Abstract
Introduction
Evidence-based medicine (EBM) has become the quintessential goal of clinical decision-making. The study objective is to determine if a novel interactive EBM curriculum will improve resident physician EBM comprehension, assessed via a common EBM evaluation instrument, the Berlin Questionnaire (BQ).
Methods
The BQ was administered to all residents at the start of the academic year and again following completion of the 12-month study period and EBM curriculum. The curriculum was designed based on readings from the JAMA Users’ Guides to the Medical Literature coupled with real-world, specialty-specific articles that reflect the major topic of each chapter of the text and was utilized to supplement the Emergency Medicine (EM) residency’s monthly “journal club.” Descriptive statistics, examination of self-evaluation, and analysis of test results were evaluated.
Results
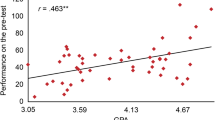
Fifty-four EM residents completed the course. Wilcoxon signed-rank testing revealed a significant difference between pre- and post-intervention scores: [Z = − 3.114, p = 0.002], [Z = −3.327, p = 0.001] for post-graduate year (PGY)1 and PGY2, respectively. PGY3 had a borderline significant difference pre to post with [Z = − 1.693, p = 0.05], and PGY4 had a non-significant difference with [Z = − 1.769, 0.77]. Kruskal-Wallis H testing confirmed a significant difference between PGY pre-intervention scores with χ2(3) = 13.957, p = 0.003. A pairwise comparison of PGYs demonstrated a significant difference between the pre-intervention scores of PGY4s compared to PGY1s (p = 0.006) and PGY2s (p = 0.015). There was no significant difference between other PGYs. Kruskal-Wallis H testing comparing post-intervention scores demonstrated no significant difference between PGYs with χ2(3) = 0.575, p = 0.902.
Conclusions
The post-intervention difference in PGY1, PGY2, and PGY3 BQ scores suggests improved knowledge after new EBM curriculum. Significant difference between pre-intervention scores of PGY1 or PGY2 when compared to PGY4 suggests that capacity to learn EBM is dependent on the training year. A clustering of high scores among all years post-intervention suggests that the EBM course improved PGY1 and PGY2 to PGY4 level over the course of 12 months.
Similar content being viewed by others
References
Guyatt G, Cairns J, Churchill D, et al. Evidence-based medicine. A new approach to teaching the practice of medicine. JAMA. 1992;268(17):2420–5.
Fritsche L, Greenhalgh T, Falck-Ytter Y, Neumayer HH, Kunz R. Do short courses in evidence based medicine improve knowledge and skills? Validation of Berlin questionnaire and before and after study of courses in evidence based medicine. BMJ. 2002;325(7376):1338–41.
Green ML. Evidence-based medicine training in graduate medical education: past, present and future. J Eval Clin Pract. 2000;6(2):121–38.
Haynes RB, Devereaux PJ, Guyatt GH. Physicians’ and patients’ choices in evidence based practice. BMJ. 2002;324(7350):1350.
Khan KS, Awonuga AO, Dwarakanath LS, Taylor R. Assessments in evidence-based medicine workshops: loose connection between perception of knowledge and its objective assessment. Med Teach. 2001;23(1):92–4.
Shaneyfelt T, Baum KD, Bell D, Feldstein D, Houston TK, Kaatz S, et al. Instruments for evaluating education in evidence-based practice: a systematic review. JAMA. 2006;296(9):1116–27.
Kunz R, Wegscheider K, Fritsche L, et al. Determinants of knowledge gain in evidence-based medicine short courses: an international assessment. Open Med. 2010;4(1):e3–e10.
Ramos KD, Schafer S, Tracz SM. Validation of the Fresno test of competence in evidence based medicine. BMJ. 2003;326(7384):319–21.
Ilic D. Assessing competency in evidence based practice: strengths and limitations of current tools in practice. BMC Med Educ. 2009;9:53.
Gagliardi JP, Stinnett SS, Schardt C. Innovation in evidence-based medicine education and assessment: an interactive class for third- and fourth-year medical students. J Med Libr Assoc. 2012;100(4):306–9.
Keddis MT, Beckman TJ, Cullen MW, Reed DA, Halvorsen AJ, Wittich CM, et al. Senior internal medicine residents’ confidence with essential topics in evidence-based medicine taught during internship. J Grad Med Educ. 2011;3(4):490–6.
Accreditation Council for Graduate Medical Education Common Program Requirements. 2011; http://www.acgme.org/acgmeweb/Portals/0/dh_dutyhoursCommonPR07012007.pdf. Accessed November 15, 2013.
Davidson RA, Duerson M, Romrell L, Pauly R, Watson RT. Evaluating evidence-based medicine skills during a performance-based examination. Acad Med. 2004;79(3):272–5.
Gruppen LD, Rana GK, Arndt TS. A controlled comparison study of the efficacy of training medical students in evidence-based medicine literature searching skills. Acad Med. 2005;80(10):940–4.
Kasuya RT, Sakai DH. An evidence-based medicine seminar series. Acad Med. May 1996;71(5):548–9.
Harewood GC, Hendrick LM. Prospective, controlled assessment of the impact of formal evidence-based medicine teaching workshop on ability to appraise the medical literature. Ir J Med Sci. 2010;179(1):91–4.
Green ML, Ellis PJ. Impact of an evidence-based medicine curriculum based on adult learning theory. J Gen Intern Med. 1997;12(12):742–50.
Smith CA, Ganschow PS, Reilly BM, Evans AT, McNutt RA, Osei A, et al. Teaching residents evidence-based medicine skills: a controlled trial of effectiveness and assessment of durability. J Gen Intern Med. 2000;15(10):710–5.
McGinn T, Seltz M, Korenstein D. A method for real-time, evidence-based general medical attending rounds. Acad Med. 2002;77(11):1150–2.
Korenstein D, Dunn A, McGinn T. Mixing it up: integrating evidence-based medicine and patient care. Acad Med. 2002;77(7):741–2.
Welch HG, Lurie JD. Teaching evidence-based medicine: caveats and challenges. Acad Med. 2000;75(3):235–40.
Guyatt G, Rennie D, Evidence-Based Medicine Working Group., American Medical Association. Users' guides to the medical literature : a manual for evidence-based clinical practice. Chicago: AMA Press; 2002.
Beeson MS, Carter WA, Christopher TA, Heidt JW, Jones JH, Meyer LE, et al. Emergency medicine milestones. J Grad Med Educ. 2013;5(1 Suppl 1):5–13.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Bentley, S., Slovis, B.H. & Shah, K. Introduction of a Novel Evidence-Based Medicine Curriculum in Emergency Medicine. Med.Sci.Educ. 28, 497–501 (2018). https://doi.org/10.1007/s40670-018-0575-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-018-0575-9