Abstract
Purpose of Review
Workplace noise negatively impacts health, and noise-induced hearing loss is the most common work-related disease in many countries. Occupational noise may also cause cardiovascular disease, and there is epidemiologic evidence on the non-auditory effects of noise. This paper aims to briefly present and summarize the latest evidence on the auditory and non-auditory health effects of occupational noise exposure from the last 5 years.
Recent Findings
Two systematic reviews assessing the cardiovascular effects of occupational noise exposure were published in the last year. Our own recent review found convincing evidence of an association between occupational noise exposure > 80 dB(A) and hypertension and a dose-response relationship between noise exposure and hypertension risk. Another review of cardiovascular disease conducted by the World Health Organization (WHO) and the International Labour Organization (ILO) found an increased risk of incident ischemic heart disease at noise exposures ≥ 85 dB(A). Recent reviews on work-related injuries, diabetes, acoustic neuroma, and pregnancy outcomes also find noise-related associations.
Summary
Evidence of an association between occupational noise and cardiovascular outcomes was recently evaluated. We found the risk of hypertension increases with a clear dose-response relationship at noise levels > 80 dB(A). The WHO/ILO review highlights the lack of quality research including women. Additional high-quality research on epigenetic effects, oxidative stress, work-related injuries, diabetes, acoustic neuroma, and pregnancy outcomes is also needed. Urgently needed (increased) measures of workplace noise reduction will reduce the incidence of noise-induced hearing loss and help prevent cardiovascular diseases, especially hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Noise is one of the most common work-related occupational hazards. According to the 2015 European Survey on Working Conditions (ECWS), 28% of European workers reported being exposed to loud noise during at least one-fourth of their working time, with the percentage ranging from 18% in Malta and Portugal to 44% in Turkey [1]. In the USA, 25% of workers reported a history of occupational noise exposure, with a point prevalence of 14% [2]. Of the estimated 22 million workers in the USA exposed to loud noise at work, 34.3% report never using hearing protection devices [3].
Noise-induced hearing loss (NIHL) is also the most frequently recognized occupational disease in many countries. NIHL was the most commonly confirmed occupational disorder in Finland between 2012 and 2016 [4]. In Germany, NIHL is continuously the most frequently recognized occupational disease, comprising 38.3% (n = 6951) of all recognized occupational diseases in 2019 [5]. A comparison of five countries, France, Spain, Italy, Germany, and Denmark, found the recognization of NIHL as an occupational disease ranged from 6 cases per 100,000 persons in France to 33 cases per 100,000 in Denmark [6]. Thus, understanding and recognizing the health effects of noise exposure is essential to promoting a safe workplace for millions of workers.
A growing body of evidence indicates that noise exposure increases the risk of cardiovascular disease [7••, 8], and recent World Health Organization (WHO) reviews of environmental noise find increased psychosocial and cardiovascular risks associated with traffic noise levels ranging from around 40 to 80 dB(A) [9,10,11,12,13,14,15,16]. However, the best understood and most researched health effect of occupational noise is hearing damage.
Epidemiology of NIHL—International Comparison
Noise-induced hearing loss (NIHL) plays an important role worldwide, with over 450 million people—corresponding to more than 5% of the world’s population—suffering from disabling hearing loss [17]. For adults, the latter is defined as hearing loss exceeding 40 decibels (dB) measured in the better hearing ear. According to the WHO, disabling hearing loss occurs in about 30% of all people older than 65 years of age, the majority of them living in low- and middle-income countries. While hearing loss can be induced by congenital abnormalities, injuries, use of ototoxic medication, exposure to environmental or recreational noise [17], occupational noise exposure is the most common cause of NIHL.
Today, occupational noise-induced hearing loss is a work-related disease of international importance. It is considered the most prevalent work-related disease worldwide, affecting more than 10% of all workers in developed countries [18]. A recent systematic review from China estimated a prevalence of 21.3% for occupational NIHL in noise-exposed Chinese workers over the last 26 years [19]. A similar figure was calculated for workers in the USA: there, the prevalence of hearing loss in noise-exposed workers was about 20% between 1981 and 2010. However, a slow but steady decrease in the incidence of noise-induced hearing loss in the USA can be observed in most industry sectors [20].
According to a WHO report, about 16% of the disabling hearing loss in adults worldwide could be attributed to occupational noise exposure, and the global burden of disease caused by occupational NIHL was estimated at over 4.1 million (4,151,000) disability-adjusted years of life lost (DALYFootnote 1) in 2005 [22]. However, this number probably underestimates the global burden of occupational noise exposure. It only comprises burden due to NIHL, and other health-affecting consequences of occupational noise exposure—e.g., hyperacusis or tinnitus—are not considered [23•]. The burden of occupational NIHL is also increasing. Zhou et al. [24] report that the health burden due to occupational NIHL increased from 3.3 to 6 million DALYs between 1990 and 2017, with low-income countries experiencing the highest increase in burden. Actual DALY data from the Institute for Health Metrics Evaluation (IHME) show the burden increasing most in the Western Pacific WHO Region (including, e.g., China, Japan, South Korea, Philippines, Australia, New Zealand), while remaining relatively stable in the rest of the world (Fig. 1).
Typical for NIHL caused by occupational noise exposure are its bilateral occurrence and sensorineural appearance, the latter due to the damaged hair cells in the cochlea of the inner ear. Usually, hearing loss due to noise exposure does not exceed 40 dB in lower (≤ 1000 Hz) and 75 dB in higher (> 1000 to 8000 Hz) frequencies [25]. However, this must not be true for other forms of hearing loss, such as presbyacusis. The first sign for NIHL can be seen in an audiometric curve, which typically shows a “notch” at high frequencies in the range of 3 to 6 kHz with a recovery at 8 kHz [25]. This recovery at even higher frequencies can be used to demarcate NIHL from age-induced hearing loss (presbyacusis), which leads to a declining curve at high frequencies without recovery. However, the exact form of the audiometric curve depends on several factors, such as the particular frequency or length of noise exposure [25]. Besides the level of noise exposure, there are several modifiable and non-modifiable risk factors associated with an increase in the prevalence of NIHL in general, such as increasing age, genetics, smoking, lack of exercise, or the presence of diabetes and cardiovascular diseases [26].
Furthermore, it should be considered that NIHL can have a meaningful impact on safety and quality of life. For example, it has been shown that workers with NIHL are at a higher risk for hospital admission due to work-related injuries than people with normal hearing [27]. Also, NIHL can induce social consequences such as fear, depression, and difficulties in relationships [28], as well as increased annoyance [29], and is independently associated with incident cognitive impairment and accelerated cognitive decline [30].
Five systematic reviews on occupational NIHL were published in the last 5 years [19, 31•, 32,33,34]. Of these reviews, one focused on asymmetric hearing loss [33], another focused on hearing loss in China [19], and three reviews considered occupational NIHL in general [31•, 32, 34].
Lie et al. [31•] conducted a comprehensive review of occupational NIHL that comprised a qualitative summary of 187 articles. Although different criteria for recognizing occupational NIHL complicated international comparisons, the authors found 7 to 21% of hearing loss is attributable to occupational noise. Increased risks for occupational NIHL were observed for workers in industry, shipbuilding, construction, the military, and farming. No increased risk was observed for kindergarten workers, and research on professional musicians was inconclusive. The summarized research also indicated exposure to impulse noise is more damaging than exposure to continuous noise, and exposure to solvents and secondhand smoke might increase the risk of NIHL. The review by Mazitova et al. [34] summarized five reviews (including Lie et al. [31•]) and two original studies [20, 35] and came to similar conclusions. Chen et al. [32] summarized 108 studies on the epidemiology, pathogenesis, and prevention of NIHL published between 2000 and 2020, finding the raw prevalence of occupational NIHL ranged from 11.2% in a group of South African gold miners (average age not reported) [36] to 58% in a group of construction workers in the USA (average age = 59.2 years) [37].
Zhou et al. [19] synthesized 88 articles of occupational NIHL in Chinese workers and found that Chinese workers in manufacturing, transportation, mining, and agriculture were exposed to hazardous levels of noise averaging 98.6 ± 7.2 dB(A). Masterson et al. [33] looked specifically at the etiology of asymmetrical hearing loss. Since occupational NIHL is typically symmetrical, the occupational etiology of asymmetrical hearing loss is sometimes challenged. In this review, six studies offered limited evidence of an association between occupational noise and asymmetrical hearing loss. The authors postulate that physiological differences between ears or differential shielding of one ear might lead to one ear being more susceptible.
Brief History of Occupational NIHL
It took relatively long for humankind to recognize that excessive noise causes hearing loss and even longer to determine how. In his paper, “The Worker's Ear: A History of Noise-induced Hearing Loss,” Floyd E. Thurston summarizes the history of occupational NIHL [38] and reports of ancient texts anecdotally observing hearing loss among people constantly exposed to naturally occurring noise, such as the rush of the Nile River. First reports of hearing loss due to human-made noise began with the use of gunpowder in the 13th century. In the early 1700s, Bernardo Ramazzini, “the father of occupational medicine” described groups of noise-exposed workers with hearing loss in his De Morbis Artificum Diatriba [38]. The transition from an agricultural to an industrial economy increased the number of workers exposed to noise and developing occupational NIHL. In the early part of the 20th century, experiments on guinea pigs showing cochlear damage after exposure to loud noise helped explain the pathomechanism of NIHL [39]. Later in the 20th century, the development of methods to quantify both hearing loss and sound levels facilitated the establishment of protective guidelines to limit noise exposure in the workplace [38].
Pathomechanism—How Does Noise Affect Health?
Noise exposure can affect health in two ways [40]. On the one hand, there are auditory effects. These describe the damage to hair cells in the inner ear caused by overstimulation of the cochlea through excessive and prolonged noise exposure. Excessive vibration of the inner ear structures due to intense noise exposure does not only harm single hair cells, but can also destroy cell junctions connecting cochlear cells or lead to a decrease in synaptic connections between hair cells and the auditory nerve. In particular, exposure to noise levels exceeding 130 dB(A) is said to cause direct mechanical damage to the ear [41]. For gradual-onset NIHL, metabolic changes or ischemia play an important role in the underlying pathomechanisms. For example, vasoconstriction caused by noise exposure can reduce cochlear blood supply, followed by decreasing hair cell function. Furthermore, noise exposure can provoke an accumulation of reactive oxygen species, which can also induce several biochemical pathways leading to cell death [40]. As hair cells cannot regenerate, their recurring impairment leads to the abovementioned hearing loss.
Concerning the processing of complex sounds, functioning neural networks are needed to extract relevant information from noise. A loss of function within these networks can lead to behavioral auditory disorders (e.g., understanding speech in social situations), even if audiometric thresholds are normal. Until a few years ago, these pathological changes were said to be located in the auditory cortex or cortical processes [42]. However, recent research shows that subcortical auditory processing also plays an essential role in the development of auditory disorders. In their narrative review, Felix et al. [42] point out that subcortical pathways are part of the first processing mechanisms which lead to sound perception. That is why the impairment of subcortical structures—such as the thalamus, midbrain, and auditory brainstem—can lead to difficulties in understanding complex sounds [42].
Even though there is currently no possibility to prevent or moderate the auditory symptoms caused by noise clinically, there is evidence that AMPKα (adenosine monophosphate-activated protein kinase α) could serve as a target for NIHL therapy. AMPKα plays an important role in biochemical signaling pathways activated by noise exposure [43]. Also, a review of epigenetic effects found inconclusive indications of noise-induced changes to DNA-methylation, micro RNA (miRNA) expression, and histone acetylation and methylation from several human and animal studies [44].
The second group of noise-related effects comprises non-auditory (also: extra-auditory) ones. These can be explained based on the interaction between noise acting as an acute or chronic stressor and the consecutive distribution of stress hormones, such as adrenaline, noradrenaline, and cortisol. This biological mechanism is also described in a WHO publication concerning the effects of environmental noise [45]. A review by Recio et al. [46] also describes an integrative stress model to explain how psychological stress caused by noise contributes to cardiovascular, respiratory, and metabolic disease risks. According to the general stress model, repeated or frequent stress brings the body out of homeostasis and causes allostatic load and physiological responses [47]. Repeated or prolonged adaptive responses to stress cause changes to the neural circuitry and initiate a cascade of immune responses, which in turn can lead to endothelial and mitochondrial dysfunction, and subsequently, increased blood pressure [48]. Daiber et al. [49] highlight the ensuing oxidative stress and downregulation of neuronal nitric oxide synthase caused by noise-related stress responses as a pathomechanism for cardiovascular, metabolic, and mental health diseases. As reported by Ising and Kruppa [50], an increase in the concentrations of stress hormones could be observed in several studies examining the effects of environmental noise. Similarly, narrative reviews suggest an increased secretion of the aforementioned hormones in laboratory animals and workers exposed to noise [51].
Another narrative review describes observations of vascular damage in noise-exposed humans and animals, most likely mediated by the noise-induced stress response [52]. Vascular changes due to nighttime noise are also observed in randomized trials [53, 54]. A randomized crossover study exposing study participants to nightly recorded aircraft noise found a statistically significant decrease in flow-mediated dilation (FMD) of the brachial artery following a night with noise [54]. This study also found self-reported sleep quality was worse after a night with noise but observed no difference in heart rate, heart rate acceleration, or accelerometer-based movement. A similar study conducted with nocturnal railway noise also observed decreased FMD following nighttime noise and indications of oxidative stress in the blood vessels [53].
The endocrine responses to stress are mediated by two hormone axes, the sympathetic-adrenal-medullary system (SAM) and the hypothalamic-pituitary-adrenal (HPA) axis. On the one hand, the processing of auditory stimulation leads to a stress response [45]. Stress responses are mediated by the hypothalamus, which then activates the sympathetic nervous system [48, 55]. As a result, catecholamines—the hormones adrenaline and noradrenaline—are released from the adrenal medulla. These act on various organ systems; for example, cardiac activity and the blood flow to the muscles are increased. In addition, the blood pressure rises through vasoconstriction due to the activation of the renin-angiotensin-aldosterone system [55]. An evaluation of epidemiological studies on the connection between noise and the release of stress hormones found increased norepinephrine levels in people exposed to noise [51], supporting this explanation for noise-induced stress reactions.
The second way by which noise affects biological functions is the HPA axis [45]. This biochemical pathway is activated by the release of corticotropin-releasing hormone (CRH) in the hypothalamus. CRH then causes the release of adrenocorticotropin (ACTH) in the pituitary gland, which in turn activates the production of various hormones in the cortex of the suprarenal gland. These include cortisol as a glucocorticoid, which in response to the stressor stimulates the supply of energy in the body and enhances the catecholamine effect [56]. For cortisol, a dose-dependent increase was found with an increasing level of occupational noise exposure [57]. Individual noise sensitivity may also contribute to the physical or psychological effects of noise. Though several publications describe positive correlations between increased individual noise sensitivity and the occurrence of different health problems, i.e., sleep disturbances [58, 59] or noise annoyance [60], findings concerning a relationship between noise sensitivity and physical or mental health are inconsistent [61,62,63].
Next to noise sensitivity, multiple effect modifiers and mediators may influence the effects of (occupational) noise on health. Teixeira et al. [7••] propose a causal model which includes factors that mediate the relationship between occupational noise exposure and cardiovascular health via one of two pathways. On the first pathway, alcohol use, tobacco consumption, stress, and job strain are intermediate factors between noise exposure and cardiovascular disease. Blood pressure and obesity are suggested to mediate cardiovascular disease through an alternative pathway. Furthermore, Teixeira et al. [7••] also name factors that could act as effect modifiers, such as country, age, sex, socioeconomic position, occupation, or occupational factors.
With the knowledge of these pathomechanisms, it becomes clear that intense occupational noise exposure does not only affect anatomical structures of the inner ear but that it may also lead to non-auditory biological changes such as cardiovascular changes [51, 64].
Recent Reviews on Occupational Noise and Cardiovascular Health
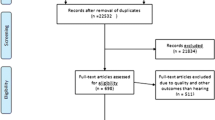
The last two decades have seen an increase in research on the non-auditory effects of noise exposure. A simple search of in PubMed (“noise, occupational”[MeSH Terms] OR “noise, transportation”[MeSH Terms]) NOT (“Hearing Loss, Noise-Induced”[MeSH Terms]) shows an increase in publications beginning around the year 2000. To summarize evidence from recent reviews on occupational noise exposure, we combined search terms for occupational noise exposure with the PubMed systematic review filter and conducted a (non-systematic) search of recent reviews. We sorted the reviews according to health outcome categories, outcomes and we describe the results of these reviews below, beginning with the outcome most frequently researched: cardiovascular disease. We also briefly summarized the findings for each major outcome category in Table 1.
Nine systematic reviews on the association between chronic occupational (and environmental) noise exposure and cardiovascular disease have been published since 2002 [7••, 8, 65,66,67,68, 70, 79,80,81]. Six of these were published in the last 5 years [7••, 8, 65,66,67,68, 70]. In general, recent systematic reviews repeatedly find associations between chronic noise exposure at work and an increased risk of cardiovascular disease. In the following section, the latest systematic reviews on cardiovascular disease and arterial hypertension will be discussed, including one co-authored by the authors of this paper [8].
In 2016, a systematic review was performed by Skogstad et al. [65] to investigate the effect of occupational noise exposure on cardiovascular disease incidence and mortality, which included prospective studies published between 2000 and 2013. Based on four studies examining workers exposed to noise exceeding 85 dB(A), the authors determined a statistically significant hazard ratio (HR) of 1.38 (95% confidence interval (CI) 1.01–1.87) for the development of arterial hypertension (defined as blood pressure ≥ 140/90 mmHg, hospital-diagnosed hypertension or intake of antihypertensive medication). In addition, statistically significant risk estimates were found regarding the development of cardiovascular diseases (relative risk (RR) = 1.34; 95% CI 1.15–1.56) and cardiovascular mortality (HR 1.12; 95% CI 1.02–1.24) in noise-exposed workers [65, 66].
Dzhambov and Dimitrova [67] also conducted a systematic review of occupational noise and ischemic heart disease (IHD). This review included cross-sectional and prospective studies, as well as studies using a self-rated noise exposure assessment and examining any level of occupational noise exposure. Although a meta-analysis was planned, the wide variety of risk estimates and assessment methods used in the original studies prevented a quantitative data synthesis. The qualitative summary of the 11 studies on IHD morbidity gave some evidence of an increased risk. That is, five out of six studies using a self-rated noise exposure assessment and three out of five studies examining objectively measured noise exposure reported an increased risk for IHD. Dzhambov and Dimitrova [67] also determined there might be an increased IHD risk for women based on two of the included studies [82, 83]. Regarding IHD mortality, the four included studies provided inconclusive results.
Another systematic review of hypertension risks was published in 2017 by Fu et al. [68], including occupational and environmental noise exposure. Of the 32 studies included in this systematic review, most were cross-sectional studies (n = 26). In total, the review shows an odds ratio (OR) of 1.62 (95% CI 1.40–1.88) for the risk of hypertension in people exposed to occupational or environmental noise. A subgroup analysis was performed for occupational noise exposure, resulting in an OR of 1.08 (95% CI 1.05–1.11; 17 studies). However, there were different levels of noise exposure in the exposed groups and comparison groups, respectively, and there was no definition given for hypertension [68]. Although traffic noise is typically lower, higher hypertension risks were found from the meta-analysis of road traffic (OR = 1.44; 95% CI 1.22–1.68; 7 studies) and air traffic noise (OR = 1.21; 95% CI 1.05–1.20; 6 studies). Fu et al. also examined the dose-response relationship between noise and hypertension. The linearity test found no indication of a linear association between noise and hypertension risks, but risk increased by 6% (95% CI 4% to 8%) per 10 dB(A) increase in noise.
Yang et al. [69] also conducted a systematic review examining the association between occupational noise exposure and hypertension (defined as blood pressure ≥ 140/90 mmHg) as well as electrocardiograph (ECG) abnormalities. In this review, only Chinese studies published between 2000 and 2017 were included. The meta-analysis yielded an OR of 2.55 (95% CI 1.94–3.36) for the risk of hypertension in subjects exposed to occupational noise exceeding 85 dB(A). A statistically significant effect estimate was also calculated in the analysis of ECG abnormalities. Although Yang et al. [69] point out that hypertension and ECG abnormalities are an incomplete depiction of cardiovascular health and exposure measurements in the original studies were inconsistent, they still regarded occupational noise as an important risk factor for cardiovascular disease.
In 2020, our research group performed a systematic review examining the influence of chronic occupational noise exposure on hypertension [8]. In contrast to the abovementioned publications, this review was carried out on observational epidemiological studies (including cross-sectional studies) regardless of their publication date, language, or country of origin. We used a variety of hypertension definitions, such as systolic arterial blood pressure ≥ 130 mmHg, diastolic arterial blood pressure ≥ 80 mmHg, physician-diagnosed arterial hypertension, or intake of anti-hypertensive medication. We only included studies with comparison groups exposed to noise levels of ≤ 80 dB(A) averaged over an 8-h work shift (Lex,8h). Overall, the pooled RR for occupational noise exceeding 80 dB(A) was 1.72 (95% CI 1.48–2.01) based on 23 studies (4 cohort; 19 cross-sectional). The effect estimate for the subgroup of studies applying the 140/90 mmHg hypertension definition currently used by the WHO [84] was statistically significant as well, amounting to 1.81 (95% CI 1.51–2.18). Furthermore, we observed a positive dose-response relationship between noise exposure and hypertension risk. Based on studies using the 140/90 mmHg hypertension definition, the risk estimate for workers exposed to noise between > 80 dB(A) and ≤ 85 dB(A) was 1.77 (95% CI 1.36–2.29), and increased to 3.50 (95% CI 1.56–7.86) for workers exposed to noise between > 85 dB(A) and ≤ 90 dB(A). Also, a sensitivity analysis of studies with noise exposures < 80 dB(A) did not find a statistically significant effect estimate (RR = 1.21; 95% CI 0.78–1.87). Additionally, we calculated an increased risk of 88% per 10 dB(A) increase in “working-life noise exposure” or noise averaged over (an assumed) 40 years of working life (Lex,40year) (RR = 1.88; 95% CI 1.12–3.15). For example, exposure to 85 dB(A) over approximately 16 years leads to a doubled hypertension risk in comparison to noise exposure of 70 dB(A) over 40 years [8].
Following our analyses, we used the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach to evaluate the entire body of evidence, adapting it for observational epidemiological studies according to the Navigation Guide [85,86,87]. Eight criteria were assessed: study limitations (risk of bias), indirectness of evidence, inconsistency of evidence, imprecision, publication bias, effect size, dose-response-gradient, and residual confounding. Starting with a moderate quality of evidence because only observational studies were included in the review, we downgraded once for publication bias because of the asymmetric funnel plot. We upgraded for dose-response-gradient (as described above), and effect size (RR in the subgroup of workers exposed to > 85 to ≤ 90 dB(A) was > 2). Based on this evaluation, we determined an overall high trustworthiness of evidence for occupational noise-related hypertension [8].
Recently, the WHO, together with the International Labour Organization (ILO), conducted a systematic review of longitudinal studies examining risks for ischemic heart disease, stroke, and hypertension in groups of workers exposed to quantified or self-reported noise ≥ 85 dB(A) [7••, 85]. Like Skogstad et al. [65], this review included only prospective and retrospective studies (cohort, case-control). Despite an extensive search of six electronic literature databases and databases of grey literature, including only longitudinal studies examining noise exposures ≥ 85 dB(A) limited the number of eligible studies. Further restrictions for the quantitative synthesis led to meta-analyses combining two to four studies per cardiovascular health outcome. Based on two cohort studies, Teixeira et al. [7••] found a risk increase for incident ischemic heart disease (RR = 1.29; 95% CI 1.15–1.43). The pooled risk for ischemic heart disease mortality included four studies but did not achieve statistical significance (RR = 1.22; 95% CI 0.94–2.02). Meta-analyses for stroke incidence (RR = 1.11; 95% CI 0.88–1.39; 2 studies), stroke mortality (RR = 1.02; 95% CI 0.93–1.12; 3 studies), and incident hypertension (RR = 1.07; 95% 0.90–1.28; 3 studies) also did not reach statistical significance.
The WHO/ILO review highlights the lack of research including women and the lack of longitudinal studies on occupational noise and cardiovascular outcomes. Longitudinal studies typically deliver more convincing evidence by establishing temporality and providing precise longitudinal exposure estimations. However, some of the included longitudinal studies on noise used subjective exposure assessments, and exposure estimates were dichotomized for the meta-analyses [7••]. Although cross-sectional studies examine only one time point, the fundamental importance of evidence from cross-sectional studies in determining an association should not be disregarded. At least with regard to hypertension, reverse causality—a fundamental problem with cross-sectional studies—is unlikely because uncomplicated hypertension is largely free of symptoms.
Other Non-auditory Health Effects of Noise
In 2016, Domingo-Pueyo et al. [88] reviewed the health effects of occupational noise exposure. The systematic search for studies was open-ended with regard to health outcomes, so that, much like a scoping review, the results gave an overview of occupational noise-related health effects researched until January 2015. Most of the primary studies identified researched the risk of NIHL or tinnitus (20 studies), while only four researched cardiovascular disease. Respiratory outcomes were additionally considered in one study of workers in the stone-crushing industry [89], and another study was on sleep disorders among noise-exposed rickshaw drivers [90].
In addition, systematic reviews examining associations between (occupational) noise and injuries [71•], reproductive outcomes [72, 73], diabetes [77], and acoustic neuroma [75, 76] were also published in the last decade.
Workplace Injury
Dzhambov and Dimitrova [71•] summarized the findings of 21 studies on noise-related injury risk. Noise exposure more than doubled the risk for work-related injury (RR = 2.16; 95% CI 1.61–2.90; 19 estimates) in a meta-analysis combining self-reported exposure and the highest categories of measured noise (> 80 dB(A)). A second meta-analysis of nine studies found the RR per 5 dB(A) was 1.22 (95% CI 1.15–1.29). At first glance, these results suggest that noise is associated with an increased risk of work-related injuries. However, when Dzhambov and Dimitrova [71•] applied the GRADE approach, they concluded that the evidence level for noise-related injury risk is very low due to inadequate adjustment of confounding in most of the original studies and publication bias.
Reproductive Outcomes
Stress during pregnancy can negatively impact fetal development [91]; thus, noise-induced stress may also increase the risk of adverse pregnancy and birth outcomes. In 2014, two reviews summarized the research of pregnancy-related outcomes, such as gestational size, low birth weight, and preterm births [72, 73]. Ristovska et al. [72] narratively summarized the findings from 14 occupational and nine environmental noise studies. This review determined that the studies were too few and heterogeneous to draw any definitive conclusions because some studies found increased risks only in combination with other workplace exposures, such as shift work.
In the same year, Dzhambov et al. [73•] published an update of a previous systematic review of occupational noise by Croteau et al. [92]. Dzhambov et al. [73•] used broader inclusion criteria (which included environmental noise studies) and detected statistically significantly increased risks for small for gestational age (RR = 1.19; 95% CI 1.03–1.38; 12 studies), gestational hypertension (RR = 1.27; 95% CI 1.21–1.79; 7 studies), and congenital malformations (RR = 1.47; 95% CI 1.21–1.79; 5 studies) for exposure to noise levels ≥ 80 dB(A). However, the studies included in this review used different exposure thresholds, so the meta-analysis compares two imprecise exposure categories (high versus low).
More recent results from the large population-based FENIX (fetal noise exposure cohort study) in Sweden also support these results [74•]. The FENIX study assessed occupational noise exposure using a job-exposure matrix and considered pregnancy outcomes for all single births in Sweden between 1992 and 2008. Among women working full-time with low absence from work (≤ 21 days), risks for small for gestational age and low birthweight followed a dose-response relationship for the noise exposure categories of < 75 dB(A), 75-84 dB(A), and ≥ 85 dB(A). Exposure to ≥ 85 dB(A) increased the risk of small for gestational age by 44% (RR = 1.44; 95% 1.01–2.03) and the risk for low birth weight by 36% (RR = 1.36; 95% CI 1.03–1.80) compared to < 75 dB(A) after adjusting for body mass index, smoking, parity, education, physically strenuous work, and low job control. A statistically significant increased risk of 13% was detected for preterm birth only for women exposed to 75–84 dB(A) (RR = 1.13; 95% CI 1.08, 1.18).
Acoustic Neuroma
Acoustic neuromas are benign intracranial tumors that develop on the nerve cells that originate in the inner ear and lead into the brain. In 1989, Preston-Martin et al. [93] hypothesized that acoustic trauma might promote cell proliferation and favor tumor growth induced initially by exposure to carcinogens such as radiation. Two systematic reviews looked at the evidence of an association between noise exposure and acoustic neuromas. Chen et al. [76] and Cao et al. [75] included eight case-control studies in their meta-analyses of noise. Both studies observed high heterogeneity and inconclusive results. In both reviews, overall analyses (ever exposed to noise) showed no (statistically significant) increased risk. Still, some sub-analyses showed increased risks for occupational noise exposure ≥ 5 years and for continuous occupational noise exposure [75].
Diabetes
Two systematic reviews examining a possible relationship between noise exposure and diabetes were published within the last years. Dzhambov [77] included 9 studies (4 for occupational and 5 for environmental noise). For residential noise exposure, an increased risk for type 2 diabetes could be found in people exposed to day-evening-night weighted noise (LDEN) > 60 dB(A) compared to people exposed to LDEN < 64 dB(A) with a relative risk of 1.22 (95% CI 1.09–1.37). However, for occupational noise exposure, the risk was not statistically significant (RR = 0.91; 95% CI 0.78–1.06). Although the authors report methodological differences between the studies, there was no heterogeneity detected. Overall, the results show that noise pollution might lead to endocrine health effects [77].
Another systematic review analyzing possible effects of long-term exposure to traffic, residential, or occupational noise on diabetes was conducted by Zare Sakhvidi et al. [78]. This study included 15 studies and combined nine in a meta-analysis (5 prospective cohort, 2 cross-sectional, and 2 case-control studies). The meta-analysis yielded a RR of 1.06 (95% CI 1.03–1.09) per 5 dB(A) increase in noise exposure irrespective of the source of the noise. Greater risk estimates were derived in source-specific analyses with regard to air traffic noise (OR = 1.17; 95% CI 1.06–1.29 per 5 dB increase in noise exposure) and road traffic noise (OR = 1.07; 95% CI 1.02–1.12). Both systematic reviews indicate possible noise-related endocrine effects of environmental noise, but further research is needed to explain the discrepancies between environmental and occupational noise exposure studies.
Evidence from Environmental Traffic Noise Studies
Studies of environmental traffic noise provide additional evidence of a connection between noise exposure and non-auditory health effects. Recently, a series of systematic reviews were conducted to examine the effect of environmental noise on health for the WHO environmental noise guidelines [9,10,11,12,13,14,15,16]. Regarding cardiovascular and metabolic effects due to noise exposure, a statistically significant relative risk of 1.08 (95% CI 1.01–1.15) per 10 dB(A) LDEN was estimated for the association between road traffic noise and incident ischemic heart disease [14]. This effect estimate suggests an association between noise exposure and cardiac effects, which is also observed in the reviews of occupational noise described above.
Cardiac effects of noise exposure were also examined as part of the German Noise-Related Annoyance, Cognition and Health (NORAH) study on disease risks. NORAH results were not included in the WHO reviews mentioned, as these were based on studies published prior to June 2015. The NORAH study on disease risks analyzed the relationship between exposure to traffic noise of L24h ≥ 40 dB(A) and risk of hypertensive heart disease or heart failure and found a positive, linear dose-response-relationship for all types of noise examined (road, rail, and aircraft noise) [94]. Regarding the development of arterial hypertension due to noise exposure, no statistically significant association was identified. However, a higher risk for arterial hypertension was found in people who developed hypertensive heart disease after being diagnosed with hypertension. In this subgroup, exposure to aircraft noise led to the highest risk estimate with an increased risk to develop hypertension of 13.9% per 10 dB(A) increase in sound pressure level [95]. The NORAH study on health risks also found increased odds for myocardial infarction with an OR of 1.028 (95% CI 1.012–1.045) per 10 dB(A) for road traffic noise and an OR of 1.023 per 10 dB(A) (95% CI 1.005–1.042) for railroad noise [96].
Noise-related sleep disturbances are an additional possible pathomechanism for the health effects associated with environmental traffic noise exposure that may be less applicable to occupational noise exposure. The WHO found the risk of being highly sleep-disturbed increased significantly per 10 dB(A) increase in nighttime noise (Lnight) due to aircraft, road, and rail traffic noise; the latter leading to the highest risk estimate of 1.27 (95% CI 0.89–1.81) [15]. Similarly, statistically significant (unadjusted) odds ratios were found for the probability of awakening for a 10 dB(A) increase in the maximum indoor noise levels (Lmax). Though, the authors reported a moderate to low quality of evidence according to the GRADE criteria [15].
For annoyance caused by traffic noise, a statistically significant, medium-strength relationship between noise levels and the percentages of highly annoyed people was identified [12]. Evidence of low or very low quality was found for the associations between aircraft noise and preterm birth, low birth weight, and congenital anomalies, as well as road traffic noise and low birth weight, preterm birth, and small for gestational age outcomes [11]. Due to limited data, the reviews exploring the association between environmental noise and the occurrence of permanent hearing loss and tinnitus [10], changes in cognition, as well as well-being and mental health, were less conclusive and did not include any meta-analyses [13, 16]. With regard to the aforementioned reviews, the evidence concerning the health effects of environmental noise is still limited. However, noise levels of environmental traffic noise are generally lower than occupational noise, so it is plausible that observed effects may be weaker and more difficult to detect. Further high-quality prospective studies should be carried out to increase the quality of evidence in this field.
Outlook and Interventions
International data on the prevalence of occupational NIHL shows that much work is still needed to prevent adverse health effects of occupational noise exposures effectively. Recently, a Cochrane review assessing non-pharmaceutical interventions on occupational noise exposure or occupational hearing loss which aim at reducing noise exposure to prevent NIHL was published by Tikka et al. [97•]. Initially published in 2009 [98], the review was updated for the second time in 2020. Studies using a randomized-controlled, controlled before-after or interrupted time-series study design, including workers exposed to noise exceeding 80 dB(A), were examined in this review. Out of these, 13 studies evaluated the effects of personal hearing protective devices (HPD), and 15 studies examined the effects of hearing loss prevention programs. For each outcome, the quality of evidence was rated according to the GRADE approach.
Multiple case studies (107 cases) of engineering control interventions were also considered by Tikka et al. [97•]. Engineering control interventions led to an immediate decrease in the absolute noise level (decrease ranging from 11.1 to 19.7 dB(A)). However, many studies suffered from the lack of a long-term follow-up, the absence of a control group, or a conflict of interest. For HPD, a noise reduction of about 20 dB(A) through HPD use was found in four studies (low-quality evidence). Moreover, moderate-quality evidence showed that personal instructions on using HPD correctly could lead to increased noise protection. Comparing earmuffs and earplugs as two possible HPDs, there was very low-quality evidence that earmuffs have a better effect than earplugs in high-level noise but a worse effect in low-level noise. Although supported by very low-quality evidence, the usage of HPDs could lead to less hearing loss at very long-term follow-ups [97•].
Regarding the effectiveness of hearing loss prevention programs, very low-quality evidence showed a decreased risk of hearing loss in workers with better HPD use. However, intensive or individualized information on noise exposure did not significantly affect noise levels or hearing loss. Additionally, one interrupted time-series study found that new legislation in the mining industry led to decreased noise levels of about 4.5 dB(A) in underground coal mining. Tikka et al. [97•] conclude that a modest decrease in noise exposure and hearing loss due to hearing loss prevention interventions could be found. However, the authors point out the necessity of studies of higher quality and better implementation of HPD and noise control measures.
The positive effect of the interventions examined by Tikka et al. [97•] refers to a decrease in NIHL as an auditory effect of noise. Therefore, the interventions may not be directly transferable to non-auditory effects of noise exposure, such as cardiovascular diseases. To the best of our knowledge, interventional studies or a review on the effect of hearing protection on non-auditory noise effects are not yet available. Further research is needed to determine whether specific interventions could reduce non-auditory health effects of occupational noise exposure.
In the last years, several papers were published dealing with the role of oxidative stress in the pathomechanisms of noise-induced stress. It was found that the administration of exogenous antioxidants can reduce noise-induced stress and could be used for prophylactic and therapeutic interventions [99,100,101]. In an animal model, oral administration of antioxidant vitamins and minerals helped prevent NIHL damage [102]. Oxidative stress as a possible pathomechanism and intervention target is an area of noise-related health research requiring further investigation.
Sheppard et al. [23•] recently summarized the occupational noise level regulations and recommendations shown in Table 2. They discuss how these regulations and recommendations attempt to strike a balance between preventing NIHL and hindering economic growth in a way that may underestimate the long-term healthcare costs of the acoustic and non-acoustic health effects. In their review, Sheppard et al. [23•] suggest that current methods for NIHL screening could be made more sensitive by screening for hearing loss at higher frequencies (> 10 kHz) and monitoring for other signs of cochlear damage. Current noise regulations will not prevent all occupational NIHL and overlook possible cardiovascular effects of noise-related stress responses, which may occur at lower noise levels.
Depending on the workplace setting and the character of the work, lower levels of occupational noise can also be a source of stress and annoyance. Background noise in open-space offices, especially background speech, is an encumbering disturbance for office workers. Schlittmeier and Liebl [103] summarized the results of three intervention studies which found that intelligible background speech consistently reduces working memory performance and increases perceived annoyance. Lowering noise levels and reducing the intelligibility of background speech was found to improve cognitive performance and mitigate disruptions. Thus, how different forms of lower occupational noise levels create stress and reduce productivity in different working situations requires additional research.
With regard to the measures mentioned in Table 2 and the interventions examined by Tikka et al. [97•], the fact that they mainly focus on individual prevention (i.e., earplugs or earmuffs as HPD) is notable. According to European work protection law, prevention methods for occupational NIHL should focus primarily on noise elimination or, if this is not possible, technical measures for noise reduction (working methods requiring less noise exposure or changes in work equipment). According to this procedure, organizational measures (i.e., limitation of exposure time and intensity) need to be implemented if the approaches mentioned above are not sufficient, and individual prevention has to be made available for the workers if technical and organizational measures do not adequately reduce noise exposure [104]. Therefore, future research and interventions should prioritize the prevention of ambient noise to reduce noise exposure at the workplace.
Conclusions
Recent data shows that not only is noise-induced hearing loss as an auditory effect of occupational noise exposure a continuing health problem worldwide but that there is increasing evidence for non-auditory consequences of occupational noise exposure. Multiple reviews indicate harmful effects of occupational noise on the cardiovascular system (i.e., hypertension), a higher risk for work-related injuries, as well as adverse reproductive outcomes. Non-pharmaceutical interventions (HPD, instructions on HPD use, engineering controls) have a moderate preventative effect on the occurrence of noise-induced hearing loss. Thus, future research should focus on the prevention of ambient noise to reduce NIHL. It can be presumed that consistent noise reduction can not only help to prevent NIHL but will also reduce non-auditory adverse health effects, such as hypertension and its secondary diseases. Furthermore, prospective studies of both men and women are needed to strengthen the evidence for non-auditory health effects of occupational noise, such as endocrine diseases. Also, further research on the epigenetic effects of noise will improve our understanding of how noise is impacting health.
Notes
DALY (disability-adjusted years of life lost) are a metric used to determine the overall burden of a disease or health condition in a population [21]. DALY are the sum of the disability-weighted number of years lived with a health condition (YLD) and the years of life lost to premature mortality (YLL) due to the health condition. Thereby, DALY provide a measure, which is suitable for assessing the burden of both non-fatal and fatal diseases.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
EWCS 2016. Are you exposed to loud noise? (Physical environment) visualisation : European bar chart by : Age, All - European Working Conditions Survey - Data visualisation. 2012. https://www.eurofound.europa.eu/data/european-working-conditions-survey?locale=EN&dataSource=EWCS2017NW&media=png&width=740&question=Q29b&plot=euBars&countryGroup=linear&subset=agecat_3&subsetValue=All.
Kerns E, Masterson EA, Themann CL, Calvert GM. Cardiovascular conditions, hearing difficulty, and occupational noise exposure within US industries and occupations. Am J Ind Med. 2018;61(6):477–91. https://doi.org/10.1002/ajim.22833.
Tak S, Davis RR, Calvert GM. Exposure to hazardous workplace noise and use of hearing protection devices among US workers--NHANES, 1999-2004. Am J Ind Med. 2009;52(5):358–71. https://doi.org/10.1002/ajim.20690.
Koskela K. Noise-induced hearing loss is still the most common confirmed occupational disease. In: Work-Life Knowledge Service. Finnish Institute of Occupational Health. 2020. https://www.worklifedata.fi/#/en/articles/analysisOccupationalDiseases-10-2020.
DGUV (Deutsche Gesetzliche Unfallversicherung e.V.). DGUV-Statistiken für die Praxis 2019 - Aktuelle Zahlen und Zeitreihen aus der Deutschen Gesetzlichen Unfallversicherung. Berlin2019 Contract No.: Webcode: p021547.
Kieffer C. Reporting of occupational diseases: issues and good practices in five European countries. Paris: EUROGIP 2015 Contract No.: Eurogip-102/E.
•• Teixeira LR, Pega F, Dzhambov AM, Bortkiewicz A, da Silva DTC, de Andrade CAF, et al. The effect of occupational exposure to noise on ischaemic heart disease, stroke and hypertension: a systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-Related Burden of Disease and Injury. Environ Int. 2021:106387. https://doi.org/10.1016/j.envint.2021.106387This review offers a current summary of longitudinal studies examining an association between occupational noise exposures ≥ 85 dB(A) and incident ischemic heart disease, ischemic heart disease mortality, incident stroke, stroke mortality and incident arterial hypertension.
•• Bolm-Audorff U, Hegewald J, Pretzsch A, Freiberg A, Nienhaus A, Seidler A. Occupational noise and hypertension risk: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(17). https://doi.org/10.3390/ijerph17176281Our own review offers an up-to-date and comprehensive overview of the evidence for an association between occupational noise exposures ≥80 dB(A) and the development of arterial hypertension.
Brown AL, Van Kamp I. WHO Environmental Noise Guidelines for the European Region: a systematic review of transport noise interventions and their impacts on health. Int J Environ Res Public Health. 2017;14(8):873.
Śliwińska-Kowalska M, Zaborowski K, WHO. Environmental Noise Guidelines for the European Region: a systematic review on environmental noise and permanent hearing loss and tinnitus. Int J Environ Res Public Health. 2017;14(10). https://doi.org/10.3390/ijerph14101139.
Nieuwenhuijsen MJ, Ristovska G, Dadvand P. WHO Environmental Noise Guidelines for the European Region: a systematic review on environmental noise and adverse birth outcomes. Int J Environ Res Public Health. 2017;14(10):1252.
Guski R, Schreckenberg D, Schuemer R. WHO Environmental Noise Guidelines for the European Region: a systematic review on environmental noise and annoyance. Int J Environ Res Public Health. 2017;14(12):1539.
Clark C, Paunovic K. WHO Environmental Noise Guidelines for the European Region: a systematic review on environmental noise and cognition. Int J Environ Res Public Health. 2018;15(2):285.
Van Kempen E, Casas M, Pershagen G, Foraster M. WHO Environmental Noise Guidelines for the European Region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int J Environ Res Public Health. 2018;15(2):379.
Basner M, McGuire S. WHO Environmental Noise Guidelines for the European Region: a systematic review on environmental noise and effects on sleep. Int J Environ Res Public Health. 2018;15(3):519.
Clark C, Paunovic K. WHO Environmental Noise Guidelines for the European Region: a systematic review on environmental noise and quality of life, wellbeing and mental health. Int J Environ Res Public Health. 2018;15(11):2400.
WHO. Deafness and hearing loss. World Health Organization. 2020. https://www.who.int/en/news-room/fact-sheets/detail/deafness-and-hearing-loss. Accessed 19.02.2020.
Konings A, Laer LV, Camp GV. Genetic studies on noise-induced hearing loss: a review. Ear Hear. 2009;30(2):151–9. https://doi.org/10.1097/AUD.0b013e3181987080.
Zhou J, Shi Z, Zhou L, Hu Y, Zhang M. Occupational noise-induced hearing loss in China: a systematic review and meta-analysis. BMJ Open. 2020;10(9):e039576. https://doi.org/10.1136/bmjopen-2020-039576.
Masterson EA, Deddens JA, Themann CL, Bertke S, Calvert GM. Trends in worker hearing loss by industry sector, 1981-2010. Am J Ind Med. 2015;58(4):392–401. https://doi.org/10.1002/ajim.22429.
World Health Organization. WHO methods and data sources for global burden of disease estimates 2000-2015. Geneva: WHO; 2017.
Nelson DI, Nelson RY, Concha-Barrientos M, Fingerhut M. The global burden of occupational noise-induced hearing loss. Am J Ind Med. 2005;48(6):446–58. https://doi.org/10.1002/ajim.20223.
• Sheppard A, Ralli M, Gilardi A, Salvi R. Occupational noise: auditory and non-auditory consequences. Int J Environ Res Public Health. 2020;17(23):8963 This narrative review provides an up-to-date comparison of current noise regulations and recommendations, as well as valuable insights into how to improve hearing loss monitoring.
Zhou H, Zhou Y, Zhang H, Yu A, Zhu B, Zhang L. Socio-economic disparity in the global burden of occupational noise-induced hearing loss: an analysis for 2017 and the trend since 1990. Occup Environ Med. 2021;78(2):125–8. https://doi.org/10.1136/oemed-2020-106556.
Mirza R, Kirchner DB, Dobie RA, Crawford J. Occupational noise-induced hearing loss. J Occup Environ Med. 2018;60(9):e498–501. https://doi.org/10.1097/jom.0000000000001423.
Daniel E. Noise and hearing loss: a review. The Journal of school health. 2007;77(5):225–31. https://doi.org/10.1111/j.1746-1561.2007.00197.x.
Girard SA, Leroux T, Courteau M, Picard M, Turcotte F, Richer O. Occupational noise exposure and noise-induced hearing loss are associated with work-related injuries leading to admission to hospital. Injury prevention : journal of the International Society for Child and Adolescent Injury Prevention. 2015;21(e1):e88–92. https://doi.org/10.1136/injuryprev-2013-040828.
Hong O, Kerr MJ, Poling GL, Dhar S. Understanding and preventing noise-induced hearing loss. Disease-a-month: DM. 2013;59(4):110–8. https://doi.org/10.1016/j.disamonth.2013.01.002.
Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. Auditory and non-auditory effects of noise on health. Lancet (London, England). 2014;383(9925):1325–32. https://doi.org/10.1016/s0140-6736(13)61613-x.
Lin FR, Yaffe K, Xia J, Xue Q-L, Harris TB, Purchase-Helzner E, et al. Hearing loss and cognitive decline in older adults. JAMA Intern Med. 2013;173(4):293–9. https://doi.org/10.1001/jamainternmed.2013.1868.
• Lie A, Skogstad M, Johannessen HA, Tynes T, Mehlum IS, Nordby KC, et al. Occupational noise exposure and hearing: a systematic review. Int Arch Occup Environ Health. 2016;89(3):351–72. https://doi.org/10.1007/s00420-015-1083-5This review conducted a thorough search and offers a comprehensive summary of general research on occupational noise-induced hearing loss.
Chen KH, Su SB, Chen KT. An overview of occupational noise-induced hearing loss among workers: epidemiology, pathogenesis, and preventive measures. Environ Health Prev Med. 2020;25(1):65. https://doi.org/10.1186/s12199-020-00906-0.
Masterson L, Howard J, Liu ZW, Phillips J. Asymmetrical hearing loss in cases of industrial noise exposure: a systematic review of the literature. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2016;37(8):998-1005. doi:https://doi.org/10.1097/mao.0000000000001104.
Mazitova NN, Adeninskaya EE, Pankova VB, Simonova NI, Fedina LN, Preobrazhenskaya EA, et al. Influence of occupational noise on hearing: systematic review of foreign literature. Med Tr Prom Ekol. 2017;2:48–53.
Masterson EA, Bushnell PT, Themann CL, Morata TC. Hearing impairment among noise-exposed workers—United States, 2003-2012. MMWR Morb Mortal Wkly Rep. 2016;65(15):389–94. https://doi.org/10.15585/mmwr.mm6515a2.
Strauss S, Swanepoel DW, Becker P, Hall JI, Eloff Z. Prevalence and degree of noise-induced hearing loss in South African gold miners. Occupational Health Southern Africa. 2012;18(6):20–5.
Dement J, Welch LS, Ringen K, Cranford K, Quinn P. Hearing loss among older construction workers: updated analyses. Am J Ind Med. 2018;61(4):326–35. https://doi.org/10.1002/ajim.22827.
Thurston FE. The workerʼs ear: a history of noise-induced hearing loss. Am J Ind Med. 2013;56(3):367–77. https://doi.org/10.1002/ajim.22095.
Hawkins JE, Schacht J. Sketches of otohistory. Part 10: noise-induced hearing loss. Audiol Neurootol. 2005;10(6):305–9. https://doi.org/10.1159/000087347.
Themann CL, Masterson EA. Occupational noise exposure: a review of its effects, epidemiology, and impact with recommendations for reducing its burden. J Acoust Soc Am. 2019;146(5):3879–905. https://doi.org/10.1121/1.5134465.
Le T, Straatman L, Lea J, Westerberg B. Current insights in noise-induced hearing loss: a literature review of the underlying mechanism, pathophysiology, asymmetry, and management options. J Otolaryngol Head Neck Surg. 2017;46:41. https://doi.org/10.1186/s40463-017-0219-x.
Felix RA 2nd, Gourevitch B, Portfors CV. Subcortical pathways: towards a better understanding of auditory disorders. Hear Res. 2018;362:48–60. https://doi.org/10.1016/j.heares.2018.01.008.
Hill K, Yuan H, Wang X, Sha SH. Noise-induced loss of hair cells and cochlear synaptopathy are mediated by the activation of AMPK. J Neurosci. 2016;36(28):7497–510. https://doi.org/10.1523/jneurosci.0782-16.2016.
Leso V, Fontana L, Finiello F, De Cicco L, Luigia Ercolano M, Iavicoli I. Noise induced epigenetic effects: a systematic review. Noise & health. 2020;22(107):77–89. https://doi.org/10.4103/nah.NAH_17_20.
Eriksson C, Petershagen G, Nilsson M. Biological mechanisms related to cardiovascular and metabolic effects by environmental noise. WHO Regional Office for Europe: Denmark; 2018.
Recio A, Linares C, Banegas JR, Diaz J. Road traffic noise effects on cardiovascular, respiratory, and metabolic health: an integrative model of biological mechanisms. Environ Res. 2016;146:359–70. https://doi.org/10.1016/j.envres.2015.12.036.
McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci. 1998;840:33–44. https://doi.org/10.1111/j.1749-6632.1998.tb09546.x.
Mocayar Maron FJ, Ferder L, Saravi FD, Manucha W. Hypertension linked to allostatic load: from psychosocial stress to inflammation and mitochondrial dysfunction. Stress. 2019;22(2):169–81. https://doi.org/10.1080/10253890.2018.1542683.
Daiber A, Kröller-Schön S, Oelze M, Hahad O, Li H, Schulz R, et al. Oxidative stress and inflammation contribute to traffic noise-induced vascular and cerebral dysfunction via uncoupling of nitric oxide synthases. Redox Biol. 2020;34:101506. https://doi.org/10.1016/j.redox.2020.101506.
Ising H, Kruppa B. Health effects caused by noise: evidence in the literature from the past 25 years. Noise and Health. 2004;6(22):5–13.
Babisch W. Stress hormones in the research on cardiovascular effects of noise. Noise & health. 2003;5(18):1–11.
Münzel T, Schmidt FP, Steven S, Herzog J, Daiber A, Sorensen M. Environmental noise and the cardiovascular system. J Am Coll Cardiol. 2018;71(6):688–97. https://doi.org/10.1016/j.jacc.2017.12.015.
Herzog J, Schmidt FP, Hahad O, Mahmoudpour SH, Mangold AK, Garcia Andreo P, et al. Acute exposure to nocturnal train noise induces endothelial dysfunction and pro-thromboinflammatory changes of the plasma proteome in healthy subjects. Basic Res Cardiol. 2019;114(6):46. https://doi.org/10.1007/s00395-019-0753-y.
Munzel T, Steven S, Hahad O, Daiber A. Noise and cardiovascular risk: nighttime aircraft noise acutely triggers cardiovascular death. Eur Heart J. 2021;42(8):844–6. https://doi.org/10.1093/eurheartj/ehaa984.
Ayada C, Toru Ü, Korkut Y. The relationship of stress and blood pressure effectors. Hippokratia. 2015;19(2):99–108.
Frodl T, O'Keane V. How does the brain deal with cumulative stress? A review with focus on developmental stress, HPA axis function and hippocampal structure in humans. Neurobiol Dis. 2013;52:24–37. https://doi.org/10.1016/j.nbd.2012.03.012.
Zare S, Baneshi MR, Hemmatjo R, Ahmadi S, Omidvar M, Dehaghi BF. The effect of occupational noise exposure on serum cortisol concentration of night-shift industrial workers: a field study. Saf Health Work. 2019;10(1):109–13. https://doi.org/10.1016/j.shaw.2018.07.002.
Marks A, Griefahn B. Associations between noise sensitivity and sleep, subjectively evaluated sleep quality, annoyance, and performance after exposure to nocturnal traffic noise. Noise and Health. 2007;9(34):1–7. https://doi.org/10.4103/1463-1741.34698.
Öhström E, Björkman M. Effects of noise-disturbed sleep—a laboratory study on habituation and subjective noise sensitivity. J Sound Vib. 1988;122(2):277–90. https://doi.org/10.1016/S0022-460X(88)80354-7.
Park SH, Lee PJ, Jeong JH. Effects of noise sensitivity on psychophysiological responses to building noise. Build Environ. 2018;136:302–11. https://doi.org/10.1016/j.buildenv.2018.03.061.
Stansfeld SA. Noise, noise sensitivity and psychiatric disorder: epidemiological and psychophysiological studies. Psychol Med. 1992;Suppl 22:1-44.
Schreckenberg D, Griefahn B, Meis M. The associations between noise sensitivity, reported physical and mental health, perceived environmental quality, and noise annoyance. Noise and Health. 2010;12(46):7–16. https://doi.org/10.4103/1463-1741.59995.
Shepherd D, Welch D, Dirks KN, Mathews R. Exploring the relationship between noise sensitivity, annoyance and health-related quality of life in a sample of adults exposed to environmental noise. Int J Environ Res Public Health. 2010;7(10):3579–94. https://doi.org/10.3390/ijerph7103580.
Ising H, Babisch W, Kruppa B. Noise-induced endocrine effects and cardiovascular risk. Noise and Health. 1999;1(4):37–48.
Skogstad M, Johannessen HA, Tynes T, Mehlum IS, Nordby KC, Lie A. Systematic review of the cardiovascular effects of occupational noise. Occupational medicine (Oxford, England). 2016;66(6):500. https://doi.org/10.1093/occmed/kqw113.
Skogstad M, Johannessen HA, Tynes T, Mehlum IS, Nordby K-C, Lie A. Corrigendum: systematic review of the cardiovascular effects of occupational noise Occupational medicine (Oxford, England). 2016;66(6):500.
Dzhambov AM, Dimitrova DD. Occupational noise and ischemic heart disease: a systematic review. Noise & health. 2016;18(83):167–77. https://doi.org/10.4103/1463-1741.189241.
Fu W, Wang C, Zou L, Liu Q, Gan Y, Yan S, et al. Association between exposure to noise and risk of hypertension: a meta-analysis of observational epidemiological studies. J Hypertens. 2017;35(12):2358–66. https://doi.org/10.1097/HJH.0000000000001504.
Yang Y, Zhang E, Zhang J, Chen S, Yu G, Liu X, et al. Relationship between occupational noise exposure and the risk factors of cardiovascular disease in China: a meta-analysis. Medicine (Baltimore). 2018;97(30):e11720–e. https://doi.org/10.1097/MD.0000000000011720.
Yang Y, Zhang E, Zhang J, Chen S, Yu G, Liu X, et al. Relationship between occupational noise exposure and the risk factors of cardiovascular disease in China: a meta-analysis. Medicine. 2018;97(30):e11720. https://doi.org/10.1097/md.0000000000011720.
• Dzhambov A, Dimitrova D. Occupational noise exposure and the risk for work-related injury: a systematic review and meta-analysis. Annals of work exposures and health. 2017;61(9):1037–53. https://doi.org/10.1093/annweh/wxx078This is the only systematic review to consider work-related injury and occupational noise exposure.
Ristovska G, Laszlo HE, Hansell AL. Reproductive outcomes associated with noise exposure—a systematic review of the literature. Int J Environ Res Public Health. 2014;11(8):7931–52. https://doi.org/10.3390/ijerph110807931.
• Dzhambov AM, Dimitrova DD, Dimitrakova ED. Noise exposure during pregnancy, birth outcomes and fetal development: meta-analyses using quality effects model. Folia Med. 2014;56(3):204–14. https://doi.org/10.2478/folmed-2014-0030This is the most recent and comprehensive systematic review and meta-analysis examining pregnancy and fetal development in association with occupational noise exposure.
• Selander J, Rylander L, Albin M, Rosenhall U, Lewné M, Gustavsson P. Full-time exposure to occupational noise during pregnancy was associated with reduced birth weight in a nationwide cohort study of Swedish women. Sci Total Environ. 2019;651:1137–43. https://doi.org/10.1016/j.scitotenv.2018.09.212This is a large population-based study of pregnancy outcomes that updates and supports the findings of the most recent systematic reviews on occupational noise and reproductive outcomes.
Cao Z, Zhao F, Mulugeta H. Noise exposure as a risk factor for acoustic neuroma: a systematic review and meta-analysis. Int J Audiol. 2019;58(9):525–32. https://doi.org/10.1080/14992027.2019.1602289.
Chen M, Fan Z, Zheng X, Cao F, Wang L. Risk factors of acoustic neuroma: systematic review and meta-analysis. Yonsei Med J. 2016;57(3):776–83. https://doi.org/10.3349/ymj.2016.57.3.776.
Dzhambov AM. Long-term noise exposure and the risk for type 2 diabetes: a meta-analysis. Noise & health. 2015;17(74):23–33. https://doi.org/10.4103/1463-1741.149571.
Zare Sakhvidi MJ, Zare Sakhvidi F, Mehrparvar AH, Foraster M, Dadvand P. Association between noise exposure and diabetes: a systematic review and meta-analysis. Environ Res. 2018;166:647–57. https://doi.org/10.1016/j.envres.2018.05.011.
van Kempen EE, Kruize H, Boshuizen HC, Ameling CB, Staatsen BA, de Hollander AE. The association between noise exposure and blood pressure and ischemic heart disease: a meta-analysis. Environ Health Perspect. 2002;110(3):307–17. https://doi.org/10.1289/ehp.02110307.
Tomei G, Fioravanti M, Cerratti D, Sancini A, Tomao E, Rosati MV, et al. Occupational exposure to noise and the cardiovascular system: a meta-analysis. Sci Total Environ. 2010;408(4):681–9. https://doi.org/10.1016/j.scitotenv.2009.10.071.
Hwang WJ, Hong O. Work-related cardiovascular disease risk factors using a socioecological approach: implications for practice and research. European journal of cardiovascular nursing : journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology. 2012;11(1):114–26. https://doi.org/10.1177/1474515111430890.
Dimitrova T, Karaslavova E. Vibrations in the working environment and risk of acute myocardial infarction. Meditsinski Pregled/Medical Review. 2008;44(4):54–7.
Kersten N, Backe E. Occupational noise and myocardial infarction: considerations on the interrelation of noise with job demands. Noise & health. 2015;17(75):116–22. https://doi.org/10.4103/1463-1741.153403.
WHO. Hypertension. World Health Organization. 2019. https://www.who.int/news-room/fact-sheets/detail/hypertension. Accessed 20.02.2021.
Teixeira LR, Azevedo TM, Bortkiewicz A, Correa da Silva DT, de Abreu W, de Almeida MS, et al. WHO/ILO work-related burden of disease and injury: protocol for systematic reviews of exposure to occupational noise and of the effect of exposure to occupational noise on cardiovascular disease. Environ Int. 2019;125:567–78. https://doi.org/10.1016/j.envint.2018.09.040.
Woodruff TJ, Sutton P. The Navigation Guide systematic review methodology: a rigorous and transparent method for translating environmental health science into better health outcomes. Environ Health Perspect. 2014;122(10):1007–14. https://doi.org/10.1289/ehp.1307175.
Schünemann H, Brożek J, Guyatt G, Oxman A. Grade handbook for grading quality of evidence and strength of recommendations. Updated october 2013. The grade working group, 2013. 2013.
Domingo-Pueyo A, Sanz-Valero J, Wanden-Berghe C. Disorders induced by direct occupational exposure to noise: systematic review. Noise & health. 2016;18(84):229–39. https://doi.org/10.4103/1463-1741.192479.
Kitcher E, Ocansey G, Tumpi D. Early occupational hearing loss of workers in a stone crushing industry: our experience in a developing country. Noise and Health. 2012;14(57):68–71. https://doi.org/10.4103/1463-1741.95134.
Gitanjali B, Dhamodharan R. Effect of occupational noise on the nocturnal sleep architecture of healthy subjects. Indian J Physiol Pharmacol. 2004;48(1):65–72.
Mulder EJ, Robles de Medina PG, Huizink AC, Van den Bergh BR, Buitelaar JK, Visser GH. Prenatal maternal stress: effects on pregnancy and the (unborn) child. Early Hum Dev. 2002;70(1-2):3–14. https://doi.org/10.1016/s0378-3782(02)00075-0.
Croteau A, Poulin M, Goulet L, Trottier M. Effets du bruit en milieu de travail durant la grossesse: synthèse systématique avec méta-analyse et méta-régression [Effects of noise in the workplace during pregnancy: systematic review with meta-analysis and meta-regression]: Institut national de santé publique du Québec 2009.
Preston-Martin S, Thomas DC, Wright WE, Henderson BE. Noise trauma in the aetiology of acoustic neuromas in men in Los Angeles County, 1978-1985. Br J Cancer. 1989;59(5):783–6. https://doi.org/10.1038/bjc.1989.163.
Seidler A, Wagner M, Schubert M, Dröge P, Römer K, Pons-Kühnemann J, et al. Aircraft, road and railway traffic noise as risk factors for heart failure and hypertensive heart disease—a case-control study based on secondary data. Int J Hyg Environ Health. 2016;219(8):749–58. https://doi.org/10.1016/j.ijheh.2016.09.012.
Zeeb H, Hegewald J, Schubert M, Wagner M, Dröge P, Swart E, et al. Traffic noise and hypertension—results from a large case-control study. Environ Res. 2017;157:110–7. https://doi.org/10.1016/j.envres.2017.05.019.
Seidler A, Wagner M, Schubert M, Dröge P, Pons-Kühnemann J, Swart E, et al. Myocardial infarction risk due to aircraft, road, and rail traffic noise: results of a case–control study based on secondary data. Dtsch Arztebl Int. 2016;113(24):407–14.
• Tikka C, Verbeek J, Kateman E, Morata TC, Dreschler W, Ferrite S. Cochrane method for systematic review and meta-analysis of interventions to prevent occupational noise-induced hearing loss - abridged. CoDAS. 2020;32(2):e20190127. https://doi.org/10.1590/2317-1782/20192019127This review updates a comprehensive Cochrane review on interventions to prevent occupational noise-induced hearing loss, and provides an up-to-date summary of the evidence.
Verbeek JH, Kateman E, Morata TC, Dreschler W, Sorgdrager B. Interventions to prevent occupational noise induced hearing loss. The Cochrane database of systematic reviews. 2009(3). Cd006396. https://doi.org/10.1002/14651858.CD006396.pub2.
Falasca V, Greco A, Ralli M. Noise induced hearing loss: the role of oxidative stress. Otolaryngol Open J. 2017;5:1–5.
Isaac O, Victor O. Mitigative effects of antioxidants in noise stress. Journal of Clinical Nutrition & Dietetics. 2017;3(03).
Panjali Z, Jafari-Tehrani B, Münzel T, Hahad O, Tansaz M, Hamidi M, et al. Effect of tea consumption on oxidative stress and expression of DNA repair genes among metal press workers exposed to occupational noise. Toxicology research. 2021;10(1):134–40. https://doi.org/10.1093/toxres/tfaa101.
Alvarado JC, Fuentes-Santamaria V, Melgar-Rojas P, Gabaldon-Ull MC, Cabanes-Sanchis JJ, Juiz JM. Oral antioxidant vitamins and magnesium limit noise-induced hearing loss by promoting sensory hair cell survival: role of antioxidant enzymes and apoptosis genes. Antioxidants (Basel). 2020;9(12). https://doi.org/10.3390/antiox9121177.
Schlittmeier SJ, Liebl A. The effects of intelligible irrelevant background speech in offices—cognitive disturbance, annoyance, and solutions. Facilities. 2015;33(1/2):61–75. https://doi.org/10.1108/F-05-2013-0036.
European Parliament and Council. Directive 2003/10/EC of the European Parliament and of the Council on the minimum health and safety requirements regarding the exposure of workers to the risks arising from physical agents (noise). 2003.
Acknowledgements
We would like to thank the anonymous reviewers for their valuable suggestions.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors co-authored one of the reviews described in this paper [8••].
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Noise Pollution
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pretzsch, A., Seidler, A. & Hegewald, J. Health Effects of Occupational Noise. Curr Pollution Rep 7, 344–358 (2021). https://doi.org/10.1007/s40726-021-00194-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40726-021-00194-4