Abstract
Introduction
Golimumab is a human monoclonal antibody that inhibits tumor necrosis factor-α (TNF-α). Inhibition of TNF-α by golimumab inhibits the inflammatory response, thereby modulating the immune response in immune-mediated inflammatory diseases. Although the efficacy of golimumab has been demonstrated in randomized controlled trials (RCTs), various patient populations, such as those at high risk of infection, including those with latent tuberculosis and various comorbidities, or on co-administered medications, were excluded from the RCTs. Therefore, safety cannot be sufficiently evaluated by RCTs in the patient group with heterogenous characteristics. The aim of this study was to assess the safety and effectiveness of golimumab in patients with rheumatoid arthritis (RA), psoriatic arthritis (PsA), and ankylosing spondyloarthritis (AS) in a real-world setting in Korea.
Methods
We conducted an open-label, prospective, non-interventional study as post-marketing surveillance. Safety was evaluated by collecting and recording adverse events, and effectiveness was evaluated by assessing disease activity using DAS28-CRP, DAS28-ESR, ACR20, and ASAS20 outcome measures. Multiple logistic regression was performed to identify factors associated with the incidence of adverse events, and changes in disease activity scores from baseline were analyzed using the Wilcoxon signed-rank test.
Results
A total 673 patients were enrolled, of whom 621 were included in the safety analysis. During the study, 97 adverse drug reactions (ADRs) were reported in 62 patients (10.0%). The most frequently reported ADRs were related to infection, including nasopharyngitis (0.8%), upper respiratory tract infection (0.6%), and herpes zoster (0.5%). The mean (± standard deviation) changes from baseline in global disease activity at weeks 12 and 24 were − 3.37 ± 2.529 and − 3.68 ± 2.404, respectively, with statistical significance. In those patients with RA, 72.5 and 47.0% of individuals had a good response based on DAS28-CRP and DAS28-ESR outcomes at week 24. At week 24, 71.4% of patients with PsA had an ACR20 response and 72.9% of patients with AS had an ASAS20 response.
Conclusion
In the real-world setting, golimumab was safe and effective in Korean patients with RA, PsA, and AS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Although golimumab has been approved through randomized controlled trials, there is a necessity to evaluate safety because of heterogenous patients’ characteristics in real clinical practice. |
Post-marketing surveillance (PMS) is a prospective observational study design that can be used to investigate the safety and effectiveness in real-world clinical settings in Korea. |
What was learned from the study? |
Golimumab had an acceptable safety profile in the real-world clinical setting in Korea. |
Golimumab had a favorable effectiveness profile in lowering disease activity of rheumatoid arthritis, psoriatic arthritis, and ankylosing spondyloarthritis. |
Introduction
Key Summary Points:
Why carry out this study?
Golimumab, a human monoclonal antibody, inhibits tumor necrosis factor-alpha (TNF-α). It binds with high affinity to both the soluble and membrane-bound forms of TNF-α, creating stable complexes and preventing TNF-α from binding to its receptors [1, 2]. TNF-α promotes an inflammatory response, and abnormally high levels of TNF-α have been observed in several immune-mediated inflammatory diseases, such as rheumatoid arthritis (RA), psoriatic arthritis (PsA), and spondyloarthritis, including ankylosing spondylitis (AS) [3,4,5,6,7]. Inhibition of TNF-α by golimumab inhibits downstream signaling cascades of excessive inflammatory response and consequently modulates the immune response in these immune-mediated inflammatory diseases.
Several randomized controlled trials (RCTs) hav demonstrated the efficacy of golimumab in reducing disease activity, preventing radiologic progression, and improving physical function, with a favorable safety profile [8,9,10,11,12,13]. In Korea, golimumab has been approved since 2012 to treat patients with moderate-to-severe RA, active PsA, or axial spondyloarthritis who have not responded adequately to conventional therapy. Because of the exclusion of various patient populations at high risk of infection, including those with latent tuberculosis and various comorbidities, or those with co-administered medications in the pivotal RCTs, the prospective observational study presented here was conducted as post-marketing surveillance (PMS) with the aim to investigate the safety and effectiveness of golimumab in real-world clinical settings in Korea.
Methods
Study Design and Patients
This study was a prospective, multi-center, open-label, non-interventional study conducted in Korea. Patients eligible for inclusion were aged ≥ 18 years, had received golimumab for the treatment of moderate-to-severe active RA, active PsA, or and moderate-to-severe active AS, and had experienced inadequate response to conventional therapies, such as disease-modifying antirheumatic drugs (DMARDs) for RA/PsA and non-steroidal anti-inflammatory drugs (NSAIDs) for AS. Patients who had severe active infections, opportunistic infections, or moderate-to-severe renal insufficiencies were excluded based on the locally approved label. The dosage of golimumab administered was in accordance to the label for each disease. Patients were observed for up to 24 weeks, with an additional 4 weeks for the safety follow-up, after the last dose of golimumab.
The study protocol, including all ethical aspects, was reviewed and approved by the institutional review board of each participating medical institution (see Electronic Supplementary Material 1). All patients provided written informed consent to participate and have their data collected. This study was approved by the Korean Ministry of Food and Drug Safety and was conducted under the Korean regulation for re-examination of new drugs and the Declaration of Helsinki 1964 and its later amendments.
Measurements
This study collected data to evaluate the safety and effectiveness of golimumab, including its administration. Demographic data, including patients’ age, sex, height, and weight, were collected. In addition, the date of diagnosis, duration of disease, medical history of rheumatic and other diseases, and accompanying functional impairment of the liver or kidney were recorded. Regarding the administration status of golimumab, data on the indication, daily dose, administration date, and dose change (along with the reason) were collected.
Safety
Safety assessment was performed by examining the incidence of any adverse events (AEs) and serious adverse events (SAEs) in terms of their severity and association with golimumab. The severity of AEs was categorized into three levels: “mild,” “moderate,” or “severe.” The causal relationship with golimumab was categorized by participating physicians as: “certain,” “probable/likely,” “possible,” “unlikely,” “conditional/unclassified,” and “unassessable/unclassifiable.” Adverse drug reactions (ADRs) were defined as all AEs except those for which the causal relationship was classified as “unlikely.” All AEs collected were coded according to System Organ Class (SOC) using the Medical Dictionary for Regulatory Activities (MedDRA).
Effectiveness
Effectiveness was assessed using both global assessment and disease-specific evaluations at each visit. Global assessment for disease activity was performed by the patients themselves using a 0− to 10-point Visual Analogue Scale (VAS). The effectiveness of golimumab in RA was evaluated using the Disease Activity Score 28-joint counts (DAS28), which was calculated separately using both C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) as variables [14, 15]. The treatment response was classified in accordance with The European League Against Rheumatism (EULAR) criteria [16]. The effectiveness of golimumab in PsA was evaluated based on the proportion of patients achieving ≥ 20% improvement from baseline per the American College of Rheumatology (ACR) response (ACR20) criteria [14]. The disease-specific endpoint for AS was the proportion of patients who achieved an improvement of ≥ 20% from baseline according to the Assessment of SpondyloArthritis International Society (ASAS20) criteria [17].
Statistical Analyses
The safety set (SS) was defined as the patients who had received at least one dose of golimumab and had completed the safety follow-up; patients were excluded from the SS if they previously received golimumab monotherapy for RA, did not receive treatment for latent tuberculosis infection (LTBI), did not provide informed consent, were foreign patients who did not qualify for statutory health coverage, or had been treated with golimumab before the start of this study. The effectiveness set (ES) included patients in the SS group who were evaluated for effectiveness at least once.
Descriptive statistics for continuous variables were presented as means ± standard deviation (SD), and dichotomous variables were presented as frequencies with percentages in parentheses. AEs were summarized in terms of the number of patients (with percentages). In addition, multiple logistic regression was performed to determine the clinical predictors (sex, age, hepatic impairment, renal impairment, golimumab formulation, golimumab indication, comorbidity, and prior treatment) for AE incidence. Change in the global VAS score from baseline by each patient to each time point was analyzed using the Wilcoxon signed-rank test. The number of patients who experienced a response to treatment for each disease was analyzed based on the available results at each visit. All statistical tests were performed using two-sided tests, and p values < 0.05 were considered to be statistically significant. All analyses were performed using the statistical software package SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
Demographics and Baseline Characteristics
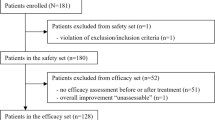
A total of 673 patients were enrolled between August 2012 and August 2018, of whom 621 patients were ultimately included in the SS group analyzed for safety assessments and 52 were excluded due to uncertainty regarding whether the safety assessments were appropriate for golimumab off-label cases (Fig. 1). Of the 621 patients included in the SS group, 201 had RA, 14 had PsA, and 406 had AS; the baseline characteristics of these patients are given in Table 1. Among the SS group, 192 patients were excluded from the effectiveness evaluation due to missing effectiveness outcomes and early discontinuation of the study (< 24 weeks) (Fig. 1).
In the SS group, the mean (± SD) age of patients was 44.0 ± 13.9 years, and 57.3% of patients were male. More than half of the patients (65.4%) were treated with golimumab for AS and 32.4% were treated with golimumab for RA. Prior to golimumab treatment, most patients (97.4%) were treated with DMARDs, NSAIDs, and/or steroids, and a few patients (2.3%) underwent surgical treatment, such as hip arthroplasty, for their rheumatic disease. In addition, 20.3% of patients were previously exposed to other biologics, mainly TNF inhibitors (adalimumab, infliximab, etanercept); most of these patients discontinued these agents due to lack of effectiveness. There were 330 patients (53.1%) in the SS group with comorbidities, such as hypertension, hyperlipidemia, osteoporosis, gastroesophageal reflux disease, and uveitis. All enrolled patients were screened for latent tuberculosis using a tuberculin test, and 103 patients (16.6%) with latent tuberculosis had prophylactic treatment prior to initiation of golimumab.
Safety
A total of 265 AEs were reported in 162 patients (26.1%) and 97 ADRs in 62 patients (10.0%). Unexpected AEs (n = 170 events) were reported in 110 patients (17.7%) and 14 SAEs including death were reported in 11 patients (1.8%) (Table 2). The most frequently reported ADRs were related to infection and infestations (3.1%). Among the infection and infestation ADRs, nasopharyngitis (0.8%) was the most frequently reported, followed by upper respiratory tract infections (0.6%) and herpes zoster (0.5%). Other than infection, pruritus (1.3%) was the most common ADR, followed by elevated alanine aminotransferase level (0.6%), rash, arthralgia, back pain, injection site rash, and elevated aspartate aminotransferase level (0.5% each). One case of death by cardiac arrest was reported in one patient with a history of dyslipidemia, hypertension, arrhythmia, and osteoporosis; this death was judged to be without causality to golimumab.
Seven patients had a reported history of tuberculosis prior to golimumab initiation; of these, three had tuberculosis, three had pulmonary tuberculosis, and one had lymph node tuberculosis. However, there was no worsening of tuberculosis reported during the study. There were 103 patients with latent tuberculosis at baseline, and all of them received tuberculosis prophylaxis prior to golimumab initiation according to the Korean Guidelines for Tuberculosis [18]. There was no activation of tuberculosis in these patients throughout the study period.
To explore if there was any association between patient demographics and clinical features and the incidence of AEs during the study, we performed a multiple logistic regression analysis (Table 3). This analysis showed that patients with uveitis had 3.29-fold higher odds (95% confidence interval 1.397, 7.762) of experiencing an AE than those without uveitis (p = 0.090).
Effectiveness
The mean change (± SD) in VAS scores, which indicates patients’ global disease activity from baseline at week 12 (n = 366) and week 24 (n = 295), were − 3.37 ± 2.529 and − 3.68 ± 2.404, respectively, showing a statistically significant reduction (p < 0.0001) (Table 4).
In the effectiveness assessment for RA, the proportion of patients with good response in DAS28-CRP and DAS28-ESR were 48.1% (n = 37/77) and 36.1% (n = 26/72), respectively, at week 12. At week 24, the proportions of patients with good response in DAS28-CRP and DAS28-ESR were 72.5% (n = 58/80) and 47.0% (n = 39/83), respectively (Fig. 2a).
In the effectiveness assessment for PsA, the ACR20 responder rate was 66.7% (n = 4/6) and 71.4% (5/7) at weeks 12 and 24, respectively (Fig. 2b). For AS patients, the ASAS20 responder rates were 68.6% (n = 118/172) and 79.2% (n = 118/149) at weeks 12 and 24, respectively (Fig. 2c).
Percentage of responders to therapy by disease specific index. aThe response is categorized by EULAR classification using the DAS28 score with CRP or ESR. Good refers to responders (patients) with an improvement of > 1.2 and a present score of ≤ 3.2; Moderate refers to responders with an improvement of > 0.6 to ≤ 1.2 and a present score of ≤ 5.1, or an improvement of > 1.2 and a present score of >3.2; No refers to non-responders, i.e., any patient with an improvement of ≤ 0.6, or a patient with an improvement of > 0.6 to ≤ 1.2 and a present score of > 5.1. b Response measured with the ACR20. A responder is defined as a patient who showed an improvement of ≥ 20% from baseline in swollen joint count, tender joint count, and ≥ 3 of patient’s pain assessment, patient global assessment of disease activity, physician’s global assessment of disease activity, health assessment questionnaire, and CRP. c Response measured with the ASAS20. A responder is defined as a patient who had an improvement of ≥ 20% from baseline and absolute improvement to 0/1 score in at least 3 global assessments: total back pain, bath ankylosing spondylitis functional index, and inflammation. ACR20 Composite measure indicating 20% improvement from baseline per the American College of Rheumatology (ACR) response criteria, ASAS20 Improvement of ≥ 20% from baseline according to the Assessment of SpondyloArthritis International Society (ASAS) criteria, DAS28-CRP, -ESR Disease Activity Score 28-joint counts calculated separately using both C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) as variables
Discussion
In this study, we evaluated the safety and effectiveness of golimumab treatment using the locally approved label in Korea.
The composition of the patient population in our study is consistent with that reported in previous observational studies conducted in Korea [19, 20]. Our study shows that RA occurs at a relatively old age, similar to findings from Japan [21,22,23,24]. In comparison, the mean age of patients with AS in our study was 39.1 years, which was considerably younger than that of the RA patients (53.3 years). This finding is similar to that of other studies which also confirmed that AS patients are relatively younger. [25, 26]
Most of the patients included in our study had previous experience with conventional treatments due to the Korean reimbursement guidelines which allows biologic treatment only after evidence of intolerance or failure of conventional treatments.
Since this study included only patients who were treated with methotrexate (MTX) used in combination with golimumab, the safety and effectiveness of golimumab monotherapy in real-world practice remains unconfirmed. In accordance with the results of PMS studies conducted in Japanese patients with RA, the incidence of SAEs among our study population was significantly lower in patients who were treated only with MTX compared to patients receiving golimumab or adalimumab monotherapy. However, these PMS studies were conducted in Japan at a time when the maximum approved MTX dose for RA was 8 mg/week, which could have contributed to lower numbers of reported SAEs [23, 24]. The authors of these studies interpreted this result in the golimumab and adalimumab monotherapy groups to be due to older age and longer disease duration, which would increase the risk for SAEs. In a meta-analysis, there were higher discontinuation rates among patients receiving combination therapy with golimumab + MTX, due to AEs, than among those receiving MTX monotherapy, but the difference was not statistically significant [27]. Based on this result, it would appear that MTX is more likely to be tolerated, but there is no clear evidence that the golimumab + MTX combination increases the risk of AEs.
In one of the above-mentioned Japanese study [24], there was no significant difference in the incidence of total ADRs between patients receiving 50 or 100 mg of golimumab with concomitant use of MTX and those receiving 50 or 100 mg of GLM monotherapy (4 groups of patients categorized according to treatment). The incidence of ADRs in the present study (10.0%) was similar to that of this Japanese study for golimumab (15.03%), Therefore, the use of golimumab and MTX in combination within the local approved label should be considered without major safety concerns.
The regression analysis of factors that could affect safety demonstrated that there was no significant effect of patient’s age, previous treatment history, golimumab formulation, indication, and prior treatments. However, the odds of AEs were higher in patients with uveitis than those without uveitis. Uveitis is the most common, clinically important extra-articular manifestation of AS [28], and all except one patient with uveitis reported in this study were patients with AS. The higher rate of AEs reported in patients with uveitis in this study led to a significant result in the regression analysis. However, this result is simply based on the frequency of reported AEs, and it has not been confirmed whether the reported AEs are clearly related to golimumab. These results can be attributed to the fact that the overall health condition of patients with uveitis is generally worse, taking into account the use of different concomitant medications. Therefore, we suggest that this result indicates the need for further studies to evaluate the risk of golimumab in AS patients with uveitis.
There was no malignancy reported with and after treatment using golimumab. There is a recent database study confirming that anti-TNF therapy is a safe therapeutic option in Korea [29]. However, the duration of the follow-up period of our study was insufficient to observe the onset of cancer; we therefore suggest that further studies are required to identify the risk of malignancy.
It has been reported that anti-TNFs increase the risk of reactivation of LTBI [30, 31]. Tuberculosis in Korea remains an important health problem, with a prevalence 49.4 per 100,000 people [32]. This study included seven patients who had a history of tuberculosis, but these patients did not exhibit tuberculosis reactivation. In addition, when latent tuberculosis was confirmed at baseline, appropriate chemoprophylactic treatment was administered and there were no cases of active tuberculosis during the study. Therefore, although golimumab belongs to the anti-TNF drug class, the risk of tuberculosis reactivation or infection can be reduced through proper screening for tuberculosis and patient monitoring while on golimumab treatment.
In this study, significant changes in global disease activity assessment were observed after golimumab treatment. In a disease-specific assessment, > 90% of RA patients had a moderate or good response, and treatment responder rate of PsA or AS also reached > 70%.
One limitation of this study is that there was no control group with which to directly compare the safety and effectiveness to golimumab. A second limitation is that this study had relatively short follow-up period, which limited observation of AEs which have a longer latency, such as malignancy.
Conclusions
In conclusion, the results of this study demonstrate that golimumab has favorable safety and effectiveness profiles for the treatment of RA, PsA, and AS in Korea. We suggest that golimumab can be considered as an appropriate drug to control disease activity since it demonstrated significant disease activity-lowering effects in this study population.
References
Rossini M, De Vita S, Ferri C, et al. Golimumab: a novel anti-tumor necrosis factor. Biol Ther. 2013;3:83–107.
Zidi I, Bouaziz A, Mnif W, Bartegi A, Al-Hizab FA, Amor NB. Golimumab therapy of rheumatoid arthritis: an overview. Scand J Immunol. 2010;72:75–85.
Gratacós J, Collado A, Filella X, et al. Serum cytokines (IL-6, TNF-alpha, IL-1 beta and IFN-gamma) in ankylosing spondylitis: a close correlation between serum IL-6 and disease activity and severity. Br J Rheumatol. 1994;33:927–31.
Lange U, Teichmann J, Stracke H. Correlation between plasma TNF-alpha, IGF-1, biochemical markers of bone metabolism, markers of inflammation/disease activity, and clinical manifestations in ankylosing spondylitis. Eur J Med Res. 2000;5:507–11.
Partsch G, Steiner G, Leeb BF, Dunky A, Bröll H, Smolen JS. Highly increased levels of tumor necrosis factor-alpha and other proinflammatory cytokines in psoriatic arthritis synovial fluid. J Rheumatol. 1997;24:518–23.
Ritchlin C, Haas-Smith SA, Hicks D, Cappuccio J, Osterland CK, Looney RJ. Patterns of cytokine production in psoriatic synovium. J Rheumatol. 1998;25:1544–52.
Grossman JM, Brahn E. Rheumatoid arthritis: current clinical and research directions. J Womens Health. 1997;6:627–38.
Keystone EC, Genovese MC, Klareskog L, et al. Golimumab, a human antibody to tumour necrosis factor alpha given by monthly subcutaneous injections, in active rheumatoid arthritis despite methotrexate therapy: the GO-FORWARD Study. Ann Rheum Dis. 2009;68:789–96.
Smolen JS, Kay J, Doyle MK, et al. Golimumab in patients with active rheumatoid arthritis after treatment with tumour necrosis factor alpha inhibitors (GO-AFTER study): a multicentre, randomised, double-blind, placebo-controlled, phase III trial. Lancet. 2009;374:210–21.
Weinblatt ME, Bingham CO 3rd, Mendelsohn AM, et al. Intravenous golimumab is effective in patients with active rheumatoid arthritis despite methotrexate therapy with responses as early as week 2: results of the phase 3, randomised, multicentre, double-blind, placebo-controlled GO-FURTHER trial. Ann Rheum Dis. 2013;72:381–9.
Emery P, Fleischmann RM, Moreland LW, et al. Golimumab, a human anti-tumor necrosis factor alpha monoclonal antibody, injected subcutaneously every four weeks in methotrexate-naive patients with active rheumatoid arthritis: twenty-four-week results of a phase III, multicenter, randomized, double-blind, placebo-controlled study of golimumab before methotrexate as first-line therapy for early-onset rheumatoid arthritis. Arthritis Rheum. 2009;60:2272–83.
Kavanaugh A, McInnes IB, Mease P, et al. Clinical efficacy, radiographic and safety findings through 5 years of subcutaneous golimumab treatment in patients with active psoriatic arthritis: results from a long-term extension of a randomised, placebo-controlled trial (the GO-REVEAL study). Ann Rheum Dis. 2014;73:1689–94.
Inman RD, Davis JC Jr, Heijde D, et al. Efficacy and safety of golimumab in patients with ankylosing spondylitis: results of a randomized, double-blind, placebo-controlled, phase III trial. Arthritis Rheum. 2008;58:3402–12.
Felson DT, Anderson JJ, Boers M, et al. American College of Rheumatology. Preliminary definition of improvement in rheumatoid arthritis. Arthritis Rheum. 1995;38:727–35.
Prevoo ML, van 't Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38:44–48.
van Gestel AM, Prevoo ML, van 't Hof MA, van Rijswijk MH, van de Putte LB, van Riel PL. Development and validation of the European League Against Rheumatism response criteria for rheumatoid arthritis. Comparison with the preliminary American College of Rheumatology and the World Health Organization/International League Against Rheumatism criteria. Arthritis Rheum. 1996;39:34–40.
Anderson JJ, Baron G, van der Heijde D, Felson DT, Dougados M. Ankylosing spondylitis assessment group preliminary definition of short-term improvement in ankylosing spondylitis. Arthritis Rheum. 2001;44:1876–86.
Joint Committee for the Revision of Korean Guidelines for Tuberculosis. Korean guidelines for tuberculosis, 2nd edn. 2014.
Sung YK, Cho SK, Choi CB, Bae SC. Prevalence and incidence of rheumatoid arthritis in South Korea. Rheumatol Int. 2013;33:1525–32.
Won S, Cho SK, Kim D, et al. Update on the prevalence and incidence of rheumatoid arthritis in Korea and an analysis of medical care and drug utilization. Rheumatol Int. 2018;38:649–56.
Schiff MH, Burmester GR, Kent JD, et al. Safety analyses of adalimumab (HUMIRA) in global clinical trials and US postmarketing surveillance of patients with rheumatoid arthritis. Ann Rheum Dis. 2006;65:889–94.
Soliman MM, Hyrich KL, Lunt M, Watson KD, Symmons DPM, Ashcroft DM. Effectiveness of rituximab in patients with rheumatoid arthritis: observational study from the British Society for Rheumatology Biologics Register. J Rheumatol. 2012;39:240–6.
Koike T, Harigai M, Ishiguro N, et al. Safety and effectiveness of adalimumab in Japanese rheumatoid arthritis patients: postmarketing surveillance report of 7740 patients. Mod Rheumatol. 2014;24:390–8.
Kanbori M, Suzuka H, Yajima T, et al. Postmarketing surveillance evaluating the safety and effectiveness of golimumab in Japanese patients with rheumatoid arthritis. Mod Rheumatol. 2018;28:66–75.
Park J-S, Hong J-Y, Park Y-S, Han K, Suh S-W. Trends in the prevalence and incidence of ankylosing spondylitis in South Korea, 2010–2015 and estimated differences according to income status. Sci Rep. 2018;8:7694.
Jeong H, Yoon JY, Park E-J, et al. Clinical characteristics of nonradiographic axial spondyloarthritis in Korea: a comparison with ankylosing spondylitis. Int J Rheum Dis. 2015;18:661–8.
Hazlewood GS, Barnabe C, Tomlinson G, Marshall D, Devoe D, Bombardier C. Methotrexate monotherapy and methotrexate combination therapy with traditional and biologic disease modifying antirheumatic drugs for rheumatoid arthritis: abridged Cochrane systematic review and network meta-analysis. BMJ. 2016;353:i1777.
Rosenbaum J, Chandran V. Management of comorbidities in ankylosing spondylitis. Am J Med Sci. 2012;343(5):364–6.
Jung SM, Kwok S-K, Ju JH, Park Y-B, Park S-H. Risk of malignancy in patients with rheumatoid arthritis after anti-tumor necrosis factor therapy: results from Korean National Health Insurance claims data. Korean J Intern Med. 2019;34:669–77.
Minozzi S, Bonovas S, Lytras T, et al. Risk of infections using anti-TNF agents in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis: a systematic review and meta-analysis. Expert Opin Drug Saf. 2016;15:11–34.
Cantini F, Niccoli L, Goletti D. Adalimumab, etanercept, infliximab, and the risk of tuberculosis: data from clinical trials, national registries, and postmarketing surveillance. J Rheumatol. 2014;91:47–55.
Korea Disease Control and Prevention Agency. Annual report of tuberculosis patients in Korea. 2020. http://www.kdca.go.kr/npt/biz/npp/portal/nppPblctDtaMain.do. Accessed 31 May 2021.
Acknowledgements
We appreciate the contribution of all physicians, medical institutions, and patients who participated in this study.
Funding
This study was designed, managed and funded by Janssen Korea Ltd. All fees relating to publication and journal’s Rapid Service Fee were also funded by Janssen Korea Ltd.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contributions
All authors contributed to the study conception and design. Material preparation and data collection and analysis were performed by Hyeongyeong Kim, Youngdoe Kim and YoungJa Lee. The first draft of the manuscript was written by Hyeongyeong Kim, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosures
Hyeongyeong Kim, Youngdoe Kim, and YoungJa Lee are full-time employees of Janssen Korea Ltd.
Compliance with Ethics Guidelines
The study was conducted according to the Declaration of Helsinki 1964 and its later amendments. The study protocol, including all ethical aspects, was reviewed and approved by the institutional review board of each participating medical institution (Electronic Supplementary Material 1). All patients provided written informed consent to participate and have their data collected.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due to privacy and ethical restrictions.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kim, H., Kim, Y. & Lee, Y. Real-World Safety and Effectiveness of Golimumab in Rheumatic Diseases: Post-Marketing Surveillance in Korea. Rheumatol Ther 8, 1393–1404 (2021). https://doi.org/10.1007/s40744-021-00352-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-021-00352-6