Abstract
Introduction
Rheumatoid arthritis (RA) produces debilitating morning stiffness. Exogenous glucocorticoids can help with these symptoms when timed appropriately. Bedtime dosing of delayed-release prednisone (DR-prednisone) matches the rise of inflammatory cytokines before awakening and can improve stiffness and other RA symptoms. A prospective open-label study was conducted in patients currently on stable doses of immediate-release prednisone (IR-prednisone) who were switched to DR-prednisone to analyze the incremental benefit of better timed and lower dose glucocorticoid therapy.
Methods
Twelve US sites enrolled patients with moderate-severe RA into a 12-week prospective study. Patients were switched from IR- to DR-prednisone while maintaining other existing background therapies. Change from baseline in morning stiffness severity, morning stiffness duration, swollen and tender joint counts (S-TJC), 28 joint disease activity score (DAS28), and patient/physician global assessment (PGA/PhGA), among others, were measured. Post-hoc analyses were performed on those completing 10 weeks of treatment and those with >60 min of morning stiffness at baseline.
Results
Fifty-six patients had at least one follow-up visit and were similar in demographics to previous controlled trials with DR-prednisone with regard to baseline age and DAS28-CRP but had lower morning stiffness and RA duration. DR-prednisone produced a trend toward lower morning stiffness severity and duration with a reduction in daily prednisone dose of almost 1 mg. Patients treated with DR-prednisone for ≥10 weeks demonstrated significant reductions in morning stiffness duration, SJC, TJC, DAS28-CRP, and PhGA (all p ≤ 0.04). Patients treated for ≥10 weeks with >60 min of baseline morning stiffness produced similar results in these measures as well as a 21% reduction in morning stiffness severity (p = 0.02).
Conclusion
Patients switched to DR-prednisone from IR-prednisone in this practice-based study maintained or improved their outcomes across a variety of domains, and results were comparable to previous controlled trials in which patients completed at least 10 weeks of treatment.
Funding
Horizon Pharma USA, Inc.
Trial Registration
ClinicalTrials.gov identifier, NCT02287610.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory joint disease that can cause cartilage and bone destruction if left untreated [1]. Upon confirming a diagnosis of RA, a variety of treatment approaches are typically considered, including non-steroidal anti-inflammatory drugs (NSAIDs), synthetic disease-modifying anti-rheumatic drugs (DMARDs), biologic DMARDs, and glucocorticoids. The use of glucocorticoids has long been a therapeutic option to treat RA, but their long-term administration is often hampered by adverse effects, many of which may be dose dependent. The use of low-dose prednisone therapy results in less joint damage and improved disease control and physical function when combined with other DMARDs as compared to DMARD therapy alone [2]. Further, the addition of prednisone to DMARD therapy may reduce the need to add biologic therapy or escalate DMARD doses to meet disease target measures [2].
RA is commonly treated with low-dose immediate-release prednisone (IR-prednisone) in the morning upon awakening. This timing may not optimize control of inflammation and disease symptoms because inflammatory cytokines peak before awakening, typically around 2–4 a.m. [3]. Administering a delayed-release prednisone (DR-prednisone) tablet at bedtime enables timed delivery of prednisone before and during this circadian peak of inflammatory cytokine release and thereby potentially influences disease symptoms [4]. IR-prednisone is typically dosed upon awakening after the peak of the inflammatory process in RA. A 12-week, randomized controlled study previously demonstrated that patients treated with concomitant DMARDs and DR-prednisone had a significant reduction in morning stiffness compared with patients treated with DMARD monotherapy [5]. Another 12-week, randomized trial showed that patients treated with DR-prednisone had significantly reduced morning stiffness compared with those treated with IR-prednisone [6], and similar improvements were observed in patients who switched from IR- to DR-prednisone in an open-label extension trial [7, 8]. No previous controlled trial has allowed for prednisone dose adjustments to determine whether efficacy could be maintained at a lower total glucocorticoid dose. The current study was undertaken to assess the effectiveness of switching from conventional IR-prednisone therapy to DR-prednisone in patients with moderately to severely active rheumatoid arthritis in a practice-based setting using standard rheumatoid arthritis patient assessments and permitting dose adjustments.
Methods
Study Design
This was a 12-week, prospective study (ClinicalTrials.gov: NCT02287610) of patients in the USA at 14 sites (Alabama, Arizona, California, Florida, Georgia, Kentucky, New York, North Carolina, Ohio, Texas) who were aged 18 years or older with moderate to severe rheumatoid arthritis (according to the 2010 American College of Rheumatology and/or European League Against Rheumatism classification criteria), with RA disease activity as defined by disease activity score in 28 joints (DAS28) of ≥3.2 [calculated with either C-reactive protein (DAS28-CRP) or erythrocyte sedimentation rate (DAS28-ESR)] and additionally morning stiffness duration of ≥45 min at study entry. To be eligible for study participation, at the time of study entry patients had to be receiving conventional immediate-release prednisone at a dose ≥2.5 mg every morning. Patients subsequently made the decision with their physicians to convert to DR-prednisone (Horizon Pharma USA, Inc., Lake Forest, IL). The choice of DR-prednisone dose was at the physician’s discretion, and alterations of the dose during the study were allowed based on individual considerations. Patients were maintained on existing background therapies during the study. Physicians queried patients regarding their actual utilization of DR-prednisone and, as appropriate, other prescription and over-the-counter treatments.
The study protocol was reviewed and approved by an institutional review board. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients for inclusion in the study.
Endpoints
The primary endpoint was mean reduction in morning stiffness severity [using a 100-mm visual analog scale (VAS)] from baseline to final follow-up visit. Secondary endpoints included change in duration of morning stiffness (minutes), patient global assessment in disease activity (PGA; 0–10 cm VAS; 0, very well; 10, very poor), physician global assessment in disease activity (PhGA, 0–10 cm VAS; 0, very well; 10, very poor), DAS28-CRP, DAS28-ESR, Clinical Disease Activity Index (CDAI; composite tool; score 0–76), Simple Disease Activity Index (SDAI; composite tool; score 0–86), and routine assessment of patient index data (RAPID3), which includes physical function, pain, and three patient-reported assessments, utilizing a portion of the Multidimensional Health Assessment Questionnaire (MDHAQ). Secondary endpoints also included evaluation of change in the total daily prednisone dose from baseline to final follow-up visit. The changes from baseline in other measurements used in composite tools of CDAI and SDAI, such as tender joint count of 28 joints (TJC28) and swollen joint count of 28 joints (SJC28), were also evaluated.
Primary and secondary endpoints were evaluated in patients with baseline and any follow-up measurements. No pre-defined visits, medical or laboratory tests, procedures, or interventions were required. Rather, all evaluations and procedures were at the discretion of the investigator. As the length of time between baseline and follow-up measurements was not mandated by the study design, the number of patients and length of time on study may have differed within each measurement and cohort examined. A subset of the endpoints was evaluated in the patients receiving DR-prednisone for ≥10 weeks and in patients who were receiving DR-prednisone for ≥10 weeks and had >60 min of morning stiffness at baseline to match that seen in the previously published controlled trials [5, 6, 8, 9].
Adverse Events
Adverse events (AEs) were defined as any untoward medical occurrence in a patient receiving treatment that did not necessarily have a causal relationship with the treatment; relation to treatment with DR-prednisone was determined by the investigator. A serious AE was defined as any event that resulted in death, was life-threatening, required hospitalization or prolongation of existing hospitalization, resulted in persistent or significant disability or incapacity, resulted in a congenital anomaly or birth defect, or was otherwise deemed an important medical event. Evaluation of AEs occurred at three follow-up visits, estimated to occur at 4, 8, and 12 weeks after baseline. AEs and serious AEs were categorized according to the Medical Dictionary for Regulatory Activities (MedDRA), system organ class, and preferred term.
Statistical Analysis
Analyses and tabulations were performed using Microsoft Excel 2010 and SAS®. For the primary and most of the secondary endpoints, data are presented as a comparison between results obtained when patients were treated with conventional IR-prednisone (baseline) vs. results obtained when patients were treated with DR-prednisone at follow-up visits. As each patient served as their own control, significance was determined using paired t tests; R 2 coefficients were used for associations.
Results
Study Population
Patients were enrolled into the study between November 2014 and September 2015. Practicing rheumatologists at 14 sites enrolled 75 patients: 11 did not meet eligibility criteria, 3 never received DR-prednisone, and 5 were not included because of lack of follow-up (Fig. 1). Of the 56 patients who had follow-up data (follow-up population) included in the analysis, 29 patients were receiving therapy for ≥10 weeks and 16 patients were receiving therapy for ≥10 weeks and had >60 min of baseline morning stiffness. Patient demographics, baseline disease characteristics, and prior and concomitant medications were similar to previous studies (Table 1). In the follow-up population, the mean [SD] baseline dose of prednisone was 6.53 mg [3.73] (range, 2.5–20 mg).
Endpoints
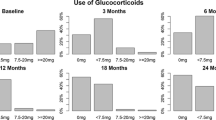
In the follow-up population, patients were receiving DR-prednisone for a mean (SD) of 9.92 (4.47) weeks (range 0.43–18.71 weeks); the average morning stiffness severity and duration at baseline were 56.37 mm and 114.02 min, respectively. Upon switching to DR-prednisone, patients with a follow-up visit had a mean (SD) decrease of 5.16 (27.26) mm in the primary endpoint of morning stiffness severity and 18.90 (77.49) minutes in the secondary endpoint of morning stiffness duration. While the primary endpoint was not statistically significant, comparison of baseline measurements with those at the last follow-up visit revealed significant reductions in the clinically important secondary endpoints of swollen joint count of 28 joints (SJC28; −21.97%), routine assessment of patient index data (RAPID3; −11.95%), physician global assessment (PhGA; −13.73%), and DAS28 by C-reactive protein (DAS28-CRP; −11.93%) (Fig. 2). Tender joint count of 28 joint (TJC28) scores decreased but were not statistically significant [mean (SD), 10.97 (8.73) vs. 13.05 (7.75) at baseline; n = 39; p = 0.07]. Although the changes in CDAI and SDAI scores were not statistically significant, 24% of patients improved by one category (i.e., high, moderate, or low disease activity or remission) from baseline to final follow-up. Additionally, the prednisone dose decreased by 15% from baseline [mean (SD), 5.57 (2.32) vs. 6.53 (3.73) mg at baseline; n = 56; p = 0.05] (Fig. 3).
SJC28 (a), RAPID3 (b), PhGA of disease activity (c), and DAS28-CRP (d) for patients on DR-prednisone with follow-up. Data are summarized as the mean (standard deviation). DAS28-CRP disease activity score in 28 joints by C-reactive protein, PhGA physician global assessment, RAPID3 routine assessment of patient index data, SJC28 swollen joint count of 28 joints, VAS visual analog scale
Baseline and last follow-up prednisone dosage for patients on DR-prednisone with a follow-up visit, a subset of patients on DR-prednisone for ≥10 weeks, and a subset of patients on DR-prednisone for ≥10 weeks with >60 min of morning stiffness at baseline. Data are summarized as the mean (SD). MS morning stiffness
Length of Treatment
Due to the nature of the study, patients were not required to attend visits at a defined time point or to remain on therapy for a set period of time to be included in analysis; therefore, the length of time between baseline and follow-up varied (range 0.43–18.71 weeks). To overcome this study limitation, post hoc analyses evaluated the change from baseline in those patients exposed to DR-prednisone treatment for a period of time more consistent with a controlled clinical trial. Patients completing ≥10 weeks of DR-prednisone treatment [mean (SD), 13.16 (2.26) weeks] had significant reductions in morning stiffness duration (−27.22% or −35.00 [81.89] min, which exceeds the minimum threshold for clinically important morning stiffness reduction [9]). SJC28 (−36.50%), PhGA (−18.90%), DAS28-CRP (−17.57%) (Fig. 4), and TJC28 scores (−29.69%) also improved. The disease activity index scores were also significantly reduced [CDAI: 27.08 (15.53) vs. 37.93 (17.69) at baseline; n = 20; p < 0.01; SDAI: 28.44 (17.61) vs. 38.17 (18.43) at baseline; n = 17; p < 0.01]. The mean change in CDAI of −10.85 (12.35) exceeds the minimum threshold (7.3) for clinically important improvement in moderate disease activity [13]. Approximately 30% of patients improved by one category in both CDAI and SDAI. The change in morning stiffness severity between baseline and follow-up was −11.89% but not significant (p = 0.22); similarly, RAPID3 scores decreased but were not statistically significant (p = 0.11). The prednisone dose decreased by 13% from baseline but was not statistically significantly different [mean (SD), 5.31 (2.55) vs. 6.09 (3.44) mg at baseline] (Fig. 3). Among patients treated for <10 weeks (n = 27), only the improvement in the functional component of the Multidimensional Health Assessment Questionnaire was significant (−22.59%; p = 0.02).
SJC28 (a), morning stiffness duration (b), PhGA of disease activity (c), and DAS28-CRP (d) for patients on DR-prednisone for ≥10 weeks. Data are summarized as the mean (standard deviation). DAS28-CRP disease activity score in 28 joints by C-reactive protein; PhGA physician global assessment; RAPID3 routine assessment of patient index data; SJC28 swollen joint count of 28 joints; VAS visual analog scale
Patients who received DR-prednisone for ≥10 weeks and had greater disease burden at entry (>60 min of baseline morning stiffness) had significant reductions in morning stiffness severity (−20.84%), morning stiffness duration (−30.98%), PhGA (−21.47%), and SJC28 (−30.64%) (Fig. 5). CDAI scores were also significantly reduced [mean (SD), 27.79 (16.36) vs. 35.83 (17.60) at baseline; n = 12; p = 0.01]. DAS28-CRP scores decreased but were not significant [mean (SD), 4.27 (1.71) vs. 4.74 (1.35) at baseline; n = 10; p = 0.11]. The prednisone dose decreased by 15% from baseline over the study period, but this was not statistically significant [mean (SD), 4.88 (1.82) vs. 5.75 (3.61) mg at baseline] (Fig. 3). Post hoc analysis revealed that morning stiffness severity and duration improvements were moderately correlated (R 2 = 0.54); no other correlations were demonstrated.
Morning stiffness severity (a), morning stiffness duration (b), PhGA of disease activity (c), DAS28-CRP (d), SJC28 (e), and RAPID3 (f) for patients on DR-prednisone for ≥10 weeks with >60 min of morning stiffness at baseline. Data are summarized as the mean (standard deviation). DAS28-CRP disease activity score in 28 joints by C-reactive protein; PhGA physician global assessment; RAPID3 routine assessment of patient index data; SJC28 swollen joint count of 28 joints; VAS visual analog scale
Adverse Events
Twelve adverse events (AEs) occurred in the study and are summarized in Table 2. Six events were considered by the investigator to be related to DR-prednisone. Of these, one patient continued taking DR-prednisone, and DR-prednisone was discontinued in the remaining patients because of high blood pressure, elevated blood glucose, worsening of joint pain, insomnia, and the single serious AE of severe abdominal pain with hospitalization.
Discussion
Due to the circadian release of pro-inflammatory mediators, pain and stiffness arising from RA are most severe in the early morning hours, significantly reducing patients’ quality of life [10]. DR-prednisone has previously been shown to reduce morning stiffness in clinical trials [5, 6]; however, not all trials permitted changes in prednisone dosage in patients switching from IR- to DR-prednisone.
Patients with moderate-to-severe RA who switched from IR- to DR-prednisone in this practice-based study maintained or improved their outcomes across a variety of domains. The results were comparable to previous studies of IR- versus DR-prednisone [6, 8, 9], showing improved morning symptoms, but added to those data in that several other disease measures were improved with a lower total daily dose. These findings mirror two previous studies in polymyalgia rheumatica (PMR). One showed a clear trend for improved short-term outcomes using DR-prednisone as compared to IR-prednisone [11], and another showed that 7 mg of DR-prednisone given in the evening achieved a similar percentage reduction in mean duration of morning stiffness as achieved with twice the dose of prednisolone in the morning [12].
In the overall intention-to-treat (follow-up) population, there were significant reductions in swollen joint counts and physician global assessment of disease activity, RAPID3 and DAS28-CRP. Of particular note, patients treated for ≥10 weeks had significant reductions in morning stiffness duration, swollen joint counts, DAS28-CRP, physician global assessment of disease activity scores, and SDAI as well as a statistically and clinically significant improvement in CDAI [13], indicating that DR-prednisone improved multiple clinical outcomes compared with its IR baseline counterpart, at a lower dose.
It has been shown that morning stiffness severity is strongly correlated with the intensity of morning pain and, to a lesser extent, disease activity and pain on waking [14]. We completed subgroup analyses intending to match the baseline population characteristics from the previously published trials of DR-prednisone [5,6,7,8,9], and these results indicated there was significant improvement in morning stiffness severity, morning stiffness duration, physician global assessment of disease activity, clinical disease activity index, and swollen joint counts among patients with an initially high disease burden (>60 min of morning stiffness at baseline) who were treated with DR-prednisone for ≥10 weeks. These results differed from those patients treated less than 10 weeks, who had lower disease activity, where there was no difference in disease measures. This may indicate that patients with active disease as reflected by prolonged morning stiffness have the potential to benefit more from treatment with a lower dose of DR-prednisone compared with IR-prednisone, validating the benefit of chronotherapy.
Despite its benefits in rheumatoid arthritis, long-term treatment with high-dose prednisone (>10 mg) is associated with an increase in AEs. One study demonstrated that, compared with former users, current corticosteroid users had increased mortality, work disability, and total joint replacement [15]. Furthermore, a large observational study of glucocorticoid users and nonusers found an increased relative risk of cardiovascular events among patients receiving high-dose prednisone [16]. Studies have previously shown dose-dependent linear and threshold increases in AEs from lower (<5 mg) to higher doses (7.5–10 mg); therefore, any reduction in prednisone dosage is advantageous for patients [17,18,19,20,21]. In the current study, the treating physician was allowed to decrease the dose of DR-prednisone at any time. A statistically nonsignificant but potentially clinically relevant reduction of prednisone dose by almost 1 mg/day/patient was observed in all the cohorts. The reduction in total prednisone dose over the treatment period was comparable to the 18% reduction found in a previous analysis [22]. The reduction in glucocorticoid burden seen in these analyses with DR-prednisone is notable given the maintenance or improvement in disease measures.
This study has limitations primarily attributable to its practice-based nature, including lack of blinding and differing evaluation and follow-up intervals. The length of time between baseline and follow-up measurements was not mandated, resulting in varying lengths of drug exposure between subjects. Subgroup analysis of those in the study for ≥10 weeks created a more homogeneous population in terms of length in study, but reduced the sample size and concomitantly statistical power. Additionally, the average baseline morning stiffness in the follow-up study population was approximately 40–50 min less than in previous studies [5, 6], indicating that these patients, despite having similar disease scores, had lower morning disease symptoms. Another limitation of the study is patient adherence to the prescribed DR-prednisone regimen was not verified.
Conclusions
Patients with moderate-to-severe RA who had been maintained on IR-prednisone chronically and were switched to DR-prednisone in this practice-based study maintained or improved outcomes across a variety of domains, particularly when treated for ≥10 weeks. There was a statistically non-significant but potentially clinically relevant reduction of prednisone dose by almost 1 mg/day/patient in the cohorts evaluated.
These findings suggest that patients with moderately to severely active RA who have been treated with low-dose IR-prednisone may benefit from switching to DR-prednisone at a lower dose.
References
Goronzy JJ, Weyand CM. Developments in the scientific understanding of rheumatoid arthritis. Arthritis Res Ther. 2009;11:249.
Bakker MF, Jacobs JW, Welsing PM, et al. Low-dose prednisone inclusion in a methotrexate-based, tight control strategy for early rheumatoid arthritis: a randomized trial. Ann Intern Med. 2012;156:329–39.
Cutolo M, Seriolo B, Craviotto C, et al. Circadian rhythms in RA. Ann Rheum Dis. 2003;62:593–6.
Cutolo M. Glucocorticoids and chronotherapy in rheumatoid arthritis. RMD Open. 2016;2:e000203.
Buttgereit F, Mehta D, Kirwan J, et al. Low-dose prednisone chronotherapy for rheumatoid arthritis: a randomised clinical trial (CAPRA-2). Ann Rheum Dis. 2013;72:204–10.
Buttgereit F, Doering G, Schaeffler A, et al. Efficacy of modified-release versus standard prednisone to reduce duration of morning stiffness of the joints in rheumatoid arthritis (CAPRA-1): a double-blind, randomised controlled trial. Lancet. 2008;371:205–14.
Buttgereit F, Doering G, Schaeffler A, et al. Targeting pathophysiological rhythms: prednisone chronotherapy shows sustained efficacy in rheumatoid arthritis. Ann Rheum Dis. 2010;69:1275–80.
Alten R, Holt R, Grahn A, et al. Morning stiffness response with delayed-release prednisone after ineffective course of immediate-release prednisone. Scand J Rheumatol. 2015;44:354–8.
Buttgereit F, Kent JD, Holt RJ, et al. Improvement thresholds for morning stiffness duration in patients receiving delayed- versus immediate-release prednisone for rheumatoid arthritis. Bull Hosp Jt Dis 2013. 2015;73:168–77.
da Silva JA, Phillips S, Buttgereit F. Impact of impaired morning function on the lives and well-being of patients with rheumatoid arthritis. Scand J Rheumatol Suppl. 2011;125:6–11.
Cutolo M, Hopp M, Liebscher S, et al. Modified-release prednisone for polymyalgia rheumatica: a multicentre, randomised, active-controlled, double-blind, parallel-group study. RMD Open. 2017;3:e000426.
Zakout SA, Lynsey LC, Jessop D, et al. Circadian variation in plasma IL-6 and the role of modified-release prednisone in polymyalgia rheumatica. Int J Clin Rheumatol. 2014;9:431–9.
Aletaha D, Funovits J, Ward MM, et al. Perception of improvement in patients with rheumatoid arthritis varies with disease activity levels at baseline. Arthritis Rheum. 2009;61:313–20.
Boers M, Buttgereit F, Saag K, et al. What is the relationship between morning symptoms and measures of disease activity in patients with rheumatoid arthritis? Arthritis Care Res. 2015;67:1202–9.
Caplan L, Wolfe F, Russell AS, Michaud K. Corticosteroid use in rheumatoid arthritis: prevalence, predictors, correlates, and outcomes. J Rheumatol. 2007;34:696–705.
Wei L, MacDonald TM, Walker BR. Taking glucocorticoids by prescription is associated with subsequent cardiovascular disease. Ann Intern Med. 2004;141:764–70.
Da Silva JA, Jacobs JW, Kirwan JR, et al. Safety of low dose glucocorticoid treatment in rheumatoid arthritis: published evidence and prospective trial data. Ann Rheum Dis. 2006;65:285–93.
Huscher D, Thiele K, Gromnica-Ihle E, et al. Dose-related patterns of glucocorticoid-induced side effects. Ann Rheum Dis. 2009;68:1119–24.
Kirwan JR. The effect of glucocorticoids on joint destruction in rheumatoid arthritis. The Arthritis and Rheumatism Council Low-Dose Glucocorticoid Study Group. N Engl J Med. 1995;333:142–6.
van Everdingen AA, Jacobs JW, Siewertsz Van Reesema DR, Bijlsma JW. Low-dose prednisone therapy for patients with early active rheumatoid arthritis: clinical efficacy, disease-modifying properties, and side effects: a randomized, double-blind, placebo-controlled clinical trial. Ann Intern Med. 2002;136:1–12.
Wassenberg S, Rau R, Steinfeld P, Zeidler H. Very low-dose prednisolone in early rheumatoid arthritis retards radiographic progression over two years: a multicenter, double-blind, placebo-controlled trial. Arthritis Rheum. 2005;52:3371–80.
Cutolo M, Iaccarino L, Doria A, et al. Efficacy of the switch to modified-release prednisone in rheumatoid arthritis patients treated with standard glucocorticoids. Clin Exp Rheumatol. 2013;31:498–505.
Acknowledgements
Horizon Pharma USA, Inc., funded the development, conduct, and analysis of the study. Horizon Pharma USA, Inc., also funded the article processing charges. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Compliance with Ethics Guidelines
The study protocol was reviewed and approved by an institutional review board. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all patients for being included in the study.
Disclosures
Ara H. Dikranian has served as a consultant to Horizon Pharma USA, Inc. Rubaiya Mallay has served as a consultant to Horizon Pharma USA, Inc., and AbbVie. Robert J. Holt is an employee of and current stock/stock option holder of Horizon Pharma USA, Inc. Mike Marshall is an employee of and current stock/stock option holder of Horizon Pharma USA, Inc. Megan Francis-Sedlak is an employee of and current stock/stock option holder of Horizon Pharma USA, Inc.
Data availability
The data sets generated during the current study are not publicly available but may be available from the corresponding author. Data are also available on clinicaltrials.gov (NCT02287610).
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article, go to http://www.medengine.com/Redeem/157AF060227539A6.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Dikranian, A.H., Mallay, R., Marshall, M. et al. Switching From Immediate-Release to Delayed-Release Prednisone in Moderate to Severe Rheumatoid Arthritis: A Practice-Based Clinical Study. Rheumatol Ther 4, 363–374 (2017). https://doi.org/10.1007/s40744-017-0075-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-017-0075-1