Abstract
Purpose
Patient hand-over is a critical skill to develop in the era of reduced duty hours. There is insufficient data in the literature that medical students, especially in the third year, are being instructed to participate in a patient hand-over. Early introduction into the curriculum should provide earlier competency which has the potential to decrease the number of medical errors related to communication.
Methods
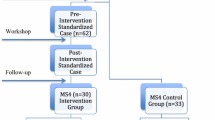
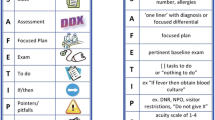
All students were expected to use our institution’s hand-over mnemonic SAFETIPS when signing out on inpatient wards. Students were randomly assigned to a curriculum or control group and completed patient hand-over student confidence pre-surveys. The curriculum group participated in a faculty-led workshop at the beginning of the clerkship teaching hand-overs. Faculty members assessed student hand-overs at the end of clerkship, followed by a student post-survey.
Results
The statistically significant difference (P = .001) in median inventory scores (alpha = .70) for students in the curriculum (13.0(±2.0)) vs. control (12.0(±5.0)) is coupled to an effect size (Cliff’s d = 0.34). Five SAFETIPS items reported significant increases (p ≤ .050) for students in the curriculum vs. control. Significant increases in pre-/post-survey (alpha = .84/.87) scores are reported for students in the curriculum (pre/post difference = 9.0, P = .001) and in the control group (difference = 7.3, P = .001) for the survey. The largest individual item increases for both groups were “using SAFETIPS to give/listen to hand-over of patients” (difference = 2.0, P = .001).
Conclusions
Third-year medical student skill and confidence level giving patient hand-over using SAFETIPS is improved with the use of a formal curriculum.
Similar content being viewed by others
References
Accreditation Council for Graduate Medical Education. Report of the work group on resident duty hours. http://www.ttuhsc.edu/sop/residencies/documents/ACGME_work_hour_policy.pdf. Accessed December 10, 2014.
Steinbrook R. The debate over residents’ work hours. N Engl J Med. 2002;347:1296–302.
Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, et al. Effect of reducing interns’ work hours on serious medical errors in intensive care units. N Engl J Med. 2004;351:1838–48.
Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP, Rothschild JM, Katz JT, Lilly CM, Stone PH, Aeschbach D, Czeisler CA. Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351:1829–37.
Philibert I, Friedmann P, Williams WT. New requirements for resident duty hours. JAMA. 2002;288:1112–4.
Horwitz LI, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between house staff on internal medicine wards: a national survey. Arch Intern Med. 2006;166:1173–7.
Vidyarthi AR, Arora V, Schnipper JL, Wall SD, Wachter RM. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1:257–66.
Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH. What are covering doctors told about their patients? Analysis of sign-out among internal medicine house staff. Qual Saf Health Care. 2009;18:248–55.
Van Eaton EG, Tarpley JL, Solorzano CC, Cho CS, Weber SM, Termuhlen PM. Resident education in 2011: three key challenges on the road ahead. Surgery. 2011;149:465–73.
Petersen LA, Brennan TA, O’Neil AC, Cook EF, Lee TH. Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med. 1994;121:866–72.
Mukherjee S. A precarious exchange. N Engl J Med. 2004;351:1822–4.
Agency for Healthcare Research and Quality. Patient safety primers: handoffs and signouts. http://www.psnet.ahrq.gov/primer.aspx?primerID=9. Accessed February 10, 2015.
Accreditation Council for Graduate Medical Education. Common program requirements. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/CPRs2013.pdf. Accessed December 10, 2014.
Gakhar B, Spencer AL. Using direct observation, formal evaluation, and an interactive curriculum to improve the sign-out practices of internal medicine interns. Acad Med. 2010;85:1182–8.
DeRienzo CM, Frush K, Barfield ME, Gopwani PR, Griffith BC, Jiang X, et al. Handoffs in the era of duty hours reform: a focused review and strategy to address changes in the accreditation council for graduate medical education common program requirements. Acad Med. 2012;87:403–10.
Gordon M. Training on handover of patient care within UK medical schools. Med educ online. 2013;18:1–5.
Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med. 2005;80:1094–9.
Farnan JM, Paro JA, Rodriguez RM, Reddy ST, Horwitz LI, Johnson JK, et al. Hand-off education and evaluation: piloting the observed simulated hand-off experience (OSHE). J Gen Intern Med. 2010;25:129–34.
Chu ES, Reid M, Burden M, Mancini D, Schulz T, Keniston A, et al. Effectiveness of a course designed to teach handoffs to medical students. J Hosp Med. 2010;5:344–8.
Darbyshire D, Gordon M, Baker P. Teaching handover of care to medical students. Clin Teach. 2013;10:32–7.
Arora VM, Johnson JK, Meltzer DO, Humphrey HJ. A theoretical framework and competency-based approach to improving handoffs. Qual Saf Health Care. 2008;17(1):11–4.
Humphris GM, Kaney S. Assessing the development of communication skills in undergraduate medical students. Med Educ. 2001;35:225–31.
Gordon M, Findley R. Educational interventions to improve handover in health care: a systematic review. Med Educ. 2011;45:1081–9.
Chang VY, Arora VM, Lev-Ari S, D’Arcy M, Keysar B. Interns overestimate the effectiveness of their hand-off communication. Pediatrics. 2010;125:491–6.
Cleland JA, Ross S, Miller SC, Patey R. “There is a chain of chinese whispers…”: empirical data support the call to formally teach handover to prequalification doctors. Qual Saf Health Care. 2009;18:267–71.
Shaughnessy EE. Pediatric resident sign-out education. https://www.mededportal.org/publication/8321. Accessed March, 2013.
Shaughnessy EE, Ginsbach K, Groeschl N, Bragg D, Weisgerber M. Brief educational intervention improves content of intern handovers. J Grad Med Educ. 2013;5:150–3.
Arora V, Johnson J. A model for building a standardized hand-off protocol. Jt Comm J Qual Patient Saf. 2006;32:646–55.
Arora V, Johnson J, Lovinger D, Humphrey HJ, Meltzer DO. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14:401–7.
WHO Collaborating Center for Patient Safety Solutions. Communication during patient hand-overs. http://www.who.int/patientsafety/solutions/patientsafety/PS-Solution3.pdf. Accessed December 20, 2014.
Chu ES, Reid M, Schulz T, Burden M, Mancini D, Ambardekar AV, et al. A structured handoff program for interns. Acad Med. 2009;84:347–52.
Riesenberg LA, Leitzsch J, Massucci JL, Jaeger J, Rosenfeld JC, Patow C, et al. Residents’ and attending physicians’ handoffs: a systematic review of the literature. Acad Med. 2009;84:1775–87.
Starmer AJ, Spector ND, Srivastava R, West DC, Rosenbluth G, Allen AD, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371:1803–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding/Support
This study was funded in part by a Medical College of Wisconsin Learning Resource Fund grant PRO00019619.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the institutional review board of the Medical College of Wisconsin/Froedtert Hospital.
Rights and permissions
About this article
Cite this article
Saudek, K., Treat, R. Does Medical Student Hand-Over Training on a Third-Year Pediatric Clerkship Improves Skill and Confidence Level?. Med.Sci.Educ. 26, 649–655 (2016). https://doi.org/10.1007/s40670-016-0327-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-016-0327-7