Abstract
Background
Around 20–30% of all prescribed drugs are estimated to be metabolised by the cytochrome P450 (CYP) 2D6 enzyme. In a medical practice, it is usually not known whether a patient is a poor, intermediate, normal or ultra-rapid metaboliser for CYP2D6-metabolised drugs.
Objective
This study aims to explore the clinical relevance and the extent of hazardous prescriptions by analysing the metaboliser status of patients already taking such drugs.
Methods
This is a family practice-based observational study performed in a rural practice for general and family medicine in Lower Austria providing care for approximately 2100 patients annually. In 287 consecutive patients, who had taken or were taking a drug metabolised by CYP2D6 during the last 3 years, the metaboliser status was analysed.
Results
The genetic analysis of 287 patients resulted in 51.22% normal metabolisers, 38.68% intermediate metabolisers, 6.27% poor metabolisers and 3.83% ultra-rapid metabolisers. In 50 cases (poor metaboliser, intermediate metaboliser and ultra-rapid metaboliser, i.e. 17.42% of all tested patients taking a CYP2D6-specific drug), an altered gene function was identified, for which clinical guideline annotations, drug label annotations, or clinical annotations are available. Allele and genotype frequencies were in accordance with data from other European studies.
Conclusions
In 17.42% of all patients already taking a drug metabolised by CYP2D6, knowledge of the genetically defined metaboliser status would have been of immediate clinical relevance before prescribing the drug.
ClinicalTrials.gov identifier
NCT03859622.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Poor, intermediate and ultra-rapid drug metabolisers of the cytochrome P450 (CYP) 2D6 enzyme have an elevated risk to experience serious adverse drug reactions. |
In general practice, a patient’s metaboliser status is usually unknown when a prescription of a CYP2D6-relevant drug takes place. |
This study revealed that in 17.42% of patients with a prescription of a CYP2D-relevant drug during the previous 3 years, knowledge of a patient’s CYP2D6 metaboliser status would have been of immediate clinical relevance before prescription took place. |
1 Background
A significant proportion (20–30%) of frequently prescribed drugs in various medical disciplines is metabolised by the hepatic cytochrome P450 (CYP) 2D6 enzyme. This isoenzyme is a genetically highly polymorphic member of the CYP superfamily, with remarkable inter-individual and inter-ethnic differences in its activity [1,2,3,4,5,6,7]. In contrast with other CYP enzymes, the genetic polymorphism largely explains the variable CYP2D6 enzyme function [6]. Numerous studies demonstrate the broad range of differences in inter-ethnic frequencies of non-functional and reduced function alleles as the main determinants of the metabolising status [8].
Similar to other members of this superfamily (e.g. CYP1A2, 2B6, 2C8, 2C9, 2C19, 2E1 and 3A4/5), CYP2D6 is an important phase I enzyme that metabolises and eliminates drugs by demethylation, hydroxylation and de-alkylation, leading to metabolites with increased hydrophilicity and increased or diminished activity [9]. For clinical purposes, it is useful to categorise the various combinations of more than 100 normal, reduced and no-function alleles as well as copy number variants into four phenotypic groups, namely poor (PM), intermediate (IM), normal (NM) and ultra-rapid metabolisers (UM) [10,11,12]. A consensus paper was elaborated by different working groups to standardise the terminology describing the impact of the genotype on the phenotype status [13].
Comprehensive worldwide data on various CYP2D6 genotypes in different major ethnicities as well as the prediction of their more definitive phenotype by using an activity score (AS) allow a comparison of different studies with respect to inter-ethnic or nationwide differences [12, 14]. From the clinical point of view, the question arises whether knowledge of the genetically determined metaboliser status has an impact on the decision of which drug should be chosen or how the dosage should be adapted according to published guidelines [15,16,17,18,19,20,21]. Not knowing the metaboliser status of a patient can have significant clinical consequences if a CYP2D6-relevant drug is prescribed. For example, in the case of an UM, a drug can be metabolised too rapidly, thus losing its therapeutic effect and requiring a higher dosage, or it can have serious potentially life-threatening effects if it is converted too rapidly into the effective form (e.g. tramadol, which is converted to high levels of its active metabolite O-desmethyltramadol).
Regarding regulatory pharmacogenomics communications on safety-related genetic markers for adverse drug reactions mentioned on drug labels, no internationally standardised recommendations can be found but several studies and programmes were initiated to facilitate the implementation of pharmacogenomics into routine care [22,23,24]. It is difficult to estimate in how many cases knowledge of the CYP2D6 metaboliser status would have an impact on the prescription of a specific drug in daily practice. There is limited pharmacogenetics research on the frequencies of CYP2D6 alleles, genotypes and metaboliser status, as well as on the potential benefit of pre-emptive pharmacogenetics testing in patients in Austria [25,26,27,28].
In the daily work of a general practitioner, drug prescription takes place without knowing the CYP2D6 metaboliser status of a patient. Attention is given to age, sex, and renal, hepatic, and gastric function of the patient as well as to possible drug–drug interactions, especially in view of increasing polypharmacy in the elderly [29, 30]. Knowledge of the CYP2D6 metaboliser status could potentially alter the prescription or dosage of a specific drug with regard to clinical guideline annotations, drug label annotations or clinical annotations, even though the usefulness of pharmacogenetics testing is not always supported by evidence [31,32,33,34,35,36,37]. Apart from evidence-based recommendations on which drug should be omitted or cautiously chosen, knowledge of the metaboliser status should increase the physician’s vigilance regarding a closer monitoring of possible adverse drug reactions and enhanced or diminished effects of the prescribed drug.
To predict the genetic metaboliser status of patients prescribed CYP2D6-metabolised drugs or inhibitors, we analysed their CYP2D6 alleles and calculated their AS. Furthermore, we investigated if this knowledge would have implications on drug prescription with respect to published guidelines or studies, [18, 38, 39] and if differences in genetic profiles related to CYP2D6 polymorphisms between the Austrian and worldwide populations existed [12, 14].
To elucidate the impact of the CYP2D6 metaboliser status in the real setting of a medical practice, we searched in the practice’s electronic medical records for the number of patients who were prescribed CYP2D6-metabolised drugs or inhibitors at least once during the previous 3 years. Annual prescription rates were compared with the corresponding percentage in the large dataset of the Lower Austrian Area Health Insurance (NOEGKK) with approximately 993,000 insured patients. Prescription rates of the single practice and the dataset of the NOEGKK were compared to find out the proportion of CYP2D6-metabolised drugs in relation to all prescribed drugs. A further aim of the study was to find out if there is a significant age difference between CYP2D6-tested and not tested patients with a prescription of a CYP2D6-relevant drug.
2 Methods
2.1 Study Population, Study Design and Data Source
This observational study was performed in a common general medical practice in 2017 and 2018. All patients visiting the practice from 2016 to 2018 (N = 3036) had a very similar mean age (47.38 years, standard deviation 24.57) and a constant sex distribution (approximately 53% female and 47% male). On scheduling the routine blood test because of various chronic medical conditions, the patients were asked to participate and provide their informed consent. Patients of either sex aged ≥ 18 years with a prescription of a CYP2D6-metabolised drug or inhibitor during the previous 3 years, and who were able to provide written informed consent were included. Patients who were not capable of providing written consent or who were unable to understand the aim of the study were excluded. Among 668 patients with a prescription of at least one CYP2D6-dependent drug within the previous 3 years, the genetic polymorphism of CYP2D6 was determined in 287 patients, while 378 patients did not visit the practice for a routine blood test during the study period (see Table 1 and File 1 of the Electronic Supplementary Material [ESM]). No further genetic investigations or additional blood collections were performed. All relevant demographic data and data on prescribed drugs were extracted from the electronic medical records and de-identified before further processing. The number of prescriptions in the years 2015–17 of all CYP2D6-metabolised drugs or strong CYP2D6 inhibitors, as identified by their Anatomical Therapeutic Chemical code, was compared to the total number of prescribed drugs of the practice (File 2 of the ESM). Further, relative per-capita prescription rates of CYP2D6-specific drugs in patients insured with the NOEGKK were used for comparison.
2.2 Assessments
The study investigated the proportion of patients with a prescription of a CYP2D6-relevant drug with respect to their metaboliser status (PM, IM, NM, UM), including allele frequencies, genotypes and AS. Based on the suggestion of Gaedigk et al. and on an updated consensus of an international group of experts who recently published revised CYP2D6 genotype-to-phenotype translation recommendations, ASs were assigned to alleles with no (0), decreased (0.25–0.5), intermediate (1), normal (1.25–2) and increased (> 2) function to enable translation of genotypes into phenotypes. The AS translated into metaboliser status as following: 0 = PM, 0.25–1 = IM, 1.25–2 = NM, > 2 = UM [12, 40].
2.3 Procedures and Laboratory Methods
For the genetic analysis of CYP2D6 polymorphisms and copy number variations (CNV) in all 287 tested patients, the PGX-CYP2D6 XL StripAssay® and the CYP2D6 RealFast™ CNV Assay (both ViennaLab, Vienna, Austria) were used, respectively. All assays were carried out in the laboratory of the medical practice.
2.3.1 Blood Sampling and Processing of the Specimens
A standardised blood sampling using BD Vacutainer® 4-mL EDTA tubes (Becton–Dickinson, Franklin Lakes, New Jersey, USA) for the red and white blood count was performed. For determination of the genetic CYP2D6 polymorphism, 300 mL of the collected blood were used.
2.3.2 Isolation of DNA
DNA was extracted from EDTA blood with the Spin Micro DNA Extraction Kit® (ViennaLab), and the concentration and quality of DNA were measured using a Bio Photometer plus (Eppendorf, Hamburg, Germany). The extracted DNA was stored at − 81 °C in an ultra-low temperature deep freezer (U101-86; New Brunswick Scientific Co., Inc., Edison, New Jersey, USA) without any further additives.
2.3.3 Real-Time Polymerase Chain Reaction for Determination of the Copy Number of the CYP2D6 Gene
To identify UM patients, determination of the copy number of the CYP2D6 gene was performed in triplicates on an ABI StepOnePlus instrument. The CYP2D6 RealFast™ CNV Assay was carried out according to the manufacturer’s instructions for use.
2.3.4 CYP2D6 Allele Determination by Polymerase Chain Reaction and Reverse Hybridisation Technology
The PGX-CYP2D6 XL StripAssay® was used for the determination of 20 clinically relevant CYP2D6 alleles (*1; *2 A, *2 B-M; *3; *4A-H, K, L or P, *4J or N, *4M; *5; *6 A, B or D, *6C; *7; *8; *9; *10A or B, *10 C or D; *11; *12; *14; *15; *17; *29; *35; *39; *40 or *58; *41). Briefly, a multiplex polymerase chain reaction using biotinylated primers was performed on a Palm-Cycler (Corbett Life Science, Mortlake, New South Wales, Australia) under the following cycling conditions: pre-polymerase chain reaction: 95 °C/4 min; thermocycling: 95° C/25 s–60° C/45 s–72 °C/1 min (36 cycles); final extension: 72 °C/3 min. The amplification products were subsequently hybridised to a test strip containing allele-specific oligonucleotide probes immobilised as an array of parallel lines. Bound amplicons were detected using streptavidin–alkaline phosphatase and colour substrates. The evaluation of the resulting band pattern was carried out by using the StripAssay® Evaluator (ViennaLab), a proprietary software to determine the homozygous or heterozygous genotype.
According to the manufacturer, results of the PGX-CYP2D6 XL StripAssay® and the CYP2D6 RealFast™ CNV Assay were 100% concordant with genotypes and copy numbers obtained by reference methods (i.e. Sanger sequencing, long-range polymerase chain reaction) and reference materials (i.e. pre-typed Coriell DNAs). The PGX-CYP2D6 XL StripAssay® and the CYP2D6 RealFast™ CNV Assay have been successfully validated on 118 and 98 samples, respectively. For internal verification of the applied genetic test, the study laboratory participated successfully in the PGX-CYP2D6 XL StripAssay® and CYP2D6 RealFast™ CNV Assay Confirmation Program offered by the manufacturer.
2.4 Statistical Analysis
Standard methods were used for the description of data (frequencies and percentages for categorical data, mean and standard deviation for continuous data), 95% confidence intervals (CIs) were calculated for observed percentages. To compare ranks of CYP2D6-specific drugs prescribed in the single practice with ranks of the total number of the respective prescriptions in Lower Austria, Spearman’s rank correlation coefficients (CCs) were calculated. A p value < 0.05 was considered to indicate statistical significance. Calculation of the Hardy–Weinberg equilibrium was used to determine if genotype frequencies (Table 3) are a simple function of allele frequencies in the practice population without disturbing influences, e.g. mutations. Deviations from the Hardy–Weinberg equilibrium are tested by Pearson’s \(x^{2}\) test or Fisher’s exact test, in the case of small numbers of observed genotypes.
3 Results
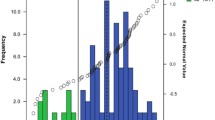
Of the whole practice population (N = 3036), 22% (CI 20.5–23.5) of patients (n = 668) received at least one CYP2D6-specific drug prescription (i.e. inhibitor or substrate) during a period of 3 years. Yearly per-capita drug prescription rates of the top ten CYP2D6-relevant drugs as well as prescription rates of all CYP2D6-relevant drugs show a high similarity between the single practice and all NOEGKK insured patients as shown by high Spearman’s CCs (Fig. 1, Files 2 and 3 of the ESM).
The mean age of all patients receiving CYP2D6-specific medications was 64.9 years. The age distribution of genetically tested and not tested patients, both with a prescription of a CYP2D6-specific drug, showed a significant difference of almost 10 years (Table 1).
3.1 Frequencies of Alleles, Enzyme Function, Activity Scores and Genotypes
3.1.1 Frequencies of Alleles, Enzyme Function and Activity Score of CYP2D6
Table 2 summarises the frequencies of alleles and the allocation of the metaboliser status to the AS. The no-function alleles *7, *8, *11, *12, *14 and *40 as well as the reduced function allele *29 were not detected in the group of 287 patients.
3.1.2 Frequencies of Genotypes, Activity Scores and Metaboliser Type of CYP2D6
Table 3 displays the genotypes as determined by genotyping assay and CNV determination, their frequencies and the metaboliser status based on the calculated AS. The PGX-CYP2D6 XL StripAssay® revealed 3.83% (CI 1.9–6.8) UM, 6.27% (CI 3.8–9.7) PM, 38.68% (CI 33–44.6) IM and 51.22% (CI 45.3–57.1) NM in a total of 287 patients. These percentages, with the exception of IM and NM, are within the range reported for Europeans (UM: 0–9.47%; PM: 1.8–11.29%; IM: 1.21–7.98% and NM: 59.47–89.31%) [12, 41]. The higher frequency of IM is explainable by the necessity to move several NM to the group of IM to comply with the recently published guidelines of the CYP2D6 Genotype to Phenotype Standardization Project of the Clinical Pharmacogenetics Implementation Consortium [40]. The distribution of genotypes presented in Table 3 complied with the Hardy–Weinberg equilibrium. Results of genotyping and of CNV determination were translated into the metaboliser status of the 287 tested patients and summarised in Table 4.
3.2 Clinical Relevance of CYP2D6 Metaboliser Status
Table 5 provides detailed figures on the prescriptions of CYP2D6-metabolised drugs and inhibitors as well as the respective metaboliser status of all tested patients. Numbers in bold letters indicate the number of patients for whom knowledge of the metaboliser status prior to drug prescription would have been of immediate importance in view of alternative drug selection or an altered dosage. The decision to consider a drug prescription as clinically relevant with respect to the patient’s metaboliser status was based on the availability of clinical guideline annotations, drug label annotations and clinical annotations [42,43,44]. Fifty patients (i.e. 17.42% of all tested patients) who were prescribed a CYP2D6-relevant drug were found to have an altered metaboliser status, of whom seven were identified as PM, 37 as IM and six as UM.
3.3 Comparison of CYP2D6-Specific Drug Prescriptions in Patients of the Single Practice and all NOEGKK-Insured Patients
High Spearman CCs of the top ten prescriptions are found between the years 2015–17 of the NOEGKK (CC: 0.987–1.0) and the single practice (CC: 0.866–0.987) as well as in comparing the top ten drug prescriptions of the NOEGKK with the single general practice (CC: 0.878–0.963) (Fig. 1).
Similar high CCs are found between the years 2015–17 of the NOEGKK and the single practice (CC: 0.870–0.988) as well as in comparing all drug prescriptions of the NOEGKK with the single general practice (CC: 0.775–0.833) [Files 2 and 3 of the ESM]. In the observer practice (approximately 17,000 prescriptions/year), the proportion of CYP2D6-specific drug prescriptions in relation to all prescribed drugs for the years 2015–17 was 9.61%, 10.91% and 10.76%, respectively, while it was 12.36%, 12.78% and 12.92%, respectively, for all NOEGKK-insured patients of Lower Austria (approximately 14,700,000 prescriptions/year) [File 2 of the ESM].
4 Discussion
The chosen study approach reflects the daily clinical situation in a general medical practice, when the practitioner decides to prescribe a drug metabolised by the CYP2D6 enzyme to a patient without knowing the patient’s metaboliser status. This situation is complicated by the fact that many chronically ill patients take a mixture of several drugs, of which some may be inhibitors of this important enzyme. The study focused on the analysis of the proportion of patients for whom CYP2D6 genotype information would have been relevant prior to prescription of a drug metabolised by the CYP2D6 enzyme with respect to an altered, genetically defined metaboliser status of CYP2D6. Among 287 mostly elderly patients, seven were identified as PM, 37 as IM and another six as UM. For these three patient categories, warnings exist in clinical guideline annotations, drug label annotations and clinical annotations. Thus, it appears that in 50 out of 287 tested patients (i.e. 17.42%), knowledge of the metaboliser status would have been of immediate clinical relevance before prescribing a potentially dangerous drug metabolised by CYP2D6. In fact, knowledge of the metaboliser status would have been of clinical relevance for all 287 patients, but we focused on the probability for an inappropriate and hazardous prescription of CYP2D6-dependent drugs especially in PM, IM and UM.
The significant age difference between the tested (70.3 years) and not tested patient group (60.8 years) taking drugs that are substrates or inhibitors of the CYP2D6 enzyme could be explained by an increased morbidity in the elderly with the consequence of more frequent blood examinations performed in the practice. Furthermore, this study demonstrated that during the observation time of 3 years, 22% of patients visiting an ordinary Austrian general practice were prescribed drugs being substrates or inhibitors of the CYP2D6 enzyme. In comparison to literature that reported 20–30% of all drugs being metabolised by CY2D6, we found only around 10.4% in the single observer practice and around 12.7% in all NOEGKK-insured patients [2, 45]. The drugs listed in Table 5 do not represent all available CYP2D6-dependent drugs in Austria. In addition, the following drugs are marketed in Austria but were not used in the observer practice: atomoxetine, clozapine, eliglustat, fesoterodine, fluvoxamine, gefitinib, modafinil, ranolazine, tetrabenazine and vortioxetine. The reason could be that the prescription of these drugs is not very common in general practice and reserved for specialists. Several CYP2D6-metabolised drugs are used worldwide but are not registered in Austria, e.g. acetaminophen, amoxapine, brexapiprazole, cevimeline, darifenacin, desipramine, deutetrabenazine, doxepin, flibanserin, iloperidone, imipramine, lofexidine, meclizine, nortriptyline, perphenazine, pimozide, protriptyline, quinine, thioridazine, trimipramine and valbenazine.
4.1 Comparison with Other Available Evidence in the Field
This study also intended to provide epidemiologic frequency data on CYP2D6 alleles, genotypes and metaboliser status of an elderly Austrian population for comparison with data of other epidemiological studies in Austria and Europe. Concerning allele frequencies (except for allele *35), the most frequent alleles *1, *2, *4, *41 and *10 (34.32%, 20.38%, 18.47%, 8.54% and 2.09%) are in accordance with frequencies of an Austrian population sample reported by Beer et al. (34.9%, 26.3%, 14%, 10.8% and 4.3%). Frequency data of these alleles are comparable to those found in the Croatian and Czech populations as well as in the general European population reported by Sistonen et al. (35.1%, 28.7%, 17.2%, 7% and 2.9%) [12, 28, 46, 47]. The non-function alleles *7, *8, *11, *12, *14 and *40, as well as the reduced function allele *29, were not detected. With the exception of *2/*41 and *1/*10, eight out of the ten most common genotypes (*1/*2, *1/*4, *1/*1, *2/*4, *4/*4, *2/*2, *4/*41, *1/*41) in an Austrian sample reported by Beer et al. were also found amongst the ten most frequent genotypes observed in our study [28].
4.2 Implication for Policy
As this study was not intended to find an association between adverse drug reactions and patients’ CYP2D6 metaboliser status, future prospective research on this topic is needed.
4.3 Strengths and Weaknesses of the Study
To our knowledge, this seems to be the only study performed in the setting of a general medical practice that described previously unknown allele and genotype frequencies as well as the metaboliser status in patients treated with drugs metabolised by the CYP2D6 enzyme. The study approach reflected the usual clinical situation of an unknown metaboliser status when starting the therapy. Thus, it was possible to find out that knowledge of the CYP2D6 metaboliser status would have been clinically relevant in approximately 17.42% of patients in whom a therapy with CYP2D6-specific drugs was started. Frequency data on CYP2D6 alleles, genotypes and metaboliser status found in patients of an elderly Austrian general practice population are similar to data from other epidemiological studies in Austria and Europe. However, in this study, the findings are directly linked with the clinical relevance in practice.
A limitation of our study is the fact that it was performed in a single general practice, even though patients’ characteristics and the size of the practice are typical for an ordinary Austrian practice. Besides that, the prescription rates of CYP2D6-specific drugs highly correlated between the observer practice and all NOEGKK insured patients. That allows, to a certain extent, generalisation of our results to estimate the probability of prescribing a CYP2D6-specific drug to a patient who is not a NM. Another limitation is that only one member of the CYP family was tested although several drugs are also metabolised by other relevant members (e.g. CYP2C9, 2C19 or 3A4/5).
5 Conclusions
In 17.42% of patients (PM, IM or UM) with a prescription of a CYP2D6-metabolised drug, knowledge of the genetically defined metaboliser status would have been of immediate clinical relevance with respect to clinical guideline annotations, drug label annotations and clinical annotations.
References
Sistonen J, Fuselli S, Palo JU, Chauhan N, Padh H, Sajantila A. Pharmacogenetic variation at CYP2C9, CYP2C19, and CYP2D6 at global and microgeographic scales. Pharmacogenet Genom. 2009;19(2):170–9.
Zhou SF. Polymorphism of human cytochrome P450 2D6 and its clinical significance: part I. Clin Pharmacokinet. 2009;48(11):689–723.
Zhou SF. Polymorphism of human cytochrome P450 2D6 and its clinical significance: part II. Clin Pharmacokinet. 2009;48(12):761–804.
Owen RP, Sangkuhl K, Klein TE, Altman RB. Cytochrome P450 2D6. Pharmacogenet Genom. 2009;19(7):559–62.
Ingelman-Sundberg M, Sim SC, Gomez A, Rodriguez-Antona C. Influence of cytochrome P450 polymorphisms on drug therapies: pharmacogenetic, pharmacoepigenetic and clinical aspects. Pharmacol Ther. 2007;116(3):496–526.
Zanger UM, Schwab M. Cytochrome P450 enzymes in drug metabolism: regulation of gene expression, enzyme activities, and impact of genetic variation. Pharmacol Ther. 2013;138(1):103–41.
He ZX, Chen XW, Zhou ZW, Zhou SF. Impact of physiological, pathological and environmental factors on the expression and activity of human cytochrome P450 2D6 and implications in precision medicine. Drug Metab Rev. 2015;47(4):470–519.
Bradford LD. CYP2D6 allele frequency in European Caucasians, Asians, Africans and their descendants. Pharmacogenomics. 2002;3(2):229–43.
Wang B, Yang LP, Zhang XZ, Huang SQ, Bartlam M, Zhou SF. New insights into the structural characteristics and functional relevance of the human cytochrome P450 2D6 enzyme. Drug Metab Rev. 2009;41(4):573–643.
www.PharmVar.org/gene/CYP2D6. Accessed 20 Nov 2019.
Gaedigk A, Ingelman-Sundberg M, Miller NA, Leeder JS, Whirl-Carrillo M, Klein TE, et al. The Pharmacogene Variation (PharmVar) Consortium: incorporation of the human cytochrome P450 (CYP) allele nomenclature database. Clin Pharmacol Ther. 2018;103(3):399–401.
Gaedigk A, Sangkuhl K, Whirl-Carrillo M, Klein T, Leeder JS. Prediction of CYP2D6 phenotype from genotype across world populations. Genet Med. 2017;19(1):69–76.
Caudle KE, Dunnenberger HM, Freimuth RR, Peterson JF, Burlison JD, Whirl-Carrillo M, et al. Standardizing terms for clinical pharmacogenetic test results: consensus terms from the Clinical Pharmacogenetics Implementation Consortium (CPIC). Genet Med. 2017;19(2):215–23.
Del Tredici AL, Malhotra A, Dedek M, Espin F, Roach D, Zhu GD, et al. Frequency of CYP2D6 alleles including structural variants in the United States. Front Pharmacol. 2018;9:305.
Samer CF, Lorenzini KI, Rollason V, Daali Y, Desmeules JA. Applications of CYP450 testing in the clinical setting. Mol Diagn Ther. 2013;17(3):165–84.
Reynolds KK, McNally BA, Linder MW. Clinical utility and economic impact of CYP2D6 genotyping. Clin Lab Med. 2016;36(3):525–42.
Chang KL, Weitzel K, Schmidt S. Pharmacogenetics: using genetic information to guide drug therapy. Am Fam Physician. 2015;92(7):588–94.
Swen JJ, Nijenhuis M, de Boer A, Grandia L, Maitland-van der Zee AH, Mulder H, et al. Pharmacogenetics: from bench to byte: an update of guidelines. Clin Pharmacol Ther. 2011;89(5):662–73.
Crews KR, Gaedigk A, Dunnenberger HM, Leeder JS, Klein TE, Caudle KE, et al. Clinical Pharmacogenetics Implementation Consortium guidelines for cytochrome P450 2D6 genotype and codeine therapy: 2014 update. Clin Pharmacol Ther. 2014;95(4):376–82.
Hicks JK, Sangkuhl K, Swen JJ, Ellingrod VL, Muller DJ, Shimoda K, et al. Clinical pharmacogenetics implementation consortium guideline (CPIC) for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants: 2016 update. Clin Pharmacol Ther. 2017;102(1):37–44.
Hicks JK, Bishop JR, Sangkuhl K, Muller DJ, Ji Y, Leckband SG, et al. Clinical Pharmacogenetics Implementation Consortium (CPIC) guideline for CYP2D6 and CYP2C19 genotypes and dosing of selective serotonin reuptake inhibitors. Clin Pharmacol Ther. 2015;98(2):127–34.
Tan-Koi WC, Lim ES, Teo YY. Health regulatory communications of well-established safety-related pharmacogenomics associations in six developed countries: an evaluation of alignment. Pharmacogenom J. 2017;17(2):121–7.
van der Wouden CH, Cambon-Thomsen A, Cecchin E, Cheung KC, Davila-Fajardo CL, Deneer VH, et al. Implementing pharmacogenomics in Europe: design and implementation strategy of the ubiquitous pharmacogenomics consortium. Clin Pharmacol Ther. 2017;101(3):341–58.
Bank PCD, Caudle KE, Swen JJ, Gammal RS, Whirl-Carrillo M, Klein TE, et al. Comparison of the guidelines of the Clinical Pharmacogenetics Implementation Consortium and the Dutch Pharmacogenetics Working Group. Clin Pharmacol Ther. 2018;103(4):599–618.
Blagec K, Kuch W, Samwald M. The importance of gene–drug–drug-interactions in pharmacogenomics decision support: an analysis based on Austrian claims data. Stud Health Technol Inform. 2017;236:121–7.
Kuch W, Rinner C, Gall W, Samwald M. How many patients could benefit from pre-emptive pharmacogenomic testing and decision support? A retrospective study based on nationwide Austrian claims data. Stud Health Technol Inform. 2016;223:253–8.
Scantamburlo G, Tziolia K, Zopf M, Bernardinelli E, Soyal SM, Civello DA, et al. Allele drop out conferred by a frequent CYP2D6 genetic variation for commonly used CYP2D6*3 genotyping assays. Cell Physiol Biochem. 2017;43(6):2297–309.
Beer B, Erb R, Pitterl F, Niederstatter H, Maronas O, Gesteira A, et al. CYP2D6 genotyping by liquid chromatography-electrospray ionization mass spectrometry. Anal Bioanal Chem. 2011;400(8):2361–70.
Bjerrum L, Gonzalez Lopez-Valcarcel B, Petersen G. Risk factors for potential drug interactions in general practice. Eur J Gen Pract. 2008;14(1):23–9.
Koper D, Kamenski G, Flamm M, Bohmdorfer B, Sonnichsen A. Frequency of medication errors in primary care patients with polypharmacy. Fam Pract. 2013;30(3):313–9.
Ivanova SA, Filipenko ML, Vyalova NM, Voronina EN, Pozhidaev IV, Osmanova DZ, et al. CYP1A2 and CYP2D6 gene polymorphisms in schizophrenic patients with neuroleptic drug-induced side effects. Bull Exp Biol Med. 2016;160(5):687–90.
Kapitany T, Meszaros K, Lenzinger E, Schindler SD, Barnas C, Fuchs K, et al. Genetic polymorphisms for drug metabolism (CYP2D6) and tardive dyskinesia in schizophrenia. Schizophr Res. 1998;32(2):101–6.
Koola MM, Tsapakis EM, Wright P, Smith S, Kerwin Rip RW, Nugent KL, et al. Association of tardive dyskinesia with variation in CYP2D6: is there a role for active metabolites? J Psychopharmacol. 2014;28(7):665–70.
Fleeman N, Dundar Y, Dickson R, Jorgensen A, Pushpakom S, McLeod C, et al. Cytochrome P450 testing for prescribing antipsychotics in adults with schizophrenia: systematic review and meta-analyses. Pharmacogenom J. 2011;11(1):1–14.
Pratt V, McLeod H, Rubinstein W, Dean L, Kattman B, Malheiro A. Thioridazine Therapy and CYP2D6 Genotypes. Medical Genetics Summaries. https://www.ncbi.nlm.nih.gov/pubmed/28520378. Bethesda (MD) National Center for Biotechnology Information (US); 2012–2017 Feb 9.
Taranu A, Colle R, Gressier F, El Asmar K, Becquemont L, Corruble E, et al. Should a routine genotyping of CYP2D6 and CYP2C19 genetic polymorphisms be recommended to predict venlafaxine efficacy in depressed patients treated in psychiatric settings? Pharmacogenomics. 2017;18(7):639–50.
MacNeil RR, Muller DJ. Genetics of common antipsychotic-induced adverse effects. Mol Neuropsychiatry. 2016;2(2):61–78.
https://www.pharmgkb.org/. Accessed 20 Nov 2019.
Bijl MJ, Visser LE, van Schaik RH, Kors JA, Witteman JC, Hofman A, et al. Genetic variation in the CYP2D6 gene is associated with a lower heart rate and blood pressure in beta-blocker users. Clin Pharmacol Ther. 2009;85(1):45–50.
https://cpicpgx.org/resources/cyp2d6-genotype-to-phenotype-standardization-project/. Accessed 20 Nov 2019.
Gaedigk A, Sangkuhl K, Whirl-Carrillo M, Klein T, Leeder JS. Corrigendum: prediction of CYP2D6 phenotype from genotype across world populations. Genet Med. 2016;18(11):1167.
https://www.pharmgkb.org/gene/PA128/guidelineAnnotation. Accessed 20 Nov 2019.
https://www.pharmgkb.org/gene/PA128/labelAnnotation. Accessed 20 Nov 2019.
https://www.pharmgkb.org/gene/PA128/clinicalAnnotation. Accessed 20 Nov 2019.
Ingelman-Sundberg M. Pharmacogenetics of cytochrome P450 and its applications in drug therapy: the past, present and future. Trends Pharmacol Sci. 2004;25(4):193–200.
Ganoci L, Bozina T, Mirosevic Skvrce N, Lovric M, Mas P, Bozina N. Genetic polymorphisms of cytochrome P450 enzymes: CYP2C9, CYP2C19, CYP2D6, CYP3A4, and CYP3A5 in the Croatian population. Drug Metab Pers Ther. 2017;32(1):11–21.
Buzkova H, Pechandova K, Slanar O, Perlik F. Frequency of single nucleotide polymorphisms of CYP2D6 in the Czech population. Cell Biochem Funct. 2008;26(1):76–81.
https://www.pharmgkb.org/combination/PA128,PA448385/guidelineAnnotation/PA166105006. Accessed 20 Nov 2019.
https://www.pharmgkb.org/labelAnnotation/PA166104839. Accessed 20 Nov 2019.
https://www.pharmgkb.org/labelAnnotation/PA166104813. Accessed 20 Nov 2019.
https://www.pharmgkb.org/combination/PA128,PA449048/guidelineAnnotation/PA166105007. Accessed 20 Nov 2019.
https://www.pharmgkb.org/combination/PA128,PA449088/guidelineAnnotation/PA166104996. Accessed 20 Nov 2019.
https://www.pharmgkb.org/combination/PA128,PA449273/labelAnnotation/PA166104886. Accessed 20 Nov 2019.
https://www.pharmgkb.org/combination/PA449394,PA128/labelAnnotation/PA166105113. Accessed 20 Nov 2019.
https://www.pharmgkb.org/guidelineAnnotation/PA166104969. Accessed 20 Nov 2019.
https://www.pharmgkb.org/combination/PA449673,PA128/clinicalAnnotation/1183619037. Accessed 20 Nov 2019.
https://www.pharmgkb.org/guidelineAnnotation/PA166104988. Accessed 20 Nov 2019.
https://www.pharmgkb.org/labelAnnotation/PA166178750. Accessed 20 Nov 2019.
https://www.pharmgkb.org/guidelineAnnotation/PA166104995. Accessed 20 Nov 2019.
https://www.pharmgkb.org/combination/PA450705,PA128/guidelineAnnotation/PA166161954. Accessed 20 Nov 2019.
https://www.pharmgkb.org/combination/PA450741,PA128/labelAnnotation/PA166184177. Accessed 20 Nov 2019.
https://www.pharmgkb.org/guidelineAnnotation/PA166127636. Accessed 20 Nov 2019.
https://www.pharmgkb.org/guidelineAnnotation/PA166104962. Accessed 20 Nov 2019.
https://www.pharmgkb.org/guidelineAnnotation/PA166176068. Accessed 20 Nov 2019.
https://www.pharmgkb.org/combination/PA128,PA451583/labelAnnotation/PA166160672. Accessed 20 Nov 2019.
https://www.pharmgkb.org/labelAnnotation/PA166104806. Accessed 20 Nov 2019.
https://www.pharmgkb.org/guidelineAnnotation/PA166104959. Accessed 20 Nov 2019.
https://www.pharmgkb.org/guidelineAnnotation/PA166104968. Accessed 20 Nov 2019.
Acknowledgements
This research project, co-produced by patients and researchers, was only possible as our patients agreed to participate and gave permission to analyse their CYP2D6-specific pharmacogenetics parameters. We want to thank them for their participation and trust. The authors also thank the staff of the NOEGKK (Lower Austrian Area Health Insurance) for providing prescription frequencies of CYP2D6-specific drugs and global data of drug prescriptions. The authors further thank Barbara Hauser (ViennaLab Diagnostic GmbH) for her valuable support in the laboratory work.
Author information
Authors and Affiliations
Contributions
GK initiated, planned and surveyed the study and contributed to data acquisition and laboratory work. SA performed the laboratory work, structured, compressed and analysed the raw data and helped in setting up the tables. AB provided support in the laboratory work, helped to analyse and interpret data on allele and genotype distribution and helped in the manuscript preparation. WF helped in drafting the manuscript and critically analysed the relevance of the pharmacogenetics data for general practice. LK helped in developing the research question and study concept, performed literature research and helped in manuscript preparation. HP helped with analysing and interpreting pharmacogenetics data and in the manuscript preparation. SZ was involved in the study by conducting the statistical work, preparing the tables and by critically revising the final results and conclusions of the study. All authors saw, commented and approved the final version of the paper. GK is the guarantor of the study.
Corresponding author
Ethics declarations
Funding
No sources of funding were received for the conduct of this study or the preparation of this article.
Conflict of interest
Gustav Kamenski, Seda Ayazseven, Anne Berndt, Waltraud Fink, Lukas Kamenski, Sonja Zehetmayer and Helene Pühringer have completed the Unified Competing Interest form (available on request from the corresponding author) and declare the following: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous 3 years, and no other relationships or activities that could appear to have influenced the submitted work.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the Ethics Committee of Lower Austria (ID GS1-EK-4/413-2016).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Data sharing
All data generated or analysed during the study are included in this published article and its supplementary information files.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kamenski, G., Ayazseven, S., Berndt, A. et al. Clinical Relevance of CYP2D6 Polymorphisms in Patients of an Austrian Medical Practice: A Family Practice-Based Observational Study. Drugs - Real World Outcomes 7, 63–73 (2020). https://doi.org/10.1007/s40801-019-00177-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40801-019-00177-4