Abstract
Objective
To compare the effectiveness of azathioprine (AZA) and cyclosporine (CsA) as initial treatments for patients with idiopathic inflammatory myopathies (IIM).
Methods
A retrospective cohort study was conducted using information from the National Health Insurance Service database of Republic of Korea. Patients with IIM who had started AZA or CsA as initial treatment between January 2007 and December 2011 were selected for the study. They were followed from the day of treatment initiation to the occurrence of study outcomes or the end of the study until December 2016. Effectiveness outcomes, defined as switching the drug or adding immunosuppressants, and discontinuation of corticosteroids, were compared between the two groups. The Cox proportional-hazards model was used to calculate the adjusted relative risk (aRR) with 95% confidence interval (CI) between the AZA and CsA groups.
Results
A total of 376 patients with incident IIM who used AZA (n = 288) or CsA (n = 88) were identified. The aRR of switching the drug or adding immunosuppressants (1.45 [95% CI 0.99–2.11]) was not significantly different between the CsA and AZA groups. Among patients who were treated with corticosteroids at baseline, the rate of discontinuation of corticosteroids was not different between the two groups (1.69 [95% CI 0.82–3.47]).
Conclusions
The effectiveness of AZA and CsA as initial treatments for the management of IIM was comparable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Treatment strategy of idiopathic inflammatory myopathies (IIM) includes corticosteroids as the first-line therapy and additional therapy with immunosuppressive agents. However, as IIM is a rare disease associated with clinical heterogeneity, randomized controlled trials (RCTs) and real-world evidence comparing effectiveness of immunosuppressive agents are lacking. |
This study aimed to investigate the comparative effectiveness of azathioprine and cyclosporine as initial immunosuppressive agents in patients with IIM. |
What was learned from the study? |
No difference was observed between azathioprine and cyclosporine with respect to frequency of switching the drug or adding other immunosuppressants, and the rate of discontinuation of corticosteroids. |
This is the first study based on comparative effectiveness of azathioprine and cyclosporine as initial treatment in patients with IIM. This comparative effectiveness study, which is based on real-world data, would provide evidence for the selection of initial immunosuppressive therapy. |
Introduction
Idiopathic inflammatory myopathies (IIM) is a heterogeneous group of systemic inflammatory diseases characterized by chronic inflammation of the proximal muscles and involvement of multiple organs and organ systems such as the lung, skin, joints, and gastrointestinal tract. Based on muscle symptoms, skin rash, and histopathological features, IIM has been categorized into different subgroups, including dermatomyositis (DM), polymyositis (PM), and inclusion body myositis (IBM) [1]. Despite being a rare disease with prevalence from 2.3 to 33.8/100,000 persons [2, 3], many patients with IIM have high risks of mortality and morbidities, such as malignancy and circulatory or pulmonary diseases [2, 4].
Treatment strategy of IIM includes corticosteroids as the first-line therapy and additional therapy with immunosuppressive agents such as methotrexate (MTX), azathioprine (AZA), and calcineurin inhibitors, including cyclosporine-A (CsA) and tacrolimus [5,6,7]. In addition, various studies have reported the effectiveness of mycophenolate mofetil (MMF) in patients with IIM, particularly in those with interstitial lung disease (ILD) [8, 9]. In patients with severe myositis, overlapping systemic vasculitis, or disease refractory to other immunosuppressants, cyclophosphamide can be administered [10]. Among several immunosuppressants, AZA and CsA, combined with corticosteroids or MTX, have been suggested as initial immunosuppressive agents [7]. A previous randomized trial of initial treatment with AZA, combined with a corticosteroid, reported improved effectiveness compared with corticosteroid alone, with respect to tapered dose of corticosteroid for maintenance therapy and long-term physical functions in patients [11, 12]. Since calcineurin inhibitors inhibit T-cell activation and reduce activity of the gene encoding interleukin-2, CsA with corticosteroid has been shown to be effective in the treatment of patients with ILD related to IIM [13, 14], which is a highly prevalent comorbid condition in IIM [2, 15, 16]. As it is a rare disease associated with clinical heterogeneity [17], randomized controlled trials (RCTs) and real-world evidence comparing AZA and CsA as initial immunosuppressive agents in patients with IIM are lacking.
Therefore, the present study aimed to investigate the comparative effectiveness of AZA and CsA as initial immunosuppressive agents in patients with IIM and present their subsequent treatment.
Methods
Data Source
We conducted a retrospective cohort study of new users of AZA or CsA among patients with IIM, using information from the National Health Insurance Service (NHIS) database of Republic of Korea, between January 2002 and December 2016. The NHIS database covers healthcare claims for 97% of the Korean population and contains information on demographics, healthcare use, diagnoses coded using the International Classification of Diseases (ICD-10), ambulatory care, hospital admissions and visiting dates, and date of death.
Study Population
First, patients with IIM were selected based on the ICD-10 codes for juvenile DM (JDM, M33.0), DM (M33.1 or M33.9), or PM (M33.2), and Individual Copayment Beneficiaries Program (ICBP) code for IIM (V137), between January 2007 and December 2011. The Korean patients who suffer from rare diseases have been registered to the ICBP to reduce their burden of medical expenses [18]. Patients with IIM are registered in the ICBP after meeting the diagnostic criteria proposed by Bohan and Peter [19, 20], which include comprehensive clinical and laboratory findings. We categorized patients with IIM as JDM, DM, or PM according to the ICD-10 diagnostic codes registered to the ICBP. Second, we set a 2-year washout period to extract true incident cases of IIM. Patients who did not use AZA or CsA were excluded. The first date of prescription of AZA or CsA after the diagnosis of IIM was defined as the index date. Third, after selecting the first users of AZA or CsA, they were followed up from the index date to the occurrence of study outcomes, the discontinuation of the study until December 31, 2016. The persistence of the study drugs in the database was defined if the subsequent prescription was started within 30 days of the end date of the previous prescription (Fig. 1).
Study Outcomes
We set the primary endpoint for estimation of effectiveness as switching drugs or adding immunosuppressants. Switching from CsA to AZA or vice versa, and switching to other immunosuppressants such as MMF or cyclophosphamide were considered as primary endpoints, since the patient did not adequately respond to the study drug as an initial treatment. Adding immunosuppressants was defined as addition of other immunosuppressants to the initial treatment that had not been prescribed at the index date.
Discontinuation of corticosteroids was set as the secondary endpoint of our study for the patients who had been prescribed corticosteroids at the index date. Since corticosteroid could be used on an 'as-needed’ basis, we applied a permissible gap of 180 days to assess the patients who discontinued corticosteroid use completely.
We also studied safety outcomes including hospitalization (all-cause or IIM-related), emergency visits (all-cause or IIM-related), all-cause mortality, and opportunistic infections. As opportunistic infections, we included tuberculosis, deep-seated mycosis, pneumocystosis, viral infections, and retropharyngeal abscess.
Covariates
Covariates in the present study included age, sex, and type of insurance, related data of which were collected on the index date, and the history of healthcare utilization, previous medication use, and comorbidities; related data were collected for a period of 1 year prior to the index date. We collected information on individual diseases in the Elixhauser comorbidity index [21] and IIM-related comorbidities such as ILD, pneumothorax, and pneumomediastinum using diagnostic codes. The prednisolone-equivalent dose of corticosteroid per day was calculated during the first month from the index date.
Statistical Analysis
A descriptive analysis of patient demographics and clinical characteristics was performed. Comparisons of categorical and continuous variables between the two groups were conducted using the Chi-square test and Student’s t test. Crude incidence rates were calculated as the number of events per 100 person-years (PY) for each outcome. The adjusted relative risk (aRR) with 95% confidence intervals (CIs) for outcomes in the CsA group compared with those in the AZA group was calculated using the Cox proportional-hazards model adjusted for age, sex, type of IIM, history of previous medication use, and comorbidities. We used the Fine-Gray model to account for the competing risk of death [22].
Statistical significance was set at P < 0.05. Statistical analysis was performed using the SAS software (version 9.4; SAS Institute).
Compliance with Ethics Guidelines
This study protocol was reviewed by the Institutional Review Board (IRB) of Hanyang University Medical Center and was approved as ‘exempt’ from the IRB (IRB number: HYUH 2017-09-009). Informed consent was waived because the database was de-identified and opened to the public.
Results
Baseline Characteristics
We identified total 1072 patients with incident IIM between January 2007 and December 2011. Among them, a total of 376 patients received either AZA (n = 288) or CsA (n = 88) as initial immunosuppressant treatment for IIM (Fig. 2). Baseline characteristics of the study population are shown in Table 1. CsA users were younger than AZA users (mean age: 50.54 years in the AZA group vs. 42.52 years in the CsA group, P < 0.01), and the proportion of patients with DM and JDM was higher among CsA users than among AZA users (DM: 56.82 vs. 46.88% and JDM: 12.50 vs. 1.74%, respectively, P < 0.01). While the Elixhauser comorbidity score was lower in the CsA group than in the AZA group (5.99 vs. 8.27, respectively, P = 0.01), the proportion of patients with pneumomediastinum was higher among CsA users (3.41 vs. 0.35%, respectively, P = 0.04). Although the proportion of patients with ILD was numerically higher in the CsA group than in the AZA group, the difference was not statistically significant (26.14 vs. 23.26%, respectively, P = 0.58).
Furthermore, MTX was more frequently prescribed at the index date as combined treatment in CsA users than in AZA users (23.86 vs. 9.38%, respectively, P < 0.01). However, intravenous cyclophosphamide therapy at baseline did not differ between the two groups (3.41 vs. 1.39%, respectively, P = 0.14).
Comparative Effectiveness of AZA and CsA
The observation periods for the two groups were similar (mean 1.75 years in the AZA group vs. 1.42 years in the CsA group, P = 0.19). Moreover, most patients started AZA or CsA 1 month after diagnosis of IIM (median 35.5 days in the AZA group vs. 33.0 days in the CsA group, P = 0.18).
In the AZA group, 32.3% of patients switched the drug or added other immunosuppressants, compared with 54.5% patients in the CsA group. However, the aRR of switching the drug or adding immunosuppressants did not differ between the two groups (aRR 1.45; 95% CI 0.995–2.107) (Table 2). In total, 150 AZA users and 54 CsA users were prescribed corticosteroids on the index date. In the AZA group, 40.7% of patients discontinued corticosteroid, compared with 37.4% of patients in the CsA group. However, the number of cases of corticosteroid discontinuation did not differ significantly between the two groups (aRR 1.69; 95% CI 0.82–3.47) (Table 3).
The risk of all-cause hospitalization was higher among CsA users than AZA users (aRR 1.36; 95% CI 1.04–1.79). However, the risks of IM-related hospitalization, all-cause or IIM-related emergency visits, all-cause mortality, or opportunistic infections were not significantly different (Supplementary Table).
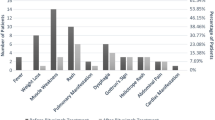
Subsequent Treatment to Initial Immunosuppressant Treatment
In the AZA group, 48.6% of the patients continued the initial treatment, compared with 31.8% in the CsA group. Among patients who did not respond to the initial treatment (n = 208), approximately 83% either switched drugs or added another immunosuppressant. Switching from AZA to CsA (16.2%) and vice versa (16.7%) were equally frequent. The frequencies of switching or adding another immunosuppressant were also similar in the two groups (83.8% in the AZA group and 83.3% in the CsA group). Intravenous cyclophosphamide was administered to 8.8% of patients in the AZA group and 11.7% in the CsA group (Fig. 2).
Discussion
Clinical practice guidelines (CPGs) proposed on the management of IIM are sparse and heterogeneous [5]. Furthermore, among 14 original CPGs identified, only half of them were evidence-based [5]. With IIM being a rare disease associated with clinical heterogeneity [17], evidence on treatment strategy for the management of patients with IIM has been lacking. In general, corticosteroids are conventionally used to induce remission in adult patients [7]. However, concomitant use of steroid-sparing immunosuppressive agents with low-dose corticosteroids might be sufficient to achieve remission induction [23]. MTX, AZA, or CsA are recommended as first-line immunosuppressive agents [7].
In the present study, based on evaluation of comparative effectiveness of AZA and CsA as initial immunosuppressants in patients with incident IIM, no difference was observed between the two treatments with respect to frequency of switching the drug or adding other immunosuppressants, and the rate of discontinuation of corticosteroids. MTX, which is one of the major immunosuppressive agents of choice to treat patients with IIM, was not included in our study because it is frequently used as a combination therapy when patients are refractory to corticosteroid therapy [24]. Nevertheless, MTX is considered as a potential immunosuppressant in the treatment of IIM [25]. Several retrospective studies have demonstrated its effectiveness against DM, PM, and JDM [26, 27]; in addition, RCTs have shown that MTX has similar efficacy to AZA [28] and CsA [29]. However, some guidelines recommend MTX for juvenile myositis only [30, 31], and due to the lack of clinical trials supporting the use of MTX in adult myositis, many patients are treated with MTX as combination therapy. In the present study, 12.8% of the study population was prescribed MTX concomitantly at the index date, and we adjusted for it. In addition, we did not include MMF as a study drug because the use of MMF for IIM treatment was not eligible for national health insurance coverage in Korea. MMF users in the database might indicate off-label use or treatment for other comorbid autoimmune diseases such as lupus.
Defining the effectiveness of the study drugs in IIM treatment using health insurance claim database is difficult; however, corticosteroid-sparing effect is a major finding defining the effectiveness of immunosuppressants such as AZA or CsA. A previous study based on comparative effectiveness of anti-tumor necrosis factor (TNF) agents in ulcerative colitis using a claim database adopted any corticosteroid prescription after initiation of the study drug as an effectiveness outcome [32]. However, the pattern of corticosteroid use in patients with IIM is diverse. Despite being the most important drug for the treatment of patients with IIM [25], some patients may not use corticosteroids during initial treatment with immunosuppressants. Therefore, we only estimated the rate of discontinuation of corticosteroid therapy combined with the study drugs as secondary outcomes in the subgroup treated with corticosteroids at baseline.
The strength of this study lies in its large population-based cohort design. To the best of our knowledge, this is the first study based on comparative effectiveness of AZA and CsA as initial treatment in patients with IIM. To date, physicians prescribe eminence-based medicine for the treatment of patients with IIM because there are no standard guidelines that cover the entire clinical and pathological spectra of IIM. In addition, the rarity of IIM makes it challenging to initiate studies including large population to evaluate the effectiveness of treatment. Therefore, we believe that this comparative effectiveness study, which is based on real-world data, would provide evidence for the selection of initial immunosuppressive therapy.
This study had several limitations. First, we defined patients with IIM using diagnostic codes without any information about clinical symptoms and autoantibodies. However, we used not only the ICD-10 code but also the ICBP registration code for myositis meeting the diagnostic criteria proposed by Bohan and Peter. Second, potential residual confounding by unmeasured IIM severity may have affected our results because information on laboratory, histological, or radiological findings was not recorded in the database. We could not perform propensity score-based analysis to address potential selection bias in this study because obtaining propensity scores with adequate balance between the two groups was not applicable. Third, we were not unable to assess improvement of clinical symptoms, such as muscle power or skin rash, due to lack of information. However, we set the primary outcomes as switching the drug or adding immunosuppressants, which might have reflected the refractory disease or intolerance to prior treatment. Fourth, we could not perform a subgroup analysis based on autoantibody profile, due to the absence of information on laboratory results in the database. Patients with IIM can be categorized into homogenous groups based on autoantibodies, which may predict treatment outcomes [33]. Moreover, we were not able to perform subgroup analyses according to DM and PM because of the small sample size of each disease.
Conclusions
In conclusion, no significant difference was observed in the effectiveness of AZA and CsA as initial treatments for IIM. Further studies using prospective study design are necessary to develop treatment guidelines for the management of IIM.
References
Dalakas MC, Hohlfeld R. Polymyositis and dermatomyositis. Lancet. 2003;362:971–82.
Cho S-K, Kim H, Myung J, et al. Incidence and prevalence of idiopathic inflammatory myopathies in Korea: a nationwide population-based study. J Korean Med Sci. 2019;34:e55.
Meyer A, Meyer N, Schaeffer M, et al. Incidence and prevalence of inflammatory myopathies: a systematic review. Rheumatology. 2014;54:50–63.
Dobloug GC, Svensson J, Lundberg IE, et al. Mortality in idiopathic inflammatory myopathy: results from a Swedish nationwide population-based cohort study. Ann Rheum Dis. 2018;77:40–7.
Meyer A, Scirè CA, Talarico R, et al. Idiopathic inflammatory myopathies: narrative review of unmet needs in clinical practice guidelines. RMD Open. 2019;4:e000784.
Kohsaka H, Mimori T, Kanda T, et al. Treatment consensus for management of polymyositis and dermatomyositis among rheumatologists, neurologists and dermatologists. Mod Rheumatol. 2019;29:1–19.
Sasaki H, Kohsaka H. Current diagnosis and treatment of polymyositis and dermatomyositis. Mod Rheumatol. 2018;28:913–21.
Saketkoo LA, Espinoza LR. Experience of mycophenolate mofetil in 10 patients with autoimmune-related interstitial lung disease demonstrates promising effects. Am J Med Sci. 2009;337:329–35.
Morganroth PA, Kreider ME, Werth VP. Mycophenolate mofetil for interstitial lung disease in dermatomyositis. Arthritis Care Res. 2010;62:1496–501.
Oddis CV, Aggarwal R. Treatment in myositis. Nat Rev Rheumatol. 2018;14:279–89.
Bunch TW. Prednisone and azathioprine for polymyositis. Long-term follow-up. Arthritis Rheum. 1981;24:45–8.
Bunch TW, Worthington JW, Combs JJ, et al. Azathioprine with prednisone for polymyositis: a controlled, clinical trial. Ann Intern Med. 1980;92:365–9.
Takada K, Kishi J, Miyasaka N. Step-up versus primary intensive approach to the treatment of interstitial pneumonia associated with dermatomyositis/polymyositis: a retrospective study. Mod Rheumatol. 2007;17:123–30.
Kotani T, Makino S, Takeuchi T, et al. Early intervention with corticosteroids and cyclosporin A and 2-hour postdose blood concentration monitoring improves the prognosis of acute/subacute interstitial pneumonia in dermatomyositis. J Rheumatol. 2008;35:254–9.
Marie I, Hatron P, Dominique S, et al. Short-term and long-term outcomes of interstitial lung disease in polymyositis and dermatomyositis: a series of 107 patients. Arthritis Rheum. 2011;63:3439–47.
Fathi M, Vikgren J, Boijsen M, et al. Interstitial lung disease in polymyositis and dermatomyositis: longitudinal evaluation by pulmonary function and radiology. Arthritis Care Res. 2008;59:677–85.
In Seol Y, Jinhyun K. The role of autoantibodies in idiopathic inflammatory myopathies. J Rheum Dis. 2019;26:165–78.
National Health Insurance Corporation HIPRI. Research report on health care utilization of patients with rare and intractable disorder and improvement of individual copayment beneficiaries program for rare and intractable disorder (in Korean). 2010. https://www.nhis.or.kr/static/html/wbd/g/a/wbdga0405.html.
Bohan A, Peter JB. Polymyositis and dermatomyositis (first of two parts). N Engl J Med. 1975;292:344–7.
Bohan A, Peter JB. Polymyositis and dermatomyositis (second of two parts). N Engl J Med. 1975;292:403–7.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Nzeusseu A, Brion F, Lefèbvre C, et al. Functional outcome of myositis patients: can a low-dose glucocorticoid regimen achieve good functional results? Clin Exp Rheumatol. 1999;17:441–6.
Villalba L, Hicks JE, Adams EM, et al. Treatment of refractory myositis: a randomized crossover study of two new cytotoxic regimens. Arthritis Rheum. 1998;41:392–9.
Oddis CV. Update on the pharmacological treatment of adult myositis. J Intern Med. 2016;280:63–74.
Newman ED, Scott DW. The use of low-dose oral methotrexate in the treatment of polymyositis and dermatomyositis. J Clin Rheumatol. 1995;1:99–102.
Miller LC, Sisson BA, Tucker LB, et al. Methotrexate treatment of recalcitrant childhood dermatomyositis. Arthritis Rheum. 1992;35:1143–9.
Miller J, Walsh Y, Saminaden S, et al., editors. Randomised double blind trial of methotrexate and steroids compared with azathioprine and steriods in the treatment of idiopathic inflammatory myopathy. J Neurol Sci. 2002: Elsevier Science BV, Amsterdam.
Vencovsky J. Cyclosporine A versus methotrexate in the treatment of polymyositis and dermatomyositis. Scand J Rheumatol. 2000;29:95–102.
Sunderkötter C, Nast A, Worm M, et al. Guidelines on dermatomyositis—excerpt from the interdisciplinary S2k guidelines on myositis syndromes by the German Society of Neurology. JDDG Journal der Deutschen Dermatologischen Gesellschaft. 2016;14:321–38.
Bellutti Enders F, Bader-Meunier B, Baildam E, et al. Consensus-based recommendations for the management of juvenile dermatomyositis. Ann Rheum Dis. 2017;76:329–40.
Singh S, Heien HC, Sangaralingham LR, et al. Comparative effectiveness and safety of infliximab and adalimumab in patients with ulcerative colitis. Aliment Pharmacol Ther. 2016;43:994–1003.
Argolini LM, Frontini G, Elefante E, et al. Multicentric study comparing cyclosporine, mycophenolate mofetil and azathioprine in the maintenance therapy of lupus nephritis: 8 years follow up. J Nephrol. 2021;34(2):389–98. https://doi.org/10.1007/s40620-020-00753-w.
Acknowledgements
We would like to thank Editage (http://www.editage.co.kr) for English language editing.
Funding
This research and the journal’s Rapid Service Fee were supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2021R1A6A1A03038899). This work was supported by the research fund of Hanyang University (HY-202000000003326).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by HK, EJC and EJJ. The first draft of the manuscript was written by S-YJ and Y-KS, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Please amend to: Sun-Young Jung, Yoon-Kyoung Sung, Hyoungyoung Kim, Eom Ji Cha, Eun Jin Jang, Dae-Hyun Yoo, Soo-Kyung Cho have nothing to disclose.
Compliance with Ethics Guidelines
This study protocol was reviewed by the Institutional Review Board (IRB) of Hanyang University Medical Center and was approved as ‘exempt’ from the IRB (IRB number: HYUH 2017-09-009). Informed consent was waived because the database was de-identified and opened to the public.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jung, SY., Sung, YK., Kim, H. et al. Comparative Effectiveness of Azathioprine Versus Cyclosporine as an Initial Treatment for Idiopathic Inflammatory Myopathies: A Population-Based Observational Study. Rheumatol Ther 9, 139–149 (2022). https://doi.org/10.1007/s40744-021-00392-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-021-00392-y