Abstract
Background
Simulations aim to supplement historic teacher-centric methods by facilitating experiential, self-guided learning and the application of students’ knowledge in a controlled environment. The objective of our study is to describe the methodology of developing and facilitating simulations, and to assess their effectiveness as an educational tool for global health training.
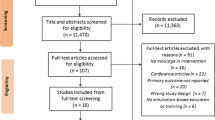
Methods
We describe the methodology used by Global Health Sim between October 2016 and March 2019 to design and facilitate simulations for participants at the high school through graduate school levels, and at conferences and online. Using a mixed-methods evaluation design, we assessed self-reported quantitative measures of content knowledge before and after participating in the simulation and different aspects of the simulation experience. We also conducted a qualitative thematic analysis of the experience and lessons learned as reported by evaluation respondents.
Results
We conducted a total of 20 simulations on six unique topics for 213 evaluation respondents. Self-reported knowledge of the topic increased an average of 3.3 points on a 10-point scale (4.1–7.4) and the seven aspects of the experience were rated highly (3–5 points on a 5-point Likert scale). Thematic analysis revealed an increased understanding of the complexity of global health problems and strategies for effectively responding to issues in a multidisciplinary manner.
Conclusions
Respondents valued the opportunity to learn about the complexities of responding to global health events, which confirmed that simulations can be utilized as teaching tools for students and professionals. Further research is required to assess the long-term educational impact of simulations in global health.



Similar content being viewed by others
References
McLaughlin JE, Roth MT, Glatt DM, Gharkholonarehe N, Davidson CA, Griffin LM, et al. The flipped classroom: a course redesign to foster learning and engagement in a health professions school. Acad Med. 2014;89(2):236–43.
Bishop JL, Verleger MA, editors. The flipped classroom: a survey of the research. American Society for Engineering Education. 2013.
Gilboy MB, Heinerichs S, Pazzaglia G. Enhancing student engagement using the flipped classroom. J Nutr Educ Behav. 2015;47(1):109–14.
Herreid CF, Schiller NA. Case studies and the flipped classroom. J Coll Sci Teach. 2013;42(5):62–6.
Tucker B. The flipped classroom. Educ Next. 2012;12(1):82–3.
Heale J, Davis D, Norman G, Woodward C, Neufeld V, Dodd P. A randomized controlled trial assessing the impact of problem-based versus didactic teaching methods in CME. Res Med Educ. 1988;27:72–7.
Srinivasan M, Wilkes M, Stevenson F, Nguyen T, Slavin S. Comparing problem-based learning with case-based learning: effects of a major curricular shift at two institutions. Acad Med. 2007;82(1):74–82.
Bergmann J, Sams A. Flip your classroom: reach every student in every class every day. International Society for Technology In Education. 2012.
Hsieh J-L, Sun C-T, Kao GY-M, Huang C-Y. Teaching through simulation: epidemic dynamics and public health policies. Simulation. 2006;82(11):731–59.
Miller JL, Rambeck JH, Snyder A. Improving emergency preparedness system readiness through simulation and interprofessional education. Public Health Rep. 2014;129(Suppl4):129–35.
Spinello EF, Fischbach R. Using a web-based simulation as a problem-based learning experience: perceived and actual performance of undergraduate public health students. Public Health Rep. 2008;123(Suppl2):78–84.
Foronda C, Liu S, Bauman EB. Evaluation of simulation in undergraduate nurse education: an integrative review. Clin Simul Nurs. 2013;9(10):e409–e16.
Rauen CA. Using simulation to teach critical thinking skills: you can’t just throw the book at them. Crit Care Nurs Clin North Am. 2001;13(1):93–103.
Waag WL, Bell HH. Estimating the training effectiveness of interactive air combat simulation. United States Air Force Armstrong Laboratory. 1997. https://apps.dtic.mil/dtic/tr/fulltext/u2/a459625.pdf. Accessed 2 May 2020.
Fitchett JR, Reidy PG, Anderson EJ, Forte S, Chiu K. The WHO simulation initiative: improving global health partnerships. Philos Ethics Humanit Med. 4Y;8(6).
Cohen D, Vlaev I, McMahon L, Harvey S, Mitchell A, Borovoi L, et al. The Crucible simulation: behavioral simulation improves clinical leadership skills and understanding of complex health policy change. Health Care Manag Rev. 2019;44(3):246–55.
Araz OM, Jehn M, Lant T, Fowler JW. A new method of exercising pandemic preparedness through an interactive simulation and visualization. J Med Syst. 2012;36(3):1475–83.
Carney JK, Schilling LM, Frank SH, Biddinger PD, Bertsch TF, Grace CJ, et al. Planning and incorporating public health preparedness into the medical curriculum. Am J Prev Med. 2011;41(4):S193–S9.
Mylopoulos M, Kulasegaram K, Woods NN. Developing the experts we need: fostering adaptive expertise through education. J Eval Clin Pract. 2018;24(3):674–7.
Doran GT. “There’s a SMART way to write management’s goals and objectives.” and Miller. Arthur F & Cunningham, James A “How to avoid costly job mismatches” Management Review. 1981;70(11).
Global Health Sim - Innovation education by simulation: Global Health Sim Inc. 2019. http://www.ghsim.com/. Accessed 2 May 2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
We collected anonymous, optional, written evaluations as part of a quality improvement exercise for educational content development. As such, research ethics board approval was not required.
Informed Consent
Participants included in the paper voluntarily completed the evaluations after participating in simulations.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Loutet, M.G., Zhang, J., Varsaneux, O. et al. Using Experiential Simulation-Based Learning to Increase Engagement in Global Health Education: an Evaluation of Self-reported Participant Experience. Med.Sci.Educ. 30, 1245–1253 (2020). https://doi.org/10.1007/s40670-020-00999-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-020-00999-w