Abstract
Introduction
It is unclear whether polymyalgia rheumatica (PMR) should be considered an inflammatory disease or an autoimmune disease.
Methods
Eighteen untreated early PMR patients and 18 sex- and age-matched healthy controls (HCs) were included. PMR patients received tocilizumab from week 0 to week 12 and glucocorticoids from week 12 to week 24. Leukocytes, neutrophils, platelets, hemoglobin, γ-globulins, IgG, IgA, and IgM were compared between the PMR patients and HCs and before and after tocilizumab treatment in the PMR group.
Results
The mean age was 68 ± 7 and 66 ± 11 years, and the mean serum C-reactive protein level was 82 ± 16 and 5 ± 2 mg/l for PMR patients and HCs, respectively. At inclusion, leukocytes (p < 0.0001), neutrophils (p < 0.0001), and platelets (p < 0.0001) were increased and hemoglobin (p < 0.0001) decreased in the PMR group compared to the HC group. After tocilizumab therapy, leukocytes, neutrophils, and platelets decreased, and hemoglobin increased. At inclusion, all four parameters were significantly associated with the serum IL-6 level, though it was not associated after tocilizumab therapy. Levels of γ-globulin were increased in the PMR patients compared to HCs (p = 0.0087), and PMR patients with γ-globulins levels over 11 g/l at inclusion responded more quickly to tocilizumab therapy. Autoantibody profiles did not differ between the PMR patients and HCs.
Conclusions
This study suggests that PMR is more an inflammatory disease than an autoimmune disease. Tocilizumab improves all markers of inflammation. Patients with elevated γ-globulins respond more quickly to tocilizumab.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Whole blood count is affected by inflammation in polymyalgia rheumatica. |
Tocilizumab quickly improves all markers of inflammation in polymyalgia rheumatica patients. |
The association between IL-6 and blood count is no longer observed after tocilizumab therapy. |
Gamma globulins over 11 g/l predict a quick response to tocilizumab in early polymyalgia rheumatica. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14170013.
Introduction
Polymyalgia rheumatica (PMR) is a common cause of arthralgia in elderly patients. PMR occurs after 50 years of age and is responsible for pain in the shoulder girdle and the pelvic girdle. A main characteristic of PMR is an increase in acute-phase reactants (APRs), namely, C-reactive protein and the erythrocyte sedimentation rate. PMR may be associated with giant cell arteritis (GCA) but occur most often isolated [1]. Glucocorticoids remain the cornerstone of treatment for PMR. Although methotrexate has been studied as a glucocorticoid-sparing agent (GSA), the data are controversial [2].
It is unclear if PMR is an autoinflammatory or an autoimmune condition [3]. Inflammation is the main pathogenic mechanism identified in PMR, e.g., interleukin (IL)-6 is strongly increased in these patients [4]; monocytes are probably involved [5] but are not responsible for IL-6 secretion. However, disruptions in the adaptive immune system T cells [6] and B cells [4, 7] have also been described. Despite the description of anti-ferritin auto-antibodies in PMR and GCA, no specific autoantibody screening assay is currently used [8]. Recently, leukocyte dynamics have been studied in early PMR and GCA, and a myeloid shift was observed in untreated patients [9], sustaining the hypothesis of a prevailing inflammatory mechanism.
In this context of strong inflammation, the blockade of IL-6 is a promising track. Tocilizumab, a monoclonal antibody targeting the IL-6 receptor, is known for its strong anti-inflammatory effects and is currently being studied in the cytokine storms generated by SARS-CoV2 infection [10], and recently, tocilizumab has demonstrated efficacy in early PMR [11]. Nonetheless, several studies are ongoing to evaluate the use of tocilizumab in PMR as an induction treatment or as a GSA [12, 13]. The understanding of the pharmacodynamic of tocilizumab is crucial to enable a proper use of this therapy in PMR patients, but data about the pharmacodynamic effects of tocilizumab are scarce.
Our aim was to describe the pharmacodynamic effect of tocilizumab on inflammatory markers in a well-characterized population of PMR patients and to identify markers to optimize the use of tocilizumab.
Methods
First, we aimed to describe the inflammatory and autoimmune characteristics of a well-defined population of untreated early PMR patients. Then, we aimed to observe their evolution under tocilizumab therapy. We first analyzed the whole blood of PMR patients to determine whether modifications are overall caused by inflammation that specifically affects the lymphoid compartment. Next, we evaluated γ-globulins, as hypergammaglobulinemia is often associated with autoimmune disease and inflammation, and we searched for a specific decrease in immunoglobulin isotypes. Finally, we searched for marks of autoimmunity with a large panel of autoantibodies to determine whether autoimmunity is pronounced in PMR patients.
Patients
Data for PMR patients included in the TENOR study [11] were used in the present study. Chuang’s criteria for PMR were applied and fulfilled. GCA was excluded using 18-fluorodesoxyglucose positron emission tomography. The patients received three intravenous infusions of tocilizumab at visit (V) 0 (week 0), V3 (week 4) and V4 (week 8); from V5 (week 12), the patients received glucocorticoids until V8 (week 24). Glucocorticoids were administered as a decreasing oral and daily dose, starting at 0.15 mg/kg/day at V5 (week 12). Glucocorticoids were decreased by 1 mg every 2 weeks if PMR activity score was under 10. As previously reported, all patients responded to tocilizumab therapy at V5 and V8 according to the PMR activity score [14].
Healthy Controls
Age- and sex-matched healthy controls (HCs) were recruited from the Rheumatology Department of Brest University Hospital (CHRU Cavale-Blanche). The HCs had no infection, no active neoplastic affection, and no autoimmune disease. Moreover, they had no increase in APRs, and all HCs gave informed and written consent. An ethics committee (CCP-OUEST-VI) provided approval for the study. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Data Collection
For PMR patients, age and sex were collected for the present study. Leukocytes, neutrophils, platelet counts, and hemoglobin levels were assessed at each available visit (V0 and V3 to V8). Levels of γ-globulins, immunoglobulin (Ig) A, IgG and IgM were collected at V0, V5, V6, and V8. Autoantibodies were tested only at inclusion. For HCs, a preliminary testing for antinuclear antibodies (ANA) was performed by indirect immunofluorescence (IIF). If ANA IIF was positive at 1/80 dilution, antibody screening was performed as described above for the patients. PMR-AS was collected at each visit between inclusion and V5 (week 12), and PMR-AS < 10 was used to define a response for survival analysis.
Interleukin-6
IL-6 was assessed using Human IL-6 enzyme-linked immunosorbent assay (ELISA) Kit II (BD Biosciences, San Jose, CA, USA) according to the manufacturer’s instructions. The detection threshold was 2.2 pg/ml.
Autoantibodies Assay
Sera were tested for ANA by indirect immunofluorescence (IIF) using HEp-2 cells, and the autoantibody profile comprised antidouble-stranded (ds) DNA, anti-SSA (52 + 60 kDa), anti-SSB, anti-Sm, anti-U1RNP, anti-Scl70, anti-Jo1, and anti-cardiolipin from the IDS-ISYS chemiluminescent system (Immunodiagnostic Systems Ltd, Boldon, UK); anti-dsDNA-NcX, anti-MPO, and anti-PR3 (EUROIMMUN, Lübeck, Germany); anti-CCP3 (Werfen, Cheshire, UK); rheumatoid factor, anti-alpha actinin and anti-histone assays were as previously described [15, 16]. For heatmap analysis, autoantibodies were standardized using the threshold for positivity (P +) determined by the laboratory as follows: (patient value)/(P +).
Statistical Analysis
Data are presented as the mean ± standard error of the mean or number (percentage) when appropriate. First, leukocytes, neutrophils, platelets, and hemoglobin were compared between the HCs and PMR patients at each available visit. The correlation between IL-6 and leukocytes, neutrophils, platelets, or hemoglobin was examined at V0 and V5. Next, the level of γ-globulin in the serum of the HCs and PMR patients at each available visit was compared, and IgA, IgG and IgM levels in the serum of the PMR patients were compared between V0 and V5. The Kruskal–Wallis nonparametric test was used to compare the PMR patients and HCs when more than two variables were considered. The paired Wilcoxon test was employed to compare the PMR patients over time. The Spearman correlation test was applied for correlations. The profile likelihood method using a log-rank (Mantel–Cox) regression model to compare the time for PMR-AS response was used in univariate analysis to determine the optimal threshold, and the patients were stratified into two groups with a Kaplan–Meier survival curve. RStudio® was used for heatmap analysis with reordering of both rows and columns and dendrogram construction. p < 0.05 was considered statistically significant. Statistical analyses were performed using GraphPad Prism® software v6.05 (GraphPad Software, La Jolla, CA, USA) and RStudio® v1.2.5042 (2009–2020 RStudio, Inc.) for Windows.
Results
Full Blood Count is Mainly Affected by Inflammation and Quickly Improved by Tocilizumab in Polymyalgia Rheumatica Patients
The characteristics of 18 PMR patients were previously reported in the TENOR study, (supplementary Table 1) [11]. Eleven of the patients were men (idem for the HCs). The mean age was 68 ± 7 and 66 ± 11 years, and the mean C-reactive protein level in the serum was 82 ± 16 and 5 ± 2 mg/l for the PMR patients and HCs, respectively. All patients fulfilled the Chaung’s classification criteria and the ACR/EULAR classification criteria. Confidence in the PMR diagnosis was unmodified after the complete follow-up. None of the patients received glucocorticoids before inclusion. At inclusion, leukocytes were significantly increased in the PMR patients (9.5 ± 0.8G/l) compared to HCs (7.1 ± 0.4G/l) (Fig. 1a), as were neutrophils (respectively 6.8 ± 0.7G/l and 4.3 ± 0.4G/l, Fig. 1b). In contrast, hemoglobin was slightly decreased in the PMR patients (12.3 ± 0.3 g/dl) compared to HCs (12.8 ± 0.4 g/dl) (Fig. 1c). Compared to the HCs (278 ± 92G/l), platelets were also increased in the PMR patients (388 ± 33G/l) at inclusion (Fig. 1d). After only one infusion of tocilizumab, at V3, leukocytes decreased to 6.0 ± 0.6 G/l, neutrophils decreased to 3.0 ± 0.4, hemoglobin increased to 13.4 ± 0.2 g/dl, and platelets decreased to 230 ± 16 G/l (Fig. 1). Moreover, a slight increase in leukocytes (from 5.5 ± 0.4 G/l) and neutrophils (from 2.6 ± 0.2 G/l) was observed after the introduction of glucocorticoids (from V5 to V8). Platelets and hemoglobin were both stable during the time of glucocorticoid treatment (from 203 ± 9 G/l to 239 ± 10.7 G/l and from 14.2 ± 0.1 g/dl to 13.8 ± 0.2 g/dl, respectively).
Whole blood count test in polymyalgia rheumatica patients. Leukocytes (a), neutrophils (b), hemoglobin (c) and platelets (d) were extracted from the whole blood of 18 PMR patients at each available visit and from sex- and age-matched healthy controls. Patients were treated with tocilizumab from V0 to V5 and with oral glucocorticoids from V5 to V8. Data are presented as the mean and standard error of the mean in red
The Association Between Interleukin-6 and Inflammatory Disturbances is No Longer Observed After Tocilizumab Therapy
At inclusion, a strong association was observed between IL-6 and all markers of inflammation from the full blood count (Fig. 2). Leukocytes were significantly associated with IL-6 (r = 0.715, p < 0.001), as were neutrophils (r = 0.767, p < 0.001), hemoglobin (r = 0.575, p = 0.012), and platelets (r = 0.47, p = 0.049). However, these associations were no longer observed after tocilizumab treatment (Fig. S1).
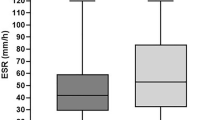
Levels of γ-Globulins are Increased in Early PMR, and a Quick Decrease is Observed After Tocilizumab Therapy
At inclusion, γ-globulins were increased in the PMR patients (12.1 ± 0.6 g/l) compared to HCs (8.8 ± 0.8 g/l) (Fig. 3a), but the level in the PMR patients’ serum progressively decreased after tocilizumab therapy (10.8 ± 0.5 g/l at V5) and glucocorticoids (9.8 ± 0.5 g/l at V8). Treatment with tocilizumab induced a rapid decrease in IgA (from 2.9 ± 0.4 g/l at V0 to 2.1 ± 0.2 g/l, Fig. S2A), IgG (from 11.7 ± 0.6 g/l at V0 to 10.2 ± 0.5 g/l, Fig. S2B) and IgM (from 1.0 ± 0.1 g/l at V0 to 0.9 ± 0.1 g/l, Fig. S2C) levels in the serum of the PMR patients. Furthermore, the levels of IgA, IgG and IgM were stable in the serum after glucocorticoid administration (2.2 ± 0.2 g/l, 9.4 ± 0.5 g/l, and 1.0 ± 0.1 g/l, respectively, at V8).
Gamma globulins are increased in polymyalgia rheumatica (PMR) patients, but the autoantibody profile is not different from that of healthy controls. Gamma globulins (a) were extracted from standard biological evaluations of 18 PMR patients at each available visit and from sex- and age-matched healthy controls (HCs). Patients were treated with tocilizumab from V0 to V5 and with oral glucocorticoids from V5 to V8. Data are presented as the mean and standard error of the mean in red. A survival curve (b) was calculated for PMR patients with gamma globulins over 11 g/l (black) and for PMR patients with 11 g/l or less (blue). The event considered was a PMR activity score under 10, and week 12 corresponded to visit 5. The optimal cut-off (11 g/l) was calculated using the profile likelihood method in a Cox regression model. The heatmap (c) represents a standardized ratio for all antibodies for PMR patients and HCs (antibody titer/antibody positivity threshold); reordering by a dendrogram considering all antibodies was then performed
Regarding time for PMR-AS response (Fig. 3b), Kaplan–Meier log-rank analysis retrieved a significant difference for γ-globulins (p = 0.01), and the best cut-off was set at 11 g/l. Patients with a serum level of γ-globulin greater than 11 g/l responded more rapidly than patients with 11 g/l or less [hazard ratio of 5.4; 95% confidence interval (1.4–20.7)].
Despite γ-Globulin Modifications, No Mark of Autoimmunity is Observed in Early Polymyalgia Rheumatica
Among the 18 PMR patients, 12 (66.7%) had ANA positivity. Eleven were positive at a dilution of 1/160 and 1 at a dilution of 1/320. In comparison, among the 13 HCs with available ANA testing, only six (46.1%) exhibited ANA positivity (three at a dilution of 1/160 and three at a dilution of 1/320). The difference was not significant. No PMR patients and no HCs were positive for anti-centromere autoantibodies. To assess whether nonspecific autoimmunity was increased in PMR patients compared to HCs, autoantibody values were standardized as described. The results are presented in Fig. 3c. No clustering enabled a distinction between the PMR patients and HCs.
Discussion
We showed that levels of leukocytes, neutrophils, and platelets were higher in early PMR patients than in HCs but that hemoglobin was decreased. Moreover, these modifications correlated with the IL-6 level in patient serum at inclusion. Quickly after tocilizumab therapy, leukocytes, neutrophils, and platelets decreased and hemoglobin increased in PMR patients and no longer correlated with IL-6. In addition, γ-globulins were increased, but no autoimmune mark enabled the differentiation of PMR patients and HCs. Finally, a γ-globulin level over 11 g/l was a biological marker associated with a quick response to tocilizumab.
The pathophysiology of PMR is poorly understood. Consequently, it is not clear whether PMR should be considered an autoimmune disease or an inflammatory or autoinflammatory disease [3]. The role of the innate immune system, the absence of interferon-γ secretion (compared to autoimmune diseases), the strong increase in APRs and the lack of specific autoantibodies suggest mechanisms closer to autoinflammation. Even if occurring mostly isolated, PMR can be associated with GCA, a large vessel vasculitis, and might share common pathophysiological pathways. In this study, we highlight the absence of specific autoantibodies among a large panel and the absence of an autoantibody background when compared to HCs.
Glucocorticoids remain the cornerstone of PMR treatment but are associated with many complications. Tocilizumab has shown promising results in early PMR and is currently evaluated as a GSA, though its place in the therapeutic strategy has yet to be determined. The speed of the efficacy has also been discussed and may be, for some authors, an obstacle to its use in PMR [12, 17]. In this study, all the inflammatory markers observed in PMR patients (leukocytes, neutrophils, platelets, hemoglobin, gammaglobulins) quickly decreased after tocilizumab therapy suggesting a fast-acting efficacy of tocilizumab in controlling inflammatory pathways in those patients. The clinical efficacy may be delayed compared to the inflammatory markers, but it is essential to notice that none of the patients received glucocorticoids before inclusion. Then patients were treated with tocilizumab only until week 12. Finally, tocilizumab was stopped, and patients received glucocorticoids from week 12 to week 24. One can imagine that glucocorticoids may be used for few days to wait for tocilizumab efficacy in early disease and then, suddenly stopped.
It is underlining that the tocilizumab positioning must be discussed in PMR. Tocilizumab might not be used in all patients affected by PMR, but so far, no biomarker, prognostic factor, or factor predicting response to treatment is currently available for PMR. In our study, patients with γ-globulin levels over 11 g/l responded more quickly than did other patients. The delay between treatment initiation and clinical improvement with tocilizumab therapy has been discussed and appears to be longer than that with glucocorticoids [12]. As a routinely available biological marker that predicts a rapid response for tocilizumab, the γ-globulin level is of clinical utility but has yet to be confirmed in other studies.
Our study is limited by the small number of patients. This small number might explain the prevalence of men over women, not commonly observed in PMR. Moreover, the data were obtained using common daily practice assay (except for the IL-6). This is a limitation in regard of the search for autoantibodies, but this is also an advantage to replicate and extrapolate our results to other cohorts. Nevertheless, no large cohort of PMR patients treated with tocilizumab and with extensive clinical and biological characterization is available to date.
Conclusions
To conclude, our study suggests that despite a strong increase of the inflammatory markers in early untreated PMR, tocilizumab quickly improves all those inflammatory components and that γ-globulins might be used to predict a quick response to tocilizumab therapy.
References
Mahr A, Belhassen M, Paccalin M, Devauchelle-Pensec V, Nolin M, Gandon S, et al. Characteristics and management of giant cell arteritis in France: a study based on national health insurance claims data. Rheumatol Oxf Engl. 2020;59:120–8.
Caporali R, Cimmino MA, Ferraccioli G, Gerli R, Klersy C, Salvarani C, et al. Prednisone plus methotrexate for polymyalgia rheumatica: a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2004;141:493–500.
Floris A, Piga M, Cauli A, Salvarani C, Mathieu A. Polymyalgia rheumatica: an autoinflammatory disorder? RMD Open. 2018;4:e000694.
Carvajal Alegria G, Devauchelle-Pensec V, Renaudineau Y, Saraux A, Pers J-O, Cornec D. Correction of abnormal B-cell subset distribution by interleukin-6 receptor blockade in polymyalgia rheumatica. Rheumatol Oxf Engl. 2017;56:1401–6.
van Sleen Y, Wang Q, van der Geest KSM, Westra J, Abdulahad WH, Heeringa P, et al. Involvement of monocyte subsets in the immunopathology of giant cell arteritis. Sci Rep. 2017;7:6553.
Samson M, Audia S, Fraszczak J, Trad M, Ornetti P, Lakomy D, et al. Th1 and Th17 lymphocytes expressing CD161 are implicated in giant cell arteritis and polymyalgia rheumatica pathogenesis. Arthritis Rheum. 2012;64:3788–98.
van der Geest KSM, Abdulahad WH, Chalan P, Rutgers A, Horst G, Huitema MG, et al. Disturbed B cell homeostasis in newly diagnosed giant cell arteritis and polymyalgia rheumatica. Arthritis Rheumatol Hoboken NJ. 2014;66:1927–38.
Baerlecken NT, Linnemann A, Gross WL, Moosig F, Vazquez-Rodriguez TR, Gonzalez-Gay MA, et al. Association of ferritin autoantibodies with giant cell arteritis/polymyalgia rheumatica. Ann Rheum Dis. 2012;71:943–7.
van Sleen Y, Graver JC, Abdulahad WH, van der Geest KSM, Boots AMH, Sandovici M, et al. Leukocyte dynamics reveal a persistent myeloid dominance in giant cell arteritis and polymyalgia rheumatica. Front Immunol. 2019;10:1981.
Xu X, Han M, Li T, Sun W, Wang D, Fu B, et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci USA. 2020. https://doi.org/10.1073/pnas.2005615117.
Devauchelle-Pensec V, Berthelot JM, Cornec D, Renaudineau Y, Marhadour T, Jousse-Joulin S, et al. Efficacy of first-line tocilizumab therapy in early polymyalgia rheumatica: a prospective longitudinal study. Ann Rheum Dis. 2016;75:1506–10.
Akiyama M, Kaneko Y, Takeuchi T. Tocilizumab in isolated polymyalgia rheumatica: a systematic literature review. Semin Arthritis Rheum. 2020;50:521–5.
Devauchelle-Pensec V. Has the time come for biotherapies in giant cell arteritis and polymyalgia rheumatica? Jt Bone Spine. 2016;83:471–2.
Cleuziou C, Binard A, De Bandt M, Berthelot J-M, Saraux A. Contribution of the polymyalgia rheumatica activity score to glucocorticoid dosage adjustment in everyday practice. J Rheumatol. 2012;39:310–3.
Renaudineau Y, Croquefer S, Jousse S, Renaudineau E, Devauchelle V, Guéguen P, et al. Association of alpha-actinin-binding anti-double-stranded DNA antibodies with lupus nephritis. Arthritis Rheum. 2006;54:2523–32.
Zachou K, Oikonomou K, Renaudineau Y, Chauveau A, Gatselis N, Youinou P, et al. Anti-α actinin antibodies as new predictors of response to treatment in autoimmune hepatitis type 1. Aliment Pharmacol Ther. 2012;35:116–25.
Carvajal Alegria G, Saraux A, Devauchelle-Pensec V. Is tocilizumab as efficient as steroids early in polymyalgia rheumatica? Semin Arthritis Rheum. 2020;50:582.
Acknowledgements
The authors thank the patients and the controls included in the present study.
Funding
Roche-Chugai provided an unconditional grant for the TENOR study. Tocilizumab was donated free of charge by Roche-Chugai. Roche-Chugai had no role in the design or execution of the study; the collection, management, analysis, or interpretation of the data; or in the preparation, revision, or approval of the manuscript. No funding was received for the publication of this article.
Editorial Assistance
The authors thank the American Journal Experts for their editorial assistance (funded by the association GUERIR).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Guillermo Carvajal Alegria, Divi Y. K Cornec, Yves Renaudineau, Alain Saraux and Valérie Devauchelle-Pensec have no conflicts of interest related to this work. Alain Saraux is a member of the journal’s Editorial Board.
Compliance with Ethics Guidelines
An ethics committee (CCP-OUEST-VI) and a local ethics committee (comité d’éthique du CHRU de Brest, séance du 09/12/2014) provided approval for the study. The TENOR trial has been registered on ClinicalTrials under the number NCT01713842. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. All healthy controls included in this study gave informed and written consent.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Carvajal Alegria, G., Cornec, D.Y.K., Renaudineau, Y. et al. Inflammatory Markers are Quickly Improved by Tocilizumab in Early Polymyalgia Rheumatica and Might Predict Early Response to Interleukin-6 Blockade. Rheumatol Ther 8, 751–760 (2021). https://doi.org/10.1007/s40744-021-00299-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-021-00299-8