Abstract
Introduction
This post hoc analysis of the phase 3 rheumatoid arthritis (RA) filgotinib clinical trial program assessed the effect of filgotinib on body mass index (BMI) in patients with RA and the impact of BMI on the efficacy and safety of filgotinib.
Methods
FINCH 1–3 were randomized, double-blind, active- or placebo-controlled phase 3 trials of filgotinib 100 and 200 mg in patients with RA (N = 3452). BMI assessments included the mean change from baseline in BMI and the proportion of patients whose BMI increased by incremental thresholds. Efficacy measures included American College of Rheumatology (ACR) 20/50/70 response and low disease activity/remission according to Disease Activity Score 28 using C-reactive protein. The exposure-adjusted incident rate (EAIR) of adverse events (AEs) was assessed by baseline BMI, using integrated data from the FINCH 1–4 and the phase 2 DARWIN 1–3 studies (total filgotinib exposure = 8085 patient-years).
Results
Mean change from baseline in BMI over time was similar across treatment arms. In most patients, BMI increased by ≤ 1 or 2 kg/m2 at both weeks 12 and 24, regardless of treatment group or baseline BMI; few patients had increases of ≥ 4 kg/m2. For most efficacy measures, filgotinib 200 mg was more efficacious than filgotinib 100 mg or active comparators or placebo across BMI subgroups. For the higher filgotinib dose, the EAIR of serious treatment-emergent AEs, venous thrombotic and embolic events, and major adverse cardiovascular events increased with increasing BMI.
Conclusions
Filgotinib did not lead to substantial changes in BMI, and BMI did not appear to affect the efficacy of filgotinib.
Trial Registration
ClinicalTrials.gov identifiers: NCT02889796, NCT02873936, NCT02886728, NCT03025308, NCT01888874, NCT01894516, NCT02065700.
Plain Language Summary
Some rheumatoid arthritis treatments cause patients to gain weight or are less effective in patients with obesity than in patients without obesity. Also, obesity can make rheumatoid arthritis worse. Filgotinib is a rheumatoid arthritis treatment that was evaluated in seven randomized clinical studies (FINCH 1–4 and DARWIN 1–3). We investigated whether filgotinib causes changes in weight and whether body mass index (BMI) affects the efficacy or safety of filgotinib. We analyzed how the BMI of patients who participated in FINCH 1, 2, or 3 changed over time. Most patients had a small increase in BMI (around 1–2 kg/m2) after 24 weeks of filgotinib treatment. This change in BMI was not affected by patients’ BMI at baseline. Baseline BMI did not impact the efficacy of filgotinib, which was assessed using standard measures of disease activity. Filgotinib was more effective than other rheumatoid arthritis treatments and placebo in all patients, regardless of BMI subgroup. Using safety data from all seven clinical studies (FINCH 1–4 and DARWIN 1–3), we found that some adverse events occurred more often in patients with obesity (a BMI of ≥ 30 kg/m2) than in those without obesity. The increased adverse events included venous thrombotic and embolic events and major adverse cardiovascular events, for which obesity is a known risk factor. These results show that filgotinib did not substantially change BMI (which increased by around 1–2 kg/m2 in most patients), and that baseline BMI did not affect the efficacy of filgotinib.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Obesity has been shown to negatively affect the effectiveness of some rheumatoid arthritis (RA) treatments; in addition, some RA treatments are associated with weight gain. |
This post hoc analysis of the FINCH 1–3 studies was conducted to assess the effect of filgotinib on the body mass index (BMI) of patients with RA and to evaluate the efficacy and safety of filgotinib according to baseline BMI. |
What was learned from the study? |
Filgotinib did not substantially change the BMI in patients with RA. |
Baseline BMI did not appear to affect the efficacy of filgotinib. |
Certain adverse events, including cardiovascular-related adverse events, occurred more frequently in high-BMI subgroups. |
Introduction
Rheumatoid arthritis (RA) is a chronic autoimmune disease that can lead to substantial pain, disability, and increased mortality [1,2,3]. As in the general population, a significant proportion of patients with RA (approximately two-thirds) are overweight or are obese [4, 5]. A recent study showed that although trends in body mass index (BMI) over time are similar in patients with and without RA, BMI is significantly more variable in those with RA [6]. Furthermore, the relationship between obesity and RA is complex. Due to the pain and joint damage associated with the condition, patients with RA may have inactive lifestyles, increasing the likelihood of obesity [7]. Secretion of pro-inflammatory cytokines from adipose tissue contributes to bone and cartilage damage, and, therefore, excess body weight may exacerbate RA disease activity [5, 8]. Such pro-inflammatory cytokines may also result in changes in body composition, which can extend to reduced muscle mass (cachexia), although this does not necessarily result in weight loss [3, 9]. Patients with RA and obesity have worse clinical and patient-reported outcomes and are less likely to achieve remission, compared with patients with RA without obesity [10,11,12]. The pharmacokinetics and effective dose of any drug is highly dependent on the BMI, and obesity in patients with RA has been shown to negatively impact the effectiveness of some RA treatments, such as tumor necrosis factor (TNF) inhibitors [12, 13]. In addition, weight gain has been reported as an effect of some RA treatments, including TNF inhibitors [14,15,16]. Therefore, for physicians to accurately inform patients and prescribe appropriate therapy, it is important to determine the potential impact of RA treatment on body weight or BMI and to understand if and to what extent therapeutic effects of RA treatments will be affected by a patient’s weight/BMI. Such information has not yet been determined for filgotinib, a Janus kinase (JAK) 1-preferential inhibitor, for the treatment of moderate-to-severe RA.
The primary objective of this post hoc analysis was to assess the effect of filgotinib on the BMI in patients with RA. The secondary objective was to assess the efficacy and safety of filgotinib according to baseline BMI. Analyses were based on data from 3452 patients from the FINCH 1–3 studies [17,18,19]; the safety analysis also included data from the FINCH 4 and DARWIN 1–3 studies (total filgotinib exposure = 8085 patient-years) [20,21,22,23].
Methods
Study Design
The effect of filgotinib on the BMI and the impact of BMI on the efficacy of filgotinib was assessed using data from the FINCH 1–3 studies. FINCH 1, 2, and 3 were randomized, double-blind, active- or placebo-controlled phase 3 trials of filgotinib 100 mg and 200 mg in patients with active RA. FINCH 1 (NCT02889796; N = 1755) was a 52-week study in which patients with an inadequate response to methotrexate were randomized to receive filgotinib (100 or 200 mg), adalimumab or placebo, each with background methotrexate. The primary endpoint was the proportion of patients to achieve American College of Rheumatology (ACR)20 response at week 12 [17]. FINCH 2 (NCT02873936; N = 448) was a 24-week study in which patients with an inadequate response to biologic disease-modifying anti-rheumatic drugs (bDMARDs) were assigned filgotinib (100 mg or 200 mg) or placebo, in addition to one or two protocol-specified conventional synthetic DMARDs. The primary endpoint was the proportion of patients to achieve ACR20 response at week 12 [18]. In FINCH 3 (NCT02886728; N = 1249), a 52-week study, patients who were methotrexate naïve received filgotinib 200 mg, methotrexate, or filgotinib 100 mg or 200 mg with methotrexate. The primary endpoint was the proportion of patients to achieve ACR20 response at week 24 [19]. The studies did not specify an upper BMI limit within their inclusion criteria, although patients were to be excluded if they had a chronic, uncontrolled condition, such as morbid obesity, that would, in the opinion of the investigator, put them at increased risk during the study [17,18,19]. To assess the impact of BMI on the safety of filgotinib, data from the FINCH 4 study and the DARWIN 1–3 studies were also assessed, in addition to safety data from FINCH 1–3. DARWIN 1 (NCT01888874) and DARWIN 2 (NCT01894516) were phase 2b, 24-week studies in which patients received filgotinib 50 mg, 100 mg or 200 mg, or placebo, either as an add-on treatment to methotrexate (DARWIN 1) or as monotherapy (DARWIN 2) [21, 22]. The phase 2 DARWIN 3 study (NCT02065700) and phase 3 FINCH 4 (NCT03025308) study are ongoing, open-label long-term extensions for patients who completed treatment in the DARWIN or FINCH parent studies, respectively [20, 23].
Ethical Approval
All studies were conducted in accordance with the Declaration of Helsinki of 1964, and its later amendments, and approved by the institutional review board or ethics committee; all patients provided written informed consent to participate in the study.
Assessments
Baseline Characteristics
Using pooled data from the three FINCH studies, baseline characteristics were assessed according to baseline BMI subgroup: < 25 (underweight/normal weight), 25 to < 30 (overweight), or ≥ 30 kg/m2 (obese). BMI categories of < 18.5 or ≥ 40 kg/m2 (corresponding to underweight or severe obesity, respectively) were not included as separate subgroups as these each encompassed less than 5% of the total number of patients. BMI (kg/m2) was calculated as follows: weight (kg)/height (m)2.
Changes from Baseline in BMI
Mean changes from baseline in BMI were assessed over time by treatment group for FINCH 1, 2, and 3. For each study, the following were assessed according to treatment group and baseline BMI subgroup: mean change from baseline in BMI at week 12 and week 24, the proportion of patients whose BMI increased by incremental thresholds (1, 2, and 3 kg/m2, etc.) and cumulative probability of change from baseline in BMI at week 12 and week 24. The proportion of patients who moved from one BMI category into the ≥ 25 to < 30 kg/m2 category or the ≥ 30 kg/m2 category, and the proportion of patients whose body weight increased from baseline by > 7%, were also assessed according to treatment group.
Efficacy
The efficacy of filgotinib was assessed by treatment group and baseline BMI subgroup at week 12 for FINCH 1 and 2 and at week 24 for FINCH 3. Efficacy measures included the proportion of patients to achieve: ACR20/50/70 response; Disease Activity Score 28 using C-reactive protein (DAS28-CRP) low disease activity and remission (≤ 3.2 and < 2.6, respectively); and Clinical Disease Activity Index (CDAI) low disease activity and remission (≤ 10.0 and ≤ 2.8, respectively). Mean change from baseline in Health Assessment Questionnaire–Disability Index (HAQ-DI) was also assessed.
Predictive Analysis Regression
Exploratory analyses were performed to further study the association between baseline BMI and treatment response using multivariate linear regression, with the following included as covariates: age, sex, ethnicity, smoking status, anti-cyclic citrullinated peptide (anti-CCP) antibody status, steroid use, and filgotinib dose. The analysis was performed with study included as a fixed effect, then repeated with study included as a random effect.
Safety
The safety of filgotinib was assessed by calculating the exposure-adjusted incident rate (EAIR) of advents events (AEs) per 100 patient-years of exposure, according to the baseline BMI subgroup, using integrated data from seven RA clinical trials (FINCH 1–4 and DARWIN 1–3) [24].
Results
Baseline Characteristics
Mean (SD) baseline BMI was 26.7 (5.83) kg/m2 in FINCH 1, 30.2 (7.59) kg/m2 in FINCH 2 and 27.7 (6.41) kg/m2 in FINCH 3. Supplementary Figure S1a shows the distribution of BMI values at baseline using pooled data from FINCH 1–3. Distributions were broadly similar in each study (Supplementary Figure S1b–d). Baseline characteristics according to baseline BMI, based on pooled data from FINCH 1–3, are shown in Table 1 (median values are provided in Supplementary Table S1). The overall mean duration of RA was 6.4 years. There were 1332 patients in the BMI < 25 kg/m2 subgroup, 1102 patients in the 25 to < 30 kg/m2 subgroup and 1018 patients in the ≥ 30 kg/m2 subgroup. The proportion of patients with rheumatoid factor and with anti-CCP antibodies present at baseline decreased with increasing BMI. The proportion of patients with prior exposure to bDMARDs was greatest in the ≥ 30 kg/m2 subgroup (21.2% vs. 9.9% and 13.2% in the < 25 and 25 to < 30 kg/m2 subgroups, respectively). Disease severity indicators (including HAQ-DI, DAS28-CRP, and CDAI) showed a slight increase with increasing BMI, but values were generally similar across BMI subgroups. In the ≥ 30 kg/m2 subgroup, 64.0% of patients had a history of cardiovascular risk, compared with 30.1% and 47.9% of those in the < 25 and 25 to < 30 kg/m2 subgroups, respectively. Mean creatinine clearance increased with increasing BMI (97.2 ml/min, 111.6 ml/min and 138.6 ml/min in the < 25, 25 to < 30 and ≥ 30 kg/m2 subgroups, respectively) as did the proportion of patients with high-sensitivity C-reactive protein (CRP) level ≥ 6 mg/l (57.8, 59.5, and 67.0% in the < 25, 25 to < 30, and ≥ 30 kg/m2 subgroups, respectively).
Change from Baseline in BMI
In general, mean changes from baseline in BMI were similar across treatment groups (Fig. 1a–c) and slightly greater with active treatment than with placebo. When assessed by baseline BMI subgroup at week 12 and 24, the greatest increase was 0.8 kg/m2, which was seen at week 24 in the filgotinib 200 mg treatment arm of FINCH 3, in both the < 25 and 25 to < 30 kg/m2 subgroups (Table 2). In all three FINCH studies, the majority of patients had increases in BMI of ≤ 1 or 2 kg/m2 regardless of treatment group or baseline BMI; very few patients had increases of ≥ 4 kg/m2 (Supplementary Tables S2–4). The proportion of patients who changed from one BMI category to another is shown in Supplementary Table S5. At week 24, the proportion of patients who moved into the obese state ranged from 1.7% (adalimumab) to 2.1% (placebo) in FINCH 1; 2.1% (placebo) to 5.1% (filgotinib 100 mg) in FINCH 2; and 1.6% (filgotinib 200 mg + methotrexate) to 5.9% (filgotinib 200 mg) in FINCH 3. The proportion of patients with a change from baseline in body weight of > 7% at week 24 was 6.2, 6.3, 4.5, and 2.9% in the filgotinib 200 mg, filgotinib 100 mg, adalimumab, and placebo arms, respectively (FINCH 1); 6.3, 9.4, and 5.3% in the filgotinib 200 mg, filgotinib 100 mg, and placebo arms, respectively (FINCH 2); and 9.9, 15.3, 15.5, and 8.6%, in the filgotinib 200 mg plus methotrexate, filgotinib 100 mg plus methotrexate, filgotinib 200 mg, and methotrexate arms, respectively (FINCH 3) (Supplementary Table S6). Cumulative probability plots of change from baseline in BMI according to baseline BMI in FINCH 1–3 are presented in Supplementary Figures S2–4.
Mean change from baseline in BMI over time in FINCH 1 (a) FINCH 2 (b), and FINCH 3 (c). Safety analysis set (includes enrolled patients who received ≥ 1 dose of study drug). Baseline value was the last available value collected on or prior to first dose of study drug. In FINCH 1 at week 24, all subjects assigned to PBO who did not discontinue study drug were re-randomised 1:1 to either FIL200 or FIL100 and continued in the study through week 52. For re-randomized PBO patients, baseline value after week 24 was the last available value collected on or prior to the first dose of FIL. Follow-up visit was defined as from (last dose date of any study drug + 8 days [FINCH 1 and 3] or + 6 days [FINCH 2]) to (last dose date of any study drug + 30 days). BMI (kg/m2) = [weight (kg)/height (cm)2] × 10,000. ADA adalimumab, BMI body mass index, FIL(100/200), filgotinib 100/200 mg, MTX methotrexate, PBO placebo, SD standard deviation
Efficacy
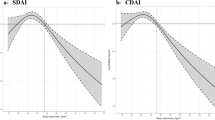
Filgotinib 200 mg with or without methotrexate was more efficacious than controls regardless of baseline BMI at each timepoint for most measures, including ACR20, ACR50, and ACR70 responses (Fig. 2a–c), DAS28-CRP low disease activity or remission (Fig. 3a,b), CDAI low disease activity or remission (Supplementary Figure S5a,b) and HAQ-DI (Supplementary Figure S6). Across BMI subgroups, filgotinib 200 mg was generally more efficacious than filgotinib 100 mg for most efficacy outcomes.
Proportion of patients to achieve ACR20 (a), ACR50 (b), and ACR70 (c) responses at week 12 (FINCH 1 and 2) or week 24 (FINCH 3), by baseline BMI. Full analysis set. Values above each column are the number of evaluable patients. ACR American College of Rheumatology, ADA adalimumab, BMI body mass index, FIL100/200 filgotinib 100/200 mg, MTX methotrexate, PBO placebo
Proportion of patients to achieve DAS28-CRP low disease activity (a) or remission (b) at week 12 (FINCH 1 and 2) or week 24 (FINCH 3) by baseline BMI. Full analysis set. Values above each column are the number of evaluable patients. ADA adalimumab, BMI body mass index, DAS28-CRP Disease Activity Score 28 using C-reactive protein, FIL100/200 filgotinib 100/200 mg, MTX methotrexate, PBO placebo
Predictive Regression
After accounting for patient age, sex, ethnicity, smoking status, anti-CCP status, steroid use, and filgotinib dose, a linear regression model with study included as a fixed effect indicated that a higher BMI was associated with a poorer DAS28-CRP response. However, the absolute difference in response was small, with a 10 kg/m2 difference in BMI corresponding to a 0.2-unit difference in DAS28-CRP change (Supplementary Table S7). Similar results were observed when study was included as a random effect (Supplementary Table S8).
Safety
Table 3 summarizes EAIRs of AEs of special interest across baseline BMI subgroups, using integrated safety data from FINCH 1–4 and DARWIN 1–3. In patients with BMI ≥ 30 kg/m2, the EAIR of serious treatment-emergent adverse events (TEAEs) was higher than in those with a BMI of 25 to < 30 or < 25 kg/m2 in both the filgotinib 200 mg and filgotinib 100 mg groups. The EAIR of venous thrombotic and embolic (VTE) events was numerically higher in the ≥ 30 kg/m2 subgroup than in the other subgroups within the filgotinib 200 mg arm, although the absolute number of events was low. Within the filgotinib 200 mg arm, the EAIR (95% CI) of major adverse cardiovascular events (MACE) was 0.5 (0.2, 1.0) in the ≥ 30 kg/m2 subgroup versus 0.3 (0.1, 0.7) and 0.3 (0.2, 0.7) in the 25 to < 30 and < 25 kg/m2 subgroups, respectively. In the filgotinib 200 mg treatment arm, the rate of serious infections was numerically highest in the ≥ 30 kg/m2 subgroup, while in the filgotinib 100 mg treatment arm, it was numerically highest in the < 25 kg/m2 subgroup. The EAIRs of deaths, herpes zoster, and malignancies excluding non-melanoma skin cancer were similar across BMI subgroups for each filgotinib dose. When comparing filgotinib doses, the EAIR of deaths was numerically higher with filgotinib 200 mg vs. 100 mg in the 25 to < 30 and ≥ 30 kg/m2 subgroups but not in the < 25 kg/m2 subgroup. Long-term data are not available for the active comparator or placebo groups.
Discussion
During the FINCH 1–3 studies, BMI did not substantially change from baseline with filgotinib treatment. Filgotinib 200 mg was generally more efficacious than controls, regardless of baseline BMI. Filgotinib 100 mg was also generally more efficacious than controls across BMI subgroups but to a lesser extent and less consistently than the higher dose. Across BMI subgroups, filgotinib 200 mg was generally more effective than filgotinib 100 mg for most efficacy outcomes. Similar to our findings, a pooled analysis of data from six phase 3 trials showed that compared with placebo, tofacitinib treatment was associated with greater improvements in efficacy measures for each baseline BMI subgroup assessed (< 25, 25 to < 30, and ≥ 30 kg/m2) [25]. Previous studies have demonstrated that obesity has a negative impact on response to TNF inhibitors, particularly infliximab, even when dosed according to body weight [26,27,28]. In contrast, therapeutic response to the interleukin (IL)-6 receptor inhibitor tocilizumab (administered intravenously according to body weight) was found to be unaffected by baseline BMI [29]. A recent study found that the difference in effect of obesity on therapeutic responses to TNF inhibitors and tocilizumab was likely due to mechanisms involved in the production of pro-inflammatory cytokines; the authors concluded that therapies other than TNF inhibitors would be more suitable for patients with obesity [30]. These findings may be relevant to JAK inhibitors, as they also inhibit IL-6 signaling [31] and therefore may be less impacted by BMI than TNF inhibitors. In our study, while the results of the predictive regression analysis suggested that higher BMI may be associated with poorer DAS28-CRP responses to filgotinib, the absolute differences in response were unlikely to be clinically meaningful. In addition, this association may be partially influenced by the higher CRP levels seen in the ≥ 30 kg/m2 subgroup at baseline. Of note, we observed that the proportion of patients who had prior exposure to bDMARDs increased with increasing BMI, which may indicate that prior bDMARDs have been less effective in patients with obesity.
Pooled safety data from FINCH 1–4 and DARWIN 1–3 showed that the rate of TEAEs, including serious TEAEs and VTEs, was numerically higher in the ≥ 30 kg/m2 subgroup than in the 25 to < 30 or < 25 kg/m2 subgroups. These findings are as expected given that high BMI is a known risk for the TEAEs reported [32,33,34,35]. Cardiovascular risk associated with RA treatment is an important consideration, especially in patients with obesity who are already at increased cardiovascular risk. In our analysis, as expected, increased levels of CRP, which are associated with increased cardiovascular risk, were observed in patients with the highest BMI at baseline. In addition, the proportion of patients with cardiovascular risk factors, which included a medical history of ischemic heart disease, was greater in the ≥ 30 kg/m2 subgroup than in the 25 to < 30 or < 25 kg/m2 subgroups, and the former subgroup also had a numerically higher rate of VTEs. This observation is in line with the results of a post hoc analysis of the Oral Rheumatoid Arthritis Trial (ORAL) Surveillance study, which found tofacitinib-treated patients with a history of atherosclerotic cardiovascular disease to be at increased risk of MACE [36]. In our analysis, the rate of serious infections was highest in the ≥ 30 and < 25 kg/m2 subgroups in the filgotinib 200 mg and 100 mg treatment arms, respectively; mean baseline fasting glucose levels also generally increased with increasing BMI, which may be linked to increased risk of infection [37]. Our assessment of baseline characteristics showed that creatinine clearance increased with increasing BMI. This finding is consistent with previously published data which also indicated a positive correlation between these two parameters [38]. Our analysis showed that the proportion of RF-positive patients decreased with increasing BMI, in agreement with an association that has been described previously in patients with RA [39].
Weight gain is reported as an uncommon side effect (may affect up to one in 100 people) of baricitinib and tofacitinib, and as a common side effect (may affect up to one in ten people) of upadacitinib [40,41,42]. Compared with patients taking placebo, a numerically greater proportion of those treated with baricitinib experienced abnormal weight gain, defined as an increase of 7% or more from the highest value recorded at baseline, regardless of baseline body weight [43]. The proportion of patients with abnormal weight gain decreased with increasing baseline body weight or BMI; the difference with placebo was only statistically significant for patients with the lowest body weight at baseline (those who had a body weight < 60 kg and a BMI < 25 kg/m2) [40]. Across the FINCH studies, there was no apparent dose-dependent effect of filgotinib on body weight, as measured by an increase of > 7%, and the proportion of patients whose body weight increased by > 7% from baseline was generally similar between active comparators.
There is no standard definition for abnormal or clinically meaningful changes in BMI. Weight loss of ≥ 5% is often used to indicate a clinically meaningful reduction for patients with obesity [44]. As noted above, an increase of 7% or more from the highest recorded baseline body weight was used to define an abnormal increase in patients in baricitinib trials [43]. Whether or not a change in BMI is clinically relevant is dependent on the patient’s baseline BMI. In patients who are underweight at baseline, weight gain may be a return to normal weight, so it would not be considered an AE. However, if a patient of normal weight at baseline became overweight or obese, weight gain would be considered an AE. Patients who are overweight or obese may lose weight if their RA improves and they become more active.
Limitations of the analysis include its post hoc nature and the possible effect of external weight loss interventions, such as changes to diet or physical activity, which could not be controlled or measured. In addition, weight gain is a reported side effect of corticosteroids [45], which were taken concurrently by 44.2% of patients at baseline. Information regarding corticosteroid use throughout the studies, such as the proportion of patients who discontinued corticosteroids or tapered the dose of corticosteroids, is lacking, so it is not possible to ascertain their potential impact on the findings. Furthermore, while the mean corticosteroid dose at baseline has been reported, we are unable to report the dose level for each corticosteroid administered. Given that specific corticosteroids are dosed differently to reach equivalent levels the extent to which the mean dose can be interpreted is limited. Ethnicity data were also not available for the pooled populations by BMI subgroup, so it is not possible to determine possible impact on weight. Patients with a BMI ≥ 40 kg/m2 were not included as a separate subgroup given the low number of patients comprising this category. Therefore, outcomes in patients with severe obesity, who may present in clinical practice, were not assessed. There are also limitations associated with the use of BMI as a parameter. In RA, changes in body composition, specifically a loss of lean body mass and an increase in adiposity, have been reported, which may be associated with increased cardiovascular risk [7, 46, 47]. Such changes may be predominantly due to the systemic inflammation associated with the condition. However, alterations may also be induced by corticosteroids or bDMARDs [46]. In the current analysis, BMI ≥ 30 kg/m2 was used as a surrogate for obesity; there is an absence of data regarding changes in fat mass/body composition, which can only be determined by dual-energy X-ray absorptiometry or bioelectrical impedance analysis [48]. In addition, cardio-metabolic risk may be better reflected by other measures, such as waist circumference or waist-to-hip ratio [7, 25]. However, BMI is a suitable parameter for physicians to use in clinical practice.
Conclusions
Patient weight/BMI is an important consideration when treating RA, as obesity has been shown to negatively affect clinical outcomes and response to treatment [10,11,12]. Findings from this post hoc analysis of the FINCH 1–3 studies indicate that filgotinib did not result in substantial changes from baseline in BMI, and that it was an effective treatment for RA across all BMI subgroups. While the predictive regression analysis indicated poorer DAS28-CRP response with higher BMI, the difference was small and not considered clinically meaningful. As expected, the incidence of serious TEAEs and VTE events was higher in the ≥ 30 kg/m2 baseline BMI subgroups than in the 25 to < 30 or < 25 kg/m2 baseline BMI subgroups.
Data Availability
Anonymized individual patient data will be shared upon request for research purposes dependent upon the nature of the request, the merit of the proposed research and the availability of the data and their intended use. The full data sharing policy for Gilead Sciences, Inc., can be found at https://www.gilead.com/about/ethics-and-code-of-conduct/policies. Data sharing policy for Galapagos NV can be found at https://www.clinicaltrials-glpg.com/us/en/data-transparency.html.
References
Shams S, Martinez JM, Dawson JRD, et al. The therapeutic landscape of rheumatoid arthritis: current state and future directions. Front Pharmacol. 2021;12: 680043.
Romao VC, Fonseca JE. Etiology and risk factors for rheumatoid arthritis: a state-of-the-art review. Front Med (Lausanne). 2021;8: 689698.
Santo RCE, Fernandes KZ, Lora PS, Filippin LI, Xavier RM. Prevalence of rheumatoid cachexia in rheumatoid arthritis: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle. 2018;9:816–25.
Stavropoulos-Kalinoglou A, Metsios GS, Koutedakis Y, Kitas GD. Obesity in rheumatoid arthritis. Rheumatology (Oxford). 2011;50:450–62.
Arias de la Rosa I, Escudero-Contreras A, Ruiz-Ponce M, et al. Molecular changes in the adipose tissue induced by rheumatoid arthritis: effects of disease-modifying anti-rheumatic drugs. Front Immunol. 2021;12:744022.
Challener GJ, Myasoedova E, Crowson CS, Giblon RE, Atkinson EJ, Davis JM 3rd. Body mass index trend and variability in rheumatoid arthritis. Clin Rheumatol. 2022;41:349–55.
Zegkos T, Kitas G, Dimitroulas T. Cardiovascular risk in rheumatoid arthritis: assessment, management and next steps. Ther Adv Musculoskelet Dis. 2016;8:86–101.
Feng J, Chen Q, Yu F, et al. Body mass index and risk of rheumatoid arthritis: a meta-analysis of observational studies. Medicine (Baltimore). 2016;95: e2859.
Masuko K. Rheumatoid cachexia revisited: a metabolic co-morbidity in rheumatoid arthritis. Front Nutr. 2014;1:20.
Liu Y, Hazlewood GS, Kaplan GG, Eksteen B, Barnabe C. Impact of obesity on remission and disease activity in rheumatoid arthritis: a systematic review and meta-analysis. Arthritis Care Res (Hoboken). 2017;69:157–65.
Vidal C, Barnetche T, Morel J, Combe B, Daien C. Association of body mass index categories with disease activity and radiographic joint damage in rheumatoid arthritis: a systematic review and meta-analysis. J Rheumatol. 2015;42:2261–9.
Levitsky A, Brismar K, Hafstrom I, et al. Obesity is a strong predictor of worse clinical outcomes and treatment responses in early rheumatoid arthritis: results from the SWEFOT trial. RMD Open. 2017;3: e000458.
Singh S, Facciorusso A, Singh AG, et al. Obesity and response to anti-tumor necrosis factor-alpha agents in patients with select immune-mediated inflammatory diseases: a systematic review and meta-analysis. PLoS ONE. 2018;13: e0195123.
Lutf A, Hammoudeh M. Weight gain and hair loss during anti-TNF therapy. Int J Rheumatol. 2012;2012: 593039.
Alcorn N, Tierney A, Wu O, Gilmour H, Madhok R. Impact of anti-tumour necrosis factor therapy on the weight of patients with rheumatoid arthritis. Ann Rheum Dis. 2010;69:1571.
Engvall IL, Tengstrand B, Brismar K, Hafstrom I. Infliximab therapy increases body fat mass in early rheumatoid arthritis independently of changes in disease activity and levels of leptin and adiponectin: a randomised study over 21 months. Arthritis Res Ther. 2010;12:R197.
Combe B, Kivitz A, Tanaka Y, et al. Filgotinib versus placebo or adalimumab in patients with rheumatoid arthritis and inadequate response to methotrexate: a phase III randomised clinical trial. Ann Rheum Dis. 2021;80:848–58.
Genovese MC, Kalunian K, Gottenberg JE, et al. Effect of filgotinib vs placebo on clinical response in patients with moderate to severe rheumatoid arthritis refractory to disease-modifying antirheumatic drug therapy: the FINCH 2 randomized clinical trial. JAMA. 2019;322:315–25.
Westhovens R, Rigby WFC, van der Heijde D, et al. Filgotinib in combination with methotrexate or as monotherapy versus methotrexate monotherapy in patients with active rheumatoid arthritis and limited or no prior exposure to methotrexate: the phase 3, randomised controlled FINCH 3 trial. Ann Rheum Dis. 2021;80:727–38.
ClinicalTrials.gov. NCT03025308: long term extension study to assess the safety and efficacy of filgotinib in adults with rheumatoid arthritis (FINCH 4). https://clinicaltrials.gov/ct2/show/NCT03025308?term=FINCH+4&draw=2&rank=1. Accessed 17 Jan 2023.
Kavanaugh A, Kremer J, Ponce L, et al. Filgotinib (GLPG0634/GS-6034), an oral selective JAK1 inhibitor, is effective as monotherapy in patients with active rheumatoid arthritis: results from a randomised, dose-finding study (DARWIN 2). Ann Rheum Dis. 2017;76:1009–19.
Westhovens R, Taylor PC, Alten R, et al. Filgotinib (GLPG0634/GS-6034), an oral JAK1 selective inhibitor, is effective in combination with methotrexate (MTX) in patients with active rheumatoid arthritis and insufficient response to MTX: results from a randomised, dose-finding study (DARWIN 1). Ann Rheum Dis. 2017;76:998–1008.
ClinicalTrials.gov. NCT02065700: long-term follow-up study of GLPG0634 in active rheumatoid arthritis patients (DARWIN3). https://clinicaltrials.gov/ct2/show/NCT02065700?term=DARWIN+3&draw=2&rank=1. Accessed 17 Jan 2023.
Winthrop K, Tanaka Y, Takeuchi T, et al. Integrated safety analysis update for filgotinib in patients with moderately to severely active rheumatoid arthritis receiving treatment over a median of 2.2 years. Arthritis Rheumatol. 2021;73(Suppl 9):1698 (abstract).
Dikranian AH, Gonzalez-Gay MA, Wellborne F, et al. Efficacy of tofacitinib in patients with rheumatoid arthritis stratified by baseline body mass index: an analysis of pooled data from phase 3 studies. RMD Open. 2022;8: e002103.
Klaasen R, Wijbrandts CA, Gerlag DM, Tak PP. Body mass index and clinical response to infliximab in rheumatoid arthritis. Arthritis Rheum. 2011;63:359–64.
Ottaviani S, Gardette A, Tubach F, et al. Body mass index and response to infliximab in rheumatoid arthritis. Clin Exp Rheumatol. 2015;33:478–83.
Gremese E, Carletto A, Padovan M, et al. Obesity and reduction of the response rate to anti-tumor necrosis factor alpha in rheumatoid arthritis: an approach to a personalized medicine. Arthritis Care Res (Hoboken). 2013;65:94–100.
Pers YM, Godfrin-Valnet M, Lambert J, et al. Response to tocilizumab in rheumatoid arthritis is not influenced by the body mass index of the patient. J Rheumatol. 2015;42:580–4.
Novella-Navarro M, Genre F, Hernandez-Breijo B, et al. Obesity and response to biological therapy in rheumatoid arthritis: the role of body mass index and adipose tissue cytokines. Clin Exp Rheumatol. 2022;40:1726–32.
McInnes IB, Byers NL, Higgs RE, et al. Comparison of baricitinib, upadacitinib, and tofacitinib mediated regulation of cytokine signaling in human leukocyte subpopulations. Arthritis Res Ther. 2019;21:183.
Lutsey PL, Zakai NA. Epidemiology and prevention of venous thromboembolism. Nat Rev Cardiol. 2023;20:248–62.
Poirier P, Giles TD, Bray GA, et al. Obesity and cardiovascular disease: pathophysiology, evaluation, and effect of weight loss. Arterioscler Thromb Vasc Biol. 2006;26:968–76.
Falagas ME, Kompoti M. Obesity and infection. Lancet Infect Dis. 2006;6:438–46.
Wolin KY, Carson K, Colditz GA. Obesity and cancer. Oncologist. 2010;15:556–65.
Charles-Schoeman C, Buch MH, Dougados M, et al. Risk of major adverse cardiovascular events with tofacitinib versus tumour necrosis factor inhibitors in patients with rheumatoid arthritis with or without a history of atherosclerotic cardiovascular disease: a post hoc analysis from ORAL surveillance. Ann Rheum Dis. 2023;82:119–29.
Butler SO, Btaiche IF, Alaniz C. Relationship between hyperglycemia and infection in critically ill patients. Pharmacotherapy. 2005;25:963–76.
Gerchman F, Tong J, Utzschneider KM, et al. Body mass index is associated with increased creatinine clearance by a mechanism independent of body fat distribution. J Clin Endocrinol Metab. 2009;94:3781–8.
Baker JF, George M, Baker DG, Toedter G, Von Feldt JM, Leonard MB. Associations between body mass, radiographic joint damage, adipokines and risk factors for bone loss in rheumatoid arthritis. Rheumatology (Oxford). 2011;50:2100–7.
European Medicines Agency. Olumiant: summary of product characteristics 2022. https://www.ema.europa.eu/en/documents/product-information/olumiant-epar-product-information_en.pdf. Accessed 26 July 2022.
European Medicines Agency. XELJANZ: summary of product characteristics. 2022. https://www.ema.europa.eu/en/documents/product-information/xeljanz-epar-product-information_en.pdf. Accessed 27 Jan 2023.
European Medicines Agency. RINVOQ: summary of product characteristics. 2022. https://www.ema.europa.eu/en/documents/product-information/rinvoq-epar-product-information_en.pdf. Accessed 27 Jan 2023.
Eli Lilly. Olumiant® (baricitinib): weight gain in rheumatoid arthritis. 2022. https://www.lillymedical.eu/en-gb/answers/olumiant-baricitinib-weight-gain-in-rheumatoid-arthritis-92642#reference-2ec6b15b-be79-4810-9bbf-b800b079c723-9. Accessed 14 Nov 2022.
Horn DB, Almandoz JP, Look M. What is clinically relevant weight loss for your patients and how can it be achieved? A narrative review. Postgrad Med. 2022;134:359–75.
Ethgen O, de Lemos EF, Bruyere O, Reginster JY. What do we know about the safety of corticosteroids in rheumatoid arthritis? Curr Med Res Opin. 2013;29:1147–60.
Letarouilly JG, Flipo RM, Cortet B, Tournadre A, Paccou J. Body composition in patients with rheumatoid arthritis: a narrative literature review. Ther Adv Musculoskelet Dis. 2021;13:1759720X211015006.
de Souza M, Guimaraes N, Guimaraes M, de Souza V, Kakehasi A. Effect of biological disease-modifying antirheumatic drugs on body composition in patients with rheumatoid arthritis: a systematic review and meta-analysis. Adv Rheumatol. 2022;62:16.
Marra M, Sammarco R, De Lorenzo A, et al. Assessment of body composition in health and disease using bioelectrical impedance analysis (BIA) and dual energy X-ray absorptiometry (DXA): a critical overview. Contrast Media Mol Imaging. 2019;2019:3548284.
Acknowledgements
We thank the physicians and patients who participated in these studies.
Medical Writing, Editorial and Other Assistance
Publication coordination was provided by Fabien Debailleul, PhD, of Galapagos NV. Medical writing support was provided by Debbie Sherwood, BSc, CMPP (Aspire Scientific Ltd, Bollington, UK), and funded by Galapagos NV (Mechelen, Belgium).
Funding
The FINCH studies were funded by Gilead Sciences (Foster City, CA, USA). The journal’s Rapid Service Fee was funded by Galapagos NV (Mechelen, Belgium).
Author information
Authors and Affiliations
Contributions
All authors (Alejandro Balsa, Siegfried Wassenberg, Yoshiya Tanaka, Anne Tournadre, Hans-Dieter Orzechowski, Vijay Rajendran, Udo Lendl, Pieter-Jan Stiers, Chris Watson, Roberto Caporali, James Galloway and Patrick Verschueren) made substantial contributions to the conception or design of the work, or the acquisition, analysis or interpretation of data; critically revised the manuscript for intellectual content; approved the final version submitted for publication and take responsibility for the integrity and accuracy of the work.
Corresponding author
Ethics declarations
Conflict of Interest
Alejandro Balsa has received grants/research support from AbbVie, Pfizer and UCB; worked as a paid consultant for AbbVie, Galapagos, Lilly, Nordic, Pfizer and UCB; and has been paid as a speaker for AbbVie, Galapagos, Gilead, Lilly, Nordic, Pfizer, Sandoz and UCB. Siegfried Wassenberg has received grants/research support from Pfizer; worked as a paid consultant for Galapagos, Lilly and UCB; and has been paid as a speaker for AbbVie, Medac, MSD and Pfizer. Yoshiya Tanaka received speaker fees and/or honoraria from AbbVie, AstraZeneca, Boehringer-Ingelheim, BMS, Chugai, Eisai, Eli Lilly, Gilead, GlaxoSmithKline, Pfizer, Taiho, and Taisho and received research grants from Chugai, Eisai, Mitsubishi-Tanabe Taisho. Anne Tournadre has received grants/research support from Novartis, Pfizer and UCB; worked as a paid consultant for AbbVie, Fresenius Kabi, Lilly, Novartis and Sanofi; and has been paid as an instructor for Fresenius Kabi, and as a speaker for Fresenius Kabi, Lilly, MSD and Sanofi. Hans-Dieter Orzechowski is a former employee of Galapagos and a shareholder in Gilead; Udo Lendl is an employee of Galapagos; Pieter-Jan Stiers is a former employee of Galapagos; Vijay Rajendran and Chris Watson are employees at, and shareholders in, Galapagos. Roberto Caporali worked as a paid consultant, and has been paid as a speaker, for AbbVie, Accord, BMS, Celltrion, Fresenius Kabi, Galapagos, Lilly, MSD, Novartis, Pfizer, Sandoz and UCB. James Galloway has worked as a paid consultant for AbbVie, Galapagos, Gilead, Janssen, Lilly, Novartis and Pfizer; has received grant/research support from AstraZeneca, Celgene, Gilead, Jansen, Medicago, Novavax and Pfizer; has received speaker fees/honoraria from AbbVie, Biogen, Galapagos, Gilead, Janssen, Lilly, Novartis, Pfizer, Roche and UCB. Patrick Verschueren has received institutional grants/research support from Galapagos (Galapagos Chair in Rheumatoid Arthritis at KU Leuven, Belgium, outside the scope of the current study) and Pfizer (Pfizer Chair Management of Early Rheumatoid Arthritis at KU Leuven, Belgium); worked as a paid consultant for AbbVie, BMS, Celltrion, Eli Lilly, Galapagos, Gilead, Nordic Pharma, Pfizer, Sidekick Health and UCB; and has been paid as a speaker for Eli Lilly, Galapagos, MSD and Roularta.
Ethical Approval
All studies were conducted in accordance with the Declaration of Helsinki of 1964, and its later amendments, and approved by the institutional review board or ethics committee; all patients provided written informed consent to participate in the study.
Additional information
Prior Presentation: Selected data in this manuscript were previously presented at EULAR 2022 (June 1–4, 2022, Copenhagen, Denmark).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Balsa, A., Wassenberg, S., Tanaka, Y. et al. Effect of Filgotinib on Body Mass Index (BMI) and Effect of Baseline BMI on the Efficacy and Safety of Filgotinib in Rheumatoid Arthritis. Rheumatol Ther 10, 1555–1574 (2023). https://doi.org/10.1007/s40744-023-00599-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-023-00599-1