Abstract
Introduction
Diagnosis difficulties are common for ankylosing spondylitis (AS) patients, leading to inadequate and inconsistent treatment. We evaluated the national and geographic variability in disease diagnosis and treatment in the United States.
Methods
This retrospective, cross-sectional analysis utilized the IBM® MarketScan® Administrative Claims Database from 2014 to 2019. AS patients ≥ 18 years of age with continuous medical and pharmacy enrollment during the calendar year and complete geographic information during the study period were included. Patient cohorts assessed were D1 (≥ 1 AS diagnoses within each calendar year of assessment between 2014 and 2019), D2 (≥ 2 non-rheumatologist AS diagnoses), and D3 (≥ 2 rheumatologist AS diagnoses). For D2 and D3, diagnoses were ≥ 6 months apart, but within 18 months. Annual AS diagnostic prevalence and treatment rates were determined from 2014 to 2019 nationally and per state in 2019. Treatments assessed were disease-modifying antirheumatic drugs (DMARDs), opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and methotrexate.
Results
Nationally, AS diagnostic prevalence increased from 2014 to 2019, with 2019 rates of 9.6 (D1), 5.1 (D2), and 3.5 (D3) per 10,000 persons. Diagnostic prevalence varied between states, which was not explained by age, sex, racial distribution, or rheumatologists per capita. Nationally, a greater percentage of D3 patients vs. D1 and D2 patients received biologic/targeted synthetic DMARDs (bDMARD/tsDMARDs) and conventional synthetic DMARD. Opioid use ranged from 37 to 40% in 2019 and decreased from 2014 for all cohorts. Corticosteroid and methotrexate use decreased slightly, while NSAID and bDMARD/tsDMARD use generally increased from 2014 to 2019.
Conclusions
AS diagnostic prevalence is increasing nationally, though it remains low among some states. bDMARD/tsDMARDs use was more common among patients treated by rheumatologists. Opioid and corticosteroid use is decreasing, though national rates remain high with significant state variability. Further education is needed, particularly in states with low prevalence and inadequate treatment, to improve diagnosis and treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Variations in diagnostic disease prevalence and treatment patterns for ankylosing spondylitis throughout the United States is not known. |
National data over time can identify trends and highlight where improvements have been made and where gaps may continue to exist. |
State-level data may provide opportunity to tailor educational efforts, based on regional needs, to address persisting gaps and improve diagnosis and treatment for ankylosing spondylitis patients. |
What was learned from this study? |
The diagnostic prevalence of ankylosing spondylitis is low in the United States, though increasing annually from 2014 to 2019 with significant variability across states. |
Inappropriate treatment both nationally and on a state level exists, particularly in the high use of opioids and corticosteroids, indicating the need for greater education. |
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory immune-mediated condition primarily affecting the sacroiliac joints and spine, with a prevalence of 0.2–0.5% in the United States [1, 2]. Patients with AS suffer mostly with inflammatory back pain, peripheral inflammatory arthritis, enthesitis, and dactylitis [2]. As a consequence of these symptoms, patients with AS have reduced capability to perform day-to-day tasks, ability to work, and overall health-related quality of life and increased need of care [3,4,5].
Diagnosis of AS can be delayed by more than 10 years because radiographic features of the disease can take years to develop [6]. Furthermore, based on a retrospective analysis of administrative claims data from 2000 to 2012, only 37% of patients with AS were diagnosed by a rheumatologist in the United States [5]. Rheumatologist visit frequency, which can influence diagnosis rates, can be affected by various factors, including the number of rheumatologists in the region and length of time to obtain care [5, 7]. Additionally, sex and human leukocyte antigen (HLA)-B27 status can affect AS diagnosis rates. Women with AS present with less structural damage in the sacroiliac joints and the spine than men, which could influence diagnosis [8, 9]. AS is strongly associated with HLA-B27 status, with 85–95% of White patients with AS being HLA–B27-positive [10]. The prevalence of HLA-B27 positivity is higher in Whites (7.5%) than Blacks (1.1%) [11], which may at least partly explain the lower prevalence of AS in Blacks (0.9%) than Whites (1.5%) [12].
With diagnosis difficulties, proper treatment of patients with this disease can be substantially deferred. The 2019 treatment guideline recommendations by the American College of Rheumatology (ACR), Spondylitis Association of America (SAA), and Spondyloarthritis Research & Treatment Network (SPARTAN) for AS include nonsteroidal anti-inflammatory drugs (NSAIDs) and biologic disease-modifying antirheumatic drugs (bDMARDs), including tumor necrosis factor (TNF) inhibitors and the interleukin-17A antagonists secukinumab or ixekizumab [13]. The Janus kinase (JAK) inhibitor tofacitinib can also be considered in patients with coexisting ulcerative colitis if TNF inhibitors are not an option [13]. Conventional synthetic DMARDs (csDMARDs), such as sulfasalazine or methotrexate, should be considered only in patients with prominent peripheral arthritis or when TNF inhibitors are not available [13]. Rheumatologists strongly recommend against the use of systemic corticosteroids [13]. Although opioids are not a recommended treatment in current guidelines, chronic opioid use is common among patients with AS despite issues associated with opioid misuse [14].
Given the variability in diagnosis and approaches to treatment for AS, it is important to understand how they differ across the United States. This type of investigation is particularly relevant for identifying regional gaps in the diagnosis and treatment of these patients to better target efforts to improve the management of patients with AS. Currently, there is a lack of knowledge on the variation in diagnosis and treatment approaches for AS throughout the United States. To the best of our knowledge, previous studies have not evaluated geographic variation of AS diagnostic prevalence and treatment in the United States. Consequently, we conducted a retrospective cross-sectional analysis of an insurance-claims database to describe geographic variations in diagnostic prevalence and treatment of AS in the United States.
Methods
Study Design
This was a retrospective cross-sectional analysis using the IBM® MarketScan® Commercial Claims Database for the period of January 2014 to December 2019. This database contains claims data from approximately 66 million employees and their dependents in the United States and consists of standardized inpatient, outpatient, pharmaceutical, and health plan enrollment data [15]. A variety of employee-sponsored private health insurance types are covered by this database, including health maintenance organization, point-of-service, and preferred provider organization plans [15].
All database records were de-identified and compliant with United States patient confidentiality requirements, including the Health Insurance Portability and Accountability Act of 1996 [15]. Because of this, institutional review board approval was not required.
Study Population
Patients ≥ 18 years of age with ≥ 1 AS International Classification of Diseases (ICD)-9 (720.0) or ICD-10 (M45.x) codes in the calendar year were included in the study. Eligible patients were required to have continuous medical and pharmacy enrollment during the calendar year and complete geographic information during the study period. If a patient had ≥ 2 states recorded for a given year, the last state recorded was used.
Three AS cohort definitions were used for this study. Definition 1 (D1) included patients with ≥ 1 AS diagnosis in the year by any provider. Definition 2 (D2) included patients with ≥ 2 AS diagnoses at least 6 months apart, but within 18 months by a non-rheumatologist. Definition 3 (D3) included patients with ≥ 2 AS diagnoses at least 6 months apart, but within 18 months by rheumatologists. For D3, a rheumatologist visit was defined as an AS diagnosis and rheumatologist visit occurring in the same claim.
Outcomes
Outcomes evaluated were the rates of AS diagnoses (per 10,000 persons), calculated across cohort definitions, and the proportion of patients with AS who received NSAIDs, bDMARD/targeted synthetic DMARDs (tsDMARDs), csDMARDs (including methotrexate, reported separately), corticosteroids, and opioids (Supplemental Table S1). bDMARD/tsDMARDs included adalimumab, certolizumab, etanercept, golimumab, infliximab, secukinumab, ustekinumab, and tofacitinib. csDMARDs included hydroxychloroquine, leflunomide, methotrexate, and sulfasalazine. Methotrexate was reported separately as it is more prevalently used than other csDMARDs [16]. Treatments were identified through National Drug Code and Health Common Procedure Coding System (HCPCS) codes.
Variations in AS diagnosis by age, sex, race (surrogate for HLA-B27), and rheumatologists per capita were determined for 2019 on a state level. Age, sex, and race were based on United States census data and presented as percentiles on a state level. The category rheumatologists per capita was based on American Board of Internal Medicine Specialty data and was presented as percentiles on a state level.
Outcomes were evaluated on a national level for each calendar year from 2014 to 2019. Outcomes were evaluated on a state level for 2019 and were reported for all states with the highest and lowest states indicated for states in which > 20 patients had an AS diagnosis for prevalence or received an AS respective treatment for treatment rates.
Statistical Analyses
Categorical variables were reported as frequency and percentages and continuous variables as mean with standard deviation. All data analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
Study Population
The number of patients diagnosed with AS from 2014 to 2019 ranged from 10,811–13,077 for D1, 5569–6532 for D2, and 3775–4901 for D3 (Table 1 and Supplemental Table S2). Overall age did not vary between cohorts and for each evaluation year while an increase of 3–5% from 2014 to 2019 was noted in the percent of females (Table 1).
National AS Diagnosis Rates
From 2014 to 2019, diagnosis rates per 10,000 persons increased from 6.7 to 9.6 (D1), 3.3–5.1 (D2), and 2.5–3.5 (D3) (Table 2). Interestingly, the total population of the database decreased over time, reflecting decreasing enrollment in the plans captured by the MarketScan database. However, trends indicating increasing diagnosis rates over time remained consistent over the study period and diagnosis definitions. This increase did not appear to be related to changes in the percentage of patients who visited a rheumatologist, which fluctuated each year from 2014 to 2019 and ranged from 44 to 49% for D1 and 48 to 54% for D2 (Supplemental Table S3).
State-Level AS Diagnosis Rates
In 2019, diagnosis rates per 10,000 persons were highest in Idaho (26, 20, and 13 for D1, D2, and D3, respectively) and lowest in Iowa and Nebraska for D1 (6), Iowa and Nevada for D2 (3), and Michigan for D3 (2) (Fig. 1).
AS diagnostic prevalence (per 10,000 persons) by state in 2019. A Patients with ≥ 1 AS diagnosis (D1), B patients with ≥ 2 AS diagnoses by non-rheumatologists (D2), C patients with ≥ 2 AS diagnoses by rheumatologists (D3). AK Alaska, AL Alabama, AR Arkansas, AS ankylosing spondylitis, AZ Arizona, CA California, CO Colorado, CT Connecticut, D Definition, DE Delaware, FL Florida, GA Georgia, HI Hawaii, ID Idaho, IL Illinois, IN Indiana, IO Iowa, KS Kansas, KY Kentucky, LA Louisiana, MA Massachusetts, MD Maryland, ME Maine, MI Michigan, MN Minnesota, MO Missouri, MS Mississippi, MT Montana, NC North Carolina, ND North Dakota, NE Nebraska, NH New Hampshire, NJ New Jersey, NM New Mexico, NV Nevada, NY New York, OH Ohio, OK Oklahoma, OR Oregon, PA Pennsylvania, RI Rhode Island, SC South Carolina, SD South Dakota, TN Tennessee, TX Texas, UT Utah, VA Virginia, VT Vermont, WA Washington, WI Wisconsin, WV West Virginia, WY Wyoming
The states with the highest diagnosis rates (4–13 per 10,000 persons) stratified by percentiles for mean age, percent of females and Whites, and rheumatologists per capita with diagnosis rates was determined for D3 (Supplemental Figures S1–S4). With age, the states with the highest diagnosis rates were located primarily in the Northwest for the top 25% age percentile and West and Southwest regions for the lowest 25% age percentile (Supplemental Figure S1). Based on the proportion of females in each state, the states with the highest diagnosis rates were primarily located in the South for the top 25% percentile and Midwest regions for the lowest 25% percentile (Supplemental Figure S2). With White race distribution, the states with the highest diagnosis rates were located in the West for the highest 20% percentile and South regions for the lowest 20% percentile (Supplemental Figure S3). Based on the number of rheumatologists per capita, the states with the highest diagnosis rates were primarily located in the Northeast for the top 25% percentile and West and South-Central regions for the lowest 25% percentile (Supplemental Figure S4).
National AS Treatment Rates
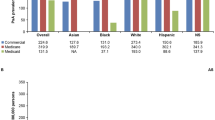
bDMARD/tsDMARDs were received by a greater percentage of patients in the D3 cohort than in the other cohorts (Fig. 2). For D3, 71% received either bDMARDs or tsDMARDs in 2014, which increased each year to 77% in 2019, while the percentage of patients receiving bDMARD/tsDMARDs in 2014 and 2019 for D1 was 45% and 46% and for D2 was 57% and 61%.
Annual AS treatment rates in the United States. A Patients with ≥ 1 AS diagnosis (D1), B patients with ≥ 2 AS diagnoses by non-rheumatologists (D2), C patients with ≥ 2 AS diagnoses by rheumatologists (D3). AS ankylosing spondylitis, bDMARD biologic DMARD, csDMARD conventional synthetic DMARD, D Definition, DMARD disease-modifying antirheumatic drug, MTX methotrexate, NSAID nonsteroidal anti-inflammatory drug, tsDMARD targeted synthetic DMARD
The percentage of patients receiving csDMARDs was also highest for D3 compared with the other cohorts (Fig. 2). For D3, 25% received csDMARDs in 2014, which decreased to 20% in 2019. By comparison, the percentage of D1 patients receiving csDMARDs was 19% in 2014 and 16% in 2019, while for D2 it was 21% in 2014 and 18% in 2019.
With opioids, use decreased for all cohorts from 2014. However, 37–40% of patients were still prescribed such treatment in 2019 (Fig. 2). For corticosteroids, NSAIDs, and methotrexate, similar usage trends from 2014 to 2019 were reported between the treatment cohorts. Furthermore, the percentage of patients in 2019 using the respective three treatments was comparable between the treatment cohorts. From 2014 to 2019, NSAID use increased while corticosteroid and methotrexate use slightly decreased.
State-Level AS Treatment Rates
For bDMARD/tsDMARDs, the highest rates in 2019 for D3 were in Minnesota and South Carolina (91%) and lowest in Idaho (69%) and Indiana (70%) (Table 3; Fig. 3). For the other cohorts, the states with the highest and lowest rates were New Mexico (67%) and Delaware (37%) for D1 and New Mexico (75%) and Alabama (50%) for D2 (Table 3; Fig. 3).
bDMARD/tsDMARD treatment rate (per 100 persons) for AS by state in 2019. A Patients with ≥ 1 AS diagnosis (D1), B patients with ≥ 2 AS diagnoses by non-rheumatologists (D2), C patients with ≥ 2 AS diagnoses by rheumatologists (D3). States in gray have ≤ 20 patients who received therapy and are not reported. AK Alaska, AL Alabama, AR Arkansas, AS ankylosing spondylitis, AZ Arizona, bDMARD biologic DMARD, CA California, CO Colorado, CT Connecticut, D Definition, DE Delaware, DMARD disease-modifying antirheumatic drug, FL Florida, GA Georgia, HI Hawaii, ID Idaho, IL Illinois, IN Indiana, IO Iowa, KS Kansas, KY Kentucky, LA Louisiana, MA Massachusetts, MD Maryland, ME Maine, MI Michigan, MN Minnesota, MO Missouri, MS Mississippi, MT Montana, NC North Carolina, ND North Dakota, NE Nebraska, NH New Hampshire, NJ New Jersey, NM New Mexico, NV Nevada, NY New York, OH Ohio, OK Oklahoma, OR Oregon, PA Pennsylvania, RI Rhode Island, SC South Carolina, SD South Dakota, TN Tennessee, tsDMARD targeted synthetic DMARD, TX Texas, UT Utah, VA Virginia, VT Vermont, WA Washington, WI Wisconsin, WV West Virginia, WY Wyoming
The rate of csDMARD use for D3 was highest in Oklahoma (33%) and lowest (16%) in North Carolina and New York (Table 3; Fig. 4). The states with the highest and lowest rates of csDMARD use for D1 were Maryland and Tennessee (both 25%) and Oregon and Wisconsin (both 11%), respectively, while for D2 it was Tennessee (32%) and North Carolina (14%) (Table 3; Fig. 4).
csDMARD treatment rate (per 100 persons) for AS by state in 2019. A Patients with ≥ 1 AS diagnosis (D1), B patients with ≥ 2 AS diagnoses by non-rheumatologists (D2), C patients with ≥ 2 AS diagnoses by rheumatologists (D3). States in gray have ≤ 20 patients who received therapy and are not reported. AK Alaska, AL Alabama, AR Arkansas, AS ankylosing spondylitis, AZ Arizona, CA California, CO Colorado, csDMARD conventional synthetic disease-modifying antirheumatic drug, CT Connecticut, D Definition, DE Delaware, FL Florida, GA Georgia, HI Hawaii, ID Idaho, IL Illinois, IN Indiana, IO Iowa, KS Kansas, KY Kentucky, LA Louisiana, MA Massachusetts, MD Maryland, ME Maine, MI Michigan, MN Minnesota, MO Missouri, MS Mississippi, MT Montana, NC North Carolina, ND North Dakota, NE Nebraska, NH New Hampshire, NJ New Jersey, NM New Mexico, NV Nevada, NY New York, OH Ohio, OK Oklahoma, OR Oregon, PA Pennsylvania, RI Rhode Island, SC South Carolina, SD South Dakota, TN Tennessee, TX Texas, UT Utah, VA Virginia, VT Vermont, WA Washington, WI Wisconsin, WV West Virginia, WY Wyoming
For opioids, the state with the highest rate was Idaho for D1 (65%), D2 (69%) and D3 (69%), while the state with the lowest rate for D1 and D2 was Massachusetts (20% and 24%, respectively), and for D3 it was Wisconsin (28%) (Table 3; Fig. 5). For corticosteroids, NSAIDs, and methotrexate, the highest and lowest state rates were similar between the cohorts (Table 3).
Opioid treatment rate (per 100 persons) for AS by state in 2019. A Patients with ≥ 1 AS diagnosis (D1), B patients with ≥ 2 AS diagnoses by non-rheumatologists (D2). C patients with ≥ 2 AS diagnoses by rheumatologists (D3). States in gray have ≤ 20 patients who received therapy and are not reported. AK Alaska, AL Alabama, AR Arkansas, AS ankylosing spondylitis, AZ Arizona, CA California, CO Colorado, CT Connecticut, DE Delaware, FL Florida, GA Georgia, HI Hawaii, ID Idaho, IL Illinois, IN Indiana, IO Iowa, KS Kansas, KY Kentucky, LA Louisiana, MA Massachusetts, MD Maryland, ME Maine, MI Michigan, MN Minnesota, MO Missouri, MS Mississippi, MT Montana, NC North Carolina, ND North Dakota, NE Nebraska, NH New Hampshire, NJ New Jersey, NM New Mexico, NV Nevada, NY New York, OH Ohio, OK Oklahoma, OR Oregon, PA Pennsylvania, RI Rhode Island, SC South Carolina, SD South Dakota, TN Tennessee, TX Texas, UT Utah, VA Virginia, VT Vermont, WA Washington, WI Wisconsin, WV West Virginia, WY Wyoming
Discussion
In this study, we evaluated the national and state trends in diagnostic prevalence and treatment for AS in the United States using data from an administrative claims database.
Nationally, diagnostic prevalence of AS was low, although it increased each year from 2014 to 2019, regardless of whether the diagnosis was from a rheumatologist or non-rheumatologist. Similar observations were made for patients with diagnoses made by any provider or non-rheumatologist. Additionally, the proportion of patients with AS who were female gradually increased each year, potentially indicating a greater awareness of the disease by women and their physicians. These diagnostic prevalence results are consistent with a previous study that found that rates of AS prevalence more than doubled from 0.04 to 0.09% between 2006 and 2016 in the United States [16]. However, the diagnostic prevalence of AS was low when compared to the population prevalence described in the 2009–2010 NHANES study [12]. The low diagnostic prevalence of AS may reflect that not all patients in the population who have the disease get diagnosed. In a systemic literature review of worldwide AS prevalence, diagnostic prevalence was 50% lower than population prevalence (11 vs. 22 per 10,000 persons) [17].
Significant state geographic variability was observed in AS diagnostic prevalence for the three diagnosis cohorts, with rates ranging from 26 per 10,000 persons in Idaho to six per 10,000 persons in Iowa and Nebraska for those diagnosed by any provider. For patients diagnosed by a rheumatologist, the diagnosis rates range was 13 per 10,000 persons in Idaho to two per 10,000 persons in Michigan. States with the highest diagnostic prevalence tended to be located primarily in the Western section of the country. Factors such as age, sex, race, and rheumatologists per capita did not explain the state variability in prevalence of diagnoses made by rheumatologists. Of note, patients included in the data source were covered by similar health plans, and therefore had similar access to care and treatment and insurance coverage; yet still, diagnosis rates were low and varied from state to state.
One reason for low national diagnostic prevalence rates and state variability reported in this current study may be the lack of awareness of this disease. In a real-world study of 235 patients with AS, about a third received a diagnosis for this disease after ≥ 10 years, while another third received a diagnosis 2–9 years following their initial physician visit [18]. Additional potential reasons for difficulties in diagnosis includes the commonality of mechanical back pain in general population; lack of diagnostic criteria or specific biomarkers; lack of awareness by primary physicians and allied providers such as chiropractors and physical therapists; low referrals to rheumatologists; and insufficient insurance coverage [7, 18,19,20]. These factors could be particularly relevant in those states with low diagnostic prevalence rates of AS. These findings highlight the need for a national education effort to increase disease awareness that would inform physicians on disease features which could indicate AS while providing criteria for referring the patient to a rheumatologist, particularly in states and regions with low diagnostic prevalence identified in this analysis [6, 21].
Annual treatment rates during 2014–2019 generally followed similar patterns across the three cohorts with bDMARD/tsDMARD and NSAID use increasing, while use of csDMARDs, opioids, corticosteroids, and methotrexate declining. Treatment rates for bDMARD/tsDMARDs were > 70% across the study period for patients with ≥ 2 AS diagnoses by a rheumatologist, and were much higher than rates of bDMARD/tsDMARD treatment for the other AS cohorts in this study. This indicates that rheumatologists may be more likely to treat confirmed AS patients with advanced therapies. The overall increase in bDMARD/tsDMARDs treatment rates from 2014 to 2019, which is generally consistent with a prior retrospective study from 2006 to 2016 [16], may be due to various factors, including greater patient awareness of these treatment options, the increased availability of bDMARD/tsDMARDs and biosimilars, the willingness of payors to reimburse patients for these treatments, and the higher referrals of patients to rheumatologists.
Notable geographic variations by state in treatment use were observed, including that for bDMARD/tsDMARDs, csDMARDs, and opioids. bDMARD/tsDMARD treatment rates ranged from 67% in New Mexico to 37% in Delaware for patients diagnosed by any provider and 91% in Minnesota to 69% in Idaho for patients diagnosed by a rheumatologist. Access to rheumatologists does not appear to explain such observed variations, as the differences persisted despite our state-level adjustment based on rheumatologists per capita. Other factors may be causing these variations, such as referrals to rheumatologists and awareness of treatment guidelines; further research is needed to confirm the underlying cause(s).
Although fewer patients were receiving treatments which have greater risks than benefits, such as opioids and corticosteroids, rates still remain higher than might be expected. Opioid use nationally occurred among 37–40% of patients with AS in 2019. The opioid use was particularly high in various states, including Idaho and Alabama, where 69% and 54% of patients, respectively, reported receiving this treatment. Similar reports of high chronic opioid use for AS been described in a retrospective study of patients from 2012 to 2017 [14]. The reasons for frequent opioid use remain uncertain, as there is no agreement in the literature to explain high opioid use rates in the US. Nonetheless, as opioid use is associated with addiction and high morbidity and mortality [22, 23], efforts to reduce the use of this treatment, particularly for those states with greater opioid treatment rates for AS, are urgently needed.
Improvements are also necessary to reduce the use of corticosteroids for the treatment of AS, where approximately 50% of patients nationally were prescribed this treatment in 2019, with rates over 60% in certain states. Increased education needs to be provided to physicians and rheumatologists on the various effective alternative options to opioids and corticosteroids that can be used to reduce treatment-associated morbidity and mortality.
A limitation of this study was that the observed rates of AS-related diagnosis, treatment, and rheumatologist visits may be affected by geography-related factors, such as clinicians’ practice behavior, population density, distance from patients’ residences to medical centers, socioeconomic status of the area, and age distribution of the area. Therefore, the observed rates across the different geographic regions may be confounded by these factors. Additionally, uninsured patients and/or patients who did not maintain insurance coverage for an entire calendar year of interest were not reported in this study, which could lead to an underestimation of diagnostic prevalence. Lastly, race was used as a surrogate for HLA-B27 prevalence, as patient-level race data were not provided in the database. Consequently, association of race with HLA-B27 prevalence in this report should be considered with caution.
Among the strengths of this study is that it used a large, nationally representative, de-identified administrative claims database that contained commercial beneficiaries, a key population of interest for this study. Although the total population of the database decreased over time, reflecting decreasing enrollment in the plans captured by the MarketScan database, the MarketScan database remains one of the largest health care claims repositories in the US and captures diverse patient populations covered by contributing employers, hospitals, and health plans. Another strength of this study was the use of choropleth heat maps to visualize rates of diagnosis, treatment utilization, and rheumatologist visits among patients with AS in different geographic regions in the United States. With described rates of AS-related diagnosis and treatment based on geographical regions, potential gaps and target education could be more precisely identified.
Conclusions
In this retrospective study of patients diagnosed with AS in the United States, although the national diagnostic prevalence of AS steadily increased from 2014 to 2019, the low diagnostic prevalence of AS compared to the population prevalence from the NHANES study [12] suggests the disease continues to be underdiagnosed. bDMARD/tsDMARD use is gradually increasing, particularly among patients visiting a rheumatologist where 77% received this treatment in 2019. However, treatment can be improved; opioids and corticosteroids are still being used at relatively high proportions. Results from this novel study can be used to identify specific areas of improvement needed throughout the county and regionally. Observed variability in diagnostic prevalence and treatment offers the opportunity to target educational efforts to address region-specific needs and to further improve diagnosis and treatment of AS.
References
Reveille JD. Epidemiology of spondyloarthritis in North America. Am J Med Sci. 2011;341:284–6.
Magrey MN, Danve AS, Ermann J, Walsh JA. Recognizing axial spondyloarthritis: a guide for primary care. Mayo Clin Proc. 2020;95:2499–508.
Law L, Beckman Rehnman J, Deminger A, Klingberg E, Jacobsson LTH, Forsblad-d’Elia H. Factors related to health-related quality of life in ankylosing spondylitis, overall and stratified by sex. Arthritis Res Ther. 2018;20:284.
Ariza-Ariza R, Hernandez-Cruz B, Collantes E, et al. Work disability in patients with ankylosing spondylitis. J Rheumatol. 2009;36:2512–6.
Deodhar A, Mittal M, Reilly P, et al. Ankylosing spondylitis diagnosis in US patients with back pain: identifying providers involved and factors associated with rheumatology referral delay. Clin Rheumatol. 2016;35:1769–76.
Deodhar A, Mease PJ, Reveille JD, et al. Frequency of axial spondyloarthritis diagnosis among patients seen by US rheumatologists for evaluation of chronic back pain. Arthritis Rheumatol. 2016;68:1669–76.
Lapane KL, Khan S, Shridharmurthy D, et al. Primary care physician perspectives on barriers to diagnosing axial Spondyloarthritis: a qualitative study. BMC Fam Pract. 2020;21:204.
Deodhar A, Strand V, Kay J, Braun J. The term ‘non-radiographic axial spondyloarthritis’ is much more important to classify than to diagnose patients with axial spondyloarthritis. Ann Rheum Dis. 2016;75:791–4.
Wright GC, Kaine J, Deodhar A. Understanding differences between men and women with axial spondyloarthritis. Semin Arthritis Rheum. 2020;50:687–94.
Reveille JD. Biomarkers for diagnosis, monitoring of progression, and treatment responses in ankylosing spondylitis and axial spondyloarthritis. Clin Rheumatol. 2015;34:1009–18.
Reveille JD, Hirsch R, Dillon CF, Carroll MD, Weisman MH. The prevalence of HLA-B27 in the US: data from the US National Health and Nutrition Examination Survey, 2009. Arthritis Rheum. 2012;64:1407–11.
Reveille JD, Witter JP, Weisman MH. Prevalence of axial spondylarthritis in the United States: estimates from a cross-sectional survey. Arthritis Care Res (Hoboken). 2012;64:905–10.
Ward MM, Deodhar A, Gensler LS, et al. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis. Arthritis Care Res (Hoboken). 2019;71:1285–99.
Sloan VS, Sheahan A, Stark JL, Suruki RY. Opioid use in patients with ankylosing spondylitis is common in the united states: outcomes of a retrospective cohort study. J Rheumatol. 2019;46:1450–7.
IBM Watson Health. Data brochure. IBM MarketScan Research Databases for life sciences researchers. 2020. Accessed on 9 Feb 2021. Available from: https://www.ibm.com/downloads/cas/OWZWJ0QO.
Walsh J, Hunter T, Schroeder K, Sandoval D, Bolce R. Trends in diagnostic prevalence and treatment patterns of male and female ankylosing spondylitis patients in the United States, 2006–2016. BMC Rheumatol. 2019;3:39.
Bohn R, Cooney M, Deodhar A, Curtis JR, Golembesky A. Incidence and prevalence of axial spondyloarthritis: methodologic challenges and gaps in the literature. Clin Exp Rheumatol. 2018;36:263–74.
Ogdie A, Benjamin Nowell W, Reynolds R, et al. Real-world patient experience on the path to diagnosis of ankylosing spondylitis. Rheumatol Ther. 2019;6:255–67.
Fallahi S, Jamshidi AR. Diagnostic delay in ankylosing spondylitis: related factors and prognostic outcomes. Arch Rheumatol. 2016;31:24–30.
Shafrin J, Griffith J, Shim JJ, Huber C, Ganguli A, Aubry W. Geographic variation in diagnostic ability and quality of care metrics: a case study of ankylosing spondylitis and low back pain. Inquiry. 2017;54:46958017707873.
Danve A, Deodhar A. Axial spondyloarthritis in the USA: diagnostic challenges and missed opportunities. Clin Rheumatol. 2019;38:625–34.
Hser YI, Mooney LJ, Saxon AJ, et al. High mortality among patients with opioid use disorder in a large healthcare system. J Addict Med. 2017;11:315–9.
Mark TL, Parish W. Opioid medication discontinuation and risk of adverse opioid-related health care events. J Subst Abuse Treat. 2019;103:58–63.
Acknowledgements
Funding
This work was supported by AbbVie Inc. AbbVie sponsored the study, funded the Rapid Service Fee and Open Access charge, contributed to the design, participated in collection, analysis, and interpretation of data, and in writing, reviewing, approval of the final version and funded the Rapid Service Fee and Open Access Fee. No honoraria or payments were made for authorship.
Medical Writing, Editorial, and Other Assistance
Medical writing assistance was provided by Alan Saltzman, PhD, CMPP, of Fishawack Facilitate Ltd, part of Fishawack Health, Conshohocken, PA, and was funded by AbbVie Inc., North Chicago, IL.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contribution
All authors contributed to the study conception and design, material preparation, data collection, and analysis. All authors were involved in the preparation and critical review of the manuscript and read and approved the final manuscript.
Prior Presentation
Presented at the European League Against Rheumatism (EULAR) 2021 Virtual Congress, 2–5 June 2021 Poster POS0943.
Disclosures
Atul Deodhar has received consultancy fees from and participated in advisory boards for AbbVie, Amgen, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Eli Lilly, Glaxo Smith & Kline, Janssen, Novartis, Pfizer, UCB and received research grants from AbbVie, Eli Lilly, Glaxo Smith & Kline, Novartis, Pfizer, UCB. Denise Kruzikas, Ana Biljan, and Christopher Saffore are employees of AbbVie and own AbbVie stock. Lili Zhou was an employee of AbbVie at the time this study was conducted.
Compliance with Ethics Guidelines
All database records were de-identified and compliant with US patient confidentiality requirements, including the Health Insurance Portability and Accountability Act of 1996. Because of this, institutional review board approval was not required.
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Deodhar, A., Kruzikas, D., Zhou, L. et al. Geographic Variations in Diagnosis and Treatment of Ankylosing Spondylitis in the United States: A Real-World Study. Rheumatol Ther 9, 447–463 (2022). https://doi.org/10.1007/s40744-021-00406-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-021-00406-9