Abstract
Introduction
Recently, a study showing the non-inferiority of a single injection of sodium hyaluronate plus sorbitol (Synolis VA®) compared to hylan G-F20 (Synvisc-One®) over a 24-week period in patients with knee osteoarthritis was published. The objective of the present study is to assess if a short-term response to a single injection of sodium hyaluronate plus sorbitol can be maintained over a 6 month-period and if the maintenance of the response to treatment is dependent on the functional status at baseline.
Methods
Responders to treatment at days 28, 84, and 168 were evaluated according to the responder criteria proposed by the OMERACT-OARSI. The Western Ontario and McMaster Universities Arthritis Index (WOMAC) was used to assess functional status at baseline. All analyses were adjusted for age, gender, BMI, and baseline WOMAC total score using data from the intention-to-treat (ITT) population.
Results
Out of the 96 patients included in the study who were receiving Synolis VA®, 59.38% were responders at day 28 according to the OMERACT/OARSI responder criteria, 59.78% at day 84, and 64.52% at day 168. Among the responders at D28, the probability of being responder at D84 and D168 was significantly higher than among non-responders, with corresponding odds ratio (95% CI) of 2.85 (1.07–7.59) and 7.28 (2.53–20.93), respectively. Patients with a poorer physical function at baseline were more likely to respond to the treatment at all time points, compared to those with a better physical function (OR 3.74 [1.37–10.21]).
Conclusions
An early response of a single injection of sodium hyaluronate plus sorbitol is predictive of long-term response, up to 24 weeks. Patients with a poorer physical function may best benefit from the treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Daily knee osteoarthritis pain trajectories are unstable in a substantial proportion of patients, suggesting that a short-term improvement with an intervention may not be sustained over time. |
There is therefore a need to understand whether a short-term response to treatment is maintained over time. |
In the present study, we show that if a patient responds within 1 month to a single injection of sodium hyaluronate plus sorbitol, prescribers can be confident in the long term (up to 6 months). |
For patients who do not respond in the short term, the likelihood of a 6-month response is limited and other treatment options can be considered. |
Introduction
The projected progressive aging of the population in the next decades will increase the incidence of osteoarthritis (OA), the most prevalent form of arthritis that may strongly affect the quality of life of patients. If it is not possible to currently definitively cure the disease, clinicians have interesting options to manage it. Recent guidelines strongly emphasize the importance to have a combination of pharmacological and non-pharmacological therapies [1]. Among pharmacological therapies, intra-articular hyaluronic acid (IAHA) injections have been proposed for many years [2]. An interesting review by Altman et al. noted that 86% (19/22) of the 13 professional organizations and 8 global agencies focusing on musculoskeletal disease that published guidelines for IAHA were either neutral or in favor of IAHA treatment for OA knee pain [3]. When focusing on recent international guidelines, i.e., the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Osteoarthritis Research Society International (OARSI), they both consider IAHA as a relevant option in the management of OA [1]. Of course, there is some heterogeneity between trials, which highlights the importance of using an IAHA product that has been thoroughly investigated and has been shown to be effective in a randomized controlled trial [4].
On the other hand, it is crucial for patients to experience meaningful and sustained improvement over an extended period. Indeed, because the daily knee OA pain trajectories are unstable in almost half of the patients, as highlighted in a recent systematic review [5], a short-term improvement with an intervention may not be sustainable over time. It is therefore necessary to study whether a short-term response to treatment is maintained over a longer period.
We have previously shown in a 6-month, randomized, double-blinded trial the non-inferiority of one IAHA compared to another one (i.e., one made of 80 mg hyaluronic acid and 160 mg sorbitol and the other made of 48 mg hylan GF-20) in terms of pain and function efficacy in patients with OA [6]. In this particular study, the response rate (i.e., using the OMERACT-OARSI set of responder criteria) to the IAHA made of HA and sorbitol was 79% at the end of the study. From that study, we also showed that the probability of a meaningful response to IAHA was increased if administered in patients with more impaired physical function at baseline [7]. The primary objective of the present post hoc study was to investigate if a short-term response to this IAHA can be maintained over a long-term period (i.e., 6 months). Our secondary objective was to assess whether the maintenance of the response to treatment was dependent on the functional status at baseline.
Methods
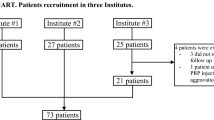
This is a post hoc analysis of a previously published randomized, double-blind trial, with non-inferiority design, comparing a single injection of sodium hyaluronate plus sorbitol (Synolis VA®) to hylan G-F20 (Synvisc-One®), which demonstrated the non-inferiority of Synolis VA® compared to Synvisc-One® [6]. The trial was conducted in accordance with the ethics principles of the Declaration of Helsinki. It was approved and registered under no. 2017-A00034-49 to the ANSM, and ethical approval was obtained from CPP Ile-de-France VI. Ref: CPP/6-17-ID RCB: 2017-A00034-49.
The Previous Studies
The original study was a 24-week duration study, with the main outcome results assessed at days 28, 84, and 168. The Synolis VA® is a viscosupplement containing 80 mg of hyaluronic acid and 160 mg of sorbitol, while the Synvisc-One® is made up of 48 mg hylan GF-20. The exhaustive methodology of the initial trial has been previously published elsewhere but briefly, the original study included male and female patients, aged between 45 and 80 years, with radiologically confirmed knee OA, according to the American College of Rheumatology criteria. The primary end point was the evolution of the Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain index from day 0 (injection time) to day 168 (end of study). The secondary end points included specific subscales of the WOMAC index (i.e., pain, function, and stiffness) and WOMAC total scores assessed at days 28, 84, and 168. The number of responders to treatment at days 28, 84, and 168 was also evaluated, according to the responder criteria proposed by the Osteoarthritis Research Society International (OARSI) Standing Committee for Clinical Trials Response Criteria Initiative and the Outcome Measures in Rheumatology (OMERACT), the OMERACT-OARSI criteria. Further details about methodological aspects of this study and statistical analyses can be found in the published manuscript [6].
Using data from the intention-to-treat (ITT) population of that trial, defined as all randomized patients who received the single injection, a response profile to Synolis VA® (n = 96 patients) was recently established [7]. Practically, the analyses demonstrated that a poorer physical function at baseline was associated with improvement in function at day 168, as well as with a better response to the treatment at the end of the study (day 168).
The Current Study
This study is a second post hoc analysis of the Synolis VA® arm of the original randomized, double-blind, non-inferiority trial. The analyses were based on the same data as for the previous responder profile analysis study, i.e., data of the ITT population of the original trial, considering the Synolis VA® arm only (n = 96 patients) [7]. Drawing on the findings of the previous responder analysis study, the current study was designed to answer two specific questions: (1) Do responders to Synolis VA® at day 28 remain responders at day 84, at day 168 or at both times, compared to non-responders at day 28? (2) Do patients with a more limited physical function at baseline have a higher chance of being responders at all time points (i.e., at D28, D84, and D168), compared to those with a less limited physical function at baseline?
We defined poorer (or more limited) versus better (or less limited) physical function according to a WOMAC function cut-off of 35, based on findings from a recent publication by MacKay et al. [8]. This was a systematic review of estimates of the minimal clinically important difference (MCID) and patient acceptable symptom state (PASS) of the WOMAC index, in patients who underwent total hip and total knee replacement (TKR). In fact, this systematic review found that PASS cut-offs for TKR ranged from 32.3 to 36.7 for WOMAC function. We therefore considered the mean of these two values, i.e., a WOMAC function score of 35, as the cut-off point in the present analysis. We also planned to use a second cut-off value, defined relative to the value corresponding to the 10th percentile of the baseline WOMAC function (value = 18.76), as in our previous study [7]. We wanted to compare the results obtained using these two different cut-off values.
Statistical Analysis
The STATA software (version 14.2, StataCorp LLC. College Station, TX, USA) was used to perform all statistical analyses. Bivariate and multivariate logistic regression models were fitted to assess the relationship between treatment response status (yes/no) at D28 (‘exposure’) and the response at D84 or D168, or at both time points (yes/no; ‘outcomes’). For multivariate models, the analyses were adjusted on the relevant variables considered in our previous responder profile analysis study, which was based on these same data, i.e., age, gender, BMI, and baseline WOMAC total score [7]. Bivariate and multivariate logistic regression models were also used to assess the association between baseline physical function status (‘exposure’) and treatment response at all time points (yes/no; ‘outcome’). Statistical significance was set at p < 0.05. Odds ratios (OR) with 95% confidence intervals (CI) were reported.
Results
The main baseline demographic and clinical characteristics of the ITT population of the trial have been reported in our previous article investigating the responder profile to the studied treatment [7]. The median age of the study population was 64.5 years (IQR 58.0–72.0), with the majority of patients being female (65.63%). Among the 96 patients of the ITT population, 59.38% were responders at day 28 according to the OMERACT/OARSI responder criteria. At days 84 and 168 respectively, 59.78 and 64.52% of the ITT population were responders to the treatment (on a total of 92 and 93 with data available, respectively).
Association Between Treatment Response at D28 and the Responses at Other Time Points
We sought to assess whether patients who were responders to the treatment at day 28 (D28) have a higher probability to remain responders at day 84 (D84), at day 168 (D168), and at both time-points (D84 and D168), compared to those who were not responders at D28, even when taking into account possible confounding factors. Our analyses showed that the odds of being a responder at D84 and D168, and at both time-points, in responders at D28, were significantly higher than these odds in non-responders at D28 (Table 1). These associations remain statistically significant, even after adjustment for possible confounding factors (Table 1).
A total of 39 patients were non-responders at D28. Among 35 of these patients, 40% (14 patients) became responders at D84 (of a total of 92 patients with full data at both time points). At D168, 37.84% of 37 patients who were non-responders at D28 became responders (93 patients with full data at both time points). Finally, for 34 patients who were non-responders at D28, only 29.41% (ten patients) were responders both at D84 and D168 (total, 90 patients). At the opposite, 67.86% of patients who were responders at D28 were also responders, both at D84 and D168 (p = 0.000).
Association Between Baseline Physical Function Status and Treatment Response Over the Duration of the Trial
We sought to investigate whether being a responder to the treatment at all time points (i.e., at D28, D84, and D168) could also be explained by the baseline physical function status (poorer vs. better physical function). Table 2 shows the results of the analyses considering a cut-off value for WOMAC function of 35. Using this cut-off value, our analyses showed that patients with a poorer physical function at baseline were more likely to respond to the treatment at all time points, compared to those with a better physical function (Table 2). We also sought to conduct the same analysis, this time, considering the cut-off value defined relatively to the value corresponding to the 10th percentile for baseline WOMAC function (value = 18.76), as in the previous study [7]. Unfortunately, there were insufficient data for this analysis (one null value in the two-by-two table).
Discussion
In our study, we observed that an early response to a single injection of sodium hyaluronate plus sorbitol is predictive of the long-term response and that patients with a poorer physical function may benefit most from the treatment.
Predicting long-term improvement based on an early improvement has rarely been investigated, and to the best of our knowledge, never with hyaluronic acid injection. There are little data available for other treatments: studies generally look at whether the early response at the group level is maintained over time, but do not take into account changes at the individual level. However, the natural history of OA has been shown to vary from patient to patient. For example, a recent systematic review including 7747 patients with knee OA highlighted that in the mid-term, the mean proportion of patients with a trajectory of increasing or decreasing pain was 6.7 and 7.9%, respectively [5]. Interestingly, in the short term (i.e., 1 month), an unstable pain trajectory (pain peaks for more than 50% of the month) was observed in 40.5% of the patients [5].
Regarding the prediction of the response to the treatment, this study confirms our previous study showing that a poorer physical function at baseline was associated with a better response to IAHA [7]. These results add to other evidence suggesting that IAHA should not be used too early in the development of OA or may be when other treatment options have failed. Indeed, it seems that a slightly more advanced form of OA should best benefit from IAHA.
From a practical point of view (i.e., for the clinician), all of these results highlight that we can be confident in the long term (up to 6 months) if a patient responds within 1 month to a single injection of sodium hyaluronate plus sorbitol. For patients who do not respond in the short term, the likelihood of a 6-month response is limited and other treatment options can be considered.
There are strengths and limitations to this study. We used data from a randomized controlled trial but we are limited by the duration of the trial and the number of pain/function were assessed during the study. More frequent assessment would have provided a better understanding of the natural history of OA after IAHA. It should also be pointed out that some concomitant medications for pain relief were allowed during the trial and they were not taken into account in this study. However, they were kept to a minimum with, consequently, a probable minimal impact on our results. On the other hand, this is probably what would happen in the real life of a patient after receiving IAHA. Also, it is important to acknowledge the limitation of our small sample size that may have impacted the statistical power of our analysis and should be taken into consideration when interpreting the results. Future studies with larger sample sizes are warranted to validate our findings and enhance the generalizability of the results. Finally, our results can only be carefully extrapolated to other HA products since it has been shown that HA efficacy varies widely across preparations [9].
Conclusions
In conclusion, our results confirm the place of IAHA in the management of OA, preferably in patients with altered physical function. Our results also highlight that the high response rate to a single injection of sodium hyaluronate plus sorbitol is maintained over time. More importantly, the likelihood of an individual patient responding over a 6-month period is predicted by their short-term response. Our results could have a major impact on management strategies for OA, but more data from other studies with other treatments are needed before the results of this study can be incorporated into various guidelines.
References
Arden NK, et al. Non-surgical management of knee osteoarthritis: comparison of ESCEO and OARSI 2019 guidelines. Nat Rev Rheumatol. 2021;17(1):59–66.
Migliore A, et al. Systematic literature review and expert opinion for the use of viscosupplementation with hyaluronic acid in different localizations of osteoarthritis. Orthop Res Rev. 2021;13:255–73.
Altman RD, et al. Missing the mark? American College of Rheumatology 2019 guidelines for intraarticular hyaluronic acid injection and osteoarthritis knee pain. J Rheumatol. 2022;49(8):958–60.
Bruyère O, et al. Inappropriate claims from non-equivalent medications in osteoarthritis: a position paper endorsed by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Aging Clin Exp Res. 2018;30(2):111–7.
Previtali D, et al. Pain trajectories in knee osteoarthritis—a systematic review and best evidence synthesis on pain predictors. J Clin Med. 2020;9(9):2828.
Cortet B, et al. Non-inferiority of a single injection of sodium hyaluronate plus sorbitol to Hylan G-F20: a 6-month randomized controlled trial. Adv Ther. 2021;38(5):2271–83.
Bruyère O, et al. Assessment of the response profile to hyaluronic acid plus sorbitol injection in patients with knee osteoarthritis: post-hoc analysis of a 6-month randomized controlled trial. Biomolecules. 2021;11(10):1498.
MacKay C, et al. A systematic review of estimates of the minimal clinically important difference and patient acceptable symptom state of the Western Ontario and McMaster Universities Osteoarthritis Index in patients who underwent total hip and total knee replacement. Osteoarthr Cartil. 2019;27(10):1408–19.
Webner D, Huang Y, Hummer CD 3rd. Intraarticular hyaluronic acid preparations for knee osteoarthritis: are some better than others? Cartilage. 2021;13(1_suppl):1619s–36s.
Acknowledgements
Funding
This study was funded by Aptissen, no funding was received for publication of this article.
Author Contributions
Conceptualization: Olivier Bruyère, Germain Honvo, and Bernard Cortet; Data curation: Olivier Bruyère and Germain Honvo; Formal analysis: Olivier Bruyère, Germain Honvo, and Eduard Vidovic; Funding acquisition: Eduard Vidovic; Methodology: Germain Honvo, Eduard Vidovic, and Bernard Cortet; Resources: Germain Honvo and Bernard Cortet; Supervision: Olivier Bruyère; Validation: Olivier Bruyère; Writing: original draft, Olivier Bruyère and Bernard Cortet; Writing: review and editing, Olivier Bruyère, Germain Honvo, Eduard Vidovic, and Bernard Cortet.
Disclosures
Olivier Bruyère and Bernard Cortet have received fees as members of the advisory board of Aptissen. Eduard Vidovic is an employee of Aptissen. Germain Honvo has nothing to declare.
Compliance with Ethics Guidelines
The trial was conducted in accordance with the ethics principles of the Declaration of Helsinki. It was approved and registered under no. 2017-A00034-49 to the ANSM, and ethical approval was obtained from CPP Ile-de-France VI. Ref: CPP/6-17-ID RCB: 2017-A00034-49.
Data Availability
The datasets generated and analyzed during the current study are stored at the Aptissen site, Plan-les-Ouates, Switzerland, and can be made available upon reasonable request to the corresponding author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bruyere, O., Honvo, G., Vidovic, E. et al. Is the Rate of Responders to Hyaluronic Acid Injection for Patients with Knee Osteoarthritis Stable Over Time? Post hoc Analyses of a 6-Month Follow-Up Study. Rheumatol Ther 10, 1297–1303 (2023). https://doi.org/10.1007/s40744-023-00573-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-023-00573-x