Abstract
Psychosocial interventions play an unclear complex role within maintenance treatment for opioid addiction. In this study, the hypothesis was that manualized psychosocial treatment was more effective than psychosocial treatment as usual. Moreover, the question was to find subgroups of patients who do not need or benefit from enhanced psychosocial treatment. The study design contains two manualized treatment groups and a control group of treatment as usual. There are two randomizations: (1) From the beginning, all patients were randomized to methadone or buprenorphine. (2) After having finished the control group treatment-as-usual, the subsequent patients were in addition randomly allocated to basic treatment or indicative treatment. From 122 patients in 3 treatment centers, 64 could be reached at the 1-year follow-up. Measurement instruments were the EuropASI, SCL-90, and documentation standards. Primary outcome criteria were drug consumption in the follow-up period of 6 months; secondary outcome criteria included individual changes in the EuropASI composite scores and the SCL-90 scales. Regarding hard drugs (all illegal drugs except cannabis, but including non-prescribed tranquilizers) the proportion of patient without use of drugs in the last 30 days increased from 1.9 % at intake to 54.7 % in the last month of the follow-up period without differences in the 3 psychosocial treatment groups. 76.1 % of those patients with at least one increased T-value (>60) in any of the 9 SCL scales showed at least one positive individual change in the follow-up period, whereas only 12.5 % of those with no increased T-value showed any positive changes. Regarding the use of hard drugs in the follow-up no psychosocial treatment was superior. The flexibility of psychosocial treatment as to meeting individual needs of the patients seems to be crucial. Those patients without a higher SCL-90 T-score may not require an intensive psychosocial treatment package.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background and Aims
Opioid maintenance and psychosocial treatment are both considered to be essential components in the long-term treatment of opioid addicts. However, although many studies exist about the effects of the opioid agonists methadone and buprenorphine (see [7, 8, 17–20, 35, 36, 39], among others), the psychosocial component of maintenance treatment was evaluated much less [2, 3, 27]. In a meta-analytic review of psychosocial interventions in illegal drug addiction [6], the effect sizes d of psychosocial interventions for opioid addiction and multiple substance abuse were .39 and .24, respectively, and were lower than those for cannabis (d = .81) and cocaine (d = .62). In a Cochrane review by [1], psychosocial treatment in combination with substitution treatment had a relative risk of .69 regarding use of heroine, but this effect was significant only during treatment. Of five different psychosocial interventions, only contingency management (reinforcement) showed a significant effect. Furthermore, the recent updated review on psychosocial interventions [2] found no difference between maintenance treatment with psychosocial interventions and control groups with maintenance treatment as usual with minimal psychosocial interventions. Regarding detoxification, psychosocial interventions had a positive effect on retention and suppression of opiate use, but no specific intervention could be proven as a single significant influencing factor [3]. Different studies have confirmed the effectiveness of contingency management during treatment, but not in later stages [26–28]. Motivational interviewing seems to enhance motivation and retention rate and to reduce of heroin use [30]. The impact of relapse training, social skills training, cognitive behavioral treatment, vocational treatment, and family therapy have been investigated [6], but their additional specific effects remain unclear [2–4].
At present, psychosocial treatment does not appear to be necessary for every patient during substitution treatment, but it may provide additional help for different subgroups of patients [39]. The challenge, therefore, is to identify the subgroups of patients who in particular require psychosocial interventions. An alternative approach would be to give every patient at least some psychosocial treatment during maintenance substitution treatment. For those with special deficits, problems, or disorders additional and more intensive help would be needed [22]. Another aspect of the indication issue is to assess subgroups of patients who neither need nor would benefit from psychosocial interventions.
In Germany, most treatment centers for substitution maintenance treatment offer psychosocial intervention in addition to replacement therapy which is also required by federal regulations. However, the components and intensity of psychosocial treatment differ greatly between centers. In many treatment centers, psychosocial interventions at the beginning of substitution treatment deal primarily with individual crisis interventions in order to prevent the negative consequences of criminal convictions, housing issues, and job and partner problems [17].
Psychosocial Treatment
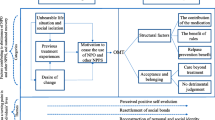
The manualized psychosocial treatment administered in the project consists of six main tasks [16]: (1) To clarify problems, aims and the motivation to cope with psychosocial problems and to change critical behavior partly through crisis interventions; (2) to help patients cope with drugs and to control their use according to the treatment aims and the patients’ conception of their lifestyle, which usually means abstinence from drugs, at least from hard drugs; (3) to stabilize the patients’ social situation, i.e. to cope with problems in areas of everyday life, including housing and the financial and work situation; (4) to solve problems and deficits in psychological functioning, which means the appropriate regulation of emotions, the perception of social reality including empathy in social relationships and asserting one’s own aims and goals; (5) to improve social relationships and to solve social conflicts and problems; (6) to conclude what has been accomplished and what has to be done in the near future. The general theory as background is based on the model of common factors in psychotherapy by [12], which are called (1) problem actuation, (2) motivation clarification, (3) personal resources activation, (4) mastery: help to cope with problems and (5) the therapist-patient relationship as a comprehensive factor (therapeutic alliance).
Not only because of comorbidity of the DSM-IV axis I or axis II disorders, most patients in substitution treatment would require psychosocial support to improve their quality of life, stabilize their goals and motivation for abstinence apart from the substitution drugs and to reduce their drug consumption to a more moderate level. Usually, axis I comorbid disorders need specific treatment besides addiction treatment. Some axis I disorders like major depression, and phobic or anxiety disorders may be regarded as reactive or consequential to the addiction disorder. We hypothesized that matching patient problem profiles, e.g. assessed by the EuropASI severity ratings, to different interventions (additional modules for everyday life coping, affect regulation and social relationships), would improve retention and treatment outcome compared to a global package of basic treatment. This type of matching procedure is based on the approach of McLellan et al. [25] who gave those patients with severe problems in the areas of employment, family or psychiatric problems (addiction severity index) three individual sessions focused on these target problems. The matched patients had a better treatment outcome than the mismatched.
The evaluation of psychosocial treatment for opiate addicts is a challenge for all participants: for the patient to be confronted with systematic psychosocial components and assessments; for the therapists committed to perform manualized treatment components in a complex individualized way; and for the researcher being in the role of an evaluator trying to control the psychosocial treatment process and data collection and to motivate the therapists to perform treatment according to the study protocol and treatment manual.
Aims
The effect of different substitution substances was analyzed in an earlier publication of this project [33]. The current study focused on four main questions regarding psychosocial treatment effects:
-
1.
What is the outcome of opioid addicts 1 year after starting substitution treatment and 6 months after completing manualized psychosocial treatment?
-
2.
Is manualized psychosocial treatment (basic and indicative treatment) more effective than treatment as usual?
-
3.
Is the indicative treatment approach more effective than the basic treatment approach?
-
4.
Is there a subgroup of patients who neither need nor benefit from psychosocial treatment?
Besides the change in average scores of different instruments used to assess treatment effects, the analysis of individual changes in test scales should give a more differentiated picture of the change processes, including negative changes.
Methods
Study Design
The study was a complex factorial design (see also Table 1). Details of the study and overall outcome of patients maintained on methadone or buprenorphine have been reported elsewhere [15, 33]. (1) It was a randomized controlled trial in relation to substitution substances (methadone or buprenorphine) for all three treatment groups: Treatment as usual (as a control group), manualized basic treatment, and manualized indicative treatment. (2) It was a quasi-experimental approach in relation to the control group of treatment-as-usual which was carried out before the two experimental groups started in the same 3 treatment centres and with the same medical management and performed by the same therapists. (3) It was an additional second randomized controlled trial of patients in relation to basic and indicative psychosocial treatment.
Psychosocial treatment was performed for 6 months, and patients were followed up for an additional 6 months. Substitution treatment was established and continued over this 1-year period.
The study design and protocol were approved by the ethics committee of the Ludwig Maximilian University, Munich and by the German Society of Psychology.
Treatment Factors
One treatment factor was substitution treatment with two arms: methadone or buprenorphine. The second treatment factor was psychosocial treatment consisting of three arms: (1) treatment as usual, (2) manualized basic treatment, or (3) manualized indicative treatment. Arm 2 and 3 were randomized as to opioid agonists and additionally to psychosocial treatment, whereas treatment as usual was carried out before the other two treatments started and was only randomized regarding opioid agonists.
Therapists were given training for 2 days in how to apply the manualized treatments, and initial training was followed by a booster session after 4 weeks. Furthermore, every 14 days one of the authors supervised the therapists during manualized treatments. Planned individual treatment sessions were conducted once per week for 6 months, with additional crisis interventions if necessary. Therapist completed a self-rating questionnaire to assess their experiences with the two manualized treatments.
The management of relapses regarding sanctions or treatment discharge was not controlled by the treatment manual. The treatment centers had their own more or less rigorous or liberal way of dealing with relapses (stepped sanctions) which was not changed throughout the project.
The matching procedure for those in the indicative treatment group:
If the patient‘s severity rating in the EuropASI is between 6 (treatment necessary) and 9 (treatment absolutely necessary) in one of the following domains, the patient is allocated to the corresponding treatment component.
-
Work/Living situation: Daily Life Activities (3 individual sessions)
-
Psychiatric Status: Resources Activation (5 individual sessions)
-
Familiy/social contacts: (Coping with family and other social conflicts 5–6 group sessions)
Outcome Criteria
Primary outcome criteria were drug consumption during follow-up, in particular in the last months of the follow-up period. Within drug consumption, all illegal drugs excluding cannabis but including tranquilizers not prescribed are distinguished from the soft drugs cannabis and alcohol. Secondary outcome criteria were the EuropASI composite scores (besides drug consumption) and changes in the SCL-90 scales as criteria of subjective strain regarding psychopathological symptoms.
Patient Samples
According to the study protocol, each new patient offered maintenance substitution treatment at one of the centers was asked to participate in the study, if the following criteria were fulfilled: Main diagnosis of opioid dependence, minimum age of 18 years, no substitution treatment in the first 6 months prior to admission, and no acute psychotic episode. Also, patients had to agree to take one of the substitution substances and regarding psychosocial interventions to accept both manualized psychosocial treatment. Each patient received written information about the study including one part about the two substitution substances and a second part for the later psychosocial treatment groups (basic and indicative treatment) and gave informed consent to participate.
Randomization occurred after the patient gave written consent to participate. The first randomization as to substitution substances was carried out for all patients by giving the treatment centers randomized allocations for each subsequent patient recruitments, the second randomization was additionally applied only for the two psychosocial manualized treatments using other sets of randomized allocations.
179 opioid addicts were recruited at 8 treatment centers. Centers with 10 or fewer patients were not included in the present analysis because they did not systematically recruit patients according to the study protocol. One center (n = 26) was excluded because it was not possible to establish treatment as usual. Therefore, this center did not have a control group. Moreover, other problems regarding this center were high data attrition at intake, a different treatment supervisor, and therapists who were at the beginning of their behavioral treatment education and training. Therefore, the decision was to exclude this treatment center from the present analysis. The remaining study sample consisted of 122 patients at three treatment centers (34, 37, and 51 patients, respectively), and each with patients in treatment as usual, basic treatment and indicative treatment (see Table 1).
At the 1-year follow-up, 92 patients (51.4 %) of the total patient sample (N = 179) could be reached (including information on two deaths) and from the study sample (N = 122) 64 patients (52.5 % with two deaths) were included in the analyses.
Instruments
Data in this analysis were collected with three instruments: (1) Documentation standards of the German Society of addiction research and treatment [5] for assessing drug consumption and sociodemographic data at intake and follow-up 1 year later. These data were collected by standardized interviews; (2) The German version of the EuropASI [7], as a standardized interview too. (3) Symptom Check List (SCL-90; [10]) as a self-rating questionnaire. Additional data were assessed but not included in this analysis [15].
For all therapists and data coordinators a diagnostic training was carried out.
Data Collection
In all treatment centers a coordinator for data collection was established. Data collection were carried at intake, after 6 months (discharge from psychosocial treatment), and at the 1-year follow-up. Within the first 14 days the three instruments should be answered by one of the psychosocial therapists or by the trained coordinator for data collection or by the patients themselves. The follow-up assessment was carried out by a trained student of psychology.
Data Analysis
Because of the high attrition rate in the follow-up sample, we analyzed the main differences between the follow-up sample and the attrition sample, who could not be reached at the 1-year follow-up, regarding three potential prognostic variables: (1) Retention or drop out from treatment in the first 6 months and number of weeks in treatment. Dropout from treatment is a well-known negative predictor of treatment outcome in addiction [29, 32]), but weeks in treatment could be more sensitive in separating the two groups. (2) Age, education, and gender are unclear predictors, but they are usually control variables to compare patient samples. 3. Suicide attempts: such attempts are an indicator of psychological instability and could be seen as a negative predictor (at least for alcoholics, see [13]). Other probable prognostic factors like severity of addiction and comorbidity were at least partially associated with treatment dropout and therefore were not analyzed separately.
The comparison of the follow-up and attrition samples found a higher retention rate in the follow-up sample (67.2 % versus 41.4 %, p = .004). Similarly, the average number of weeks in treatment was higher in the follow-up sample than in the attrition sample. No significant differences were found in relation to age, gender, and suicide attempts.
Regarding the three treatment groups, basic treatment showed the highest attrition rate (68.3 %), followed by indicative treatment (50.0 %), and treatment as usual (24.4 %) (Chi square test, p = .000). No significant differences were found for the variables gender, age, and suicide attempts. As a consequence, retention rate and age and gender must be considered as control variables throughout the statistical analyses. Because of a weak but significant correlation between age and the composite score for family relationship on the EuropASI, we decided not to include this composite score as an additional control factor (Table 2).
To define changes between intake and follow-up, not only the changes in the average score are analyzed, but primarily the individual changes are seen as relevant. To identify individual differences, the critical differences for the composite scores of the EuropASI [38] and the SCL-90 (cit. in [10]) were calculated according to the formula: dcritical = 1.96 × sx × square root of 2(1 − rxx).
Individual differences between two measurements that were equal to or exceeded the critical differences for the composite scores of the EuropASI and the SCL-90 scores (see Tables 3, 4) were seen as significant individual changes and were used to differentiate patients into positive responders with reduced scores and negative responders with increased scores or without changes.
Missing Data and Imputation
Data attrition was a problem particularly at one treatment center, where the attrition rate regarding hard drugs at intake was 31.4 % compared with 8.1 and 11.8 % at the other two treatment centers. 17 of the 22 missings in hard drugs of the study group were dropouts, but five of the missings were regular completers all coming from the problematic centre. Omitting all data from this center would have reduced the sample size considerably, in particular at follow-up, and therefore was not an acceptable solution. As mentioned above, the methodological consequences were to control for dropouts in evaluating outcome, and to impute data applied only to EuropASI and SCL-90.
Data were imputed to complete data sets for SCL-90 scales and ASI composite scores at intake and separately at follow-up by applying the expectation maximization (EM) approach to substitute the missing scores. At admission, only scores of patients with at least one valid score in the set of EuropASI composite scores or in the set of SCL-90 scores were imputed. 5.6 % of the composite scores (related to N = 116) and 4.3 % of the SCL scores (related to N = 104) had to be substituted by the EM procedure (SPSS version 16).
For imputations in the follow-up sample, information about drug consumption had to be available at follow-up, and at least one score at intake or follow-up had to be valid (N = 62). In the follow-up sample of 62 cases, 14.0 % of all SCL-90 baseline scores and 13.1 % of all EuropASI baseline scores were imputed, while 16.5 % of all SCL-90 follow-up scores and 3.9 % of the EuropASI composite follow-up scores were imputed.
Statistical Analysis
In general, outcome is analyzed by two approaches: (1) By analyzing means of outcome criteria in the treatment groups before starting treatment and at follow-up after 1 year (6 months after the end of psychosocial treatment). (2) By analyzing individual changes of the outcome criteria. The second approach is conventional regarding drug consumption as a binary nominal scaled variable, but it is usually not used for scales as continuous outcome variables like SCL scores or days of drug consumption.
Data were analyzed by means of the SPSS packages 16, 17.0, and 19. The General Linear Model with Repeated Measurement and with covariates of gender, age and dropout was applied for analyzing average score changes. For analyzing the frequencies of individual significant changes Chi Square tests were used. The different statistical procedures applied are described in the Results section below.
Results
At Intake
Regarding drug consumption in the last month before admission, almost all patients (97.4 %) used hard drugs on at least 1 day (no significant differences between the three treatment groups, Chi square exact p = .529, two-sided). Opioids were used by 87.9 %, again without any significant differences between the treatment groups (Chi square test: exact p = .799, two-sided).
Regarding the EuropASI, the mean composite scores did not differ significantly [analysis of variance for each composite score, treatment group as a fixed factor, gender as a fixed factor, and age as a covariate, Levene test for homogeneity: significant for the composite scores Family (p = .011) and Economy (p = .007)]. Mean SCL-90 scores also did not differ significantly between the three psychosocial treatment groups (the Levene test was significant for the anxiety scale, p = .021).
To characterize the total group of drug addicts regarding needs for psychosocial treatment, the scale values of SCL-90 were transformed into T-values, and the percentages of patients with T-values lower than 40 and of those with values higher than 60 were calculated (see Tables 3, 4). Noteworthy, the highest percentage of patients with increased values was found on the depression scale with 54.5 %. All other scales showed percentages with increased values of about 30 % (see Tables 3, 4). The expected percentages for the two extremes of the distribution (<40 and >60) would be 16 %. In contrast, the percentages of patients with decreased values (lower than T-values of 40) were clearly lower than 16 %. More important, 29.8 % of the patients (N = 104 with data) showed no SCL-90 scale T-values greater than 60 Using the global SCL-90 score GSI (global severity index) to assess psychopathological strain, 53.4 % had lower T-values than 60. Both subsamples may be appropriate for identifying patients who do not seriously suffer from psychopathological symptoms having presumably no need for psychosocial treatment (Table 5).
At the End of Psychosocial Treatment
After 6 months, the retention rate was 54.1 % related to the study sample of N = 122. 45.9 % of the patients terminated prematurely for different reasons: Patient’s own decision (31.1 %); discharged by the treatment facility for disciplinary reasons (6.6 %); detoxification treatment (4.9 %); in consensus between patient and therapist (1.6 %); imprisonment (.8 %); and for unknown reasons (.8 %). Four (3.3 %) patients had left basic or indicative treatment, but continued to receive substitution treatment, and 7 patients (4.7 %) had changed the substitution drug.
Retention rates differed significantly between treatment centers (Chi square test, p = .035): in particular between two more liberal centers (62.2 and 60.1 %), and the other in relation to relapse regulation more severe center (35.3 %. However, retention rates did not differ significantly between the three psychosocial treatment groups: the highest rate (56.1 %) was in the treatment as usual and basic treatment groups, while the rate in the indicative treatment was somewhat lower (50.0 %) (Chi square test, p = .818).
Also regarding the follow-up sample only, the retention rates and dropout rates did not differ significantly between the three treatment groups (Chi square test, p = .387), although, the retention rate in the basic treatment group was much higher (93.3 %) than that in the treatment-as-usual group (64.5 %) and indicative treatment group (60.0 %). This finding emphasizes the necessity of controlling for dropout from treatment (or retention) in the later outcome analysis.
In the basic treatment group, the average number of treatment sessions was 17.3 for treatment completers (SD = 4.64) and 7.1 for dropouts (s = 5.95); in the indicative treatment group, the average number of treatment sessions was 13.6 for treatment completers (SD = 6.16) and 3.4 for dropouts (SD = 2.13). These figures are based on a subsample (n = 41) with a retention rate of 58.5 %. The number of treatment sessions for treatment as usual was not available (Fig. 1).
An analysis with treatment time in weeks as an alternative outcome parameter (dependent variable) and gender and treatment dropout as control variables found a statistically significant effect of treatment groups on weeks in treatment, with differences mainly for the group of dropouts: Time in treatment for dropouts was highest in the treatment-as-usual group (mean 13.9 weeks) compared with 12.5 weeks in the indicative treatment group and 8.1 weeks in the basic treatment group. Both groups differed significantly from basic treatment (8.1 weeks, p = .008 or p = .073, general linear model with the factors treatment groups p = .024, dropout p = .000 and the interaction effect treatment groups x dropout, p = .076)
A large percentage of dropout patients could not be motivated for an interview or were not willing to answer questionnaires before leaving the treatment facility. Therefore, it seems not useful to analyze this highly selected group with data at the end of psychosocial treatment in more details.
At the 1-year Follow-up
Drug Use
The percentage of patients without any use of hard drugs in the last 30 days increased significantly from 1.9 % at intake to 54.7 % at follow-up (McNemar test: p = .000). Regarding opioid use (besides substitution substances), the number of patients with no opioid use in the past 30 days increased from 12.7 to 62.9 % (McNemar test: p = .000), whereas the numbers of patients with cannabis use and with alcohol use increased only moderately (n.s., see Table 6).
The average number of days on which hard drugs were used in the last month decreased from 19.2 to 5.6 days at follow-up. Applying the general linear model (GLM) to check the effects with the factors repeated measurement (average number of days of hard drug use at intake and follow-up) and treatment group and the control variables gender, age, and dropout, only the repeated measurement factor was significant (p = .02), but no interaction term with treatment groups was significant. This means that the treatment groups did not differ regarding number of days with hard drug use or opioid use. Regarding the number of days with cannabis or alcohol use, neither the increases of cannabis use (from 6.2 to 10.1) nor alcohol use (from 7.2 to 9.8) nor other interaction factors with treatment were significant (Table 7).
The analysis of the individual changes in the number of days with drug use at intake and at follow-up found that 79.6 % of patients had fewer days with hard drug use (more than 3 days less) and 1.9 % showed more days with hard drug use (3 days more); there was no change in 18.5 % of the patients. The number of days with alcohol consumption increased in 29.6 % of the patients, but decreased in 13 % (by more than 3 days less). The number of days with cannabis use increased in 25.5 % of patients and decreased in 12.7 % (by more than 3 days).
EuropASI (Individual Changes in Composite Scores)
In 5 of the 8 EuropASI composite scores, more individuals had positive changes (i.e. decreased composite scores at follow-up) than negative changes (see Table 8). The highest percentage of positive changes occurred in drug use (65.0 %), relationships with others (35 %), and legal status (25.0 %); the lowest rate of positive changes was found in the psychiatric status (11.7 %, balanced by 11.7 % negative changes), job satisfaction (6.7 %), and alcohol (1.6 %). The highest percentage of negative changes was found in alcohol use (30.0 %) and job satisfaction (16.7 %). For each subscale, the majority of patients showed no change and varied between 83.3 % (medical status) to 31.7 % (drug use).
Comparing the two experimental treatment groups and the control group treatment-as-usual (see Table 9), the rates of at least one positive change varied between 93.3 % (basic treatment) and 72.2 % (indicative treatment). The high composite score change rates are mainly due to the high change rate of composite score for drugs. The rate of at least one negative change was highest for the basic treatment (66.7 %) and lowest for indicative treatment (55.6 %). Each patient showed at least one positive or negative change. Although indicative treatment has the lowest rate of at least one positive ASI change, the differences between treatment groups were not significant (see Table 9).
SCL-90 (Individual Changes)
59.7 % of all patients showed at least one positive change in the SCL-90 scales and 37.1 % at least one negative change; 24.2 % of patients showed no change in the SCL-90 scales. Again, the three treatment groups did not differ significantly (Table 10).
More women (82.6 %) than men (46.2 %) showed at least one positive change (Chi square test, two-sided, p = .005), while the rate of no changes was higher among men (35.9 % versus 8.7 %, p = .029) and the rates of at least one negative change did not differ significantly (39.1 and 35.9 %).
In five SCL-90 subscales (depression, interpersonal sensitivity, general anxiety and phobic anxiety and paranoid ideation), more patients showed positive changes than negative changes, whereas in the subscales somatization, obsessive–compulsive behavior, and psychoticism more patients showed negative changes than positive changes (no differences in the SCL-90 scale hostility). Again, by far the most patients showed no change in the SLC-90 scales (between 53.6 % in phobic anxiety and 85.5 % in global severity index) (Table 10). Testing the frequencies of changes between the 3 treatment groups in each SCL-90 scales statistically, only the group differences for depression were significant (p = .052, exact test two sided: p = .047). Reductions in the depression score were found most often in the indicative treatment group (35.0 % of patients), but also most negative changes occurred in this group (15 % of patients).
To test changes in all SCL 90 scales, the average number of positive and negative changes were calculated for each patient. A linear regression analysis of the number of individual positive and separately negative changes in all SCL-90 scales (independent variables: treatment groups, gender, age, dropout) found that the ANOVA overall F-test was significant only for the positive changes (F = 4.531, p = .006). The factors treatment groups (p = .017) and gender (p = .007) both had a significant effect. The average number of individual changes in indicative treatment was 2.2 compared with 1.1 in the treatment-as-usual group and 1.2 in the basic treatment group.
Summarizing all individual SCL changes in a different way as at least one positive change (Table 11), no significant differences were found between the three treatment groups (treatment as usual, 53.3 %; indicative treatment, 59.7 %; basic treatment, 65 %). The percentage of patients with at least one negative change was highest in the basic treatment group (58.3 % versus 36.7 % in the control group and 25.0 % in the indicative treatment group). The percentage of patients with no changes at all was highest in the treatment-as-usual group (34.5 % versus 25.0 % in the control group and 20.8 % in the indicative treatment group) (Table 11).
Prediction of Outcome by SCL-90 and EuropASI Composite Scores
The number of problematic high SCL-90 scores (T-value > 60) as a need for psychosocial treatment correlates considerably with the number of positive individual SCL-90 changes (Pearson correlation, r = .594, p = .000), but hardly correlates with the number of negative changes (r = .076 p = .557). Separated for the 3 treatment groups, the correlations between positive changes and strain are different: for indicative treatment r = .707 (p = .000), for basic treatment r = .373 (p = .233), and for treatment as usual r = .599 (p = .000).
Hard drug consumption in the last month before follow-up did not correlate significantly with either the EuropASI composite scores at intake (r = −.067 to .150) or with the need for psychosocial treatment defined by the General severity score of the SCL-90 greater than a T-value of 60 (r = .127, p = .333).
Based on the hypothesis of indication that only patients with increased scores at the SCL-90 scales at intake (greater than T-values of 60) are appropriate for psychosocial interventions, the individual changes were analyzed within different subgroups of patients regarding at least one increased T-value at intake versus a subgroup of patients with all SCL-90 T-values lower or equal than T = 60. Patients with no increased T-scores (n = 16) showed only two positive changes (12.5 %) in one of the scales (see Table 12), whereas 76.1 % of those with at least one T-score higher than 60 had at least one positive SCL change (p = .000). As to negative SCL changes at follow-up, again those with at least one increased T-score showed a higher rate of at least one negative SCL-90 change (43.5 %) than the patient group with no increased T-value at admission (18.8 %, p = .078, see Table 12).
Discussion
One year after starting substitution treatment, we found a clear overall reduction (51.9 % absolute difference) in the use of hard drugs (including non prescribed tranquilizers) for the last month before assessment. Furthermore, both the experimental and treatment-as-usual groups showed a clear reduction in psychosocial symptoms and problems (at least one positive change in SCL-90 scales in 59.7 % of patients). However, alcohol consumption had increased (from 7.2 to 9.8 days with alcohol used) in the last month before asessment and about 30 % of patients may have had an alcohol problem (EuropASI: strain rating mild to extreme by patients for the last month, 16.3 % strong or extreme). Also, cannabis use had increased, but not significantly (from 6.2 to 10.1 days in the last month before assessment).
The type of psychosocial treatment showed no significant effect on intake of hard drugs (for the general hypothesis of no differences between treatments, see [38]). Together with results about dropout rates mentioned later on and the knowledge about the sensitive reactions of patients to the regulation of relapses, this finding might indicate that drug consumption can be influenced more by rules and sanctions to relapses, including medication like the take home dosage, than by relapse prevention methods. Rules and sanctions in case of relapses were not integrated into the relapse prevention part of the manualized treatments.
Patients in the indication treatment group showed a mean of two individual SCL-90 changes compared to one in the basic treatment group and one in the treatment-as-usual group. Both results could mean that the effect of a flexible manualized psychosocial treatment is restricted to psychological strain and symptoms and does not influence drug consumption.
The dropout rate within the first 6 months seems to be high, but it was related mainly to one center (64.7 %) that regulated relapses more strictly. We found no significant differences in either dropout rates or time in treatment between the different psychosocial treatments. Among the dropouts, the time in treatment was significantly longer in the treatment-as-usual and indicative treatment groups than in the basic treatment group. Dropping out of treatment correlated negatively with at least one positive individual change in the SCL-90 scales (r = −.338, p = .004), but not with the EuropASI Severity scales at intake. The predictor value of dropout seems to be small, but is in accordance with findings of other studies [32]. The relatively low dropout rate in the treatment as usual may be due to the more frequent treatment reactions to the individual risk of dropping out compared to the experimental treatment groups.
The EuropASI CS scores and the SCL-90 scale scores were not associated with the primary outcome criterion of hard drug use. However, the need for psychosocial treatment (defined by SCL-90 scales at intake with T-values greater than 60) is correlated strongly with positive changes in the SCL-90 scales. There might be an artificial regression effect explaining part of this correlation. But there is no other instrument available in the study to assess the strain of symptoms in order to clarify the regression effect. The ASI composite scores, which do not assess subjective strain, did not correlate with positive changes in the SCL-90, with the exception of the EuropASI composite score of relationships (severity of problems) with persons outside the family (r = .310). The small changes in the EuropASI psychiatric scale are in line with similar small changes in a large observational study of substituted opioid addicts with related psychiatric problems performed in Germany (PREMOS, [34]).
Negative changes in psychosocial treatments of opioid addicts occurred frequently and should be treated by specific interventions in the course of treatment. The SCL-90 scales Somatization, Phobic anxiety and Psychoticism showed the highest rates of negative changes (about 20 % each). Therefore, a broad spectrum of interventions should be available to help patients cope with such symptoms and syndromes. Negative changes occurred in the basic treatment group more frequently than in the other two groups whose greater flexibility in relation to the patient’s situation seems to be the critical difference.
Individual changes need to be analyzed in order to assess negative changes; individual changes may simply distinguish between positive, negative, and no individual changes. Although the category “no change” is usually most frequently related to a single scale, only a few patients showed no individual changes in all SCL-90 scales.
A possible conclusion from these results could be that a subgroup of patients does not need or benefit from psychosocial treatment. If patients with no increased values (greater than 60) in the SCL-90 scales did not benefit from psychosocial treatments, one might conclude that this group of patients (about 25 %) should not be allocated to psychosocial treatment in addition to substitution treatment. This conclusion needs to be confirmed in further studies on people with drug addiction, but may be investigated also in people with other kinds of addiction such as alcohol dependence.
Recent randomized studies point into a similar direction. Schwartz et al. [31] found no differences in 12-month outcomes of patients on standard methadone treatment with routine counseling and those who received no counseling. In addition, Mitchell et al. [24] did not find differences in buprenorphine-maintained patients on intensive or standard outpatient treatment. Fiellin et al. [9] reported that the addition of psychosocial therapies did not improve outcomes, but patients in this study were poorly compliant with psychosocial treatment.
Opioid maintenance can be viewed as a platform for interactions to support recovery [31], but the optimal psychosocial intervention is a matter of debate, and the use of psychosocial interventions varies significantly across Europe (www.emcdda). Best practice WHO guidelines recommend that psychosocial support is routinely offered alongside pharmacological treatments. The results of this study may help clarify which subgroup of opioid addicts may profit from enhanced psychosocial interventions.
Methodological Limitations
Data attrition was a major problem due to different reasons. Some psychosocial therapists (psychologists, social workers and physicians) comply with the treatment protocol and with systematic data documentation in a discrepant way, although they had been trained and data collection was separated from clinical work as far as possible. Imputation of data was applied in such a way that no case without any data in the respective instrument was generated as a new case by imputation. This principle is independent from statistical criteria and rather conservative. Furthermore, no data about drug consumption were substituted. The application of the EM procedure for imputation was preferred to multiple imputation, which may be preferred in relation to unbiased variance estimation of the imputed data set, but seems unclear in relation to the exact substitute scores for imputation.
In psychosocial treatment, the control of the therapist factor is essential (see [20], among others). The study was designed to control this factor by having the same therapists perform treatment as usual, basic treatment and indicative treatment. This objective was achieved in the basic and indicative treatment groups, but only partially in the treatment-as-usual group: At one treatment center, the psychosocial therapists were the same for all treatment groups; in another center, there was an overlap between psychosocial therapists performing treatment as usual and those performing the other treatments; and in the third center, the therapists performing treatment-as-usual were different from those in the experimental groups. However, the medical doctors responsible for substitution and the framework of regulations, e.g. sanctions in case of relapses, were consistent in each treatment center during the study.
Different effects of treatments are probably due to different attrition processes in the treatment groups at follow-up. Therefore, the different data attrition rates for treatment as usual, basic treatment, and indicative treatment may be interpreted as different levels of satisfaction and acceptance of the respective treatment concept. According to different attrition rates, treatment as usual is accepted best by patients and basic treatment is accepted worst. If one assumes that the more satisfied patients are, the more motivated they will be to participate in a follow-up study, one must consider that real differences in the outcome of the three treatment groups are attenuated by a positive selection trend of the participating patients. To compensate for this bias, we tried to consider dropout rate, gender and age as control variables in the statistical analyses. Therefore, results seem to be widely unbiased by selection processes in the relationship of participating in follow-up measurement.
The two approaches of analyzing average scores versus individual changes yielded more or less the same global results. Although the majority of patients showed at least one positive change in the different scales of the EuropASI and SCL-90, a considerable percentage of the patients had no changes in most of the scales and, perhaps more importantly, several negative changes had occurred, too. The cases with no change or even negative changes, if a positive one is expected based on the data at intake or later on, could be selected in order to modify interventions in the further course of maintenance treatment.
Conclusions
-
The analysis of individual changes by standardized interviews and self-rating tests gives a more comprehensive picture of changes, including negative and no individual changes, in addition to estimating changes in average group scores.
-
Individual negative changes occur relatively often and should be seen as additional tasks during treatment to be coped with. Because they cover a broad spectrum of problems and symptoms, a corresponding range of treatment interventions is required to deal with these negative changes. Job problems, medical status, and alcohol abuse are specific needs for treatment interventions in the course of substitution therapy.
-
Flexible psychosocial treatment has effects primarily on psychosocial symptoms and less on drug consumption. As a consequence, either relapse prevention should be strengthened to avoid relapses or coping mechanisms for dealing with other problems and issues should be increased to reach an indirect effect on relapses via stress reduction.
-
A general basic treatment program not regarding individual problems and progress seems to be less effective than a more flexible program for people with drug addiction and may even lead to more negative changes. Only a flexible resources- and success-oriented psychosocial treatment could be more effective.
-
Apparently, there is a group of opioid addicts without a need for psychosocial treatment defined by no increased scores in SCL-90 scales at intake. They showed almost no changes in psychological strain and could be considered as non-indicative for psychosocial treatment of opioid addicts.
A gap remains between patients’ needs in different life areas on the one hand and their readiness to accept psychosocial help on the other. This seems to be an essential aspect of the addiction disorder itself, not only a side effect of inappropriate interventions. Besides the motivational pressure of pain and strain, the expectation and hope of positive chances within the patient’s existing resources should be more greatly emphasized. In some cases, the inclusion of significant partner or friends in the psychosocial treatment may contribute to motivation and behavior change.
References
Amato L, Minozzi S, Davoli M, Vecchi S, Ferri M, Mayet S. Psychosocial combined with agonist maintenance treatments versus agonist maintenance treatments alone for treatment of opioid dependence. Cochrane Database Syst Rev. 2004;4:CD004147.
Amato L, Minozzi S, Davoli M, Vecchi S. Psychosocial combined with agonist maintenance treatments versus agonist maintenance treatments alone for treatment of opioid dependence. Cochrane Database Syst Rev. 2011;10:CD004147. doi:10.1002/14651858.CD004147.pub4.
Amato L, Minozzi S, Davoli M, Vecchi S. Psychosocial and pharmacological treatments versus pharmacological treatments for opioid detoxification. Cochrane Database Syst Rev. 2011;9:CD005031. doi:10.1002/14651858.CD005031.pub4.
Crits-Christoph P, Siqueland L. Psychosocial treatment for drug abuse: selected review and recommendations for national health care. Arch Gen Psychiatry. 1996;53(8):749–56.
Deutsche Gesellschaft für Suchtforschung und Suchttherapie (2001). Dokumentationsstandards III für die Evaluation der Behandlung von Abhängigen. SUCHT 47(8), Sonderheft 2
Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorder. Am J Psychiatry. 2008;165:179–87.
Gsellhofer B, Küfner H, Vogt M, Weiler D. European Addiction Severity Index, EuropASI. Manual für Training und Durchführung von Interviews mit dem EuropASI. Baltmannsweiler: Schneider 1999.
Fareed A, Vayalapalli S, Casarella J, Drexler K. Effect of buprenorphine dose on treatment outcome. J Addict Dis. 2013;31:8–18.
Da Fiellin, barry DT, Sullivan LE, Cutter CJ, Moore BA, O’Connor PG, Schottenfeld RS. A randomized trial of cognitive behavioral therapy in primary care-based buprenorphine. Am J Med. 2013;74:e11–7.
Franke, G.H.(2002). Die symptom-Checkliste von Derogatis-Deutsche Version (SCL-90-R) manual. Göttingen: Beltz.
Gerevich J, Bacskai E, Ko J, Rozsa S. Reliability and validity of the Hungarian version of the European Addiction Severity Index. Psychopathology. 2005;38(6):301–9.
Grawe K. Grundriss einer Allgemeinen Psychotherapie. Psychotherapeut. 1995;40:130–45.
Koeter MWJ, Hartgers C. Preliminary Procedure for the Computation of the EuropASI Composite Scores. European Cooperation in the field of scientific and technical research, 1997.
Küfner H, Feuerlein W (1989) In-patient treatment of alcoholism. A multi-centre evaluation study. Springer: Berlin
Küfner H, Hackmann K, Schnabel A, Soyka M. Optimierung der substitutionsgestützten Therapie Drogenabhängiger (OSTD): Entzugssymptome und Suchtverlangen in der ersten Einstellungswoche. Suchtmedizin. 2004;6(1):95–7.
Küfner H, Ridinger M. Psychosoziale Behandlung von Drogenabhängigen unter Substitution (PSB-D). Manual 2.0. Lengerich u.a.: Pabst. 2008.
Küfner H, Rösner S. Forschungsstand 2005 zur Substitutionsbehandlung: Ergebnisse zur Evaluation und Indikation. In: Gerlach R, Stöver H, editors. Vom Tabu zur Normalität: 20 Jahre Substitution in Deutschland: Zwischenbilanz und Aufgaben für die Zukunft. Lambertus: Freiburg; 2005.
Maddux JF, Desmond DP. Methadone maintenance and recovery from opioid dependence. Am J Drug Alcohol Abuse. 1992;18(1):63–74.
Magura S, Nwakeze PC, Sung-Yeon K, Demsky S. Program quality effects on patient outcomes during Methadone maintenance: a study of 17 clinics. Subst Use Misuse. 1999;34(9):1299–324.
Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement theapy for opioid dependence. Cochrane Database Syst Rev. 2009;3:CD002209. doi:10.1002/14651858.CD002209.pub2.
McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr HL, O’Brien CP. New data from the addiction severity index. J Nerv Ment Dis. 1985;173:412–23.
McLellan T, Hagan TA, Meyers K, Randall M, Durell J. Intensive outpatient substance abuse treatment comparisons with traditional outpatient treatment. J Addict Dis. 1997;16(2):57–84.
McLellan T. The role of psychosocial services in drug abuse treatment. In: Waal H, Haga E, editors. Maintenance treatment of heroin addiction. Evidence at the crossroads. Oslo: J. W. Cappelens; 2003.
Mitchell SG, Gryczynski J, Schwartz RP, O’Grady KE, Olsen YK, Jaffe JH. A randomized trial of intensive outpatient (IOP) vs. standard outpatient (OP) buprenorphine treatment for African Americans. Drug Alcohol Depend. 2013;128:222–9.
McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissim G, et al. The fifth edition of the addiction severity index. J Subst Abuse Treat. 1992;9:199–213.
Petry NM, Weinstock J, Alessi SM. A randomized trial of contingency management delivered in the context of group counseling. J Consult Clin Psychol. 2011;79:686–96.
Prendergast ML, Podus D, Chang E. Program factors and treatment outcomes in drug dependence treatment: an examination using meta-analysis. Subst Use Misuse. 2000;35(12–14):1931–65.
Rigter H, Van Gageldonk A, Ketelaars T. Treatment and other interventions targeting drug use and addiction: state of the art 2004. Utrecht: National Drug Monitor (of the Netherlands); 2005.
Roch I, Küfner H, Arzt J, Böhmer M, Denis A. Empirische Ergeb-nisse zum Therapieabbruch bei Drogenabhängigen: ein Literaturüber-blick. Sucht. 1992;38:304–22.
Saunders B, Wilkinson C, Phillips M. The impact of a motivational intervention with opioid users attending a methadone programme. Addiction. 1995;90(3):415–24.
Schwartz RP, Kelly SM, O’Grady KE, Gandhi D, Jaffe JH. randomized trial of standard methadone treatment compared to initiating methadone without counseling: 12-month findings. Addiction. 2012;107:943–52.
Simpson DD, Joe GW, Dansereau DF, Chatham LR. Strategies for improving methadone treatment process and outcomes. J Drug Issues. 1997;27:239–60.
Soyka M, Zingg C, Koller G, Kuefner H. Retention rate and substance use in methadone and buprenorphine maintenance therapy and predictors of outcome: results from a randomized study. Int J Neuropsychopharmacol. 2008;11(5):641–53.
Wittchen H-U, Bühringer G, Rehm JT. Effekte der langfristigen Substitution Opioidabhängiger: Prädiktoren, Moderatoren und Outcome: Ergebnisse und Schlussfolgerungen der PREMOS-Studie (Predictors, Moderators and Outcome of Substitution Treatment). Suchtmedizin 13: Sonderheft 198–299. 2011.
Waal H, Haga E, editors. Maintenance treatment of heroin addiction. Evidence at the cross-roads. Oslo: J. W. Cappelens; 2003.
Ward J, Mattick RP, Hall W, editors. Methadone maintenance treatment and other opioid replacement therapies. Amsteldijk: Harwood Academic Publishers; 1998.
Wampold BE. The great psychotherapy debate: models, methods and findings. Mahwah and London: Lawrence Erlbaum Associates; 2001.
Weiler D, Vogt M, Küfner H. Anwendung des European Addiction Severity Index (EuropASI) im Rahmen einer ambulanten Behandlung von Drogenabhängigen. Sucht. 2000;46:197–208.
WHO. Guidelines for the Psychosocially Assisted Pharmacological Treatment of Opioid Dependence Geneva: World Health Organization, 2009 http://www.lccn.loc.gov/2009447993. 2009.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Küfner, H., Melia, M. & Soyka, M. Manualized Psychosocial Treatment Versus Standard Care in Opioid Maintenance Treatment: Results of a Randomized Clinical Trial and Follow-up Study. J. Psychosoc. Rehabil. Ment. Health 1, 61–75 (2014). https://doi.org/10.1007/s40737-014-0017-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40737-014-0017-y