Abstract
Background
Residents in training have high rates of depression and are reluctant to seek treatment. The goal of the study was to conduct a survey with a high response rate to better understand resident attitudes about mental health.
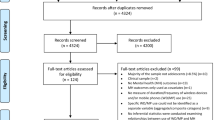
Methods
A multi-site study of residents from three teaching hospitals in the USA completed a 21-item anonymous questionnaire, on their smartphones, during mandatory lecture sessions.
Results
Three-hundred and sixteen resident surveys were completed during 24 didactic sessions. The overall response rate from resident-only presentations was 87.8% and ranged from 76.9% to 100% in presentations that included both residents and other attendees. A significant majority of residents indicated that physicians who seek treatment for medical conditions would not seek treatment for depression (87.7%), physicians do not see acceptance of mental health treatment as a sign of strength (80.1%), and most residents with depression cope with it alone (69.0%). Factors that would encourage residents to seek treatment, including easy access to mental healthcare and acceptance of treatment in the workplace environment, varied significantly when residents were grouped by age and gender.
Conclusions
While residents believe that physicians are highly resistant to mental health treatment, targeted strategies may increase the acceptance of treatment. Administration of surveys to physicians on smartphones at the time of lecture or presentation may improve the response rate.
Similar content being viewed by others
Change history
28 August 2019
The original version of this article was updated to correct the in-text citations to Tables 1 and 2.
References
Schernhammer E. Taking their own lives - the high rate of physician suicide. N Engl J Med. 2005;352(24):2473–6. https://doi.org/10.1056/NEJMp058014.
Brazeau C, Shanafelt T, Durning SJ, Massie FS, Eacker A, Moutier C, et al. Distress among matriculating medical students relative to the general population. Acad Med. 2014;89(11):1520–5. https://doi.org/10.1097/ACM.0000000000000482.
Dyrbye L, West C, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89(3):443–51. https://doi.org/10.1097/ACM.0000000000000134.
Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316(21):2214–36. https://doi.org/10.1001/jama.2016.17324.
Sen S, Kranzler HR, Krystal JH, Speller H, Chan G, Gelernter J, et al. A prospective cohort study investigating factors associated with depression during medical internship. Arch Gen Psychiatry. 2010;67(6):557–65. https://doi.org/10.1001/archgenpsychiatry.2010.41.
Shanafelt TD, Balch CM, Dyrbye L, Bechamps G, Russell T, Satele D, et al. Special report: suicidal ideation among american surgeons. Arch Surg. 2011;146(1):54–62. https://doi.org/10.1001/archsurg.2010.292.
Guille C, Speller H, Laff R, Epperson N, Sen S. Utilization and barriers to mental health services among depressed medical interns: a prospective multisite study. JGME. 2010;2(2):210–4. https://doi.org/10.4300/JGME-D-09-00086.1.
Center C, Davis M, Detre T, Ford DE, Hansbrough W, Hendin H, et al. Confronting depression and suicide in physicians: a consensus statement. JAMA. 2003;289(23):3161–6. https://doi.org/10.1001/jama.289.23.3161.
Ey S, Moffit M, Kinzie JM, Brunett P. Feasibility of a comprehensive wellness and suicide prevention program: a decade of caring for physicians in training and practice. JGME. 2016;8(5):747–53. https://doi.org/10.4300/JGME-D-16-00034.1.
Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015;314(22):2373–83. https://doi.org/10.1001/jama.2015.15845.
Ey S, Moffit M, Kinzie JM, Dongseok C, Girard DE. If you build it they will come: attitudes of medical residents and fellows about seeking services in a resident wellness program. JGME. 2013;5(3):486–92. https://doi.org/10.4300/JGME-D-12-00048.1.
Kellerman SE, Herold J. Physician response to surveys: a review of the literature. Am J Prev Med. 2001;20(1):61–7. https://doi.org/10.1016/S0749-3797(00)00258-0.
Common program requirements section VI with background and intent. Accreditation Council for Graduate Medical Education (ACGME). 2017;VI.C.:9–11.
Gagne P, Moamai J, Bourget D. Psychopathology and suicide among Quebec physicians: a nested case control study. Depress Res Treat. 2011;2011:1–6. https://doi.org/10.1155/2011/936327.
Steinert Y, Magonet G, Rubin G, Carson K. Emotional well-being of house staff. Can Fam Physician. 1991;37:2130–8.
Gross C, Mead L, Ford D, Klag M. Physician, heal thyself? Regular source of care and use of preventive health services among physicians. Archi Intern Med. 2000;160(21):3209–14. https://doi.org/10.1001/archinte.160.21.3209.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study was approved by the IRB of all the three hospitals where data was collected.
Informed Consent
The IRBs exempted the study from Informed Consent because the data collected from medical residents was de-identified.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Roane, D.M., Botticelli, L.M., Macy, M.A. et al. Resident Attitudes About Mental Health: a Real-Time Smart Phone Survey. Med.Sci.Educ. 29, 825–830 (2019). https://doi.org/10.1007/s40670-019-00745-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-019-00745-x