Abstract
Purpose of Review
Bedwetting is a common chief complaint for patients presenting to primary care and urology as well as nephrology practices. Although nocturnal enuresis caused by anatomic and/or physiologic pathology is uncommon, monosymptomatic nocturnal enuresis can still be a source of significant stress and result in quality-of-life concerns. Accurate evaluation and management of these patients will ideally result in a notable increase in quality of life and assurance of overall wellness.
Recent Findings
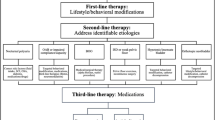
Persistent nocturnal enuresis is thought to be closely associated with deep sleeping patterns, and thus treatment with bedwetting alarms provides the best statistical opportunity for accelerated resolution of bedwetting. Pharmacotherapy options, namely, desmopressin, can provide temporary symptomatic relief which may be important in reducing anxiety related to bed-wetting based on social situations. Alternative therapies are likely worth exploring for patients without a notable response to initial treatment and concern or worry about the presence of nocturnal enuresis.
Summary
A significant volume of pediatric patients presenting to primary care and pediatric urology and nephrology practices will have voiding/enuresis-related chief complaints, and a notable proportion of these have monosymptomatic nocturnal enuresis. A thorough initial evaluation and implementation of targeted therapies can effectively enhance the quality of life for the patient and their families.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Nevéus T, Fonseca E, Franco I, et al. Management and treatment of nocturnal enuresis-an updated standardization document from the International Children’s Continence Society. J Pediatr Urol. 2020;16:10–9. https://doi.org/10.1016/j.jpurol.2019.12.020. This study is vital for establishing accepted vocabulary related to nocturnal enuresis across a variety of specialties and individual providers in a variety of practice settings. These terms further help clarify the differences between day wetting and night wetting as well as monosymptomatic vs. non-monosymptomatic enuresis. Identifying monosymptomatic vs. non-monosymptomatic enuresis is crucial for informing treatment decisions
Jansson UB, Hanson M, Sillén U, Hellström AL. Voiding pattern and acquisition of bladder control from birth to age 6 years--a longitudinal study. J Urol. 2005;174:289–93. https://doi.org/10.1097/01.ju.0000161216.45653.e3.
Nevéus T. Nocturnal enuresis-theoretic background and practical guidelines. Pediatr Nephrol. 2011;26:1207–14. https://doi.org/10.1007/s00467-011-1762-8.
Kuwertz-Bröking E, von Gontard A. Clinical management of nocturnal enuresis. Pediatr Nephrol. 2018;33:1145–54. https://doi.org/10.1007/s00467-017-3778-1.
Zeevenhooven J, Koppen IJ, Benninga MA. The New Rome IV Criteria for functional gastrointestinal disorders in infants and toddlers. Pediatr Gastroenterol Hepatol Nutr. 2017;20:1–13. https://doi.org/10.5223/pghn.2017.20.1.1.
de Sena Oliveira AC, BDS A, FCC M, et al. Attention deficit and hyperactivity disorder and nocturnal enuresis co-occurrence in the pediatric population: a systematic review and meta-analysis. Pediatr Nephrol. 2021;36:3547–59. https://doi.org/10.1007/s00467-021-05083-y. This article explores possible connections between children with enuresis and neurodiversity, namely, ADHD. Although additional studies will be needed in the future to further elucidate how this may impact treatment of enuresis, establishing the connection is a key first step
von Gontard A, Baeyens D, Van Hoecke E, Warzak WJ, Bachmann C. Psychological and psychiatric issues in urinary and fecal incontinence. J Urol. 2011;185:1432–6. https://doi.org/10.1016/j.juro.2010.11.051.
Baeyens D, Roeyers H, D'Haese L, Pieters F, Hoebeke P, Vande WJ. The prevalence of ADHD in children with enuresis: comparison between a tertiary and non-tertiary care sample. Acta Paediatr. 2006;95:347–52. https://doi.org/10.1080/08035250500434736.
Baeyens D, Roeyers H, Van Erdeghem S, Hoebeke P, Vande WJ. The prevalence of attention deficit-hyperactivity disorder in children with nonmonosymptomatic nocturnal enuresis: a 4-year followup study. J Urol. 2007;178:2616–20. https://doi.org/10.1016/j.juro.2007.07.059.
Wolf RB, Kassim AA, Goodpaster RL, DeBaun MR. Nocturnal enuresis in sickle cell disease. Expert Rev Hematol. 2014;7:245–54. https://doi.org/10.1586/17474086.2014.892412.
Al-Asadi JN, Radhi AM, Jumaa DS, Hassan MK. The role of hyposthenuria in enuresis among paediatric patients with cickle cell disease. Sultan Qaboos Univ Med J. 2023;23:206–11. https://doi.org/10.18295/squmj.9.2022.056.
Gaye O, Seck M, Thiam NM, Ndong A, Fall PA. Enuresis and overactive bladder in sickle cell patients: a narrative review of the literature [published correction appears in World J Urol 2023 Apr 6;]. World J Urol. 2023;41:953–62. https://doi.org/10.1007/s00345-023-04288-0.
Fergusson DM, Horwood LJ, Shannon FT. Factors related to the age of attainment of nocturnal bladder control: an 8-year longitudinal study. Pediatrics. 1986;78:884–90.
Bakker E, van Sprundel M, van der Auwera JC, van Gool JD, Wyndaele JJ. Voiding habits and wetting in a population of 4,332 Belgian schoolchildren aged between 10 and 14 years. Scand J Urol Nephrol. 2002;36:354–62. https://doi.org/10.1080/003655902320783863.
Howe AC, Walker CE. Behavioral management of toilet training, enuresis, and encopresis. Pediatr Clin North Am. 1992;39:413–32. https://doi.org/10.1016/s0031-3955(16)38336-5.
Walker RA. Nocturnal Enuresis. Prim Care. 2019;46:243–8. https://doi.org/10.1016/j.pop.2019.02.005.
Caldwell PH, Sureshkumar P, Wong WC. Tricyclic and related drugs for nocturnal enuresis in children. Cochrane Database Syst Rev. 2016;(1):CD002117. https://doi.org/10.1002/14651858.CD002117.pub2.
Deshpande AV, Caldwell PH, Sureshkumar P. Drugs for nocturnal enuresis in children (other than desmopressin and tricyclics). Cochrane Database Syst Rev. 2012;12(12):CD002238. https://doi.org/10.1002/14651858.CD002238.pub2.
Toale J, Kelly G, Hajduk P, Cascio S. Assessing the outcomes of parasacral transcutaneous electrical nerve stimulation (PTENS) in the treatment of enuresis in children: a systematic review and meta-analysis of randomized control trials. Neurourol Urodyn. 2022;41:1659–69. https://doi.org/10.1002/nau.25039. This article explores alterative treatments of nocturnal enuresis, specifically neurostimulation. These studies are crucial in allowing clinicians to broaden treatment options and explore variations in treatment that may lead to better response rates
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Angelina Dixon declares no conflict of interest. Brian Miller declares no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Nephrology
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dixon, A., Miller, B. Clinical Management of Nocturnal Enuresis. Curr Treat Options Peds 10, 1–12 (2024). https://doi.org/10.1007/s40746-023-00291-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-023-00291-0