Abstract
Introduction
The proportion of women being treated with biologics is growing. However, data on treatment recommendation awareness among treating physicians and women who are considering pregnancy and family planning are limited. In this study, we used a questionnaire survey to learn how rheumatologists and dermatologists address women’s needs for family planning, pregnancy, and breastfeeding, as well as their possible concerns with concurrent inflammatory rheumatic disease or psoriasis.
Methods
A 55-question (in English) survey aimed at identifying surveyed physicians' current practices regarding the reproductive health needs of women with rheumatoid arthritis, psoriasis, or psoriatic arthritis. This survey included 82 rheumatologists and 38 dermatologists from the Czech Republic, Hungary, and Slovakia.
Results
The proportion of female patients of reproductive age with the moderate-to-severe disease was 10–30% of all patients treated by the respondents. At the time of diagnosis, approximately two-thirds of the respondents discussed family planning with their patients. Rheumatologists collaborated with other specialists more frequently than dermatologists and gynecologist–obstetricians. Half of the rheumatologists revised systemic treatment 6 months before the patient planned to become pregnant, whereas dermatologists appear to act much sooner. Rheumatologists chose systemic glucocorticoids as the first-line treatment for pregnancy flares, whereas dermatologists chose topical corticosteroids. Congresses and interdisciplinary forums were rated the most valuable sources of information by physicians.
Conclusions
There is a need for more holistic, multidisciplinary, collaborative, and integrated communication between clinicians and women of childbearing age. Physicians should consider the implications of these conditions and medical treatment for women of childbearing age and family planning for those with rheumatoid arthritis and psoriatic disease. Patient-centered care that includes patients’ reproductive choices should be a routine clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Family planning represents a complex challenge to clinicians treating women with chronic inflammatory disease. |
This was a questionnaire survey to understand how rheumatologists and dermatologists address women's needs for family planning, pregnancy, and breastfeeding, as well as their potential concerns with concurrent inflammatory rheumatic disease or psoriasis. |
What was learned from the study? |
Maternal and fetal health is optimized when conception is planned during inactive disease and control is maintained throughout pregnancy. |
Close collaboration and network should occur across clinical specialties, including rheumatologists, dermatologists, obstetrician–gynecologists, and neonatologists, GPs etc., to ensure that patients’ educational and reproductive health needs are met. |
Physicians should be proactive about family planning for women with chronic inflammatory diseases. |
Introduction
Women of reproductive age are frequently affected by chronic inflammatory diseases (CID) such as rheumatoid arthritis (RA), psoriatic arthritis (PsA), or psoriasis (PSO). RA is the most common type of chronic inflammatory arthritis, with women outnumbering men. It has been reported that women experience their first RA symptoms at a younger age than men [1], and they tend to have a more severe course of the disease.
When women of childbearing age and family planning are diagnosed with CID, they face many reproductive health issues. Women with RA are more likely than the general population to experience sub- or infertility [2] and the time to pregnancy is longer (TTP > 12 months) [3]. Although the reasons for smaller family sizes have not been fully explained, they may include personal preference, uncontrolled inflammatory disease, sexual dysfunction caused by RA, psychosocial factors effects of medical treatment, or medication [4]. Pregnant women with CID are concerned about the potential complications of pregnancy, as well as how their condition will affect their health and the health of the newborn. Concerns may have been raised about how the disease and its treatment will affect conception, the natural course of their pregnancy and childbirth, fetal development in the womb, child development after birth, and their ability to breastfeed and care for the child [5,6,7,8]. Previous research has found that women with active RA have higher rates of prematurity, preeclampsia, Cesarean delivery, and low birth weight infants, but women with well-controlled RA had pregnancy outcomes comparable to the general population [9,10,11]. Concerns have also been expressed about decreased sexual activity in women as a result of psoriatic diseases, which have been shown to interfere with sexual activity [12, 13]. As a result, good CID control before conception is critical for disease remission, a safe pregnancy, and the delivery of a healthy newborn.
A multidisciplinary approach to pregnancy care may result in the best possible outcomes for both mother and newborn [14, 15]. However, shared decision-making is not always practiced. Lack of collaboration is a critical issue, as chronic disease specialists and obstetricians may not work closely together in the management of chronic diseases during pregnancy. As a result, clinicians have fewer opportunities to agree on the best treatment approach for their patients based on fertility goals and overall health needs, potentially leading to conflicting clinical advice [8, 16].
Because the severity of RA, PsA, and PSO, as well as their associated comorbidities and specific treatment, can harm pregnancy and childbirth [17, 18], optimal disease activity management is required before, during, and after pregnancy to manage the impact of disease activity on fertility, pregnancy outcomes, complications, and ability to nurse the child. Previous research has found, however, that more than half of the women with CID receive inconsistent clinical advice about their treatment options during pregnancy from a variety of healthcare professionals [8, 16]. Overall, there appears to be a lack of information and standardization of that information about reproductive health needs among women with rheumatic disease.
Women of childbearing age and family planning who have CID have special needs that should be addressed by modern medicine. Previous research has demonstrated the significance of treating physicians receiving education and training to provide appropriate care to women of childbearing age [14, 19].
Reproductive health is quickly becoming an essential component of modern comprehensive care [14]. For women with these conditions and of childbearing age, discussions about parenthood, including plans for childbearing, are critical in this context [14, 16]. As a result, we conducted a questionnaire survey to assess physicians’ knowledge about relevant issues, unmet needs, and limitations in managing sexually active, childbearing-age women with CID, such as moderate-to-severe RA, PsA, and PSO, as well as therapeutic practices and how to contribute to better health outcomes. This survey was created in collaboration with rheumatologists and dermatologists from three Central European countries.
Methods
This was a questionnaire survey that looked at the rheumatologist and dermatologists' knowledge of reproductive health in women with RA, PsA, or PSO, as well as the timing and manner of discussions between women and physicians, collaboration among different specialists, treatment options during pregnancy, and any unmet needs. The survey's goal was to gather additional information about women’s reproductive health. This article does not contain any new studies with human participants or animals performed by any of the authors.
From mid-November to mid-December 2019, the questionnaire was distributed. A total of 185 physicians were contacted about the questionnaire in advance and 120 physicians from three Central European countries agreed to take part in the survey. There was no defined strategy for selecting particular physicians. All 120 physicians were specialists who worked in biological rheumatology/dermatology centers and had prior experience with biological treatments. Rheumatologists were interviewed in Hungary (n = 50), the Czech Republic (n = 20), and Slovakia (n = 12); dermatologists were interviewed in the Czech Republic (n = 30) and Slovakia (n = 8).
The questionnaire contained a total of 55 questions in English, divided into four primary areas of inquiry:
-
1.
Epidemiology, daily clinical practice, and assessment of the general knowledge of rheumatologists and dermatologists on the topic of reproductive health (n = 29 questions)
-
2.
Multidisciplinary interactions among different specialists (n = 4 questions)
-
3.
Current clinical treatment in women of the age group 18–45 years (n = 17 questions)
-
4.
Identification of unmet needs (n = 5 questions)
The following issues were also addressed in the questionnaire:
-
Determining the impact of the patient’s age or gender on the treatment decision.
-
Assessment of the optimal conception time in women with RA, psoriasis, and psoriatic arthritis.
-
Determining whether previous treatment of the disease delays conception, as well as the best time to adjust treatment and dosage after the pregnancy, is planned.
Our questionnaire was designed to encourage the spontaneity of respondents on specific responses while also allowing for the uniform processing of these responses, their mutual comparison, and overall assessment. The respondents were given a list of possible options, which they could further expand with unmentioned variants. If the provided options did not adequately describe the situation in their local clinical practice, they were free to respond completely spontaneously in their own words.
The physicians were informed about the questionnaire prior to participating; participation was voluntary and data collected were anonymized before analysis. Consent was implied on the return of a completed questionnaire. The agreement template contains a confidentiality clause as well as a specific mention of the voluntariness to participate. Ethics committee review was not sought for this online physician’s survey research and is exempted under Hungarian Medical Research Council’s Scientific and Research Ethics Committee (Legislation: 23/2002. (V. 9.) Decree of the Minister of Health on medical research conducted on humans; Validity: 20.08.2019 to 23/2002.).
Statistical Analysis
Because this is a descriptive analysis, no statistical analysis was planned. Each of the 55 items in the questionnaire came with detailed instructions for completion (Supplementary file).
Results
This survey included a total of 120 physicians, where 82 rheumatologists and 38 dermatologists participated in the survey. A total of 55 survey questions were distributed among the physicians. According to 65% [78/120]) of respondents, the proportion of female patients of childbearing age and family planning with moderate-to-severe RA, PsA, or PSO was 10–30% (aged 18–45 years). Approximately two-thirds of the respondents discussed family planning with their female patients when making the diagnosis. According to the respondents' personal experiences, the proportion of unplanned pregnancies was less than 20%. Better patient education and collaboration were two key factors considered by these experts in reducing unplanned pregnancies.
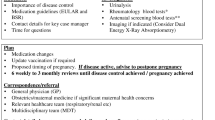
The effects of treatment during pregnancy were the primary concern for female patients, followed by concerns about the disease's effects on family planning and breastfeeding, according to surveyed physicians (Fig. 1). Additional issues and questions raised by physicians in this study are depicted in Fig. 1. All the dermatologists and 96% (79/82) of the rheumatologists surveyed were influenced by their female patient's potential fertility and pregnancy (Fig. S1). However, 11% (4/38) of the dermatologists and 39% (32/82) of the rheumatologists reported that gender did not influence treatment choice alone. The age of patients had a significant impact on the physicians’ treatment decisions; 97% (37/38) of the dermatologists and 78% (64/82) of the rheumatologists considered age before making their treatment decisions (Fig. S1).
Physicians reported that uncontrolled disease (dermatologists 29% [11/38] and rheumatologists 75% [61/82]) and disease severity (dermatologists 27% [10/38] and rheumatologists 76% [62/82]) are the main risk factors associated with conception in this female population (Fig. 2). More than half of the dermatologists (53% [20/38]) and the majority of the rheumatologists (79% [65/82]) believe that poor pregnancy outcomes in women are linked to poor disease control (Fig. S2).
The dermatologists and rheumatologists’ interdisciplinary collaboration was noticeably different. While most dermatologists collaborated almost entirely with a gynecologist–obstetrician, rheumatologists collaborated with a wider range of specialties in addition to the gynecologist–obstetrician. Compared to dermatologists, rheumatologists in greater number collaborated with the neonatologists (40% [33/82] vs. 10% [4/38]), immunologists (32% [26/82] vs. 3% [1/38]), GP/family doctors (29% [24/82] vs. 3% [1/38]) internists (18% [15/82] vs. 8% [3/38]), geneticists (34% [28/82] vs. 8% [3/38]), and infectologists (13% [10/82] vs. 3% [1/38]) (Fig. 3).
More than half of the dermatologists (53% [20/38]) and a small number of rheumatologists (17% [14/82]) had never heard of preconception treat-to-target management that takes the patient's desire to become pregnant into account (Fig. S2). More than half of the rheumatologists (44% [36/81]) reported that they usually modified systemic treatment only 6 months before their patients planned to become pregnant, whereas the dermatologists acted much earlier, 26% (10/38) acting 2–3 years before planned parenthood (Fig. 4).
Glucocorticoids were the drug of choice for moderate-to-severe disease flares during pregnancy; dermatologists preferred topical glucocorticoids for PSO patients (62.1% [23/37]), while rheumatologists used systemic glucocorticoid treatment for flares in patients with RA (86.7% [66/76]) and PsA (81.3% [52/64]) (Fig. 5a–c). The majority of dermatologists (94% [36/38]) and rheumatologists (99% [81/82]) correctly stated that there is a high risk of disease flaring after childbirth (Fig. S2).
The European League Against Rheumatism recommends that children who have been exposed to maternal biological drugs near the end of the second and third trimesters of pregnancy receive regular vaccinations. While national vaccination programs can be followed, children should not receive live or live-attenuated vaccines during the first 6 months of life [20]. Only 50% of dermatologists (19/38) were able to choose the correct time range for these vaccinations, whereas 83% (68/82) of rheumatologists were able to do so (Fig. S2).
The physicians also stated that there is a greater need for practical information on women’s health and fertility, family planning, pregnancy, and breastfeeding. Congresses (international for dermatologists and national for rheumatologists) and interdisciplinary forums where they could primarily discuss case studies were the three most appropriate services, activities, and needs that respondents perceived to be beneficial for themselves and their clinical practice in the areas of family planning, fertility, women's health, and medical care (Fig. S3).
Discussion
Reproductive health care is an important component of overall care for all women, but women with rheumatic diseases and psoriasis have unique reproductive health requirements. According to the findings of this three-country survey, roughly two-thirds of physicians discuss family planning with their patients when making a routine diagnosis for them. Rheumatologists and dermatologists may not consider family planning to be a part of their clinical commitments, or they may regard it as a burden that must be addressed during clinic visits due to other concerns. Some physicians may feel less competent or uneasy discussing reproductive health issues because they are considered taboo, which may indicate a lack of knowledge about how to begin family-planning conversations. This viewpoint is supported by the most recent European dermatology [20] and rheumatology guidelines [21], which advocate for more candid discussions about patients' goals for starting families. These guidelines recommend consultation and information sharing across specialties, including with an obstetrician [20] and the decision on drug therapy during pregnancy and lactation should be based on agreement between the internist/rheumatologist, gynecologist/obstetrician, and the patient [21]. Even though a small percentage of women with CID become pregnant unexpectedly, the physicians must discuss potential pregnancy with all female patients aged 18–45 during consultations. All women of childbearing age must also initiate discussions about family planning on time and maintain ongoing dialogue with their physicians. Treatment implications must be considered in all sexually active women with PSO, PsA, or RA, even if they do not intend to start a family. This is especially important as approximately half of all pregnancies [22, 23] are unplanned, including among PSO, RA, and PsA patients.
Patients' top concerns, according to surveyed physicians, are treatment before, during, and after pregnancy. In line with this, almost all the physicians surveyed said that their female patients' fertility and pregnancy potential influenced their treatment decisions.
According to current guidelines, glucocorticoids are safe to use during pregnancy and in breastfeeding women with rheumatic disease [24, 25]. As a result, rheumatologists stated that systemic glucocorticoids were their first choice for moderate-to-severe illness flares during pregnancy, whereas dermatologists stated that topical glucocorticoids were their first choice in this survey. Furthermore, all rheumatologists and the majority of dermatologists accurately predicted that the risk of the flare would increase after childbirth.
This survey also revealed distinct differences in the treatment strategies of dermatologists and rheumatologists. Dermatologists were more likely to consider gender and preconception discussions for treatment variations and family planning. Rheumatologists, on the other hand, are slightly more focused on reproductive health. The increased emphasis on reproductive health and family planning in various rheumatology forums over the last 3–5 years may explain some of this disparity. A recent prospective study found that nearly 80% of the patients had low disease activity at their previous visit before pregnancy, highlighting the necessity for a treat-to-target approach. In the vast majority of patients with RA, the treat-to-target approach resulted in low disease activity during pregnancy and postpartum [26]. According to this survey, only a few rheumatologists and more than half of the dermatologists in this survey were unaware of preconception treatment-to-target management, which takes into account the patient's desire to become pregnant. This finding highlights the importance of focusing more attention on the effects of the modern treatment approach on fertility and pregnancy outcomes in surveyed countries. None of the medications used in treatment of PsA or PSO are completely risk-free during pregnancy. There may be disagreements between rheumatologists/dermatologists and obstetricians regarding medication recommendations. Further, there is a need to consider the effects of pregnancy on maternal pathology, the impact of disease activity on the fetus, and pharmacology safety during pregnancy. Women generally believe they serve as a liaison between rheumatologists and obstetrician–gynecologists, but they would prefer for providers to communicate directly about their sexual and reproductive health [27]. Although there are numerous safe options for the treatment of women of childbearing age in PSO, there are genuine concerns about the safety of novel biological therapies during pregnancy and lactation. Thus, a multidisciplinary approach may enable better management of pregnancy and complications associated with it. In pregnant women with rheumatic diseases, multidisciplinary consultation could lead to a high rate of successful obstetric and neonatal outcomes [28]. In this survey, almost all rheumatologists and dermatologists consulted a gynecologist–obstetrician. However, more rheumatologists collaborated with a broader range of other specialists than dermatologists, who mostly consulted a gynecologist–obstetrician, suggesting that physicians should promote multidisciplinary treatment for pregnant women. The course of PsA is variable and unpredictable and can vary from mild and nondestructive to severe, and debilitating with destructive joint arthropathy and extra-articular manifestations. Because PsA can be destructive, systemic therapy is necessary more often in dermatology, and referral and collaboration outside their specialty is required. Furthermore, there is a need to cover not only the potential and expecting mother but also the fetus and newborn baby, for example, the use of vaccines in infants.
The following fundamental ideas, facts, and questions were highlighted during the implementation of this questionnaire survey:
-
Pregnancy and family planning is a complex challenge for clinicians treating women with chronic inflammatory disease.
-
There is currently a lack of well-established national guidelines, recommendations, and algorithms for the treatment of women of reproductive age that rheumatologists and dermatologists can use in everyday clinical practice in the countries where the surveyed physicians practice.
-
Pregnancy preparation to minimize risks and complications for both mother and fetus, women of reproductive age with chronic inflammatory diseases such as RA, psoriasis, and PsA must have consultations with their physicians. Both proper timing and discontinuation of contraindicated drugs while maintaining control of disease activity are topics that can be discussed.
-
Treatment optimization is essential before planning for pregnancy.
-
A treat-to-target management approach should be used in daily clinical practice.
-
Close collaboration among clinical specializations, such as rheumatologists, dermatologists, gynecologists–obstetricians, neonatologists, general practitioners, and others, is necessary to ensure that patients' reproductive health education and healthcare needs are satisfied.
-
The promotion of multidisciplinary medical care and shared decision-making is imperative in pregnant patients.
-
The general importance of a holistic approach.
One of the advantages of this questionnaire survey is that it is a cross-border investigation from the perspective of physicians, with the participation of two types of specialists, dermatology, and rheumatology, from different countries that are geographically and historically close. Despite all efforts, this survey is not without limitations. We did not assess or categorize the physicians’ level of experience with biologics or reproductive health. The data provided is based on actual clinic experience. Although there was no set strategy for selecting specific physicians, it stands to reason that those who have had more exposure to this interdisciplinary approach would be more open to it. In this survey, we sought to pay particular attention to the viewpoint of physicians since patients' concerns have already been taken care of elsewhere [29]. Furthermore, it is possible that patients are unaware of how the condition and available treatments may affect them at different stages of life, which is why understanding the physicians' perspective is critical. The lack of formal survey validation and the difficulties of delivering the survey in the English language are other limitations of this study.
Conclusions
To improve the reproductive health of sexually active women of childbearing age in Central Europe who have CID, rheumatologists and dermatologists must improve their education and work with other specialists. More timely discussions with women of reproductive age and family planning are needed to educate them about the disease's effects on their childbearing potential and the selection of treatment options based on their reproductive goals. Dermatologists and rheumatologists must coordinate their care for pregnant women with the recommendations of other physicians involved in pregnancy care. Best practices in patient-centered care must consider each patient's reproductive decisions in their treatment planning to give the best patient-centered care.
References
van Vollenhoven RF. Sex differences in rheumatoid arthritis: more than meets the eye. BMC Med. 2009;7:12.
Skomsvoll JF, Ostensen M, Baste V, Irgens LM. Number of births, interpregnancy interval, and subsequent pregnancy rate after a diagnosis of inflammatory rheumatic disease in Norwegian women. J Rheumatol. 2001;28:2310–4.
Jawaheer D, Zhu JL, Nohr EA, Olsen J. Time to pregnancy among women with rheumatoid arthritis. Arthritis Rheum. 2011;63:1517–21.
Provost M, Eaton JL, Clowse ME. Fertility and infertility in rheumatoid arthritis. Curr Opin Rheumatol. 2014;26:308–14.
Ackerman IN, Jordan JE, Van Doornum S, Ricardo M, Briggs AM. Understanding the information needs of women with rheumatoid arthritis concerning pregnancy, post-natal care and early parenting: a mixed-methods study. BMC Musculoskelet Disord. 2015;16:194.
Andreoli L, Lazzaroni MG, Carini C, et al. “Disease knowledge index” and perspectives on reproductive issues: a nationwide study on 398 women with autoimmune rheumatic diseases. Jt Bone Spine. 2019;86:475–81.
Carandang K, Mruk V, Ardoin SP, et al. Reproductive health needs of adolescent and young adult women with pediatric rheumatic diseases. Pediatr Rheumatol. 2020;18:66.
Chakravarty E, Clowse ME, Pushparajah DS, Mertens S, Gordon C. Family planning and pregnancy issues for women with systemic inflammatory diseases: patient and physician perspectives. BMJ Open. 2014;4: e004081.
Chakravarty EF, Nelson L, Krishnan E. Obstetric hospitalizations in the United States for women with systemic lupus erythematosus and rheumatoid arthritis. Arthritis Rheum. 2006;54:899–907.
Lin HC, Chen SF, Lin HC, Chen YH. Increased risk of adverse pregnancy outcomes in women with rheumatoid arthritis: a nationwide population-based study. Ann Rheum Dis. 2010;69:715–7.
Wallenius M, Skomsvoll JF, Irgens LM, et al. Pregnancy and delivery in women with chronic inflammatory arthritides with a specific focus on first birth. Arthritis Rheum. 2011;63:1534–42.
Meeuwis KA, de Hullu JA, van de Nieuwenhof HP, et al. Quality of life and sexual health in patients with genital psoriasis. Br J Dermatol. 2011;164:1247–55.
Kerschbaumer A, Fenzl KH, Erlacher L, Aletaha D. An overview of psoriatic arthritis—epidemiology, clinical features, pathophysiology and novel treatment targets. Wien Klin Wochenschr. 2016;128:791–5.
Murray K, Moore L, O’Brien C, et al. A multidisciplinary approach to reproductive healthcare in women with rheumatic disease. Ir J Med Sci. 2020;189:237–43.
Østensen M. Management of early aggressive rheumatoid arthritis during pregnancy and lactation. Expert Opin Pharmacother. 2009;10:1469–79.
Gordon C. How does rheumatic disease affect family planning and pregnancy? Rheumatology. 2016;55:i22–i22.
Gottlieb AB, Ryan C, Murase JE. Clinical considerations for the management of psoriasis in women. Int J Womens Dermatol. 2019;5:141–50.
Krause ML, Makol A. Management of rheumatoid arthritis during pregnancy: challenges and solutions. Open Access Rheumatol. 2016;8:23–36.
Nelson-Piercy C, Vlaev I, Harris K, Fischer-Betz R. What factors could influence physicians’ management of women of childbearing age with chronic inflammatory disease? A systematic review of behavioural determinants of clinical inertia. BMC Health Serv Res. 2019;19:863.
Nast A, Smith C, et al. EuroGuiDerm guideline on the systemic treatment of psoriasis vulgaris—Part 2: specific clinical and comorbid situations. J Eur Acad Dermatol Venereol. 2021;35:281–317.
Götestam Skorpen C, Hoeltzenbein M, Tincani A, et al. The EULAR points to consider for use of antirheumatic drugs before pregnancy, and during pregnancy and lactation. Ann Rheum Dis. 2016;75:795–810.
Kavanaugh A, Cush JJ, Ahmed MS, Bermas BL, Chakravarty E, Chambers C. Proceedings from the American College of Rheumatology Reproductive Health Summit: the management of fertility, pregnancy, and lactation in women with autoimmune and systemic inflammatory diseases. Arthritis Care Res (Hoboken). 2015;67:313–25.
Murase JE, De Simone C, Fischer-Betz R, Ecoffet C, Tincani A. Fears and misconceptions of women with chronic inflammatory diseases on their journey to motherhood. J Am Acad Dermatol. 2019; 81(4, Suppl.1):AB65.
Skorpen CG, Hoeltzenbein M, Tincani A, et al. The EULAR points to consider for use of antirheumatic drugs before pregnancy, and during pregnancy and lactation. Ann Rheum Dis. 2016;75:795–810.
Flint J, Panchal S, Hurrell A, et al. BSR and BHPR guideline on prescribing drugs in pregnancy and breastfeeding-Part I: standard and biologic disease modifying anti-rheumatic drugs and corticosteroids. Rheumatology (Oxford). 2016;55:1693–7.
Smeele HT, Röder E, Wintjes HM, Kranenburg-van Koppen LJ, Hazes JM, Dolhain RJ. Modern treatment approach results in low disease activity in 90% of pregnant rheumatoid arthritis patients: the PreCARA study. Ann Rheum Dis. 2021;80:859–64.
Wolgemuth T, Stransky OM, Chodoff A, et al. Exploring the preferences of women regarding sexual and reproductive health care in the context of rheumatology: a qualitative study. Arthritis Care Res. 2021;73:1194–200.
Añón-Oñate I, Cáliz-Cáliz R, Rosa-Garrido C, Pérez-Galán MJ, Quirosa-Flores S, Pancorbo-Hidalgo PL. Multidisciplinary unit improves pregnancy outcomes in women with rheumatic diseases and hereditary thrombophilias: an observational study. J Clin Med. 2021;10:1487.
Tincani A, Taylor P, Fischer-Betz R, EULAR, et al. FRI0693 fears and misconceptions of women with chronic rheumatic diseases on their journey to motherhood. Ann Rheum Dis. 2018;2018(77):866.
Acknowledgements
Funding
All costs associated with the development of this study were supported by eVisit Ltd., Hungary, and PharmIn s.r.o., Slovakia, and funded by UCB Pharma, which also funded the Rapid Service Fee.
Medical Writing, Editorial, and Other Assistance
Medical writing support was provided by Sreeharsha, MPharm, and Ritu Guglani, MD, Enago Life Sciences, India, and funded by UCB Pharma. Publication management was provided by Costello Medical, UK, and funded by UCB Pharma.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design. Material preparations were performed Želmíra Macejová, Spyridon Gkalpakiotis, and Leona Procházková. Data collection and analysis were performed by Zoltán Tóth and Pavel Prágr. The first draft of the manuscript was written by Marta Olejárová and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Prior Presentation
Previously presented as interim data at Hungarian MRE Congress 2021, 23–26 Sep, Debrecen, Hungary.
Disclosures
Marta Olejárová is a consultant, speaker, or investigator for AbbVie, Eli Lilly, Novartis, Sandoz, Pfizer, Amgen, Viatris, Bausch Health). Želmíra Macejová has been a speaker or investigator for AbbVie, Biogen, Eli Lilly, Janssen, Novartis, Pfizer, and UCB. Spyridon Gkalpakiotis has served as a consultant, speaker, or investigator for AbbVie, Celgene, Eli Lilly, Janssen, Leo Pharma, Novartis, Pfizer, and UCB. Leona Procházková has served as a consultant, speaker, or investigator for AbbVie, Biogen, Celgene, Eli Lilly, Gilead, Glaxo Smith Kline, Janssen, Novartis, Pfizer, and UCB.
No potential conflict of interest was reported by Zoltán Tóth. Pavel Prágr has worked as an external medical consultant for pharmaceutical companies in the Czech and Slovak Republics.
Compliance with Ethics Guidelines
This was a descriptive, voluntary, non-interventional questionnaire. The physicians were informed about the questionnaire prior to participating; participation was voluntary and data collected were anonymized before analysis. Consent was implied on the return of a completed questionnaire. The agreement template contains a confidentiality clause as well as a specific mention of the voluntariness to participate. This survey did not need IRB approval as per Hungarian Medical Research Council’s Scientific and Research Ethics Committee legislation, 23/2002. (V. 9.) Decree of the Minister of Health on medical research conducted on humans (Validity: 20.08.2019 -23/2002).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Olejárová, M., Macejová, Ž., Gkalpakiotis, S. et al. Reproductive Healthcare in Women with Rheumatoid Arthritis and Psoriatic Diseases in Routine Clinical Practice: Survey Results of Rheumatologists and Dermatologists. Rheumatol Ther 9, 1575–1586 (2022). https://doi.org/10.1007/s40744-022-00488-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-022-00488-z