J, Rodriguez-Bernal C, Peiro S, Sanfelix-Gimeno G. Improving the accuracy of medication adherence measures using linked prescription and dispensation data: findings from the ESOSVAL cohort of patients treated with osteoporosis drugs. Curr Med Res Opin. 2019;35(9):1535–44. https://doi.org/10.1080/03007995.2019.1601944.
Forbes CA, et al. A systematic literature review comparing methods for the measurement of patient persistence and adherence. Curr Med Res Opin. 2018;34(9):1613–25. https://doi.org/10.1080/03007995.2018.1477747.
DeClerq J, Choi L. Statistical considerations for medication adherence research. Curr Med Res Opin. 2020;36:1549–57.
O. World Health, "Adherence to long-term therapies: evidence for action/[edited by Eduardo Sabaté]," ed. Geneva: World Health Organization, 2003.
Gellad W, Grenard J, McGlynn E. A review of barriers to medication adherence: a framework for driving policy options. RAND Corportation, 2009.
Bagwell A, Kelley T, Carver A, Lee JB, Newman B. Advancing patient care through specialty pharmacy services in an academic health system. J Manag Care Spec Pharm. 2017;23(8):815–20. https://doi.org/10.18553/jmcp.2017.23.8.815.
Jin J, Sklar GE, Oh VMS, Li SC. Factors affecting therapeutic compliance: a review from the patient's perspective. Ther Clin Risk Manag. 2008;4(1):269–86. https://doi.org/10.2147/tcrm.s1458.
Weiss BD. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3(6):514–22. https://doi.org/10.1370/afm.405.
Tamargo C, Sando K, Prados Y, Cowart K. Change in proportion of days covered for statins following implementation of a pharmacy student adherence outreach program. J Manag Care Special Pharm. 2019;25(5):588–92. https://doi.org/10.18553/jmcp.2019.25.5.588.
Nieuwlaat R, et al. Interventions enhancing medication adherence. Cochrane Database Syst Rev. 2014;2014(11):CD000011. https://doi.org/10.1002/14651858.CD000011.pub4.
Mann A, Esse TW, Serna O, Castel LD, Abughosh SM. Effectiveness of miled letters to improve medication adherence among medicare advantage plan participants with chronic conditions. Patient Prefer Adher. 2019;13:37–46. https://doi.org/10.2147/PPA.S185848.
Mishra SI, Gioia D, Childress S, Barnet B, Webster RL. Adherence to medication regimens among low-income patients with multiple comorbid chronic conditions. Health Soc Work. 2011;36(4):249–58. https://doi.org/10.1093/hsw/36.4.249.
Márquez Contreras E, Vegazo García O, Martel Claros N, Gil Guillén V, de la Figuera von Wichmann M, Casado Martínez JJ, Fernández R. Efficacy of telephone and mail intervention in patient compliance with antihypertensive drugs in hypertension ETECUM-HTA study. Blood Press. 2009;14(3):151–8. https://doi.org/10.1080/08037050510008977.
Al-Eidan FA, McElnay JC, Scott MG, McConnell JB. Management of eradication - the influence of structured counselling and follow-up. Br J Clin Pharmacol. 2002;53(2):163–71. https://doi.org/10.1046/j.0306-5251.2001.01531.x.
Acknowledgements
The authors acknowledge Carl Reed, Victoria Reynolds, and Traci Smith for their contribution to database development, project management, and intervention delivery, respectively.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The project described was supported by the VICTR Learning Healthcare System Platform under CTSA award no. UL1 TR002243 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Conflict of interest
Amanda Kibbons, Megan Peter, DeClercq, Leena Choi, Jacob Bell, Jacob Jolly, Elizabeth Cherry, Bassel Alhashemi, Nisha Shah, and Autumn Zuckerman have no conflicts of interest that are directly relevant to the content of this article.
Availability of Data and Material
No data have yet been generated for this study.
Ethics Approval
The trial was deemed a quality improvement initiative and registered with the Vanderbilt Institutional Review Board. It was registered in ClinicalTrials.gov (NCT03709277) on 17 October 2018. The results will be made available on ClinicalTrials.gov, submitted for publication in a peer-reviewed journal, and presented at scientific conferences. The project described was supported by the VICTR Learning Healthcare System Platform under Clinical and Translational Science Award no. UL1 TR002243 from the National Center for Advancing Translational Sciences.
Consent
Not applicable.
Author contributions
Amanda Kibbons: investigation, writing, visualization, supervision. Megan Peter: methodology, data curation, writing, project administration. Josh DeClercq: validation, formal analysis, data curation, writing. Leena Choi: study design, formal analysis, writing acquisition. Jacob Bell: validation, formal analysis, data curation, writing. Jacob Jolly: conceptualization, methodology, supervision, funding. Elizabeth Cherry: conceptualization, supervision. Bassel Alhashemi: resources. Nisha Shah: supervision. Autumn Zuckerman: conceptualization, methodology, writing, supervision, project administration.
Previous Presentations
This work has not been presented in any form.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kibbons, A.M., Peter, M., DeClercq, J. et al. Pharmacist Interventions to Improve Specialty Medication Adherence: Study Protocol for a Randomized Controlled Trial. Drugs - Real World Outcomes 7, 295–305 (2020). https://doi.org/10.1007/s40801-020-00213-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-020-00213-8