Abstract
Purpose of Review
We highlight evidence within the last 5 years of racial and ethnic differences in sleep-memory associations and explore potential causes and treatments of poor sleep in minoritized racial and ethnic groups.
Recent Findings
Emerging research suggests that memory performance in Black adults may be more sensitive to sleep quality than in White adults. Sleep quality and sleep duration are also associated with memory performance in other minoritized racial and ethnic groups, including Asian and Hispanic adults. However, comparisons between groups are scarce.
Summary
Poor sleep is associated with poor memory outcomes in minoritized racial and ethnic groups. Social determinants of health, including racism-related stress, discrimination, and neighborhood conditions, may contribute to these associations. More experimental and epidemiology research is needed to fully understand the relationship between sleep and memory performance in minoritized racial and ethnic groups. We conclude with suggested future directions for sleep and memory research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The association between sleep and episodic memory performance is well documented [1,2,3,4]. Many studies have shown that sleep allows for the consolidation of episodic memories, and higher sleep quality is associated with higher memory performance [2, 4]. Racial and ethnic group differences in these associations are understudied, as a recent meta-analysis from our lab showed that less than 5% of studies on sleep-memory associations reported racial and ethnic information [4].
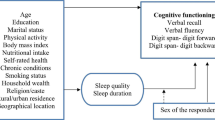
Minoritized racial and ethnic groups, including Asian, non-Hispanic Black, and Hispanic people, tend to sleep less and more poorly than non-Hispanic White people (hereafter referred to as Asian, Black, Hispanic, and White) [5]. In parallel with poor sleep quality and low sleep duration, minoritized racial and ethnic groups, particularly Black and Hispanic adults, are at higher risk of dementia and lower memory performance than White adults [6,7,8]. Social determinants of health, such as neighborhood problems, stress, and discrimination, may contribute to racial and ethnic sleep disparities in sleep, dementia, and memory performance [5, 9,10,11,12,13,14]. Furthermore, these factors may influence racial and ethnic differences in the relationship between sleep quality and episodic memory performance, such that poor sleep quality, in addition to other stressors, might exacerbate memory problems. Although there is substantial research on racial and ethnic disparities in both sleep and memory separately, there is little research investigating the potential association between poor sleep quality/duration with low memory performance in minoritized racial and ethnic groups. In this review, we discuss the existing research on sleep-memory associations in people from minoritized racial and ethnic groups.
Given the lack of consensus for measures of poor sleep that impact memory performance, we review both sleep quality and sleep duration. We define poor sleep as low sleep quality, as measured by self-report, actigraphy, or polysomnography. We also consider sleep duration at low and high extremes as poor sleep, and extremes in sleep duration vary by study (e.g., < 5 to 7 or > 9 to 10 h of sleep) [15, 16]. In alignment with recent guidelines [17], we discuss race and ethnicity as an index of experiences with racism and discrimination. We do not discuss racial and ethnic identity for genetic variation or any other biological variable. We name racial and ethnic groups using recommendations from the National Institutes of Health [18], specifically as Asian, non-Hispanic Black, Hispanic/Latino/a/x, and non-Hispanic White. For brevity, we refer to these groups as Asian, Black, Hispanic, and White, respectively.
Sleep Is Associated with Episodic Memory Performance Across the Adult Lifespan
Numerous sleep deprivation, brain stimulation, and correlational studies support an important role of sleep in the promotion of episodic learning and retention [2, 19]. Neurocomputational theories based largely on data from rodents suggest that sleep promotes memory through the redistribution of recently encoded memory representations from the medial temporal lobe to the neocortex, thereby promoting their stability, while at the same time restoring the brain’s capacity to encode new events [20]. Sleep-based memory consolidation is evident in cognitively unimpaired healthy older adults, as well as middle-aged adults [2].
Given the strong association between sleep and memory shown in younger adults, it seems plausible that age-related sleep disruptions may contribute to those in episodic memory performance. However, results from studies of older adults are mixed [19]. Imprecise selection of memory tests not sensitive to aging, including item rather than associative memory, poor control of factors affecting sleep (e.g., medications, depression), and inadequate measures of sleep (i.e., self-report only), may contribute to these mixed findings. When studies account for these factors, age-related sleep disruptions typically contribute to episodic memory impairment. For example, more minutes spent awake after falling asleep predicts worse delayed verbal recall in older adults [21]. We have shown that individuals with greater night-to-night variability in sleep quality, measured using 1 week of wrist actigraphy, had worse episodic memory performance, and this relationship was stronger with increasing age [22, 23]. Our recent meta-analysis of studies employing subjective, actigraphy, and polysomnography sleep measurement methods showed that young and older adults show similar positive associations between sleep quality and episodic memory performance [4]. Collectively, these results point to individual differences in sleep as a modifiable lifestyle factor that may contribute to individual differences in episodic memory across the adult lifespan.
Comparing Study Designs for Experimental and Epidemiological Research on Associations between Sleep Quality and Memory Performance
Epidemiological and experimental studies have unique strengths and weaknesses. An important strength of epidemiological studies is that they are typically based in large participant samples to assess disease and health outcomes. These large studies allow for advanced statistical modeling, including longitudinal data analyses to assess causal inference and directionality. Epidemiology-based studies also have several weaknesses. For example, although they are highly powered to statistically control for several confounding factors, epidemiology studies often include participants with health issues, including cardiovascular disease and cognitive impairment, which may affect associations between sleep quality and memory performance [19]. Moreover, large participant samples preclude highly detailed memory assessments, such as the neural mechanisms of encoding and retrieval, that can be captured with experimental study designs.
A key strength of experimental research studies of sleep-memory associations is the detailed assessments of sleep quality and memory performance. In experimental research studies, sleep quality is often measured with objective sleep metrics, such as polysomnography and actigraphy [4]. Furthermore, memory assessments capture task-related neural activity during memory encoding and memory retrieval, differing from neuropsychological memory tasks (e.g., word list recall) in epidemiology studies. However, experimental participant samples are typically smaller and often based on convenience sampling, which is a limiting factor for racial and ethnic diversity in experimental research.
Epidemiology and experimental studies are necessary for a full understanding of sleep-memory associations. Epidemiology research studies often report racial and ethnic demographics, and a few stratify by or target specific racial and ethnic groups to assess sleep-memory associations [24, 25]. Most experimental research studies on sleep quality and memory performance are largely opaque about the participants who make up their samples and rarely assess for racial and ethnic group differences [4]. Below, we discuss the current findings from both methodological approaches on sleep-memory associations in Black, Hispanic, and Asian adults.
Emerging Evidence on Racial and Ethnic Differences in Sleep-Memory Associations
There is a dearth of research on racial and ethnic differences in sleep-memory associations. To date, there is no research on sleep-memory associations in Pacific Islander, Alaska Native, nor American Indian adults. The research studies on the cognitive consequences of poor sleep quality in Hispanic and Asian adults are rare. Most of the sleep research in minoritized racial and ethnic groups is in Black adults, and only a few studies that have compared sleep-memory associations within the same study protocol [22,23,24,25]. Some evidence demonstrates that Black adults show stronger relationships between sleep quality and memory performance than White adults [24, 25].
Social and environmental factors may underlie racial and ethnic group differences in sleep-memory associations. As compared to White adults, minoritized groups are disproportionately affected by neighborhood disadvantages, financial strain, and discrimination, all of which are associated with poor sleep. [5, 9, 10, 12, 14, 26, 27] These negative factors may combine and worsen the detrimental effects of poor sleep quality on poor memory performance. We discuss sleep-memory associations in Black, Hispanic, and Asian people below.
Black People
Several studies have assessed sleep-memory associations in Black people [22,23,24,25, 28]. Our experimental research suggests that Black adults demonstrate lower memory-related neural activity than White adults when they have poorer actigraphy-measured sleep quality [22]. Specifically, higher night-to-night variance in sleep quality was associated with lower memory-related neural oscillations, measured using electroencephalography, in Black adults, but not White adults. In a similar follow-up study, we found that people from minoritized racial and ethnic backgrounds, who predominately identified as Black, showed stronger associations between night-to-night sleep variance and encoding-retrieval neural similarity of electroencephalography patterns, an index of memory specificity, than White adults [23].
With larger participant samples, emerging epidemiological research shows that these racial and ethnic differences are also present at the behavioral level [24, 25]. Two studies found that actigraphy-measured poorer sleep quality, including higher sleep fragmentation, was associated with worse memory performance in older Black, but not older White adults (mean ages: 65 ± 3; 73 ± 10 years) [24, 25]. In a predominately Black participant sample of older adults (mean age: 68 ± 9 years), increases in actigraphy-measured sleep efficiency over a 5-year period were associated with higher recall performance [28]. In each of these studies [24, 25, 28], Black participants reported high levels of co-morbidities, including hypertension, high blood sugar, and other risk factors for cardiovascular disease. However, sleep-memory associations remained after adjusting for co-morbidities.
Taken together, sleep in Black people may be more strongly associated with memory performance than in White people. Environmental and systemic barriers to sleep, such as neighborhood disorder and discrimination, by which Black people are disproportionately affected, may exacerbate the negative effects of poor quality sleep on memory, as discussed further below [5, 12, 22].
Hispanic People
Studies of sleep-memory associations in Hispanic adults are sparse, and to date, no studies have compared sleep-memory associations between Hispanic people with other racial and ethnic groups. However, some epidemiological evidence suggests that memory performance is sensitive to self-reported sleep duration in Hispanic adults [15, 29, 30]. The Hispanic Community Health Study/Study of Latinos is the largest longitudinal study of Hispanic/Latino adults in the USA. In a related ancillary study, Study of Latinos-Investigation of Neurocognitive Aging, researchers measured word list memory recall performance with the Spanish English Verbal Learning Test and found associations between long sleep duration, low memory performance, and memory decline (discussed below) [15, 29, 30].
In a sample of 8676 Hispanic adults (45–74 years of age), both long and short sleep durations were associated with poorer episodic memory performance [29]. The unadjusted inflection point of the curvilinear regression analysis was 7.2 h for memory performance for total and delayed recall, demonstrating that sleep durations shorter and longer than 7.2 h were associated with poorer memory performance. In a follow-up longitudinal study of 5247 Hispanic adults, longer self-reported sleep duration (> 9 h) was associated with a 7-year decline in memory performance [15]. Similarly, obesity strengthens the association between longer sleep duration (> 9 h) and decline in memory performance, particularly in adults older than 65 years of age, suggesting that metabolic health may play an important moderating role in sleep-memory associations [30].
Taken together, Hispanic adults show associations between sleep duration and memory performance, such that short and long sleep durations are related to poorer memory performance [15, 29]. However, objective measurements of sleep are needed in this population to thoroughly assess sleep-memory associations, especially involving relationships between sleep quality metrics, in addition to sleep duration, and memory performance.
Asian People
Similar to Black and Hispanic adults, Asian adults also show poorer sleep quality than non-Hispanic White adults [31]. However, few studies have investigated associations between sleep quality and memory performance in Asian adults [16, 25, 32, 33], and only one compared sleep-memory associations in Asian people to other racial and ethnic groups [25].
Two such epidemiological studies were conducted using data from the Chinese Health and Retirement Longitudinal Study (CHARLS), a longitudinal study of over 3000 Chinese adults aged 60 and older [32, 33]. These studies found associations between self-reported afternoon nap duration and nocturnal sleep duration and memory performance, assessed with a composite metric of immediate and delayed recall of a list of 10 words. Those who reported napping for more than 90 min demonstrated decline in memory performance from baseline (2011) to follow-up (2013), but memory performance for those in shorter nap groups showed no significant decline [32]. Similarly, a separate analysis done in CHARLS revealed that older Chinese adults with longer nocturnal sleep duration at baseline demonstrated poor baseline memory performance. Interestingly, long afternoon naps (> 90 min) were positively associated with baseline memory performance in men, but negatively in women [33]. An additional epidemiology study, the Guangzhou Biobank Cohort Study, assessed longitudinal associations between self-reported sleep duration and memory recall performance decline after an average of 4.1 years in 13,888 older Chinese adults [16]. They found that older Chinese people with short (≤ 5 h) and long (≥ 10 h) sleep durations showed greater memory decline as compared to those who reported sleeping 7 h. They also found that those who reported napping more often (daily) had greater memory decline than those with lower napping frequency (1–3 × /week). To date, only one study has compared sleep-memory associations in older Asian and White adults [25]. In the Study of Women’s Health Across the Nation, compared to older White women, older Chinese and Japanese women showed similar associations between higher actigraphy-measured sleep fragmentation and lower memory recall performance.
The association between poor sleep and poor memory performance is in alignment with previous research [2, 4]; however, sex may illustrate an effect modifier distinctive of older Chinese adults. More research is needed on intersectionality, including racial and ethnic group and sex differences, in the relationship between sleep and memory performance. The research on sleep-memory associations in Asian adults is scarce and limited to epidemiological studies based in primarily older Chinese adults. To better assess if there are unique cognitive consequences of poor sleep quality in Asian adults, future research should investigate associations between sleep quality and memory performance in Asian adults across the lifespan.
What is the Relationship between Stress and Sleep?
Numerous studies have identified bidirectional associations between both acute and chronic stress and sleep disturbances [34]. Acute stressors, whether psychological or physical, lead to activation of the hypothalamic–pituitary–adrenal axis (HPA), in turn, releasing several stress hormones that promote wakefulness and alter levels of non-rapid eye movement sleep (i.e., NREM) and REM sleep through a number of complex mechanisms still being investigated. On the flip side, even short-term sleep disruption can lead to increased sympathetic arousal including levels of stress hormones like cortisol [35]. Most relevant to the current paper is the association between chronic stress and sleep. There are several reasons to think that the chronic stress that minoritized racial and ethnic groups experience may contribute to or exacerbate sleep disparities. First, structural factors, including low socioeconomic status, financial strain, and shift work independently contribute to sleep loss, are often more common in minoritized racial and ethnic groups, and associated with chronic stress [11, 26, 36, 37].
Second, many studies have reported negative associations between self-reported experience of racial and ethnic discrimination (e.g., “You were discouraged by a teacher or advisor from seeking higher education”) and lower sleep quality and quantity in minoritized racial and ethnic groups, with level of discrimination partially explaining sleep disparities [12]. A recent study showed that young adults from multiple racial and ethnic groups (Asian, Black, Hispanic) reporting higher trait levels of rumination and anxiety sensitivity were most likely to experience discrimination-related sleep disturbance [38]. These results are promising for future interventions as rumination and anxiety sensitivity are amenable to treatment through cognitive behavioral therapy [39, 40].
Third, foreign-born individuals from minoritized racial and ethnic groups may additionally experience stress related to acculturating to their host country (i.e., acculturative stress) that may contribute to poor sleep. Acculturative stress encompasses factors related to perceived discrimination, fear of personal safety, homesickness, and culture shock. Large-scale epidemiological studies have shown that higher levels of acculturative stress are predictive of greater sleep disturbance (sleep quantity, sleep continuity) in Hispanic and Asian American adults [41]. Importantly, not all individuals within minoritized racial and ethnic groups have similar ethnic identity. Acculturative stress-sleep relationships may be strongest in those with stronger ethnic identity. For example, in one recent study, among middle-aged and older Chinese and Korean immigrants to the USA, only those identifying as “very Asian” and not those identifying as bicultural or “Western” showed negative associations between acculturative stress and sleep duration [42]. The authors argued that individuals with stronger ethnic identity may feel more disturbed by acculturative stress, which may, in turn, negatively impact their sleep. It should be noted that ethnic identity sometimes confers protection against the negative impact of perceived discrimination, as shown in a recent meta-analysis, which may vary according to outcome measure and racial and ethnic group [43].
Collectively, these studies suggest that minoritized racial and ethnic groups are disproportionately affected by several chronic stressors that are related to poor sleep. Given that chronic stress is known to negatively impact neural integrity and in turn, episodic memory [44], it seems plausible that chronic stress could independently [45], or perhaps interactively with poor sleep, be linked to worse episodic memory outcomes in minoritized racial and ethnic groups. However, more research is needed to evaluate this claim.
Sleep Intervention Studies in Minoritized Racial and Ethnic Groups
Only a few sleep intervention studies have been tailored to minoritized racial and ethnic groups. According to a recent review, only 6.97% of sleep intervention studies targeted populations that are underserved in research (e.g., minoritized racial and ethnic groups) [46]. Although few sleep intervention studies include racially and ethnically diverse samples [10, 47,48,49], the existing literature suggests that there are racial and ethnic differences in efficacy and acceptability of sleep interventions. Recent evidence demonstrates that sleep interventions in non-Hispanic White adults may show different effects in people from minoritized groups [47, 48]. For example, a sleep intervention study in adolescents found that sending text message reminders to prepare for bed and to get into bed at a specific time resulted in increased sleep duration in White adolescents, but not those from minoritized racial and ethnic groups [48]. The researchers concluded that environmental barriers, such as noisy neighborhoods, may interfere with sleep in minoritized racial and ethnic groups. Thus, those in the minoritized racial and ethnic groups were likely not ignoring the reminders but faced environmental challenges with getting to bed and to sleep at the specified time.
The neighborhood environment has been associated with sleep duration and sleep quality in Black and Hispanic adults [5, 10, 50, 51]. For example, people who perceive their neighborhoods to be safer and less violent show higher self-reported [5, 50, 51] and actigraphy-measured sleep quality [10]. Improving the neighborhood environment, then, may lead to better sleep quality. One quasi-experimental neighborhood intervention study demonstrated that higher neighborhood investments (e.g., grocery stores, greenspace, housing) were related to improved actigraphy-measured sleep duration and sleep quality in predominately Black adults over a 3-year period [9]. Specifically, people who lived closer to neighborhood developments demonstrated increases in sleep duration, decreases in minutes spent awake during the night, and lower decline in sleep efficiency as compared to those who did not live near an investment.
Social factors may also contribute to racial and ethnic differences in sleep intervention outcomes. Qualitative research has demonstrated that Black adults were more accepting of peer educators than medical staff [49, 52]. When Black people with sleep apnea were given instructions on treatment from a peer educator, they were more likely to seek treatment for sleep apnea at community health centers [52]. Similarly, Black adults prefer representation of other Black people when engaging with mobile applications [47]. A sleep intervention study to assess feasibility of the Headspace mobile application showed that people from minoritized racial and ethnic groups, including Asian, Black, and Hispanic adults, preferred more racial and ethnic diversity in meditation instructors [47].
Given that Asian, Black, and Hispanic people are at higher risk of poor sleep than White people [31], more sleep intervention research is needed in these groups. Some research suggests that individual-level interventions operate differently in minoritized racial and ethnic groups than in non-Hispanic White people [47, 48]. Black adults reported preferring a Black meditation instructor in a relaxation-based, feasibility sleep intervention [47]. Similarly, while simple text message reminders for light dimming and bedtimes improved sleep in White adolescents, the reminders did not improve sleep in those from racially and ethnically diverse backgrounds [48]. By contrast, neighborhood-level interventions have shown particularly promising results [10]. Investing in neighborhoods was not only related to improved sleep quality in older Black adults[10] but also those with better sleep quality demonstrated higher memory performance (see the “Emerging Evidence on Racial and Ethnic Differences in Sleep-Memory Associations” section).[28] Taken together, more sleep intervention research is warranted in minoritized racial and ethnic groups, as improving sleep quality may lead to better cognitive performance, thereby reducing racial and ethnic disparities in sleep and cognition.
Future Directions for the Field
We have identified several open questions and under-explored topics that should be investigated in future studies.
-
1)
Researchers should aim to better understand differences in sleep-memory associations among subpopulations of minoritized racial and ethnic groups and sex/gender identity groups, specifically with respect to differing experiences with chronic stressors (e.g., discrimination, acculturative stress, financial stress, food insecurity). That is, most epidemiological studies have not separated broad racial and ethnic group categories. Little research has been conducted on group subpopulations within broader racial and ethnic groups (e.g., Hispanic people: Mexican, Cuban) and no research on Indigenous peoples. People within a group likely experience different levels of stress (e.g., discrimination and/or acculturative stress) depending on contextual factors, including the region in which they live (e.g., border towns, rural/urban city), skin tone, workplace dynamics, social support, and access to healthcare. Moreover, sleep quality and quantity vary by sex, which may impact associations between sleep and memory [2]. A better understanding of these individual difference factors, sex/gender identity, and others is needed to assess moderating and mediating roles of racial and ethnic group differences in sleep-memory associations.
-
2)
More research is needed on racial and ethnic differences in sleep-memory associations in children. Black children, who showed high actigraphy-measured sleep efficiency at 9 years of age, also showed high working memory performance at age 11 [53]. No sleep measures were associated with working memory performance in White children. Sleep research in children from minoritized racial and ethnic groups is particularly lacking, but this study suggests that racial and ethnic differences in sleep-memory associations may emerge during childhood.
-
3)
Although subjective reports of sleep duration and quality are easier to collect than objective measurements, especially in the large sample studies needed to investigate individual differences, subjective reports show modest agreement with objectively measured sleep. People often overestimate their sleep quantity and underestimate sleep disruptions (e.g., awakenings) [54,55,56]. These correlations may be different in minoritized racial and ethnic groups. For example, Black adults underestimate their sleep duration as compared to actigraphy-measured sleep [57]. Moreover, the inclusion of actigraphy-measured sleep allows for a more comprehensive assessment of sleep health, including night-to-night sleep regularity, sleep efficiency, and timing, which have also shown racial and ethnic differences [58, 59]. Thus, it is important for future studies to include objective measures of sleep, such as actigraphy, for more accurate and complete racial and ethnic group comparisons of sleep-memory associations. Multi-site studies may be one mechanism by which researchers can obtain objective sleep measures in large and racially and ethnically diverse participant samples.
-
4)
Most of the current studies are cross-sectional. Longitudinal studies are needed to understand the directionality of the relationships between stress and sleep, and sleep and memory. Longitudinal studies will also be essential for understanding the impact of age on these temporal dynamics. A better understanding of directionality will help inform future interventions aiming to improve sleep, and possibly, memory functioning in adults across the lifespan.
Conclusion
People from minoritized racial and ethnic groups may show stronger associations between poorer sleep and poorer memory performance than White adults. However, evidence of racial and ethnic differences in sleep-memory associations is only recently emerging and largely based in Black adults. More experimental and epidemiology studies are needed to better understand the causes of poor sleep and their consequences on memory outcomes in racially and ethnically diverse people.
Change history
09 July 2024
A Correction to this paper has been published: https://doi.org/10.1007/s40675-024-00312-w
References
Rasch B, Born J. About sleep’s role in memory. Physiol Rev. 2013;93:681–766. https://doi.org/10.1152/physrev.00032.2012.
Mander BA, Winer JR, Walker MP. Sleep and human aging. Neuron. 2017;94:19–36. https://doi.org/10.1016/j.neuron.2017.02.004.
Born J, Wilhelm I. System consolidation of memory during sleep. Psychol Res. 2012;76:192–203. https://doi.org/10.1007/s00426-011-0335-6.
Hokett E, Arunmozhi A, Campbell J, Verhaeghen P, Duarte A. A systematic review and meta-analysis of individual differences in naturalistic sleep quality and episodic memory performance in young and older adults. Neurosci Biobehav Rev. 2021;127:675–88. https://doi.org/10.1016/j.neubiorev.2021.05.010.
Johnson DA, Lisabeth L, Hickson D, Johnson-Lawrence V, Samdarshi T, Taylor H, et al. The social patterning of sleep in African Americans: associations of socioeconomic position and neighborhood characteristics with sleep in the Jackson Heart Study. Sleep. 2016;39:1749–59. https://doi.org/10.5665/sleep.6106.
Mehta KM, Yeo GW. Systematic review of dementia prevalence and incidence in United States race/ethnic populations. Alzheimers Dement. 2017;13:72–83. https://doi.org/10.1016/j.jalz.2016.06.2360.
Manly JJ, Jones RN, Langa KM, Ryan LH, Levine DA, McCammon R, et al. Estimating the prevalence of dementia and mild cognitive impairment in the US: The 2016 Health and Retirement Study Harmonized Cognitive Assessment Protocol Project. JAMA Neurol. 2022. https://doi.org/10.1001/jamaneurol.2022.3543.
Sol K, Zaheed AB, Kraal AZ, Sharifian N, Arce Rentería M, Zahodne LB. Psychological predictors of memory decline in a racially and ethnically diverse longitudinal sample of older adults in the United States. Int J Geriatr Psychiatry. 2020;35:204–12. https://doi.org/10.1002/gps.5236.
Dubowitz T, Haas A, Ghosh-Dastidar B, Collins RL, Beckman R, Brooks Holliday S, et al. Does investing in low-income urban neighborhoods improve sleep? Sleep. 2021;44:1–8. https://doi.org/10.1093/sleep/zsaa292.
Troxel WM, DeSantis A, Richardson AS, Beckman R, Ghosh-Dastidar B, Nugroho A, et al. Neighborhood disadvantage is associated with actigraphy-assessed sleep continuity and short sleep duration. Sleep. 2018;41. https://doi.org/10.1093/sleep/zsy140.
Johnson DA, Lisabeth L, Lewis TT, Sims M, Hickson DA, Samdarshi T, et al. The contribution of psychosocial stressors to sleep among African Americans in the Jackson Heart Study. Sleep. 2016;39:1411–9. https://doi.org/10.5665/sleep.5974.
Slopen N, Lewis TT, Williams DR. Discrimination and sleep: a systematic review. Sleep Med. 2016;18:88–95. https://doi.org/10.1016/j.sleep.2015.01.012.
McKinnon II, Johnson DA, Murden RJ, Erving CL, Parker R, Van Dyke ME, et al. Extreme racism-related events and poor sleep in African-American women. Soc Sci Med. 2022;310:115269. https://doi.org/10.1016/j.socscimed.2022.115269.
Erving CL, Zajdel R, McKinnon II, Van Dyke ME, Murden RJ, Johnson DA, et al. Gendered racial microaggressions and Black women’s sleep health. Soc Psychol Q. 2023;01902725221136139. https://doi.org/10.1177/01902725221136139.
Ramos AR, Tarraf W, Wu B, Redline S, Cai J, Daviglus ML, et al. Sleep and neurocognitive decline in the Hispanic Community Health Study/Study of Latinos. Alzheimers Dement J Alzheimers Assoc. 2020;16:305–15. https://doi.org/10.1016/j.jalz.2019.08.191.
Xu L, Jiang CQ, Lam TH, Zhang WS, Cherny SS, Thomas GN, et al. Sleep duration and memory in the elderly Chinese: longitudinal analysis of the Guangzhou Biobank Cohort Study. Sleep. 2014;37:1737–44. https://doi.org/10.5665/sleep.4162.
Flanagin A, Frey T, Christiansen SL, AMA Manual of Style Committee. Updated Guidance on the Reporting of Race and Ethnicity in Medical and Science Journals. JAMA. 2021;326:621–7. https://doi.org/10.1001/jama.2021.13304.
Race and National Origin. Natl Inst Health NIH 2022. https://www.nih.gov/nih-style-guide/race-national-origin. (Accessed March 1, 2023).
Scullin MK, Bliwise DL. Sleep, Cognition, and normal aging: integrating a half century of multidisciplinary research. Perspect Psychol Sci. 2015;10:97–137. https://doi.org/10.1177/1745691614556680.
Diekelmann S, Born J. The memory function of sleep. Nat Rev Neurosci. 2010;11:114–26. https://doi.org/10.1038/nrn2762.
Cavuoto MG, Ong B, Pike KE, Nicholas CL, Bei B, Kinsella GJ. Objective but not subjective sleep predicts memory in community-dwelling older adults. J Sleep Res. 2016;25:475–85. https://doi.org/10.1111/jsr.12391.
Hokett E, Duarte A. Age and race-related differences in sleep discontinuity linked to associative memory performance and its neural underpinnings. Front Hum Neurosci. 2019;13:176. https://doi.org/10.3389/fnhum.2019.00176.
Hokett E, Mirjalili S, Duarte A. Greater sleep variance related to decrements in memory performance and event-specific neural similarity: a racially/ethnically diverse lifespan sample. Neurobiol Aging. 2022;117:33–43. https://doi.org/10.1016/j.neurobiolaging.2022.04.015.
Owusu JT, Rabinowitz JA, Tzuang M, An Y, Kitner-Triolo M, Zipunnikov V, et al. Associations between objectively measured sleep and cognition: main effects and interactions with race in adults aged ≥50 years. J Gerontol A Biol Sci Med Sci. 2022;glac180. https://doi.org/10.1093/gerona/glac180.
Swanson LM, Hood MM, Hall MH, Kravitz HM, Matthews KA, Joffe H, et al. Associations between sleep and cognitive performance in a racially/ethnically diverse cohort: the Study of Women’s Health Across the Nation. Sleep. 2021;44:zsaa182. https://doi.org/10.1093/sleep/zsaa182.
Chattu VK, Manzar MD, Kumary S, Burman D, Spence DW, Pandi-Perumal SR. The global problem of insufficient sleep and its serious public health implications. Healthcare. 2019;7:1. https://doi.org/10.3390/healthcare7010001.
Sonnega J, Sonnega A, Kruger D. The city doesn’t sleep: community perceptions of sleep deficits and disparities. Int J Environ Res Public Health. 2019;16:3976. https://doi.org/10.3390/ijerph16203976.
Troxel WM, Haas A, Dubowitz T, Ghosh-Dastidar B, Butters MA, Gary-Webb TL, et al. Sleep disturbances, changes in sleep, and cognitive function in low-income African Americans. J Alzheimers Dis JAD. 2022;87:1591–601. https://doi.org/10.3233/JAD-215530.
Ramos AR, Tarraf W, Daviglus M, Davis S, Gallo LC, Mossavar-Rahmani Y, et al. Sleep duration and neurocognitive function in the Hispanic community health study/study of Latinos. Sleep. 2016;39:1843–51. https://doi.org/10.5665/sleep.6166.
Kaur SS, Tarraf W, Wu B, Gonzalez KA, Daviglus M, Shah N, et al. Modifying pathways by age and sex for the association between combined sleep disordered breathing and long sleep duration with neurocognitive decline in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Alzheimers Dement J Alzheimers Assoc. 2021;17:1950–65. https://doi.org/10.1002/alz.12361.
Johnson DA, Jackson CL, Williams NJ, Alcántara C. Are sleep patterns influenced by race/ethnicity – a marker of relative advantage or disadvantage? Evidence to date. Nat Sci Sleep. 2019;11:79–95. https://doi.org/10.2147/NSS.S169312.
Li J, Chang Y-P, Riegel B, Keenan BT, Varrasse M, Pack AI, et al. Intermediate, but not extended, afternoon naps may preserve cognition in Chinese older adults. J Gerontol A Biol Sci Med Sci. 2018;73:360–6. https://doi.org/10.1093/gerona/glx069.
Sha T, Cheng W, Yan Y. Prospective association between sleep-related factors and the trajectories of cognitive performance in the elderly Chinese population across a 5-year period cohort study. PLoS ONE. 2019;14:e0222192. https://doi.org/10.1371/journal.pone.0222192.
Lo Martire V, Caruso D, Palagini L, Zoccoli G, Bastianini S. Stress & sleep: a relationship lasting a lifetime. Neurosci Biobehav Rev. 2020;117:65–77. https://doi.org/10.1016/j.neubiorev.2019.08.024.
McEwen BS, Karatsoreos IN. Sleep deprivation and circadian disruption: stress, allostasis, and allostatic load. Sleep Med Clin. 2015;10:1–10. https://doi.org/10.1016/j.jsmc.2014.11.007.
Peltz JS, Bodenlos JS, Kingery JN, Rogge RD. The role of financial strain in college students’ work hours, sleep, and mental health. J Am Coll Health J ACH. 2021;69:577–84. https://doi.org/10.1080/07448481.2019.1705306.
Hall M, Buysse DJ, Nofzinger EA, Reynolds CF, Thompson W, Mazumdar S, et al. Financial strain is a significant correlate of sleep continuity disturbances in late-life. Biol Psychol. 2008;77:217–22. https://doi.org/10.1016/j.biopsycho.2007.10.012.
Otto MW, Lubin RE, Rosenfield D, Taylor DJ, Birk JL, Espie CA, et al. The association between race- and ethnicity-related stressors and sleep: the role of rumination and anxiety sensitivity. Sleep. 2022;45:zsac117. https://doi.org/10.1093/sleep/zsac117.
Fitzgerald HE, Hoyt DL, Kredlow MA, Smits JAJ, Schmidt NB, Edmondson D, et al. Anxiety sensitivity as a malleable mechanistic target for prevention interventions: a meta-analysis of the efficacy of brief treatment interventions. Clin Psychol Sci Pract. 2021;28:323–37. https://doi.org/10.1037/cps0000038.
Watkins ER, Roberts H. Reflecting on rumination: consequences, causes, mechanisms and treatment of rumination. Behav Res Ther. 2020;127:103573. https://doi.org/10.1016/j.brat.2020.103573.
Aqua JK, White K, Johnson DA. A systematic review of acculturation and sleep health among adult immigrants in the United States. Sleep Health. 2023. https://doi.org/10.1016/j.sleh.2023.01.007.
Lee S, Ryu S, Lee GE, Kawachi I, Morey BN, Slopen N. The association of acculturative stress with self-reported sleep disturbance and sleep duration among Asian Americans. Sleep. 2022;45:zsab298. https://doi.org/10.1093/sleep/zsab298.
Yip T, Wang Y, Mootoo C, Mirpuri S. Moderating the association between discrimination and adjustment: a meta-analysis of ethnic/racial identity. Dev Psychol. 2019;55:1274–98. https://doi.org/10.1037/dev0000708.
McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87:873–904. https://doi.org/10.1152/physrev.00041.2006.
Quaedflieg CWEM, Schwabe L. Memory dynamics under stress. Mem Hove Engl. 2018;26:364–76. https://doi.org/10.1080/09658211.2017.1338299.
Alcántara C, Giorgio Cosenzo L, McCullough E, Vogt T, Falzon AL, Perez II. Cultural adaptations of psychological interventions for prevalent sleep disorders and sleep disturbances: a systematic review of randomized controlled trials in the United States. Sleep Med Rev. 2021;56:101455. https://doi.org/10.1016/j.smrv.2021.101455.
Johnson LCM, Aiello JJ, Jagtiani A, Moore KN, Barber L, Gujral UP, et al. Feasibility, appropriateness, and acceptability of a mobile mindfulness meditation intervention to improve sleep quality among a racially/ethnically diverse population. Sleep Health. 2022. https://doi.org/10.1016/j.sleh.2022.09.014.
Tavernier R, Adam EK. Text message intervention improves objective sleep hours among adolescents: the moderating role of race-ethnicity. Sleep Health. 2017;3:62–7. https://doi.org/10.1016/j.sleh.2016.11.002.
Jean-Louis G, Newsome V, Williams NJ, Zizi F, Ravenell J, Ogedegbe G. Tailored behavioral intervention among Blacks with metabolic syndrome and sleep apnea: results of the MetSO Trial. Sleep. 2017;40:zsw008. https://doi.org/10.1093/sleep/zsw008.
Nam S, Whittemore R, Jung S, Latkin C, Kershaw T, Redeker NS. Physical neighborhood and social environment, beliefs about sleep, sleep hygiene behaviors, and sleep quality among African Americans. Sleep Health. 2018;4:258–64. https://doi.org/10.1016/j.sleh.2018.03.002.
Johnson DA, Brown DL, Morgenstern LB, Meurer WJ, Lisabeth LD. The association of neighborhood characteristics with sleep duration and daytime sleepiness. Sleep Health. 2015;1:148–55. https://doi.org/10.1016/j.sleh.2015.06.002.
Seixas AA, Moore J, Chung A, Robbins R, Grandner M, Rogers A, et al. Benefits of community-based approaches in assessing and addressing sleep health and sleep-related cardiovascular disease risk: a precision and personalized population health approach. Curr Hypertens Rep. 2020;22:52. https://doi.org/10.1007/s11906-020-01051-3.
Philbrook LE, Hinnant JB, Elmore-Staton L, Buckhalt JA, El-Sheikh M. Sleep and cognitive functioning in childhood: ethnicity, socioeconomic status, and sex as moderators. Dev Psychol. 2017;53:1276–85. https://doi.org/10.1037/dev0000319.
Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19:838–45.
King E, Daunis M, Tami C, Scullin MK. Sleep in studio based courses: outcomes for creativity task performance. J Inter Des. 2017;42:5–27. https://doi.org/10.1111/joid.12104.
Matthews KA, Patel SR, Pantesco EJ, Buysse DJ, Kamarck TW, Lee L, et al. Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health. 2018;4:96–103. https://doi.org/10.1016/j.sleh.2017.10.011.
Jackson CL, Ward JB, Johnson DA, Sims M, Wilson J, Redline S. Concordance between self-reported and actigraphy-assessed sleep duration among African-American adults: findings from the Jackson Heart Sleep Study. Sleep. 2020;43:1–11. https://doi.org/10.1093/sleep/zsz246.
Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37:9–17. https://doi.org/10.5665/sleep.3298.
Chung J, Goodman M, Huang T, Bertisch S, Redline S. Multidimensional sleep health in a diverse, aging adult cohort: concepts, advances, and implications for research and intervention. Sleep Health. 2021;S2352721821001716. https://doi.org/10.1016/j.sleh.2021.08.005.
Acknowledgements
The authors are thankful for their participants. This research was supported by the Ruth L. Kirschstein National Research Service Award Institutional Research Training Grant from the National Institutes of Health (National Institute on Aging; 5T32AG0 0 0175 ) and the National Science Foundation Grant # 1850802 awarded to Audrey Duarte.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The article “A Review of Racial and Ethnic Differences in Sleep‑memory Associations and the Potential Contributions of Social Determinants of Sleep”, written by Emily Hokett and Audrey Duarte, was originally published Online First without Open Access. After publication in volume 10, issue 1, page 62-69 the author decided to opt for Open Choice and to make the article an Open Access publication. Therefore, the copyright of the article has been changed to © The Author(s) 2024 and the article is forthwith distributed under the terms of the Creative Commons Attribution
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hokett, E., Duarte, A. A Review of Racial and Ethnic Differences in Sleep-memory Associations and the Potential Contributions of Social Determinants of Sleep. Curr Sleep Medicine Rep 10, 62–69 (2024). https://doi.org/10.1007/s40675-024-00281-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40675-024-00281-0