Abstract
Introduction
Ixekizumab, an interleukin 17A (IL-17A) inhibitor, has demonstrated rapid and sustained improvement in the signs and symptoms in patients with active radiographic axial spondyloarthritis (r-axSpA) in global and Chinese populations. We studied the effect of ixekizumab on patient-reported outcomes (PROs) (including patient global, spinal pain, stiffness, and fatigue) and overall health-related quality of life (HRQoL) of ixekizumab in the phase 3 study in China.
Methods
In this Chinese phase 3, randomized, double-blind, placebo-controlled study, patients with r-axSpA were randomized (1:1) to receive ixekizumab 80 mg every 4 weeks (IXEQ4W; starting dose 160 mg) or placebo for 16 weeks. At week 16, patients receiving placebo were switched to IXEQ4W, and those receiving IXEQ4W continued, until week 52. Data for patient global, spinal pain, spinal pain at night, stiffness, and fatigue were collected through week 52. Minimally clinical important differences (MCIDs) were determined for spinal pain and spinal pain at night. The subgroup analyses by baseline disease duration since diagnosis and baseline C-reactive protein (CRP) level were conducted post hoc.
Results
Compared with placebo, patients treated with IXEQ4W reported significantly greater improvement with a rapid onset in changes from baseline of PROs (patient global, spinal pain, spinal pain at night, stiffness, and fatigue) through week 16. Improvements were maintained through week 52. A similar trend of improvement was also observed in MCID response in spinal pain and spinal pain at night. The improvement in overall HRQoL was supported by EQ-5D-5L assessment. Subgroup analyses demonstrated that IXEQ4W provided significantly greater efficacy at week 16 compared with placebo, irrespective of baseline disease duration or baseline CRP level.
Conclusion
IXEQ4W provided rapid and sustained improvement in clinically relevant PROs and overall HRQoL through 1-year treatment in Chinese patients with r-axSpA. Regardless of the baseline disease duration or baseline CRP level, consistent efficacy was observed.
Trial Registration
ClinicalTrials.gov identifier NCT04285229.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out the study? |
The interleukin-17A inhibitor ixekizumab (80 mg given every 4 weeks: IXEQ4W) has demonstrated rapid and sustained improvement in the signs and symptoms as well as health-related quality of life (HRQoL) in patients with active radiographic axial spondyloarthritis (r-axSpA) in two international phase 3 trials (COAST-V and COAST-W). |
The efficacy and safety results of ixekizumab in Chinese patients with r-axSpA had been proven in a randomized, double-blind, placebo-controlled, phase 3 study. |
Treatment effects of ixekizumab on pain relief and HRQoL improvement in Chinese patients with r-axSpA have not been reported. |
What was learned from this study? |
IXEQ4W (starting dose 160 mg) was associated with rapid and significant improvements in the PROs (patient global, spinal pain, spinal pain at night, stiffness, and fatigue) of active r-axSpA in Chinese patients at week 16 that were sustained until week 52. |
Regardless of the baseline disease duration since diagnosis and baseline C-reactive protein (CRP) level, patients can gain relief from the common symptoms and improve HRQoL by IXEQ4W treatment. |
Introduction
Radiographic axial spondyloarthritis (r-axSpA), also known as ankylosing spondylitis (AS), is a chronic inflammatory condition that affects the sacroiliac joint, spine, and entheses [1, 2]. Patients with r-axSpA experience negative impact on health-related quality of life (HRQoL) with signs and symptoms including spinal pain, stiffness, sleep loss, and fatigue, which can be improved after treatment [3]. Physical therapy and non-steroidal anti-inflammatory drugs (NSAIDs) are considered as first-line treatment in axSpA (including both r-axSpA and non-radiographic axial spondyloarthritis [nr-axSpA]) [4], followed by biological disease-modifying anti-rheumatic drugs (bDMARDs) including tumor necrosis factor inhibitors (TNFis) and interleukin (IL)-17 inhibitors [5, 6].
Chronic back pain is the cardinal feature of r-axSpA, associated with morning stiffness which can be improved with exercise but not rest [7]. This characteristic pattern of back pain in patients with r-axSpA is related to inflammation in the sacroiliac joints and in the spine. Inflammation can lead to bone destruction and repair, which allows subsequent new bone formation and results in mobility restrictions in axial joints.
Fatigue, correlated with quality of life, functional capacity, and depression [8], has been identified as one of the key patient-reported outcomes (PROs) in patients with r-axSpA [9, 10]. Pain is the factor most associated with fatigue and therefore treatment targeting pain management and inflammation control can relieve symptoms of fatigue in patients with r-axSpA [11].
Ixekizumab, a high-affinity interleukin-17A (IL-17A) inhibitor, has demonstrated rapid and sustained improvement in the signs and symptoms in patients with active r-axSpA in two international phase 3 trials (COAST-V and COAST-W) [12,13,14]. In addition, ixekizumab was reported to improve the HRQoL in patients with r-axSpA measured by various of PRO endpoints in these two trials [15,16,17].
The clinical characteristics of patients with r-axSpA are similar across different countries. As in other countries, the most common clinical manifestations of patients with r-axSpA in China include lower back pain and stiffness [18]. However, treatment effects on pain relief and HRQoL improvement in Chinese patients with r-axSpA are rarely reported. Previously, the efficacy and safety results of ixekizumab in Chinese patients with r-axSpA had been proven in a randomized, double-blind, placebo-controlled, phase 3 study [19]. In this article, we focus on the impact on PROs (including patient global, spinal pain, stiffness, and fatigue) and overall HRQoL of ixekizumab in this phase 3 study, as well as the subgroup analyses by baseline disease duration since diagnosis and baseline C-reactive protein (CRP) level.
Methods
Study Design
Descriptions of the designs of this Chinese phase 3, randomized, double-blind, placebo-controlled study (ClinicalTrials.gov NCT04285229) have been published previously [19]. The efficacy and safety of ixekizumab was assessed for 80 mg every 4 weeks (starting dose of 160 mg) compared with placebo during a 16-week, double-blind, placebo-controlled treatment period, followed by a 36-week, open-label extended treatment period (up to 52 weeks). Local ethics committees approved the study protocol, and the study was conducted in accordance with the principles outlined in the Declaration of Helsinki and the Council of International Organizations of Medical Sciences International Ethical Guidelines. Written informed consent was obtained for all patients.
Patients
Patients enrolled were Chinese adults fulfilling the Assessment of SpondyloArthritis International Society (ASAS) criteria for r-axSpA (having radiographic evidence of sacroilitis according to the modified New York criteria and having ≥ 1 spondyloarthritis feature), as well as a history of back pain for ≥ 3 months and age at onset < 45 years. Patients were also required to be either biologic disease-modifying antirheumatic drug (bDMARD)-naïve or have been treated with one TNFi that was discontinued as a result of an inadequate response or intolerance and have elevated baseline CRP. Full inclusion and exclusion criteria have been previously described [19].
Patient-Reported Outcomes
Changes from baseline in patient global, spinal pain, and stiffness are secondary endpoints in this study. Improvement in the symptoms of spinal pain at night and fatigue were also evaluated. The patient global Numeric Rating Scale (NRS) is an 11-point (0–10) scale used to assess the disease activity by patients’ self-report [20]. The spinal pain Numeric Rating Scale (NRS) is an 11-point (0–10) scale to used assess the pain intensity by patients’ self-report. Patients were asked to answer two questions in order to make two pain ratings corresponding to the intensity of spinal pain at any time and during the night, as described in the ASAS handbook [20]. Stiffness was evaluated as the average score from responses to BASDAI question 5 (intensity of morning stiffness) and question 6 (duration of morning stiffness) (BASDAI Q5/Q6) [20, 21]. Fatigue was measured by BASDAI question 1 (BASDAI Q1) [20, 21]. Assessments were conducted at week 0, 1, 2, 4, 8, 12, and 16 during the double-blind treatment period, and week 20, 24, 28, 32, 36, 44, 48, and 52 during the extended treatment period [19].
EQ-5D-5L is a patient-reported instrument used to assess health status [22]. The EQ-5D-5L consists of two components, including a description of the respondent’s health and a rating of their current health state using a 0- to 100-mm visual analog scale (VAS). An EQ-5D-5L Chinese population-based index score was derived to produce a patient-level index score between 0 and 1 [23]. EQ-5D-5L data were collected at week 0, 16, and 52.
Statistical Analyses
Detailed information of statistical analyses has been described previously [19]. Statistical analyses were conducted in the intention-to-treat (ITT) population, which was defined as all randomized patients (irrespective of whether they took the assigned study drug). Post hoc analyses were performed to evaluate the proportion of patients achieving minimum clinically important differences (MCIDs) in spinal pain and spinal pain at night, which was defined as a ≥ 1-point decrease from baseline [24, 25].
During the 16-week double-blind treatment period, the analyses of categorical outcomes (proportion of patients achieving MCID response) were undertaken using a logistic regression analysis with treatment, baseline CRP status, and TNFi experience in the model and using the non-responder imputation (NRI) method to impute missing data; continuous outcomes (change from baseline) were analyzed using a mixed model for repeated measures (MMRM) including treatment, baseline CRP status, TNFi experience, baseline value, visit, baseline value-by-visit, and treatment-by-visit as fixed effects (the variance–covariance matrix was unstructured) (except for EQ-5D-5L). Changes from baseline in EQ-5D-5L VAS score and Chinese population-based index score were analyzed at week 16 using an analysis of covariance (ANCOVA) model including treatment, baseline CRP status, TNFi experience, and baseline value and missing data were imputed using modified baseline observation carried forward (mBOCF) method.
During the extended treatment period from week 20 to week 52, both categorical and continuous outcomes were summarized descriptively. Missing data were imputed using the NRI method for the categorial outcomes and mBOCF method for continuous outcomes. No between-treatment comparisons were made.
In addition, post hoc subgroup analyses were conducted for changes from baseline of the PROs (patient global, spinal pain, spinal pain at night, stiffness, and fatigue) by baseline disease duration since diagnosis (< 5 years vs. ≥ 5 years) and baseline CRP level (≤ 5 mg/L vs. > 5 mg/L) using week 0 to week 16 data. Treatment group differences were evaluated within each category of the subgroup using MMRM mentioned above. Moreover, a treatment by subgroup interaction analysis was performed using MMRM mentioned above with treatment × visit × subgroup as an additional fixed effect.
Unless otherwise specified, p < 0.05 was considered statistically significant in the analyses conducted in this article.
Results
Baseline Characteristics
A total of 147 patients were randomized to receive placebo (n = 73) or ixekizumab 80 mg every 4 weeks (IXEQ4W) (n = 74) and comprised the ITT population. A total of 142 patients (96.6%) completed the 16-week, double-blind treatment period and entered the 36-week extended treatment period (placebo, 70 patients [95.9%]; IXEQ4W, 72 patients [97.3%]). Baseline disease characteristics for patients across treatment groups were generally similar (Table 1). Detailed baseline demographic and disease characteristics have been published previously [19].
Improvements in Spinal Pain, Stiffness, and Fatigue with Ixekizumab
Compared with placebo, patients treated with IXEQ4W had greater improvements in changes from baseline in patient global (Fig. 1a), spinal pain (Fig. 1b), spinal pain at night (Fig. 1c), stiffness (Fig. 1d), and fatigue (Fig. 1e) as well as MCID responses in spinal pain and spinal pain at night (Fig. 1f, g) throughout the 16-week, double-blind treatment period. Significant differences between the IXEQ4W and placebo groups across these PROs were observed as early as week 1 (Fig. 1). At week 16, MCID responses in spinal pain and spinal pain at night were achieved by 74.3% (p = 0.086, [vs. placebo]) and 78.4% (p = 0.011, [vs. placebo]) of patients receiving IXEQ4W, comparied with 60.3% and 57.5% of patients receiving placebo (Fig. 1f, g).
Changes from baseline in PROs (a patient global, b spinal pain, c spinal pain at night, d stiffness, and e fatigue) and MCID response rates (NRI) in f spinal pain and g spinal pain at night through week 52. Data of change from baseline are LSM for week 1–16 and mean for week 20–52. Changes from baseline (week 1–16) were analyzed using MMRM. Missing data of change from baseline (week 20–52) were imputed using mBOCF method (a–e). NRI was used for MCID response rates over 52 weeks in spinal pain and spinal pain at night (f, g). BASDAI Bath Ankylosing Spondylitis Disease Activity Index, IXEQ4W ixekizumab 80 mg every 4 weeks, LSM least squares mean, MCID minimally clinical important difference, MMRM mixed model for repeated measures, NRI non-responder imputation, PRO patient-reported outcome, Q question
Among patients who were initially randomized to receive IXEQ4W, improvements in these PROs were sustained through week 52 (Fig. 1). Patients randomized to receive placebo and switched to IXEQ4W at week 16 reported a rapid improvement in these PROs after switching through week 52 (Fig. 1).
Improvements in Overall HRQoL with Ixekizumab
Compared with placebo, patients treated with IXEQ4W had greater improvement in changes from baseline of EQ-5D-5L VAS score (2.6 vs. 7.9, p = 0.055) and Chinese population-based index score (0.05 vs. 0.13, p = 0.005) at week 16 (Fig. 2a, b). Improvement in EQ-5D-5L VAS score and Chinese population-based index score was sustained throughout week 52 in patients who were initially randomized to receive IXEQ4W (Fig. 2c, d). In addition, patients who received placebo from week 0 to 16 and switched to IXEQ4W showed improvement at week 52 as patients who received IXEQ4W from week 0 (Fig. 2c, d).
Changes from baseline in a, c EQ-5D-5L VAS score and b, d Chinese population-based index score at week 16 and week 52. Data of changes from baseline are LSM for week 16 and mean for week 52. China (Simplified Chinese) ©2011 EuroQol Group EQ-5D™ is a trademark of the EuroQol Group. EQ-5D-5L 5-level EQ-5D version, IXEQ4W ixekizumab 80 mg every 4 weeks, LSM least squares mean, VAS visual analog scale
Subgroup Analyses for PROs
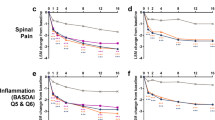
Figure 3 presents the treatment difference in change from baseline of PROs (patient global, spinal pain, spinal pain at night, stiffness, and fatigue) at week 16 for selected subgroups, including baseline disease duration since diagnosis (< 5 years vs. ≥ 5 years) and baseline CRP level (≤ 5 mg/L vs. > 5 mg/L). The subgroup analyses results were generally consistent with those from the overall population, and IXEQ4W demonstrated significantly greater efficacy compared with placebo across subgroups (all p < 0.05, except for fatigue-BASDAI [Q1] in the subgroup of baseline CRP level > 5 mg/L [p = 0.05]).
Treatment difference in change from baseline of PROs (patient global, spinal pain, spinal pain at night, stiffness, and fatigue) at week 16 in selected subgroups. Patient number in each subgroup (placebo vs. IXEQ4W): baseline CRP level > 5 mg/L, 53 vs. 44; baseline CRP level ≤ 5 mg/L, 20 vs 30; baseline disease duration since diagnosis ≥ 5 years, 36 vs. 37; baseline disease duration since diagnosis < 5 years, 37 vs. 37. BASDAI Bath Ankylosing Spondylitis Disease Activity Index, CI confidence interval, CRP C-reactive protein, Diff difference, IXEQ4W ixekizumab 80 mg every 4 weeks, LSM least squares mean, PRO patient-reported outcome, Q question
Treatment-by-subgroup interaction at week 16 for baseline disease duration since diagnosis (< 5 years vs. ≥ 5 years) and for baseline CRP level (≤ 5 mg/L vs. > 5 mg/L) did not reach significance in any of the above PROs at week 16 (all p ≥ 0.05, except for the treatment by baseline CRP interaction for fatigue-BASDAI [Q1]; p = 0.047).
Discussion
Key results from this phase 3 study in China have been published previously, showing that significant and rapid improvements in sign and symptoms were observed with IXEQ4W compared with placebo in Chinese patients with r-axSpA through week 16 and sustained through week 52 [19]. In the current article, we reported the effect of IXEQ4W on PROs and HRQoL in Chinese patients through week 16 and week 52, which was generally consistent with the published results in predominantly white populations in COAST-V and COAST-W trials [15, 17].
During the 16-week, double-blind, placebo-controlled period, significantly greater improvements with a rapid onset as early as week 1 were observed in IXEQ4W-treated patients for the PROs (patient global, spinal pain, spinal pain at night, stiffness, and fatigue). MCID responses in spinal pain at week 16 were numerically higher in the IXEQ4W group than placebo group, while the non-significant treatment effect might attributed to the limited sample size.
Effects on PROs were sustained or further improved through week 52 and were consistent for both the double-blind period (week 0 to week 16) and extended treatment period (week 16 to week 52). PROs in patients who received placebo and switched to IXEQ4W at week 16 were rapidly improved and reached a similar level at week 52 as patients who continuously received IXEQ4W.
The positive associations between concurrent improvements in PROs (including patient global, spinal pain, spinal pain at night, function, stiffness, fatigue, and sleep quality) and achievement of clinical response for ixekizumab in COAST-V and COAST-W studies were previously reported [17]. In addition, the relationship between r-axSpA remission and HRQoL improvement had been demonstrated for another IL-17 inhibitor [26]. These associations in the Chinese population warrant further investigation in the future.
Irrespective of baseline disease duration or baseline CRP level, the trend of significant improvement in the PROs (patient global, spinal pain, spinal pain at night, stiffness, and fatigue) from IXEQ4W treatment was also observed in patients with r-axSpA (Fig. 3). In addition, the treatment effects were numerically larger in patients with shorter disease duration (< 5 years) or lower CRP level (≤ 5 mg/L), suggesting IXEQ4W is also an effective therapeutic option for patients even in the absence of elevated CRP level or long disease duration. Post hoc analyses of the COAST-V and COAST-W trials demonstrated that ixekizumab was effective on ASAS40, BASDAI50, and SF-36 responses in patients with r-axSpA irrespective of the baseline CRP level [27,28,29,30,31,32]. In addition, another IL-17 inhibitor also showed efficacy at all baseline CRP levels [29, 30]. Overall, the response to IL-17 inhibitors seems to be independent of the baseline CRP level, but further evidence is needed.
The main strength of this analysis is that a diverse series of PRO endpoints were included in this phase 3 study and treatment duration was as long as 1 year. In addition, improvements in spinal pain and spinal pain at night were measured post hoc using MCID, defined as the smallest change perceived by patients to be beneficial, can be applied to further determine a clinically relevant change in a patient’s status [31, 32]. The fatigue score measured by BASDAI Q1 [21] is for r-axSpA and may be more disease-specific than FACIT-fatigue scale, which reflects the fatigue (both physical and psychological) during daily activities [33].
There were limitations in this study. Data interpretation for the extended treatment period (week 20 to week 52) is challenging and limited by no control arm (placebo) designed for this period. In addition, subgroup analyses were conducted post hoc and the sample size in subgroups was relatively limited.
Conclusion
IXEQ4W provided a rapid and sustained improvement in clinically relevant PROs (including patient global, spinal pain, stiffness, and fatigue) and HRQoL through 1 year treatment in Chinese patients with r-axSpA. Regardless of the baseline disease duration or baseline CRP level, patients can gain relief from the common symptoms and improve HRQoL by IXEQ4W treatment.
Data Availability
Lilly provides access to all individual participant data collected during the trial, after anonymization, with the exception of pharmacokinetic or genetic data. Data are available upon reasonable request. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data-sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, and blank or annotated case report forms, will be provided in a secure data-sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.
References
Walsh JA, Magrey M. Clinical manifestations and diagnosis of axial spondyloarthritis. J Clin Rheumatol. 2021;27(8):e547–60.
Sieper J, Poddubnyy D. Axial spondyloarthritis. Lancet. 2017;390(10089):73–84.
Strand V, Singh JA. Patient burden of axial spondyloarthritis. J Clin Rheumatol. 2017;23(7):383–91.
Ramiro S, Nikiphorou E, Sepriano A, et al. ASAS-EULAR recommendations for the management of axial spondyloarthritis: 2022 update. Ann Rheum Dis. 2023;82(1):19–34.
Tam LS, Wei JC, Aggarwal A, et al. 2018 APLAR axial spondyloarthritis treatment recommendations. Int J Rheum Dis. 2019;22(3):340–56.
Ward MM, Deodhar A, Gensler LS, et al. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network recommendations for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritis. Arthritis Rheumatol. 2019;71(10):1599–613.
Marina NM, Abhijeet SD, Joerg E, Jessica AW. Recognizing axial spondyloarthritis: a guide for primary care. Mayo Clin Proc. 2020;95(11):2499–508.
Schneeberger EE, Marengo MF, Dal Pra F, Maldonado Cocco JA, Citera G. Fatigue assessment and its impact in the quality of life of patients with ankylosing spondylitis. Clin Rheumatol. 2015;34(3):497–501.
Ulus Y, Akyol Y, Bilgici A, Kuru O. Association of work instability with fatigue and emotional status in patients with ankylosing spondylitis: comparison with healthy controls. Clin Rheumatol. 2019;38(4):1017–24.
Dean LE, Macfarlane GJ, Jones GT. Five potentially modifiable factors predict poor quality of life in ankylosing spondylitis: results from the Scotland Registry for Ankylosing Spondylitis. J Rheumatol. 2018;45(1):62–9.
Brophy S, Davies H, Dennis MS, et al. Fatigue in ankylosing spondylitis: treatment should focus on pain management. Semin Arthritis Rheum. 2013;42(4):361–7.
van der Heijde D, Cheng-Chung Wei J, Dougados M, et al. Ixekizumab, an interleukin-17A antagonist in the treatment of ankylosing spondylitis or radiographic axial spondyloarthritis in patients previously untreated with biological disease-modifying anti-rheumatic drugs (COAST-V): 16 week results of a phase 3 randomised, double-blind, active-controlled and placebo-controlled trial. Lancet. 2018;392(10163):2441–51.
Deodhar A, Poddubnyy D, Pacheco-Tena C, et al. Efficacy and safety of ixekizumab in the treatment of radiographic axial spondyloarthritis: sixteen-week results from a phase III randomized, double-blind, placebo-controlled trial in patients with prior inadequate response to or intolerance of tumor necrosis factor inhibitors. Arthritis Rheumatol. 2019;71(4):599–611.
Dougados M, Wei JC, Landewé R, et al. Efficacy and safety of ixekizumab through 52 weeks in two phase 3, randomised, controlled clinical trials in patients with active radiographic axial spondyloarthritis (COAST-V and COAST-W). Ann Rheum Dis. 2020;79(2):176–85.
Mease P, Walsh JA, Baraliakos X, et al. Translating improvements with ixekizumab in clinical trial outcomes into clinical practice: ASAS40, pain, fatigue, and sleep in ankylosing spondylitis. Rheumatol Ther. 2019;6(3):435–50.
Kiltz U, Wei JC, van der Heijde D, et al. Ixekizumab improves functioning and health in the treatment of radiographic axial spondyloarthritis: week 52 results from 2 pivotal studies. J Rheumatol. 2021;48(2):188–97.
Deodhar AA, Mease PJ, Rahman P, et al. Ixekizumab improves spinal pain, function, fatigue, stiffness, and sleep in radiographic axial spondyloarthritis: COAST-V/W 52-week results. BMC Rheumatol. 2021;5(1):35.
Zhang S, Peng L, Li Q, et al. Spectrum of spondyloarthritis among Chinese populations. Curr Rheumatol Rep. 2022;24(8):247–58.
Xue Y, Hu J, Liu D, et al. Ixekizumab for active radiographic axial spondyloarthritis in chinese patients: 16- and 52-week results from a phase III, randomized, double-blind, placebo-controlled study. BioDrugs. 2023. https://doi.org/10.1007/s40259-023-00625-2.
Sieper J, Rudwaleit M, Baraliakos X, et al. The Assessment of SpondyloArthritis International Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis. 2009;68(Suppl 2):1–44.
Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis: the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol. 1994;21(12):2286–91.
Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36.
Luo N, Liu G, Li M, Guan H, Jin X, Rand-Hendriksen K. Estimating an EQ-5D-5L value set for China. Value Health. 2017;20(4):662–9.
Navarro-Compán V, Wei JC, Van den Bosch F, et al. Effect of tofacitinib on pain, fatigue, health-related quality of life and work productivity in patients with active ankylosing spondylitis: results from a phase III, randomised, double-blind, placebo-controlled trial. RMD Open. 2022;8(2): e002253.
Sieper J, Kivitz A, van Tubergen A, et al. Impact of certolizumab pegol on patient-reported outcomes in patients with axial spondyloarthritis. Arthritis Care Res (Hoboken). 2015;67(10):1475–80.
Baraliakos X, Van den Bosch F, Machado PM, et al. Achievement of remission endpoints with secukinumab over 3 years in active ankylosing spondylitis: pooled analysis of two phase 3 studies. Rheumatol Ther. 2021;8(1):273–88.
Maksymowych WP, Bolce R, Gallo G, et al. Ixekizumab in radiographic axial spondyloarthritis with and without elevated C-reactive protein or positive magnetic resonance imaging. Rheumatology (Oxford). 2022;61(11):4324–34.
Maksymowych W, Marzo-Ortega H, Ǿstergaard M, et al. Efficacy of ixekizumab on disease activity and quality of life in patients with active nonradiographic axial spondyloarthritis and objective signs of inflammation, stratified by baseline CRP/Sacroiliac Joint MRI Status [abstract]. Arthritis Rheumatol. 2020;72(suppl 10)
Braun J, Deodhar A, Landewé R, Baraliakos X, et al. Impact of baseline C-reactive protein levels on the response to secukinumab in ankylosing spondylitis: 3-year pooled data from two phase III studies. RMD Open. 2018;4(2):e000749.
Deodhar A, Conaghan PG, Kvien TK, et al. Secukinumab provides rapid and persistent relief in pain and fatigue symptoms in patients with ankylosing spondylitis irrespective of baseline C-reactive protein levels or prior tumour necrosis factor inhibitor therapy: 2-year data from the MEASURE 2 study. Clin Exp Rheumatol. 2019;37(2):260–9.
Strand V, Boers M, Idzerda L, et al. It’s good to feel better but it’s better to feel good and even better to feel good as soon as possible for as long as possible. Response criteria and the importance of change at OMERACT 10. J Rheumatol. 2011;38(8):1720–7.
Beaton DE, Boers M, Wells GA. Many faces of the minimal clinically important difference (MCID): a literature review and directions for future research. Curr Opin Rheumatol. 2002;14(2):109–14.
Webster K, Cella D, Yost K. The functional assessment of chronic illness therapy (FACIT) measurement system: properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1:79.
Acknowledgements
Medical Writing/Editorial Assistance
Editorial assistance in the preparation of this article was provided by Huanjun Chen, a medical writer and employee of Eli Lilly and Company.
Authorship
All named authors of this article meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship, take responsibility for the integrity of the work as a whole, and have provided approval for this version to be published.
Funding
This study and this publication (including the journal’s Rapid Service Fee) were sponsored by Eli Lilly and Company.
Author information
Authors and Affiliations
Contributions
Hejian Zou, Xiaoxia Zhu, Jiankang Hu, Dongzhou Liu, Jingyang Li, Huaxiang Wu, Chunyu Tan, Lie Dai, Lingyun Sun, Zhijun Li, Zhengyu Xiao and Xiaomei Li contributed to the acquisition of data. Guanshen Dou and Yan Yan contributed to the design of work and the interpretation of data. Yuzi Sun contributed to data analysis and interpretation. All authors were involved in drafting or reviewing the article critically, and all authors approved the final version to be submitted for publication.
Corresponding author
Ethics declarations
Conflict of Interest
Guanshen Dou, Yan Yan and Yuzi Sun are employees and shareholders of Eli Lilly and Company. Hejian Zou received research grants from Eli Lilly and Company. Xiaoxia Zhu, Jiankang Hu, Dongzhou Liu, Jingyang Li, Huaxiang Wu, Chunyu Tan, Lie Dai, Lingyun Sun, Zhijun Li, Zhengyu Xiao and Xiaomei Li have no conflicts of interest to declare in relation to this work.
Ethical Approval
The study protocol was approved by local ethics committees and full list of the ethics review boards are available in previously published manuscript supplements [19]. The study was conducted in accordance with the principles outlined in the Declaration of Helsinki and the Council of International Organizations of Medical Sciences International Ethical Guidelines. Written informed consent was obtained for all patients.
Additional information
Prior Publication: Some of the results presented in this manuscript were accepted as “Abstract only” at the European 0) 2024, 12–15 June 2024, in Vienna, Austria (AB0912).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhu, X., Hu, J., Liu, D. et al. Rapid and Sustained Effect of Ixekizumab on Patient Global, Spinal Pain, Stiffness, and Fatigue in Chinese Patients with Radiographic Axial Spondyloarthritis. Rheumatol Ther (2024). https://doi.org/10.1007/s40744-024-00688-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40744-024-00688-9