Abstract
Cardiovascular (CV) comorbidities are a frequent extra-articular manifestation of rheumatoid arthritis (RA). Cardiovascular disease (CVD) with accelerated atherosclerosis is a major cause of morbidity and mortality in patients with RA. Subclinical CVD may be present since the early phase of RA. Not only traditional but also non-traditional CV risk factors are involved in the pathogenesis of RA-related CVD. Due to the lack of specifically designed randomized clinical trials, it is still unclear which tools to use to perform CV risk assessment, how to interpret the results and which interventions are appropriate in RA patients both to prevent and to manage CVD. Based on the available evidence, we propose a practical approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatoid arthritis (RA) is a common chronic inflammatory joint disease, which affects up to 1% of the general population. Patients with RA may experience disability due to joint involvement as well as multiple extra-articular comorbidities [1]. Although great advances have been made over the last 20 years in the understanding of the pathogenesis and in the management of RA, life expectancy is still lower than that of the general population [2]. Cardiovascular (CV) comorbidities are a common extra-articular manifestation of RA (Table 1) [3, 4]. Among RA-related cardiac diseases, accelerated atherosclerosis, particularly in the form of coronary artery disease, has the greatest clinical impact because it is the main cause of premature mortality in most autoimmune rheumatic diseases [5]. Compared with the general population, patients with RA experience a doubled risk of developing a CV disease (CVD) [6], with 60% and 48% increases, respectively, in risk of CVD mortality and morbidity [7, 8]. The excess CV burden in patients with RA is not fully explained by traditional CV risk factors although their impact in patients with RA is high [9]. Growing evidence supports the view that RA behaves as an independent risk factor for the development of CVD similarly to diabetes mellitus [10].
There are many issues that need to be considered when CVD risk is evaluated in RA. Clinical presentations are often atypical in RA patients, thus contributing to substantially underdiagnosed and untreated CVD [11, 12]. Subclinical CVD may be overlooked with traditional imaging techniques, whereas newer diagnostic tools may show the presence of subclinical myocardial dysfunction and microvascular disease are often present in these patients (Table 1) [13].
Aside from pharmacological and non-pharmacological interventions on traditional CV risk factors, the control of disease activity and inflammation in RA seems to play a pivotal role in reducing CV risk [14]. In line with this view, a very recent paper from Myasoedova et al. reported an improved overall CV mortality in patients with RA in recent years [15]. The reasons of such findings need to be further examined, but an improved control of disease activity in the latest years could be hypothesized. The optimal management of CV risk and comorbidities in RA is still open to debate. In view of this unmet need, the European League Against Rheumatism (EULAR) task force was prompted by new evidence to perform an update of the 2009 recommendations of CV risk management in inflammatory joint diseases, particularly in RA [16].
We aim to provide a practical update on the main aspects of prevention and treatment of CV comorbidities in RA, focusing on atherosclerotic CVD, in order to help the clinician in the management of this condition in a day-to-day setting.
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Pathogenesis
The pathogenic mechanisms underlying accelerated CVD in RA are complex and not completely clarified (Fig. 1). Several genetic polymorphisms at loci either inside or outside the major histocompatibility complex (MHC) region have been associated with both atherosclerosis and RA. Association between the shared epitope alleles of HLA-DRB1 * 04 and endothelial dysfunction and CV risk has been reported. Polymorphisms outside the MHC region were associated with dyslipidemia and hypertension and even with the risk of CV events independently of the presence of traditional risk factors in patients with RA [4].
The contribution of traditional and non-traditional risk factors and anti-rheumatic therapies to cardiovascular risk in patients with rheumatoid arthritis. CV cardiovascular, COXIBs cyclooxygenase-2 inhibitors, DMARDs disease-modifying anti-rheumatic drugs, NSAIDs non-steroidal anti-inflammatory drugs
The absolute CV risk for patients with RA is increased when compared with the general population even after adjusting for traditional CV risk factors. Nevertheless, traditional risk factors are important contributors to the CV risk of patients with RA and further non-traditional risk factors have been more recently identified (Table 2) [5]. In a number of autoimmune systemic diseases, immune mechanisms and inflammation may contribute to accelerated atherosclerosis since the early phase of the disease [5, 17]. Extensive cross-talk between the coagulation pathway and inflammation is clear and it is particularly relevant in the case of RA [18]. The activation of the inflammatory cytokine network induces a pro-thrombotic environment characterized by insulin resistance, dyslipidemia, endothelial dysfunction, and alterations of coagulation and fibrinolytic systems [19]. Inflammation is the main culprit in both RA and atherosclerosis [20]. Recently, also citrullination and carbamylation have been suggested as common pathways linking RA and coronary heart disease [21].
Defining the Problem: Quantifying CVD Risk in RA
It is now accepted that RA should be considered as an independent risk factor for the development of CVD and the European Society of Cardiology (ESC) guidelines have been reviewed accordingly [22]. The Systematic Coronary Risk Evaluation (SCORE) system is a CV risk-assessment tool developed for the general population that is based on the identification of selected unmodifiable (gender, age) and modifiable factors (smoking status, systolic blood pressure, and lipid profile) [23]. The risk prediction models available for the general population have demonstrated to underestimate CV risk in RA patients [24], therefore, many attempts have been made to produce RA-specific risk calculators [25,26,27] and correction factors have been suggested [23, 27, 28]. The addition of a 1.5 multiplication factor to the SCORE system in patients with RA has been approved by the European League Against Rheumatism (EULAR) for daily implementation in clinical practice. The correction must be applied independently of disease-related criteria, although high disease activity and duration (>10 years), the presence of rheumatoid factor (RF) and/or anticitrullinated peptide antibodies (ACPA) and extra-articular manifestations deserve attention [16, 29]. However, a recent study by Crowson et al. demonstrated that RA-specific risk calculators, including EULAR 1.5 multiplier, do not predict CV risk more accurately than risk calculators developed for the general population [30].
According to EULAR recommendations [16], the assessment of RA patients should be warranted from once every 5 years if the risk is low to moderate, since the impact of narrower screening intervals is not evidence-based [31] or more often for patients with intermediate and high risk (Fig. 2). EULAR recommendations do not specify the frequency, but we suggest at least once per year. When CVD risk exceeds a 10-year risk of 5% for fatal CVD events with SCORE, lifestyle changes and treatment with lipid-lowering agents is recommended. However, a healthy lifestyle is emphasized for all persons, including patients at low and intermediate CV risk. Additionally, ESC guidelines on CVD prevention in clinical practice also recommends CVD risk stratification for patients with hypertension.
Practical approach for cardiovascular risk assessment and management in patients with rheumatoid arthritis. CV cardiovascular, SCORE Systematic COronary Risk Evaluation [23]
Other non-RA conditions should be considered, such as diabetes mellitus and chronic renal disease, as well as the presence of ongoing cancer treatments, periodontitis, obstructive sleep apnea syndrome, and erectile dysfunction. Family history, ethnicity, and psychosocial factors (e.g., socio-economic status, mood disorders), which may be of difficult quantification, should be considered as well. Body weight is generally measured by the body mass index (BMI), which is optimal between the values of 20.0 and 25.0 kg/m2. However, the use of BMI in RA patients may raise concerns, especially when therapy with glucocorticoids is long-standing body fat storing may be modified (e.g., Cushing-like syndrome). The waist circumference to quantify the body fat stored in the abdomen (intra-abdominal fat) may be a valuable choice in such patients [32]. On the other hand, RA cachexia due to long-lasting disease activity may be a major issue [33] and should be considered a CV risk factor as well.
The impact on CVD risk assessment of other biomarkers, such as inflammatory (e.g., high-sensitivity C-reactive protein, fibrinogen), lipid-related (e.g., apolipoproteins) and thrombotic biomarkers (e.g., homocysteine, lipoprotein-associated phospholipase A2) is still uncertain [34,35,36,37]. Genetic analysis for methylene-tetrahydrofolate reductase (MTHFR) mutation is not routinely recommended unless hyperhomocysteinemia is present because the former alone is not associated with CV risk [38].
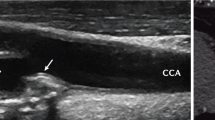
Many imaging tools such as coronary artery calcification by multi-slice computed tomography [39], intima–media thickness by carotid ultrasound [40], arterial stiffness with aortic pulse wave velocity or arterial augmentation index, ankle–brachial index [41,42,43], and echocardiography [44], have been proposed to measure subclinical vascular damage in RA. Among these, only carotid ultrasound has been included in EULAR recommendations for clinical practice, based on the evidence that carotid plaques in RA are associated with disease duration, disease activity, and ischemic heart disease with poor CVD-free survival [45,46,47]. Therefore, the routinely use of biomarkers/imaging tools regardless of first-screening CV risk assessment is not recommended in daily practice [22]. When present, unfavorable markers may be added to the general CVD risk assessment in order to guide therapy in specific situations (e.g., renal, cardiac biomarkers) or to adjust CVD risk assessment calculated by SCORE system.
When performing the SCORE risk assessment, clinicians should be aware of possible limitations in its use in RA patients. Cholesterol and triglycerides levels should be measured during the inactive phase of disease in order to limit the potential effect of systemic inflammation [48,49,50] or of concurrent therapy targeting disease remission [51, 52] on lipid profile. During active disease, the ratio of total cholesterol:high-density lipoprotein-cholesterol could be more reliable than the individual lipid parameters [53]. A re-assessment of CVD risk should be performed after achieving a stable control of disease activity. Furthermore, peculiar patterns of hypertension may be observed in active RA and approaches different from office blood pressure measurements (e.g., 24-h ambulatory monitoring) may be considered [54]. However, SCORE has not been yet validated in RA. Furthermore, as RA mainly affects women, CV risk may be underestimated even after the EULAR correction is applied. For example, young female patients may total a SCORE of 0, with a null effect of the 1.5 EULAR correction. In these cases, or when the SCORE is around thresholds, the detection of plaques by carotid ultrasound can be useful to raise the prediction of CVD in RA patients.
Coping with the Problem: Practical Management of CVD in RA
Prevention and Treatment of CVD in RA
Currently, there are no clinical trials specifically designed to define the optimal management of CVD co-morbidities in RA. Therefore, most interventions are extrapolated from studies and international guidelines on general population and based on expert opinion.
Prevention of Cardiovascular (CV) Disease in Rheumatoid Arthritis (RA): Lowering the Risk
CVD risk is expected to be lower when disease activity is properly controlled, since an association between inflammatory burden and CVD risk has been extensively reported in RA [55, 56]. The number and duration of disease flares over time seem to contribute to the risk of CVD, although disease duration does not seem to have an independent effect [55, 57]. Thus, chronic inflammation should be considered as a modifiable risk factor, and reduction of inflammation by disease-modifying antirheumatic drugs (DMARDs) plays a pivotal role in CVD risk management. In this view, an early diagnosis and an aggressive treatment of RA may contribute to control disease activity as well as to contain the CVD risk.
As in the general population, patients categorized at high or very high CV risk (e.g., SCORE ≥5% and >10%, respectively) should be promptly treated for existing CVD risk factors [16]. Regardless of risk level, all patients should receive lifestyle recommendations and be educated about the importance of regular exercise, healthy diet, and smoking cessation. Further to healthy lifestyle education, cognitive behavioral methods may improve compliance [58].
Physical inactivity may be a major issue in patients with RA, since it may contribute to raise the CVD risk [59]. Moreover, regular exercise has been shown to reduce inflammation in patients with RA, probably in relation with body fat [60]. Contraindications to high-intensity exercise have not been reported [61]. The ESC recommendations seem reasonable: at least 150 min a week of moderate-intensity or 75 min a week of vigorous-intensity aerobic physical activity [22]. Isotonic physical exercise may help to stimulate bone formation and reduce bone loss. To avoid the risk of falls in elderly patients, neuromotor exercise such as tai chi, yoga, and recreational activities, may be appropriate and may help in improving balance and motor skills.
Dietary habits, including specific dietary patterns such as a Mediterranean diet, have demonstrated to reduce CV risk [62] and also demonstrated to help control disease activity in RA [63]. Although there is no specific evidence on the effect on CVD risk in RA patients, EULAR recommends a Mediterranean diet to patients with RA [16]. A limited intake of sodium (optimal as low as 3 g/day) and an optimal intake of vitamin D and omega-3 acids (primarily from the diet) should be recommended as for the general population. Elevated serum levels of homocysteine have long been associated with the risk of CVD and stroke [64]. Homocysteine levels may be higher in patients treated with methotrexate, which is a folic acid antagonist that interferes with homocysteine metabolism by reducing the activity of MTHFR [65]. Although a recent Cochrane Review found no evidence to suggest that homocysteine-lowering interventions given alone or in combination could be effective in preventing CV events [66], in the course of treatment with methotrexate, we always recommend the dietary supplementation with folic acid.
Smoking cessation is mandatory in RA patients, as it is known to have a role in disease pathogenesis [67], and it is the most cost-effective strategy. Nicotine replacement therapy as well as electronic cigarettes might be considered for helping in smoking cessation [68]. Passive secondary smoking carries significant risk [69], and non-smoker RA patients need to receive protection.
There is no evidence that the management of hypertension and hyperlipidemia, as well as the treatment thresholds, should differ in RA patients as compared to non-RA patients [16]. However, it is evident that hypertension is underdiagnosed and undertreated in patients with RA [70]. Previous recommendations about the preferable use of angiotensin-converting enzyme inhibitor and angiotensin II receptor blockers have not been confirmed as the main benefits of blood-pressure-lowering treatment are expected to be due to lowering of blood pressure per se, and the choice of the drug should be guided by specific conditions (i.e., clinical CV events or asymptomatic organ damage such as microalbuminuria, left ventricular hypertrophy). Statins have been largely studied in RA patients and their efficacy in reducing cholesterol levels and CVD morbidity and mortality was reported to be similar when compared with non-RA controls with analogous adverse reactions [71]. Particularly, myalgia and rhabdomyolysis do not seem to be more frequent in RA patients than in the general population [72]. Moreover, statins have shown desirable anti-inflammatory properties, which have been advocated to have an effect on RA even greater when combined with DMARDs [73]. However, this overall effect needs to be confirmed and non-statin drugs may also be considered as valuable choices [74]. Finally, clinicians should always pay attention to the impact of anti-rheumatic drugs such as glucocorticoids (GC), non-steroidal anti-inflammatory drugs (NSAIDs), cyclosporine and leflunomide on hypertensive state, and lipid profile (e.g., tocilizumab, tofacitinib) when RA patients are evaluated [16].
As in the general population, anti-platelet therapy should not be routinely administered as primary prevention due to the lack of evidence and the increased risk of major bleeding, but should instead be given after an episode of myocardial infarction (MI), stroke, or peripheral artery disease following the guidelines for the general population [22].
Treatment of Cardiovascular (CV) Diseases in Rheumatoid Arthritis (RA): Ischemic Heart Disease and Heart Failure
Patterns of clinical care and disease-specific intervention may vary in patients with RA when compared with the general population. Although RA patients receive similar care to non-RA patients, outcomes are worse [12]. This may be due to undertreatment or underestimation of CV risk [70, 75]. Evidence from the general population demonstrates that women are often undertreated, probably due to the common belief that they are more protected by CV risk, which is delayed by 10 years [76]. This false belief may be particularly dangerous in patients with RA, which predominantly affects women in their third–fifth decades and leads to accelerated CV comorbidity and mortality. Furthermore, CVD in women often presents as MI associated with non-obstructive coronary arteries, spontaneous coronary artery dissection, heart failure with preserved ejection fraction, and peripheral arterial disease [76,77,78]. This could be a possible explanation of the less-effective treatment in RA patients and should be considered when choosing an intervention from the evidence coming from the general population, where men are more affected by CVD and specifically by atherosclerotic coronary artery disease. Apart from CV risk reduction and disease-specific interventions chosen after a careful consultation with an expert cardiologist, tight control of disease activity should be achieved with RA-specific treatment. According to regulatory agency safety warnings, in patients with severe congestive heart failure (New York Heart Association class III/IV), the use of a combination of conventional synthetic (cs)DMARDs with biological (b)DMARDs such as tumor necrosis factor-inhibitors (TNFi) or tofacitinib should be preferred over TNFi in patients [79]. However, due to the lack of univocal evidence, TNFi could probably be used safely in compensated heart failure or in the absence of other reasonable options.
Treatment of Patients with Rheumatoid Arthritis (RA): Considering Cardiovascular (CV) Risk
Remission or low disease activity are desirable in RA because control of systemic inflammation likely contributes to lower CV risk and mortality as well in patients with RA. The use of drugs that may increase CV risk should be limited. However, the type of treatment may be less important than reducing inflammation itself for CVD risk management in RA [19, 80]. In line with the most recent international recommendations, GC and csDMARDs are considered the first-line therapy to induce remission in RA and bDMARDs are the current mainstay of treatment of moderate-to-severe RA [81]. NSAIDs are considered a valuable yet supportive short-term treatment and their long-term use is usually discouraged (Table 3).
Non-Steroidal Anti-Inflammatory Drugs (NSAIDS) and Glucocorticoids (GC)
The long-term use of NSAIDs and GC has been associated with increased CV risk [14, 82]. Both non-selective and selective NSAIDs have adverse effects on CVD outcomes in patients with RA. Diclofenac is contraindicated in patients with documented CVD (congestive heart failure, ischemic heart disease, peripheral arterial disease, or cerebrovascular disease), and new evidence supports similar restrictions for ibuprofen use. Celecoxib (or low-dose GC) should be considered in patients treated with warfarin, other K-vitamin antagonists or clopidogrel. Recently, in a randomized controlled trial, in comparison with two widely used non-selective NSAIDs—naproxen and ibuprofen—celecoxib was non-inferior in CV safety and naproxen treatment did not result in better CV differently from previous studies [83]. Even acetaminophen, widely used as a safe analgesic may interfere with antihypertensive treatments [84]. As far as GC treatment is concerned, the daily and cumulative dose and the duration of treatment specifically associated with a high CVD risk have not been defined. However, it is advisable that the daily dose and treatment duration should be kept as low as possible [85].
Conventional Synthetic Disease-Modifying Anti-Rheumatic Drugs (csDMARDs)
The use of csDMARDs is associated with a reduction of CVD risk, particularly after long-term use [14]. Methotrexate is the csDMARDs of choice as part of the first treatment strategy in RA [81] and its use was shown to be associated with a reduction of CVD risk [86]. Beneficial effects of methotrexate on arterial stiffness as surrogate marker of CVD risk have also been described [87]. Among major csDMARDs, sulfasalazine showed to contribute to reduce CVD risk with lesser extent than methotrexate [88], yet data are sparse consistently with its limited use in RA. Interestingly, hydroxychloroquine showed to improve lipid profile and to reduce the risk of diabetes [89, 90]. Finally, cyclosporine and leflunomide are well known to have a role in development of hypertension and their use should be avoided in RA patients, especially when high blood pressure is documented [91, 92].
Biological Disease-Modifying Anti-Rheumatic Drugs (bDMARDs)
The use of bDMARDs, such as the TNFi, is associated with a significant reduction in CVD risk in patients with RA, in particular in those who respond to TNFi treatment [93, 94]. These observations further support the view that the reduction in CV risk is due to tight control of inflammation. Effects on surrogate marker for CVD (e.g., carotid intima media thickness, arterial stiffness) were described in patients treated with TNFi and non-TNFi, such as tocilizumab and rituximab [95,96,97,98,99,100,101]. The lipid increasing effect of bDMARDs is known and lipid assessment during treatment, particularly with tocilizumab, is mandatory [102]. However, the impact of these changes on CVD outcomes is still to be defined, also in view of the overall safe profile of these drugs [19, 80]. An overall increase of lipid components was observed when using TNFi and/or csDMARDs, but this may be counterbalanced by an anti-atherogenic lipid profile due to the improvement of the ratio between total cholesterol (TC) and HDL [50]. Rituximab and tocilizumab (and probably tofacitinib) are associated with an overall increase of individual lipid components without changes in TC/HDL ratio, yet with no observed increase in CVD risk [80]. In specific cases, statins are effective in reducing lipid levels in patients receiving such treatments [102].
Conclusions
Epidemiologic data demonstrate that CVD risk is increased in RA patients compared to the general population. Likely, this is due to common underlying pathogenetic mechanisms. Control of chronic inflammation is one of the targets to ameliorate CV risk profile in RA patients. Therefore, all RA patients should be assessed for CVD risk to warrant an appropriate management and to implement early strategies of prevention. First-line screening assessment with SCORE could be enough in daily clinical practice to identify high-risk patients and to avoid delayed treatment of RA patients, although it has not yet been validated in RA and has some limitations. Anti-inflammatory therapies and other non-traditional CV risk factors should be considered in CVD risk assessment and outcomes of therapies. Particularly, the choice of therapy should also be based on the CV risk of each patient. Further studies are needed to understand if CV comorbidities in RA patients should be treated differently from the general population. Rheumatologists should ensure CV risk assessment and an optimal targeted management of RA, but also should cooperate with cardiologists, general practitioners, and other specialists in a multidisciplinary setting.
References
Smolen JS, Aletaha D, McInnes IB. Rheumatoid arthritis. Lancet. 2016;388(10055):2023–38.
Dadoun S, Zeboulon-Ktorza N, Combescure C, Elhai M, Rozenberg S, Gossec L, et al. Mortality in rheumatoid arthritis over the last fifty years: systematic review and meta-analysis. Joint Bone Spine. 2013;80(1):29–33.
Sen D, Gonzalez-Mayda M, Brasington RD Jr. Cardiovascular disease in rheumatoid arthritis. Rheum Dis Clin North Am. 2014;40(1):27–49.
Nurmohamed MT, Heslinga M, Kitas GD. Cardiovascular comorbidity in rheumatic diseases. Nat Rev Rheumatol. 2015;11(12):693–704.
Hollan I, Meroni PL, Ahearn JM, Cohen Tervaert JW, Curran S, Goodyear CS, et al. Cardiovascular disease in autoimmune rheumatic diseases. Autoimmun Rev. 2013;12(10):1004–15.
Houri Levi E, Watad A, Whitby A, Tiosano S, Comaneshter D, Cohen AD, et al. Coexistence of ischemic heart disease and rheumatoid arthritis patients—a case control study. Autoimmun Rev. 2016;15(4):393–6.
Avina-Zubieta JA, Thomas J, Sadatsafavi M, Lehman AJ, Lacaille D. Risk of incident cardiovascular events in patients with rheumatoid arthritis: a meta-analysis of observational studies. Ann Rheum Dis. 2012;71(9):1524–9.
Meune C, Touze E, Trinquart L, Allanore Y. Trends in cardiovascular mortality in patients with rheumatoid arthritis over 50 years: a systematic review and meta-analysis of cohort studies. Rheumatology (Oxford). 2009;48(10):1309–13.
Baghdadi LR, Woodman RJ, Shanahan EM, Mangoni AA. The impact of traditional cardiovascular risk factors on cardiovascular outcomes in patients with rheumatoid arthritis: a systematic review and meta-analysis. PLoS One. 2015;10(2):e0117952.
Lindhardsen J, Ahlehoff O, Gislason GH, Madsen OR, Olesen JB, Torp-Pedersen C, et al. The risk of myocardial infarction in rheumatoid arthritis and diabetes mellitus: a Danish nationwide cohort study. Ann Rheum Dis. 2011;70(6):929–34.
Maradit-Kremers H, Crowson CS, Nicola PJ, Ballman KV, Roger VL, Jacobsen SJ, et al. Increased unrecognized coronary heart disease and sudden deaths in rheumatoid arthritis: a population-based cohort study. Arthritis Rheum. 2005;52(2):402–11.
Davis JM 3rd, Roger VL, Crowson CS, Kremers HM, Therneau TM, Gabriel SE. The presentation and outcome of heart failure in patients with rheumatoid arthritis differs from that in the general population. Arthritis Rheum. 2008;58(9):2603–11.
Greulich S, Kitterer D, Kurmann R, Henes J, Latus J, Gloekler S, et al. Cardiac involvement in patients with rheumatic disorders: data of the RHEU-M(A)R study. Int J Cardiol. 2016;224:37–49.
Roubille C, Richer V, Starnino T, McCourt C, McFarlane A, Fleming P, et al. The effects of tumour necrosis factor inhibitors, methotrexate, non-steroidal anti-inflammatory drugs and corticosteroids on cardiovascular events in rheumatoid arthritis, psoriasis and psoriatic arthritis: a systematic review and meta-analysis. Ann Rheum Dis. 2015;74(3):480–9.
Myasoedova E, Gabriel SE, Matteson EL, Davis JM 3rd, Therneau TM, Crowson CS. Decreased cardiovascular mortality in patients with incident Rheumatoid Arthritis (RA) in recent years: dawn of a new era in cardiovascular disease in RA? J Rheumatol. 2017;44(6):732–39.
Agca R, Heslinga SC, Rollefstad S, Heslinga M, McInnes IB, Peters MJ, et al. EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis. 2017;76(1):17–28.
Durante A, Bronzato S. The increased cardiovascular risk in patients affected by autoimmune diseases: review of the various manifestations. J Clin Med Res. 2015;7(6):379–84.
van den Oever IA, Sattar N, Nurmohamed MT. Thromboembolic and cardiovascular risk in rheumatoid arthritis: role of the haemostatic system. Ann Rheum Dis. 2014;73(6):954–7.
Cugno M, Ingegnoli F, Gualtierotti R, Fantini F. Potential effect of anti-tumour necrosis factor-alpha treatment on reducing the cardiovascular risk related to rheumatoid arthritis. Curr Vasc Pharmacol. 2010;8(2):285–92.
Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473(7347):317–25.
Cambridge G, Acharya J, Cooper JA, Edwards JC, Humphries SE. Antibodies to citrullinated peptides and risk of coronary heart disease. Atherosclerosis. 2013;228(1):243–6.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention and Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–81.
Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24(11):987–1003.
Hollan I, Dessein PH, Ronda N, Wasko MC, Svenungsson E, Agewall S, et al. Prevention of cardiovascular disease in rheumatoid arthritis. Autoimmun Rev. 2015;14(10):952–69.
Arts EE, Popa CD, Den Broeder AA, Donders R, Sandoo A, Toms T, et al. Prediction of cardiovascular risk in rheumatoid arthritis: performance of original and adapted SCORE algorithms. Ann Rheum Dis. 2016;75(4):674–80.
Solomon DH, Greenberg J, Curtis JR, Liu M, Farkouh ME, Tsao P, et al. Derivation and internal validation of an expanded cardiovascular risk prediction score for rheumatoid arthritis: a Consortium of Rheumatology Researchers of North America Registry Study. Arthritis Rheumatol. 2015;67(8):1995–2003.
Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, Minhas R, Sheikh A, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008;336(7659):1475–82.
Wiersma T, Smulders YM, Stehouwer CD, Konings KT, Lanphen J. Summary of the multidisciplinary guideline on cardiovascular risk management (revision 2011). Ned Tijdschr Geneeskd. 2012;156(36):A5104.
Ingegnoli F, Castelli R, Gualtierotti R. Rheumatoid factors: clinical applications. Dis Markers. 2013;35(6):727–34.
Crowson CS, Gabriel SE, Semb AG, van Riel PL, Karpouzas G, Dessein PH et al. Rheumatoid arthritis-specific cardiovascular risk scores are not superior to general risk scores: a validation analysis of patients from seven countries. Rheumatology (Oxford). 2017.
Ray KK, Kastelein JJ, Boekholdt SM, Nicholls SJ, Khaw KT, Ballantyne CM, et al. The ACC/AHA 2013 guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: the good the bad and the uncertain: a comparison with ESC/EAS guidelines for the management of dyslipidaemias 2011. Eur Heart J. 2014;35(15):960–8.
Giles JT, Allison M, Blumenthal RS, Post W, Gelber AC, Petri M, et al. Abdominal adiposity in rheumatoid arthritis: association with cardiometabolic risk factors and disease characteristics. Arthritis Rheum. 2010;62(11):3173–82.
Okano T, Inui K, Tada M, Sugioka Y, Mamoto K, Wakitani S, Koike T, Nakamura H. Loss of lean body mass affects low bone mineral density in patients with rheumatoid arthritis - results from the TOMORROW study. Mod Rheumatol. 2017:1–7. doi:10.1080/14397595.2017.1289645.
Yang X, Gao F, Liu Y. Association of homocysteine with immunological-inflammatory and metabolic laboratory markers and factors in relation to hyperhomocysteinaemia in rheumatoid arthritis. Clin Exp Rheumatol. 2015;33(6):900–3.
Sodergren A, Karp K, Bengtsson C, Moller B, Rantapaa-Dahlqvist S, Wallberg-Jonsson S. Is lipoprotein-associated phospholipase A2 a link between inflammation and subclinical atherosclerosis in rheumatoid arthritis? Biomed Res Int. 2015;2015:673018.
Kim JY, Lee EY, Park JK, Song YW, Kim JR, Cho KH. Patients with rheumatoid arthritis show altered lipoprotein profiles with dysfunctional high-density lipoproteins that can exacerbate inflammatory and atherogenic process. PLoS One. 2016;11(10):e0164564.
Montecucco F, Favari E, Norata GD, Ronda N, Nofer JR, Vuilleumier N. Impact of systemic inflammation and autoimmune diseases on apoA-I and HDL plasma levels and functions. Handb Exp Pharmacol. 2015;224:455–82.
Haemostasis, Thrombosis Task Force BCfSiH. Investigation and management of heritable thrombophilia. Br J Haematol. 2001;114(3):512–28.
Liu JH, Ng MY, Cheung T, Chung HY, Chen Y, Zhen Z, et al. Ten-year progression of coronary artery, carotid artery, and aortic calcification in patients with rheumatoid arthritis. Clin Rheumatol. 2017;36(4):807–16.
Ambrosino P, Lupoli R, Di Minno A, Tasso M, Peluso R, Di Minno MN. Subclinical atherosclerosis in patients with rheumatoid arthritis. A meta-analysis of literature studies. Thromb Haemost. 2015;113(5):916–30.
Scanlon EM, Mankad R, Crowson CS, Kullo IJ, Mulvagh SL, Matteson EL, et al. Cardiovascular risk assessment in patients with rheumatoid arthritis: a correlative study of noninvasive arterial health testing. Clin Rheumatol. 2017;36(4):763–71.
Ikdahl E, Rollefstad S, Wibetoe G, Olsen IC, Berg IJ, Hisdal J, et al. Predictive value of arterial stiffness and subclinical carotid atherosclerosis for cardiovascular disease in patients with rheumatoid arthritis. J Rheumatol. 2016;43(9):1622–30.
Ozturk K. Arterial stiffness and ankle brachial index in patients with rheumatoid arthritis and inflammatory bowel disease. J Inflamm (Lond). 2016;13:2.
Al-Mohaissen MA, Chan KL. Echocardiography in the assessment of patients with rheumatologic diseases. Curr Cardiol Rep. 2016;18(8):72.
Pope JE, Nevskaya T, Barra L, Parraga G. Carotid artery atherosclerosis in patients with active rheumatoid arthritis: predictors of plaque occurrence and progression over 24 weeks. Open Rheumatol J. 2016;10:49–59.
Im CH, Kim NR, Kang JW, Kim JH, Kang JY, Bae GB, et al. Inflammatory burden interacts with conventional cardiovascular risk factors for carotid plaque formation in rheumatoid arthritis. Rheumatology (Oxford). 2015;54(5):808–15.
Evans MR, Escalante A, Battafarano DF, Freeman GL, O’Leary DH, del Rincon I. Carotid atherosclerosis predicts incident acute coronary syndromes in rheumatoid arthritis. Arthritis Rheum. 2011;63(5):1211–20.
Myasoedova E, Crowson CS, Kremers HM, Roger VL, Fitz-Gibbon PD, Therneau TM, et al. Lipid paradox in rheumatoid arthritis: the impact of serum lipid measures and systemic inflammation on the risk of cardiovascular disease. Ann Rheum Dis. 2011;70(3):482–7.
Boyer JF, Bongard V, Cantagrel A, Jamard B, Gottenberg JE, Mariette X, et al. Link between traditional cardiovascular risk factors and inflammation in patients with early arthritis: results from a French multicenter cohort. Arthritis Care Res (Hoboken). 2012;64(6):872–80.
Liao KP, Diogo D, Cui J, Cai T, Okada Y, Gainer VS, et al. Association between low density lipoprotein and rheumatoid arthritis genetic factors with low density lipoprotein levels in rheumatoid arthritis and non-rheumatoid arthritis controls. Ann Rheum Dis. 2014;73(6):1170–5.
de Groot L, Jager NA, Westra J, Smit AJ, Kallenberg CG, Posthumus MD, et al. Does reduction of disease activity improve early markers of cardiovascular disease in newly diagnosed rheumatoid arthritis patients? Rheumatology (Oxford). 2015;54(7):1257–61.
Filippatos TD, Derdemezis CS, Voulgari PV, Tsimihodimos V, Elisaf MS, Tselepis AD, et al. Effects of 12 months of treatment with disease-modifying anti-rheumatic drugs on low and high density lipoprotein subclass distribution in patients with early rheumatoid arthritis: a pilot study. Scand J Rheumatol. 2013;42(3):169–75.
Choy E, Sattar N. Interpreting lipid levels in the context of high-grade inflammatory states with a focus on rheumatoid arthritis: a challenge to conventional cardiovascular risk actions. Ann Rheum Dis. 2009;68(4):460–9.
Hamamoto K, Yamada S, Yasumoto M, Yoda M, Yoda K, Tsuda A, et al. Association of nocturnal hypertension with disease activity in rheumatoid arthritis. Am J Hypertens. 2016;29(3):340–7.
Arts EE, Fransen J, den Broeder AA, Popa CD, van Riel PL. The effect of disease duration and disease activity on the risk of cardiovascular disease in rheumatoid arthritis patients. Ann Rheum Dis. 2015;74(6):998–1003.
Myasoedova E, Chandran A, Ilhan B, Major BT, Michet CJ, Matteson EL, et al. The role of rheumatoid arthritis (RA) flare and cumulative burden of RA severity in the risk of cardiovascular disease. Ann Rheum Dis. 2016;75(3):560–5.
Zhang J, Chen L, Delzell E, Muntner P, Hillegass WB, Safford MM, et al. The association between inflammatory markers, serum lipids and the risk of cardiovascular events in patients with rheumatoid arthritis. Ann Rheum Dis. 2014;73(7):1301–8.
John H, Hale ED, Treharne GJ, Kitas GD, Carroll D. A randomized controlled trial of a cognitive behavioural patient education intervention vs a traditional information leaflet to address the cardiovascular aspects of rheumatoid disease. Rheumatology (Oxford). 2013;52(1):81–90.
Hernandez-Hernandez V, Ferraz-Amaro I, Diaz-Gonzalez F. Influence of disease activity on the physical activity of rheumatoid arthritis patients. Rheumatology (Oxford). 2014;53(4):722–31.
Metsios GS, Stavropoulos-Kalinoglou A, Veldhuijzen van Zanten JJ, Nightingale P, Sandoo A, Dimitroulas T, et al. Individualised exercise improves endothelial function in patients with rheumatoid arthritis. Ann Rheum Dis. 2014;73(4):748–51.
Lemmey AB, Marcora SM, Chester K, Wilson S, Casanova F, Maddison PJ. Effects of high-intensity resistance training in patients with rheumatoid arthritis: a randomized controlled trial. Arthritis Rheum. 2009;61(12):1726–34.
Estruch R, Ros E, Martinez-Gonzalez MA. Mediterranean diet for primary prevention of cardiovascular disease. N Engl J Med. 2013;369(7):676–7.
Skoldstam L, Hagfors L, Johansson G. An experimental study of a Mediterranean diet intervention for patients with rheumatoid arthritis. Ann Rheum Dis. 2003;62(3):208–14.
Wald DS, Law M, Morris JK. Homocysteine and cardiovascular disease: evidence on causality from a meta-analysis. BMJ. 2002;325(7374):1202.
Grosflam J, Weinblatt ME. Methotrexate: mechanism of action, pharmacokinetics, clinical indications, and toxicity. Curr Opin Rheumatol. 1991;3(3):363–8.
Marti-Carvajal AJ, Sola I, Lathyris D. Homocysteine-lowering interventions for preventing cardiovascular events. Cochrane Database Syst Rev. 2015;1:CD006612.
Anderson R, Meyer PW, Ally MM, Tikly M. Smoking and air pollution as pro-inflammatory triggers for the development of rheumatoid arthritis. Nicotine Tob Res. 2016;18(7):1556–65.
Bullen C, Howe C, Laugesen M, McRobbie H, Parag V, Williman J, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382(9905):1629–37.
Law MR, Morris JK, Wald NJ. Environmental tobacco smoke exposure and ischaemic heart disease: an evaluation of the evidence. BMJ. 1997;315(7114):973–80.
Protogerou AD, Panagiotakos DB, Zampeli E, Argyris AA, Arida K, Konstantonis GD, et al. Arterial hypertension assessed “out-of-office” in a contemporary cohort of rheumatoid arthritis patients free of cardiovascular disease is characterized by high prevalence, low awareness, poor control and increased vascular damage-associated “white coat” phenomenon. Arthritis Res Ther. 2013;15(5):R142.
Semb AG, Kvien TK, DeMicco DA, Fayyad R, Wun CC, LaRosa JC, et al. Effect of intensive lipid-lowering therapy on cardiovascular outcome in patients with and those without inflammatory joint disease. Arthritis Rheum. 2012;64(9):2836–46.
Buettner C, Rippberger MJ, Smith JK, Leveille SG, Davis RB, Mittleman MA. Statin use and musculoskeletal pain among adults with and without arthritis. Am J Med. 2012;125(2):176–82.
Lv S, Liu Y, Zou Z, Li F, Zhao S, Shi R, et al. The impact of statins therapy on disease activity and inflammatory factor in patients with rheumatoid arthritis: a meta-analysis. Clin Exp Rheumatol. 2015;33(1):69–76.
Danninger K, Hoppe UC, Pieringer H. Do statins reduce the cardiovascular risk in patients with rheumatoid arthritis? Int J Rheum Dis. 2014;17(6):606–11.
Francis ML, Varghese JJ, Mathew JM, Koneru S, Scaife SL, Zahnd WE. Outcomes in patients with rheumatoid arthritis and myocardial infarction. Am J Med. 2010;123(10):922–8.
Garcia M, Mulvagh SL, Merz CN, Buring JE, Manson JE. Cardiovascular disease in women: clinical perspectives. Circ Res. 2016;118(8):1273–93.
Crea F, Camici PG, Bairey Merz CN. Coronary microvascular dysfunction: an update. Eur Heart J. 2014;35(17):1101–11.
Kobayshi H, Kobayashi Y, Yokoe I, Akashi Y, Takei M, Giles JT. Magnetic resonance-detected myocardial inflammation and fibrosis in rheumatoid arthritis: associations of disease characteristics and N-terminal pro Brain Natriuretic peptide levels. Arthritis Care Res (Hoboken). 2016.
Singh JA, Saag KG, Bridges SL Jr, Akl EA, Bannuru RR, Sullivan MC, et al. 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken). 2016;68(1):1–25.
Gualtierotti R. Understanding cardiovascular risk in rheumatoid arthritis: still a long way to go. Atherosclerosis. 2017;256:123–4.
Smolen JS, Landewé R, Bijlsma J, Burmester G, Chatzidionysiou K, Dougados M, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis. 2017;76(6):960–77.
del Rincon I, Battafarano DF, Restrepo JF, Erikson JM, Escalante A. Glucocorticoid dose thresholds associated with all-cause and cardiovascular mortality in rheumatoid arthritis. Arthritis Rheumatol. 2014;66(2):264–72.
Nissen SE, Yeomans ND, Solomon DH, Luscher TF, Libby P, Husni ME, et al. Cardiovascular safety of celecoxib, naproxen, or ibuprofen for arthritis. N Engl J Med. 2016;375(26):2519–29.
Gualtierotti R, Zoppi A, Mugellini A, Derosa G, D’Angelo A, Fogari R. Effect of naproxen and acetaminophen on blood pressure lowering by ramipril, valsartan and aliskiren in hypertensive patients. Expert Opin Pharmacother. 2013;14(14):1875–84.
van Sijl AM, Boers M, Voskuyl AE, Nurmohamed MT. Confounding by indication probably distorts the relationship between steroid use and cardiovascular disease in rheumatoid arthritis: results from a prospective cohort study. PLoS One. 2014;9(1):e87965.
Micha R, Imamura F, Wyler von Ballmoos M, Solomon DH, Hernan MA, Ridker PM, et al. Systematic review and meta-analysis of methotrexate use and risk of cardiovascular disease. Am J Cardiol. 2011;108(9):1362–70.
Ajeganova S, de Faire U, Jogestrand T, Frostegard J, Hafstrom I. Carotid atherosclerosis, disease measures, oxidized low-density lipoproteins, and atheroprotective natural antibodies for cardiovascular disease in early rheumatoid arthritis—an inception cohort study. J Rheumatol. 2012;39(6):1146–54.
van Halm VP, Nurmohamed MT, Twisk JW, Dijkmans BA, Voskuyl AE. Disease-modifying antirheumatic drugs are associated with a reduced risk for cardiovascular disease in patients with rheumatoid arthritis: a case control study. Arthritis Res Ther. 2006;8(5):R151.
Kerr G, Aujero M, Richards J, Sayles H, Davis L, Cannon G, et al. Associations of hydroxychloroquine use with lipid profiles in rheumatoid arthritis: pharmacologic implications. Arthritis Care Res (Hoboken). 2014;66(11):1619–26.
Wasko MC, Hubert HB, Lingala VB, Elliott JR, Luggen ME, Fries JF, et al. Hydroxychloroquine and risk of diabetes in patients with rheumatoid arthritis. JAMA. 2007;298(2):187–93.
Kellner H, Bornholdt K, Hein G. Leflunomide in the treatment of patients with early rheumatoid arthritis–results of a prospective non-interventional study. Clin Rheumatol. 2010;29(8):913–20.
Robert N, Wong GW, Wright JM. Effect of cyclosporine on blood pressure. Cochrane Database Syst Rev. 2010;(1):CD007893. doi:10.1002/14651858.CD007893.pub2.
Bili A, Tang X, Pranesh S, Bozaite R, Morris SJ, Antohe JL, et al. Tumor necrosis factor alpha inhibitor use and decreased risk for incident coronary events in rheumatoid arthritis. Arthritis Care Res (Hoboken). 2014;66(3):355–63.
Ljung L, Rantapaa-Dahlqvist S, Jacobsson LT, Askling J. Response to biological treatment and subsequent risk of coronary events in rheumatoid arthritis. Ann Rheum Dis. 2016;75(12):2087–94.
Rao VU, Pavlov A, Klearman M, Musselman D, Giles JT, Bathon JM, et al. An evaluation of risk factors for major adverse cardiovascular events during tocilizumab therapy. Arthritis Rheumatol. 2015;67(2):372–80.
Benucci M, Saviola G, Manfredi M, Sarzi-Puttini P, Atzeni F. Factors correlated with improvement of endothelial dysfunction during rituximab therapy in patients with rheumatoid arthritis. Biologics. 2013;7:69–75.
Vassilopoulos D, Gravos A, Vlachopoulos C, Kandili A, Ioakeimidis N, Pectasides D, et al. Adalimumab decreases aortic stiffness independently of its effect in disease activity in patients with rheumatoid arthritis. Clin Rheumatol. 2015;34(2):359–64.
Ingegnoli F, Fantini F, Favalli EG, Soldi A, Griffini S, Galbiati V, et al. Inflammatory and prothrombotic biomarkers in patients with rheumatoid arthritis: effects of tumor necrosis factor-alpha blockade. J Autoimmun. 2008;31(2):175–9.
Ingegnoli F, Fantini F, Griffini S, Soldi A, Meroni PL, Cugno M. Anti-tumor necrosis factor alpha therapy normalizes fibrinolysis impairment in patients with active rheumatoid arthritis. Clin Exp Rheumatol. 2010;28(2):254–7.
Gualtierotti R, Ingegnoli F, Griffini S, Grovetti E, Meroni PL, Cugno M. Prothrombotic biomarkers in patients with rheumatoid arthritis: the beneficial effect of IL-6 receptor blockade. Clin Exp Rheumatol. 2016;34(3):451–8.
Bacchiega BC, Bacchiega AB, Usnayo MJ, Bedirian R, Singh G, Pinheiro GD. Interleukin 6 inhibition and coronary artery disease in a high-risk population: a prospective community-based clinical study. J Am Heart Assoc. 2017;6(3). doi:10.1161/JAHA.116.005038.
Souto A, Salgado E, Maneiro JR, Mera A, Carmona L, Gomez-Reino JJ. Lipid profile changes in patients with chronic inflammatory arthritis treated with biologic agents and tofacitinib in randomized clinical trials: a systematic review and meta-analysis. Arthritis Rheumatol. 2015;67(1):117–27.
Acknowledgements
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Financial Disclosures
Roberta Gualtierotti, Nicola Ughi, Giovanni Marfia and Francesca Ingegnoli have no relevant financial relationships to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article has associated CME accreditation, valid until July 2018. Please follow this link to access the activity: https://rheumatology.medicinematters.com/journal-article-cme/.
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/6E98F0600035D73E.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Gualtierotti, R., Ughi, N., Marfia, G. et al. Practical Management of Cardiovascular Comorbidities in Rheumatoid Arthritis. Rheumatol Ther 4, 293–308 (2017). https://doi.org/10.1007/s40744-017-0068-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-017-0068-0