Abstract
Introduction
Serious infections are an important concern for patients with autoimmune conditions. We sought to estimate serious infection rates among patients with select autoimmune conditions relative to the general population in Taiwan and the USA.
Methods
This retrospective cohort study estimated setting-specific standardized serious infection incidence rates and ratios among patients with systemic lupus erythematosus, including extra-renal lupus and lupus nephritis, rheumatoid arthritis and primary membranous nephropathy, compared with the general population using insurance claims for hospitalizations between 2000 and 2013. Multivariable Cox proportional hazard models were used to estimate adjusted hazard ratios for serious infections, adjusting for age, sex, index year, prior serious infection, comorbidities and medications.
Results
In Taiwan, serious infection rates were 22.7, 28.7, 70.6, 43.4 and 215.3 per 1000 person-years among the general population and among cohorts of patients with primary membranous nephropathy, rheumatoid arthritis, extra-renal lupus and lupus nephritis, respectively. In the USA, serious infection rates were 2.6, 9.0, 15.6, 21.0 and 63.3 per 1000 person-years among the general population and among cohorts of patients with primary membranous nephropathy, rheumatoid arthritis, extra-renal lupus and lupus nephritis, respectively. Patients had significantly higher serious infection rates than the general population in both settings, largely driven by bacterial, respiratory, urinary tract and opportunistic infections. Patients with lupus nephritis had the highest burden of serious infections relative to the general population, with 7- to 25-fold higher adjusted hazard ratios in Taiwan and the USA, respectively.
Conclusion
This study identified a significant excess serious infection burden among patients with targeted autoimmune conditions compared with the general populations in Taiwan and the USA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Understanding serious infection rates among patients with autoimmune conditions who are receiving standard-of-care therapy in different settings is important for the development and introduction of new immune-targeted therapeutics, as well as for decisions related to disease management. |
This study aimed to estimate serious infection rates among patients with select autoimmune conditions relative to the general population in settings from 2 different regions that had similar data sources and disease classification methods |
What was learned from this study? |
Serious infection rates are significantly higher among autoimmune patients relative to the general population both in Taiwan and the USA. |
Among the targeted autoimmune conditions, patients with lupus nephritis have particularly high rates of serious infections. |
These findings provide evidence that can facilitate treatment decisions for patients and aid in the development and introduction of new immune-targeted therapeutics |
Introduction
Serious infections are an important concern for patients with autoimmune conditions. This is because of the effects of alterations in immune function due to the disease itself, which can lead to impaired cellular and humoral immune function, as well as the effect of immunosuppressive therapies (e.g. high-dose steroids and cyclophosphamide) used to control disease activity [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15]. Opportunistic infections, reactivation of latent infections and more severe manifestation of common infections are frequently reported among patients with autoimmune conditions and are leading causes of morbidity and mortality among patients with conditions such as systemic lupus erythematosus (SLE) or rheumatoid arthritis (RA), as well as autoimmune conditions that lead to renal manifestations such as lupus nephritis and primary membranous nephropathy [13, 16,17,18,19,20,21,22,23,24,25,26,27]. Furthermore, impaired renal function can lead to immune dysfunction and may be an independent risk factor for serious infections [28].
Understanding serious infection rates among patients with autoimmune conditions who are receiving standard-of-care therapy in different settings is important for the development and introduction of new immune-targeted therapeutics, as well as for decisions related to disease management. Existing and novel B-cell depletion or modulation therapies targeting CD20, CD19, Bruton’s tyrosine kinase inhibitors and/or B-cell activating factor are increasingly being used in patients with autoimmune conditions [29, 30]. Because global clinical trials are common for new therapeutic treatment efforts, characterizing regional variability in serious infection rates among patients with autoimmune conditions can provide valuable insights into the influence of patient-level characteristics, healthcare system(s) and treatment approaches in routine clinical practice [31].
In this study, we identified a select group of autoimmune conditions targeted by B-cell depletion therapies to estimate the incidence of serious infections, namely SLE, RA and primary membranous nephropathy, compared with the general population in both Taiwan and the USA.
Methods
Study Design and Source Populations
In this retrospective cohort study, we used data from the National Health Insurance Research Database (NHIRD) in Taiwan (the One Million General Sample Database [OMGSD] and the Catastrophic Illness Database [CID]) and the U.S.-based Truven Healthcare MarketScan® Commercial Claims (CC) and Encounters, as well as the Supplemental Medicare databases from 1 January 2000 to 30 December 2013. The NHIRD includes medical insurance claims data from an estimated 99.99% of Taiwan’s population (approximately 23 million) as part of a single-payer mandatory National Insurance Program that includes patients’ records from birth until death [32]. In Taiwan, patients identified via the NHIRD OMGSD were randomly sampled from the NHIRD in 2000 and provided follow-up time through 2013. The CID includes healthcare records for patients with a catastrophic illness certification for select conditions that entitles them to financial subsidies to cover out-of-pocket medical costs. The U.S.-based MarketScan CC database contains up to 109 million commercially insured individuals aged < 65 years who receive employer-sponsored health insurance and 8 million Medicare commercially insured patients aged ≥ 65 years, annually. U.S. patients provided follow-up time while enrolled in health insurance plans that contributed to MarketScan CC and Medicare between 2000 and 2013. Data from both Taiwan and the USA included de-identified patient-level demographic, medical and pharmacy data collected and reported for the purpose of insurance claims.
Study Population
The study population included person-time for patients of all ages who had continuous enrollment for ≥ 90 days pre-index and ≥ 365 days post-index between 1 January 2000 and 31 December 2013. Patients were excluded if they had cancer, solid-organ or bone marrow transplant and/or HIV/AIDS (Electronic Supplementary Material [ESM] Table S1).
We constructed mutually exclusive patient cohorts to identify patients with SLE (extra-renal lupus and lupus nephritis), RA and primary membranous nephropathy, as well as to identify the general population within the NHIRD OMGSD from Taiwan and the U.S.-based MarketScan CC and Medicare databases. The diagnostic algorithms used to identify patient cohorts are described in the following sections. Index dates were assigned for SLE (extra-renal lupus and lupus nephritis separately), RA and primary membranous nephropathy cohorts based on the initial claim satisfying the specified criteria. The index date for the general population was considered to be the first day after 90 days of continuous enrollment within the study period. We further characterized patients from Taiwan with SLE and RA identified in the OMGSD according to their presence in the CID during the same period.
SLE: Extra-Renal Lupus and Lupus Nephritis
Patients with SLE were identified if they had ≥ 1 inpatient or ≥ 2 outpatient claims with an International Classification of Diseases, Ninth Revision (ICD-9; https://apps.who.int/iris/handle/10665/39473) diagnostic code of 710.0 separated by ≥ 7 days and ≤ 365 days. Patients with SLE were further classified as having lupus nephritis if they had ≥ 1 inpatient or ≥ 2 outpatient claims with the ICD-9 diagnostic codes 580–586 and a lupus nephritis index date within ± 365 days of the SLE index date. Patients with extra-renal lupus were considered those individuals who did not have evidence of lupus nephritis within the 365-day post-index period.
Rheumatoid Arthritis
Patients with RA were identified if they had ≥ 1 inpatient or ≥ 2 outpatient claims with ICD-9 diagnostic code of 714.0 separated by ≥ 7 days and ≤ 365 days.
Primary Membranous Nephropathy
Patients with primary membranous nephropathy were identified if they had ≥ 1 inpatient or ≥ 2 outpatient claims with an ICD-9 diagnostic code of 581.1 or 582.1 separated by ≥ 7 days and ≤ 365 days and did not have any evidence of a secondary cause of membranous nephropathy (ESM Table S2).
General Population
Individuals who satisfied the inclusion and exclusion criteria and did not fulfill the criteria for the SLE, RA or primary membranous nephropathy cohorts were included in the general population cohort.
Ethics Compliance
The protocol for this study is in line with the 2008 Declaration of Helsinki and its subsequent amendments. The authors conducted secondary research using de-identified U.S. data licensed from IBM® Watson® question-answering computer system in compliance with U.S. Code of Federal Regulations Title 45 (45 CFR) Section 164.514(a–c) and the National Health Insurance Program in Taiwan. The data from both the USA and Taiwan had identifying information removed and were coded in such a way that the data could not be linked back to subjects from whom it was originally collected.
This research does not require Institutional Review Board or ethics review, as analyses with these data do not meet the definition of “research involving human subjects,” defined as living individuals about whom an investigator obtains identifiable private information for research purposes. Furthermore, use of claims data from Taiwan included in this research was approved by the Taichung Veterans General Hospital Institutional Review Board I and II (CE13152B-8). Neither the provider of the data nor the researchers were able to link the data with identifiable individuals. Consent to participate was not applicable in this retrospective observational study of de-identified data.
Outcomes
Incident serious infections were identified based on hospitalization that included an ICD-9 diagnostic code(s) pertaining to infections occurring as the primary (most important) diagnosis. Initial infections were identified that occurred ≤ 365 days post-index date for all patient cohorts. We categorized serious infections as a composite set of infections, as well as according to infection subtype [16] (ESM Table S3).
Cofactors
The following cofactors were assessed for each patient: age, sex, index year, pre-existing serious infection, comorbid condition(s), and systemic steroid (considered as those that were administered orally, intravenously or intramuscularly) and immunosuppressant use (ESM Table S4). We captured patient age and sex based on data contained in the enrollment files. Pre-existing serious infections were considered as hospitalizations due to serious infections identified during the 90-day pre-index period. We classified patients according to the presence of concurrent autoimmune conditions (other than SLE, RA and primary membranous nephropathy) (ESM Table S5) and individual comorbid conditions that contribute to the Charlson Comorbidity Index (with the exception of those targeted by the inclusion/exclusion study criteria) identified via diagnostic claims at any time during the study period (e.g. pre-index through to 365 days post-index) [33]. We captured claims for systemic corticosteroids and immunosuppressants as a dichotomous (yes/no) variable and the date when administered and/or filled post-index until either the occurrence of a serious infection or 365 days post-index.
Statistical Analyses
Incidence rates and ratios were calculated for initial serious infections and 95% confidence intervals (CIs) using both direct and indirect standardization based on the general population for Taiwan as well as the USA to provide straightforward rate estimations and also account for the influence of small numbers in some strata [34, 35]. Standardization was based on age, sex, index year, pre-existing serious infection and systemic steroid and immunosuppressant use. Standardized incidence ratios compared serious infection rates among patients with a specified autoimmune condition to the within-setting general population. Cox proportional hazard models were used to estimate serious infection hazard rates, adjusting for index year, age, sex, prior serious infection, co-existing comorbidities and post-index receipt of corticosteroids or immunosuppressant(s). For these models, we used 1–10 matching for all cohorts on age, sex and index year to account for potential differences in data structure between Taiwan and the USA.
Additional Analyses
In Taiwan, patients with major rheumatologic conditions, such as SLE and RA, are provided with a catastrophic illness certification that entitles them to financial subsidies to cover out-of-pocket medical costs. Patients with this certification have their healthcare records captured in the CID. The CID has greater specificity than the OMGSD due to rigorous review of patients’ diagnoses by rheumatologists commissioned by the Bureau of National Health Insurance. However, the CID is less generalizable to patients identified via diagnostic algorithms (e.g. as identified in the OMGSD for Taiwan and in the U.S.-based claims data) because patients with a catastrophic illness certificate may differ with respect to disease severity or duration and/or access to healthcare and medications. Furthermore, there is no comparable system in the USA. Thus, for patients from Taiwan only, we used the CID to compare the characteristics and serious infection rates of patients with SLE and RA who were identified via diagnostic claims algorithms in the OMGSD with those of patients who were identified via diagnostic claims and were also present in the CID.
Results
Study Population
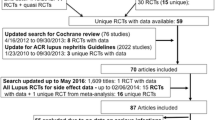
Figure 1 (Taiwan) and Fig. 2 (USA) provide the study population attrition for the inclusion and exclusion criteria for each cohort. The cohort-specific population size for Taiwan was RA = 8606, lupus nephritis = 325, extra-renal lupus = 1149, primary membranous nephropathy = 127 and general population = 912,302. The cohort-specific population size for the USA was RA = 154,255, lupus nephritis = 3725, extra-renal lupus = 41,904, primary membranous nephropathy = 3377 and general population = 640,412.
Patient cohorts in study population of Taiwan. AI autoimmune, ERL extra-renal lupus, HIV/AIDS human immunodeficiency virus/acquired immunodeficiency syndrome, ICD-9 International Classification of Diseases, Ninth Revision, ipt inpatient, LN lupus nephritis, NHIRD National Health Insurance Research Database, opt outpatient, pMN primary membranous nephropathy, RA rheumatoid arthritis, SLE systemic lupus erythematosus
Patient cohorts in study population of USA. Note that the general population cohort in the USA is based on a 1% random sample of IBM® MarketScan® Commercial Claims and Encounters Database. CCAE IBM® MarketScan® Commercial Claims and Encounters Database, MDCR MarketScan Medicare Supplemental and Coordination of Benefits Database, MN membranous nephropathy; for other abbreviations, see Fig. 1 caption
Table 1 shows the distribution of patient characteristics for each cohort based on the claims data from both settings. The general population cohorts in Taiwan and the USA were similar with respect to age (mean 33 years), concurrent autoimmune conditions (approx. 3% had autoimmune conditions other than extra-renal lupus, lupus nephritis, RA or primary membranous nephropathy) and medication use (systemic steroids and immunosuppressants). Comorbidities, such as cerebrovascular, chronic pulmonary and liver or peptic ulcer disease, were more common among patients from Taiwan relative to those from the USA. We identified modest differences between post-index claims for systemic steroids and immunosuppressants in Taiwan and the USA. RA patients from Taiwan had fewer systemic steroid and immunosuppressant claims than U.S. patients, whereas patients with lupus nephritis from Taiwan were more commonly treated with cytostatic and antiproliferative medications. Use of biologics was infrequent except among U.S. patients with RA due to lack of approval and reimbursement for target indications during the study period.
Serious Infections
Table 2 describes the standardized serious infection rates and distribution of serious infections by patient cohort for Taiwan and the USA. Among the patient cohorts assessed, patients with lupus nephritis experienced the highest frequency of serious infections regardless of setting. Overall, serious infections were largely driven by bacterial, respiratory, urinary tract and opportunistic infections among patient cohorts other than the general population in both settings. In Taiwan, pediatric patients with lupus nephritis, extra-renal lupus and RA experienced a slightly higher proportion of serious infections than their adult counterparts, which was not observed in the USA (ESM Fig. S1).
Among patients who had a serious infection ≤ 365 days post-index, the average time to the event was longer among patients from Taiwan with SLE, RA and primary membranous nephropathy than among U.S. patients with the same condition and longer in the general populations of both settings compared with the autoimmune cohorts (ESM Table S6).
Comparisons of serious infection rate to that of the general population for each setting and patient cohort are shown in Fig. 3. We identified the highest serious infection rates among patients with lupus nephritis in both settings and the lowest serious infection rates among patients with RA. Due to low serious infection rates in the U.S. general population, estimated serious infection rates in the USA were elevated for all patient cohorts.
Within-setting comparisons of serious infection rates for autoimmune patients versus the general population. Adjusted SIRs and 95% CIs of serious infection rates for autoimmune patients (extra-renal lupus, lupus nephritis, RA and pMN) were compared with the general population by setting. CI Confidence interval, SI serious infection, SIR standardized incidence ratio
Adjusted multivariable model results accounting for age, gender, index year, medications and comorbidities identified significantly heightened rates of serious infections among patients with autoimmune conditions relative to the general population in both Taiwan and the USA. Consistent with the descriptive findings, the highest adjusted hazard ratios (aHRs) were identified among patients with lupus nephritis (Taiwan: aHR 7.4, 95% CI 4.5–12.4; USA: aHR 24.9, 95% CI 19.8–31.3), followed by patients with primary membranous nephropathy (Taiwan: aHR 3.3, 95% CI 1.4–7.8; USA: aHR 10.4, 95% CI 8.1–13.4), extra-renal lupus (Taiwan: aHR 2.4, 95% CI 1.4–4.0; USA: aHR 6.3, 95% CI 5.5–7.2) and RA (Taiwan: aHR 1.3, 95% CI 1.0–1.8; USA: aHR 5.5, 95% CI 4.8–6.3). Assessment of the interactive effects of autoimmune condition and medications consistently identified heightened aHRs for serious infection among patients who had a post-index claim for systemic steroids compared to those who did not within the same patient group (e.g. Taiwan: extra-renal lupus, aHR 1.9, 95% CI 1.1–3.2; lupus nephritis, aHR 1.4, 95% CI 0.8–2.7; RA, aHR 1.3, 95% CI 1.0–1.6; primary membranous nephropathy, aHR 2.3, 95% CI 0.8–6.5; USA: extra-renal lupus, aHR 1.4, 95% CI 1.2–1.6; lupus nephritis, aHR 1.2, 95% CI 0.9–1.5; RA, aHR 1.1, 95% CI 0.9–1.2; primary membranous nephropathy, aHR 1.6, 95% CI 1.1–2.3). The influence of immunosuppressants on aHR of serious infection was mixed across autoimmune cohorts and not consistent between settings (e.g. Taiwan: extra-renal lupus, aHR 1.0, 95% CI 0.4–2.3; lupus nephritis, aHR 1.99, 95% CI 0.9–4.2; RA, aHR 1.1, 95% CI 0.6–2.1; primary membranous nephropathy, aHR 0.7, 95% CI 0.2–2.1; USA: extra-renal lupus, aHR 0.7, 95% CI 0.5–0.9; lupus nephritis, aHR 0.6, 95% CI 0.5–0.9; RA, aHR 0.5, 95% CI 0.4–0.6; primary membranous nephropathy, aHR 0.7, 95% CI 0.4–1.1). We also identified significantly increased aHRs for serious infections among patients with comorbid conditions and among those who received post-index systemic steroids and/or immunosuppressants (ESM Fig. S2).
Comparison of Patients with SLE and RA Identified via the One Million General Sample Database and the Catastrophic Illness Database in Taiwan
Among patients with SLE and RA identified via diagnostic algorithms within the OMGSD, we identified 27% (403/1474) of the SLE patients and 10.5% (904/8606) of the RA patients who were also captured in the CID (403/1474) based on unique patient-level identifiers. Among patients with certified catastrophic illness, there were a higher proportion of pediatric cases, more concurrent autoimmune conditions and more patients with a claim for post-index systemic steroids and/or immunosuppressants compared with patients identified via the study-derived algorithm in the OMGSD. ESM Table s7 provides a detailed description of the patients with SLE and RA identified in Taiwan via the OMGSD only compared with those patients who also received certification of their condition and were present in the CID. The estimated standardized incidence ratios (SIRs) for patients with SLE and RA observed in the CID were slightly higher, but not significantly higher, than those derived from the patients identified in the OMGSD (Fig. 4).
Estimated SIRs of patients from Taiwan with SLE and RA in the OMGSD and CID. Adjusted SIRs and 95% CIs of serious infection rates for patients with SLE and RA compared with the general population by database (OMGSD and CID) in Taiwan. CID Catastrophic Illness Database, OMGSD One Million General Sample Database
Discussion
Findings from this large multinational retrospective claims-based cohort study confirm the important role of infections among patients with autoimmune conditions. We identified significant excess rates of serious infection among patients with SLE (particularly among those with lupus nephritis), RA and primary membranous nephropathy compared with the general population in both Taiwan and the USA, driven largely by bacterial, respiratory, urinary tract and opportunistic infections, which is consistent with prior findings [7, 36,37,38,39,40,41,42,43,44].
We strove to use a standard methodological approach and similar real-world data systems across cohorts from both Taiwan and the USA. The OMGSD and the MarketScan CC and Medicare Supplemental databases are insurance claims systems that use the same diagnostic classification system (ICD-9) to enhance similarity between the setting-specific findings. We further assessed our findings based on identification of patients with a diagnostic algorithm compared with identification of patients with a catastrophic illness certified by rheumatologists in Taiwan. Although we identified heightened rates of serious infections among patients with SLE and RA compared with the general population in Taiwan, regardless of whether or not patients had received a catastrophic illness certification, we did observe higher post-index systemic steroid and immunosuppressant use among patients in the CID (particularly among RA patients), which did not result in significant differences in the estimated serious infection rates. This suggests that such patients may have more severe disease and/or have greater access to medications because of lower out-of-pocket costs.
Although we standardized our approach and chose the respective data systems to maximize similarities, there remained inherent differences between the Taiwan and U.S. populations and healthcare systems that are important to consider and which limit direct comparisons of our findings, such as differences in underlying sociodemographic factors, disease endemicity and potential differences in coding conventions and healthcare systems. Whereas the age and gender distribution of the identified general population cohort was comparable between Taiwan and the USA, there were important differences in the distribution of underlying comorbidities (particularly cerebrovascular, chronic pulmonary, liver and peptic ulcer disease). There are also notable differences in the endemicity of specific infectious diseases between Taiwan and the USA (e.g. hepatitis, tuberculosis, opportunistic infections) that may have influenced our findings [45, 46]. Longitudinal follow-up of patient records is more comprehensive in Taiwan than in the USA because Taiwan has a single-payer system that follows patients from birth to death (closed system), whereas insurance claims for U.S. patients may be incomplete due to a multi-payer system that results in potential enrollment changes over time due to changes in healthcare insurance coverage (dynamic system). The differential follow-up between the claims data from the two settings may have led to index dates that are earlier in the course of disease for autoimmune conditions among patients from Taiwan relative to U.S. patients. Greater subsidization of healthcare costs in Taiwan may have influenced patient behavior and subsequent capture of illness and/or medication in the patient records. In fact, in our study, patients from Taiwan had an average of 12 doctor visits per patient per year compared with four visits per year among U.S. patients. Such differences in healthcare-seeking behavior, as well as differences in medication approval and coverage, in particular the limited use of biologics in Taiwan, may have influenced our findings [47]. Furthermore, even though we used standard algorithms to identify patients and infections, it is possible that coding practices differed slightly between the two settings.
This study provides a unique assessment of SIRs among patients with autoimmune conditions receiving standard-of-care treatments in routine clinical practice based on insurance claims data from different geographical regions. We provide estimated SIRs overall and by infection subtype, accounting for the potential influence of important demographic and clinical factors in a study period spanning over a decade. We provide a novel assessment of SIRs compared with the general population in Taiwan based on the OMGSD and the CID databases that resulted in comparable estimates for patients with SLE and RA and provide an indirect assessment of the accuracy of our findings using an algorithm based on diagnostic coding. Overall, we observed heightened aHRs for serious infections among patients who received systemic steroids and immunosuppressants; however, the influence of these medications across type of autoimmune patient and setting was variable (ESM Fig. S2). Specifically, systemic steroid use in the first year post-index results in heightened aHRs of serious infection, while we did not identify similar findings among patients who received immunosuppressants in the first year post-index. While estimated aHRs for serious infections among autoimmune patients who received immunosuppressants were variable and fairly imprecise, the findings may have resulted from our assessment of serious infections in the first year post-index and may reflect an individual patient’s condition, routing treatments in the early stages of a patient’s disease, variable treatment practices across settings and patient groups, as well as variable accuracy of index date between systems as a result of variable follow-up of patients’ healthcare records. Further, these discrepant findings may have resulted from different prescribing patterns based on dosage, patient population and disease severity and/or duration, which were not captured in our study and may have differed between the two settings. Additional limitations of our study include the relatively small size of the study population from Taiwan, which limited the number of patients identified with rare conditions, such as primary membranous nephropathy, as well as the inability to identify serious infections that result in death due to the lack of available mortality data within claims databases. The use of algorithms based on diagnostic and procedural codes within insurance claims data may have limited our ability to identify and classify patient health status, as well as to ascertain potentially important intrinsic and extrinsic factors that were not captured in this type of real-world data [48,49,50].
Conclusions
In conclusion, this unique large real-world data study provides estimates of SIRs for patients with SLE, RA and primary membranous nephropathy receiving standard-of-care treatment and confirms significantly heightened serious infection rates among such patients compared with the general population in both Taiwan and the USA. These findings provide evidence that can facilitate treatment decisions for patients and aid in the development and introduction of new immune-targeted therapeutics.
References
George MD, Baker JF, Winthrop K, et al. Risk for serious infection with low-dose glucocorticoids in patients with rheumatoid arthritis: a cohort study. Ann Intern Med. 2020;173(11):870–8.
Jung JY, Yoon D, Choi Y, Kim HA, Suh CH. Associated clinical factors for serious infections in patients with systemic lupus erythematosus. Sci Rep. 2019;9(1):9704.
Singh JA, Cameron C, Noorbaloochi S, et al. Risk of serious infection in biological treatment of patients with rheumatoid arthritis: a systematic review and meta-analysis. Lancet. 2015;386(9990):258–65.
Singh JA, Hossain A, Kotb A, Wells G. Risk of serious infections with immunosuppressive drugs and glucocorticoids for lupus nephritis: a systematic review and network meta-analysis. BMC Med. 2016;14(1):137.
Sathish JG, Sethu S, Bielsky MC, et al. Challenges and approaches for the development of safer immunomodulatory biologics. Nat Rev Drug Discov. 2013;12(4):306–24.
Feldman CH, Hiraki LT, Winkelmayer WC, et al. Serious infections among adult Medicaid beneficiaries with systemic lupus erythematosus and lupus nephritis. Arthritis Rheumatol. 2015;67(6):1577–85.
Goldblatt F, Chambers S, Rahman A, Isenberg DA. Serious infections in British patients with systemic lupus erythematosus: hospitalisations and mortality. Lupus. 2009;18(8):682–9.
Atzeni F, Masala IF, di Franco M, Sarzi-Puttini P. Infections in rheumatoid arthritis. Curr Opin Rheumatol. 2017;29(4):323–30.
Pryor BD, Bologna SG, Kahl LE. Risk factors for serious infection during treatment with cyclophosphamide and high-dose corticosteroids for systemic lupus erythematosus. Arthritis Rheum. 1996;39(9):1475–82.
Falagas ME, Manta KG, Betsi GI, Pappas G. Infection-related morbidity and mortality in patients with connective tissue diseases: a systematic review. Clin Rheumatol. 2007;26(5):663–70.
Teh CL, Wan SA, Ling GR. Severe infections in systemic lupus erythematosus: disease pattern and predictors of infection-related mortality. Clin Rheumatol. 2018;37(8):2081–6.
Subesinghe S, Rutherford AI, Byng-Maddick R, Leanne Hyrich K, Benjamin GJ. Recurrent serious infections in patients with rheumatoid arthritis—results from the british society for rheumatology biologics register. Rheumatol (Oxford). 2018;57(4):651–5.
Au K, Reed G, Curtis JR, et al. High disease activity is associated with an increased risk of infection in patients with rheumatoid arthritis. Ann Rheum Dis. 2011;70(5):785–91.
Thong KM, Chan TM. Infectious complications in lupus nephritis treatment: a systematic review and meta-analysis. Lupus. 2019;28(3):334–46.
Zhang CX, Cai L, Zhou ZY, et al. Clinical manifestations, immunological features and prognosis of Chinese pediatric systemic lupus erythematosus: a single-center study. Int J Rheum Dis. 2019;22(6):1070–6.
Pawar A, Desai RJ, Solomon DH, et al. Risk of serious infections in tocilizumab versus other biologic drugs in patients with rheumatoid arthritis: a multidatabase cohort study. Ann Rheum Dis. 2019;78(4):456–64.
Nguyen-Khoa BA, Goehring EL Jr, Alexander KA, Dong W, Napalkov P, Jones JK. Risk of significant infection in rheumatoid arthritis patients switching anti-tumor necrosis factor-alpha drugs. Semin Arthritis Rheum. 2012;42(2):119–26.
Li YC, Huang J, Li X, Zhao SM. A comparison of cyclophosphamide versus tacrolimus in terms of treatment effect for idiopathic membranous nephropathy: A meta-analysis. Nefrologia. 2019;39(3):269–76.
Kim Y, Yoon HE, Chung BH, et al. Clinical outcomes and effects of treatment in older patients with idiopathic membranous nephropathy. Korean J Intern Med. 2019;34(5):1091–9.
Ocampo-Piraquive V, Nieto-Aristizábal I, Cañas CA, Tobón GJ. Mortality in systemic lupus erythematosus: causes, predictors and interventions. Expert Rev Clin Immunol. 2018;14(12):1043–53.
Kelly C, Hamilton J. What kills patients with rheumatoid arthritis? Rheumatology (Oxford). 2007;46(2):183–4.
Mehta B, Pedro S, Ozen G, et al. Serious infection risk in rheumatoid arthritis compared with non-inflammatory rheumatic and musculoskeletal diseases: a US national cohort study. RMD Open. 2019;5(1):e000935.
Listing J, Gerhold K, Zink A. The risk of infections associated with rheumatoid arthritis, with its comorbidity and treatment. Rheumatol (Oxford). 2013;52(1):53–61.
Kidney Disease Improving Global Outcomes. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;(3):1–150.
van den Brand JA, van Dijk PR, Hofstra JM, Wetzels JF. Long-term outcomes in idiopathic membranous nephropathy using a restrictive treatment strategy. J Am Soc Nephrol. 2014;25(1):150–8.
Tien YC, Yen HH, Chiu YM. Incidence and clinical characteristics of hepatitis B virus reactivation in HBsAg-negative/HBcAb-positive patients receiving rituximab for rheumatoid arthritis. Clin Exp Rheumatol. 2017;35(5):831–6.
Lin CT, Huang WN, Hsieh CW, et al. Safety and effectiveness of tocilizumab in treating patients with rheumatoid arthritis—a three-year study in Taiwan. J Microbiol Immunol Infect. 2019;52(1):141–50.
Kurts C, Panzer U, Anders HJ, Rees AJ. The immune system and kidney disease: basic concepts and clinical implications. Nat Rev Immunol. 2013;13(10):738–53.
Lee DSW, Rojas OL, Gommerman JL. B cell depletion therapies in autoimmune disease: advances and mechanistic insights. Nat Rev Drug Discov. 2021;20(3):179–99.
Shi Y, Wu Y, Ren Y, Jiang Y, Chen Y. Infection risks of rituximab versus non-rituximab treatment for rheumatoid arthritis: a systematic review and meta-analysis. Int J Rheum Dis. 2019;22(8):1361–70.
Keebler D, Teng E, Chia J, Galanter J, Peake J, Tuckwell K. Regional variations in adverse event reporting rates and ACR responses in placebo/standard-of-care arms of rheumatoid arthritis trials. Rheumatol (Oxford). 2020;59(10):3023–31.
Hsieh CY, Su CC, Shao SC, et al. Taiwan’s National Health Insurance Research Database: past and future. Clin Epidemiol. 2019;11:349–58.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Breslow NE, Day NE. Indirect standardization and multiplicative models for rates, with reference to the age adjustment of cancer incidence and relative frequency data. J Chronic Dis. 1975;28(5–6):289–303.
Bains N. Standardization of rates. Association of Public Health Epidemiologists in Ontario; Ontario, Canada; 2009. http://core.apheo.ca/resources/indicators/Standardization%20report_NamBains_FINALMarch16.pdf. Accessed 1 Nov, 2022.
Lim CC, Liu PY, Tan HZ, et al. Severe infections in patients with lupus nephritis treated with immunosuppressants: a retrospective cohort study. Nephrol (Carlton). 2017;22(6):478–84.
Battaglia M, Garrett-Sinha LA. Bacterial infections in lupus: roles in promoting immune activation and in pathogenesis of the disease. J Transl Autoimmun. 2021;4:100078.
Caporali R, Caprioli M, Bobbio-Pallavicini F, Montecucco C. DMARDS and infections in rheumatoid arthritis. Autoimmun Rev. 2008;8(2):139–43.
Pego-Reigosa JM, Nicholson L, Pooley N, et al. The risk of infections in adult patients with systemic lupus erythematosus: systematic review and meta-analysis. Rheumatol (Oxford). 2021;60(1):60–72.
Luijten RK, Cuppen BV, Bijlsma JW, Derksen RH. Serious infections in systemic lupus erythematosus with a focus on pneumococcal infections. Lupus. 2014;23(14):1512–6.
Tektonidou MG, Wang Z, Dasgupta A, Ward MM. Burden of serious infections in adults with systemic lupus erythematosus: a national population-based study, 1996–2011. Arthritis Care Res (Hoboken). 2015;67(8):1078–85.
Jinno S, Lu N, Jafarzadeh SR, Dubreuil M. Trends in hospitalizations for serious infections in patients with rheumatoid arthritis in the US between 1993 and 2013. Arthritis Care Res (Hoboken). 2018;70(4):652–8.
Herrinton LJ, Liu L, Goldfien R, Michaels MA, Tran TN. Risk of serious infection for patients with systemic lupus erythematosus starting glucocorticoids with or without antimalarials. J Rheumatol. 2016;43(8):1503–9.
Simard JF, Rossides M, Gunnarsson I, Svenungsson E, Arkema EV. Infection hospitalisation in systemic lupus in Sweden. Lupus Sci Med. 2021;8(1):e000510.
Ott JJ, Stevens GA, Groeger J, Wiersma ST. Global epidemiology of hepatitis B virus infection: new estimates of age-specific HBsAg seroprevalence and endemicity. Vaccine. 2012;30(12):2212–9.
Cohen A, Mathiasen VD, Schön T, Wejse C. The global prevalence of latent tuberculosis: a systematic review and meta-analysis. Eur Respir J. 2019;54(3):1900655.
Hsieh CR, Liu YM. Availability, health-care costs, and utilization patterns of biologics in Taiwan. Value Health. 2012;15(1 Suppl):S35-42.
Jakes RW, Bae SC, Louthrenoo W, Mok CC, Navarra SV, Kwon N. Systematic review of the epidemiology of systemic lupus erythematosus in the Asia-Pacific region: prevalence, incidence, clinical features, and mortality. Arthritis Care Res (Hoboken). 2012;64(2):159–68.
Danza A, Ruiz-Irastorza G. Infection risk in systemic lupus erythematosus patients: susceptibility factors and preventive strategies. Lupus. 2013;22(12):1286–94.
Wang Z, Wang Y, Zhu R, et al. Long-term survival and death causes of systemic lupus erythematosus in China: a systemic review of observational studies. Medicine (Baltimore). 2015;94(17):e794.
Acknowledgements
Funding
This work was funded by Genentech, Inc. a member of the Roche Group. The publication of this article along with the journal’s Rapid Service Fee was funded by Genentech, Inc.
Medical Writing, Editorial, and Other Assistance
Support for third-party medical writing/editorial assistance, furnished by Nicola Gillespie, DVM, of Health Interactions, Inc., was provided by Genentech, Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Lisa Lindsay, Ching-Yi Chuo and Wen-Nan Huang wrote the main manuscript text. Ching-Yi Chuo prepared the figures. Wei-Szu Lin and Ching-Yi Chuo conducted the statistical analyses. Lisa Lindsay, Ching-Yi Chuo, Wen-Nan Huang, Katie Tuckwell, Nicholas S. Jones, Joshua Galanter, Ching-Heng Lin and Yi-Ming Chen contributed to the study protocol and reviewed the manuscript.
Disclosures
Lisa Lindsay, Nicholas S. Jones and Joshua Galanter are employed by and hold shares in Genentech, Inc., a member of the Roche Group. Ching-Yi Chuo and Katie Tuckwell were employees and shareholders of Genentech, Inc. at the time the research was conducted. Ching-Yi Chuo’s current affiliation is Gilead Sciences. Katie Tuckwell’s current affiliation is Regeneron. Wen-Nan Huang, Ching-Heng Lin, Yi-Ming Chen and Wei-Szu Lin have nothing to disclose.
Compliance With Ethics Guidelines
The protocol for this study is in line with the 2008 Declaration of Helsinki and its subsequent amendments. The authors conducted secondary research using de-identified U.S. data licensed from IBM® Watson® question-answering computer system in compliance with U.S. Code of Federal Regulations Title 45 (45 CFR) Section 164.514(a–c) and the National Health Insurance Program in Taiwan. The data from both the USA and Taiwan had identifying information removed and were coded in such a way that the data could not be linked back to subjects from whom it was originally collected. This research does not require Institutional Review Board or ethics review, as analyses with these data do not meet the definition of “research involving human subjects,” defined as living individuals about whom an investigator obtains identifiable private information for research purposes. Furthermore, use of claims data from Taiwan included in this research was approved by the Taichung Veterans General Hospital Institutional Review Board I and II (CE13152B-8). Neither the provider of the data nor the researchers were able to link the data with identifiable individuals. Consent to participate was not applicable in this retrospective observational study of de-identified data.
Data Availability
The datasets analyzed during the current study are not publicly available due to restrictions that apply to the availability of these data available from Merative (previously IBM® Watson®) and the National Health Insurance Program in Taiwan.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Huang, WN., Chuo, CY., Lin, CH. et al. Serious Infection Rates Among Patients with Select Autoimmune Conditions: A Claims-Based Retrospective Cohort Study from Taiwan and the USA. Rheumatol Ther 10, 387–404 (2023). https://doi.org/10.1007/s40744-022-00525-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-022-00525-x