Summary
Purpose
Pollen allergy can have a significant impact on a person’s quality of life. Recently, food supplements have gained in importance for persons suffering from pollen allergy. Still, there is not much research data on the efficacy of food supplements and the experienced relief, especially when choosing study designs that require less effort than randomized controlled trials (RCT).
Methods
A food supplement containing an Astragalus membranaceus root extract was administered to 328 voluntary participants during the 2018 birch, grass and ragweed pollen season in Austria. Participants documented their symptoms and medication intake in the online Patients Hay-fever Diary (PHD). All participants were asked to answer a quality-of-life questionnaire at the end of the study. Alongside with the adherence rate the overall symptom load index (SLI) and the nasal symptoms of the participants were monitored and compared to a filtered group of users from the PHD.
Results
The adherence rates range from 32.8% to 77.3%. Additional data like a quality-of-life questionnaire and the mean overall/nasal SLI showed differences between participants and the baseline. However, they were only statistically significant for the ragweed pollen season and the nasal symptoms.
Conclusion
The study design relied on the evaluation of crowd-source symptom data alone by comparing the participants with a baseline. The participant adherence turned out lower than expected; however a trend for reduced symptoms was found and is also supported by the quality-of-life questionnaire.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In all, 3–5% of the population in industrialized countries like Austria and other central European countries, suffer from pollen allergy [1]. According to Zuberbier et al. each untreated pollen allergy sufferer costs the health care system approximately 2400 € per year [2]. Therefore, the potentially one million pollen allergy sufferers in Austria [3] might be responsible for yearly costs amounting to about 2.4 billion € in the health care system. To minimize the socioeconomic impact of allergies due to reduced work force or school performance, doctors now have the possibility to reduce the burden of allergy sufferers by selecting a treatment that works best for each individual patient.
These include symptom-relieving nonsedating H1-antihistamines and topical corticosteroids (control-therapy treatment) as well as the immune-modifying allergen-specific immunotherapy [4]. To approve the efficacy of such classic therapeutic interventions the randomized controlled trial (RCT) is currently the state-of-the-art method [5]. However, these studies are often associated with high costs [6] and drop-out rates even though frequent visits to the trial centres are a prerequisite for such RCTs [7].
In addition to the above-mentioned western medical therapy approaches, a large variety of alternative and/or complementing therapies are available such as acupuncture or food supplements which are used by an increasing number of allergy sufferers [8]. As dietary supplements are classified as food or foodstuff, for complementing the normal human diet, they are regulated by other European and national directives than medicinal products [9]. As the purpose of such supplements is not to cure or prevent diseases, RCTs or similar clinical studies are only required if certain health claims are advertised [10].
In the present study a commonly available dietary supplement, Lectranal INTENS® (KOSAN Pharma GmbH, Seewalchen, Austria), was administered to birch (Betula sp.), grass (Poaceae) or ragweed (Ambrosia sp.) pollen allergy sufferers. The active agent in this product is an herbal mineral complex, mainly consisting of an Astragalus membranaceus (Fisch. ex. Bunge) root extract. This substance has been used in traditional Chinese medicine for a long time to reinforce “Qi” (the vital energy)[11, 12]. Pharmaceutical studies have already demonstrated numerous beneficial effects of the main active compounds. Besides positive effects on hepatoprotection, neuroprotection and on anti-aging activity, some components are also attested with anti-cancer and anti-inflammatory effects, as well as cardiotonic properties [12,13,14,15,16,17,18]. A similar food supplement, with the same herbal mineral complex, was already tested in a double-blind placebo-controlled RCT study in Croatia in 2007 [19]. During that study three patient visits to the study centre were scheduled and 7 of the 48 subjects (about 15%) did not complete the trial.
Based on these results the present work tests a novel study approach with the aim to decrease not only the dropout rate but the effort for all participants in general, while still being able to record the efficacy of a food supplement treatment. This innovative study design is based solely on the evaluation of allergy symptom data of study participants and users of the Patients Hay-fever Diary (PHD, www.pollendiary.com). Therefore, all Austrian study participants represent the “treatment group” of this study, whereas the crowd-sourced data of the remaining Austrian PHD-users act as a baseline for further analysis. The present pilot study aims to demonstrate that a simple questionnaire of the PHD and the statistical evaluation of crowd-sourced symptom data can be used to prove the efficacy of food supplements and lead to a lower dropout rate as a result of reducing the effort of study participants.
Materials and methods
This study was conducted during the 2018 pollen season from March until September, with a total of 328 participants from all Austrian counties. By self-assessment 145 participants classified themselves as sensitized to birch pollen (Betula sp.), 119 to grass pollen (Poaceae) and 64 to ragweed pollen (Ambrosia sp.). The participants had the option to select more than one aeroallergen in this assessment. All were supplied with a batch of food supplement that lasts for a period of 8 weeks per allergen selected in the self-assessment. The active component is a 160 mg herbal and mineral complex of an Astragalus membranaceus (Fisch. ex Bunge) root extract. The participants were instructed to take the capsules twice a day on an empty stomach and 30 min before a meal. This routine was initiated 2 weeks prior to the calculated start of the pollen season. Depending on their location the data for one of the 7 biogeographical regions of Austria (ATR1-7) was used (Fig. 1). Pollen data for these regions originate from Austrian monitoring stations and from neighbouring countries (Table 1). In case a sampling site was located at the border of two biogeographic regions, it was used for season calculations of both. This applied to the stations ATTATZ, ATLIEN, ATSVPG, ATVILL and ATVOEC. For further analysis no individual pollen concentrations but the average from all active pollen monitoring stations in the respective biogeographical region was used. Hence, the start of the 2018 pollen seasons in each region were estimated by calculating the average start date of the respective aeroallergen over years 2013–2017, by applying the European Aeroallergen Network (EAN) season definition that is based on the calculation of the Annual Pollen Integral (APIn) defined by Galán et al. [20, 21]. According to the EAN definition, the respective pollen season starts at the day where 1% of the APIn is reached and lasts until 95% of the APIn [20].
Austrian biogeographic regions (ATR). ATR1 Bohemian massif, ATR2 Danube valley and prealpine area, ATR3 Pannonian lowlands, ATR4 Illyrian basins, ATR5 Northern limestone alps, ATR6 Alpine valleys central/south, ATR7 Alpine valleys Austria west; 1–37 pollen monitoring stations (for details see Table 1)
In addition to the predicted dates of the 2018 pollen season the actual start and end dates were calculated by applying the EAN standard season definition to the 2018 pollen data retrospectively. To assess the accuracy of the pollen season forecast all the requested aeroallergens were compared to the actual start dates of the 2018 pollen season. For a retrospective assessment of the pollen seasons graphs of the seven Austrian biogeographic regions were drafted to compare the 2018 pollen season with the historical data (Figs. 2, 3 and 4).
Birch pollen season 2018 (black) in comparison to the historical average from 2013–2017 (grey) for the seven austrian biogeographic Regions (ATR); x‑axis shows the timeline, y‑axis the pollen concentration in particles/m3 air; a Bohemian massif (ATR1), b Danube valley and prealpine area (ATR2), c Pannonian lowlands (ATR3), d Illyrian basins (ATR4), e Northern limestone alps (ATR5), f Alpine valleys central/south (ATR6), g Alpine valleys Austria west (ATR7)
Grass pollen season 2018 (black) in comparison to the historical average from 2013–2017 (grey) for the seven austrian biogeographic Regions (ATR); x‑axis shows the timeline, y‑axis the pollen concentration in particles/m3 air; a Bohemian massif (ATR1), b Danube valley and prealpine area (ATR2), c Pannonian lowlands (ATR3), d Illyrian basins (ATR4), e Northern limestone alps (ATR5), f Alpine valleys central/south (ATR 6), g Alpine valleys Austria west (ATR7)
Ragweed pollen season 2018 (black) in comparison to the historical average from 2013–2017 (grey) for the seven austrian biogeographic Regions (ATR); x‑axis shows the timeline, y‑axis the pollen concentration in particles/m3 air; a Bohemian massif (ATR1), b Danube valley and prealpine area (ATR2), c Pannonian lowlands (ATR3), d Illyrian basins (ATR4), e Northern limestone alps (ATR5), f Alpine valleys central/south (ATR6), g Alpine valleys Austria west (ATR7)
During the pollination period of the respective plant groups, the participants had to continuously enter their allergic symptoms into the PHD. This free-of-charge online questionnaire is available as a mobile app and via a web portal (www.pollendiary.com) and allows for a daily record of allergic symptoms throughout the pollen season. Using this tool, pollen allergy sufferers can document their overall wellbeing, the experienced symptoms of eyes (foreign body sensation, itching, redness, watering), nose (blocked, itching, running nose, sneezing) and lungs (asthma, cough, shortness of breath, wheezing) as well as the severity of the above-mentioned symptoms and the applied medication. The symptoms and medication parameters were then combined to an overall symptom and medication score [22]. As a benefit for using this service, the participants received a personalized pollen forecast for the following days [23]. This anonymized symptom data can be used for various research purposes [22,23,24,25,26].
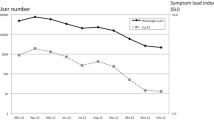
To label the participants their PHD accounts were marked with a study code. To test the food supplements efficacy, the symptom complexes (eyes, nose and lungs) of the participants were compared with those of other PHD users who were not participating in the study but were located in the same biogeographical region. To make this data set comparable the individual symptom and medication scores need to be normalized, as pollen allergy sufferers can react differently to the same amount of allergen exposure [27]. This parameter, the symptom load index (SLI), was developed by Bastl et al. [24] and results in values ranging from 0 to 10 which allows a more comprehensible visualization of symptom severity [28]. In addition to the overall SLI, the SLI of the nasal symptom complex was calculated since nasal symptoms tend to affect the quality-of-life of pollen allergy sufferers the most [27]. This nasal SLI was calculated for participants and baseline by combining only nose symptoms and the applied medication [24].
For calculating the SLI values of the baseline, all PHD users from a biogeographic region (excluding the study participants) were considered, as long as they entered symptoms for 7 or more days in a row and showed a positive correlation to the pollen concentrations of the respective aeroallergen.
After the end of the trial the self-assessment of the participants was checked for positive correlation to the pollen seasons of interest followed by an eventual reclassification to match symptoms and pollen concentrations to achieve a better consistency.
In addition, the participants had to complete a special questionnaire provided by KOSAN Pharma at the end of the study period (Online Resource 1). It consisted of 38 questions to evaluate basal information on the participant (i.e. age, sex, diagnosed pollen allergy), the effect of the food supplement on the participants (i.e. quality of life questions, experienced symptom relief, tolerability) and questions relevant for marketing purposes (i.e. recommendation of the product, reasons for participation, comparison to conventional drugs).
The statistical analysis was performed in R Statistics (R foundation for statisical computing, Vienna, Austria) [29]. A Shapiro–Wilk test for the overall SLI and the nasal SLI scores of participants and the baseline was performed to check for normality of the score vectors. Normality was rejected, so a Wilcoxon–Mann–Whitney rank sum test was performed to compare participants with the baseline. To refine the results, an additional analysis was performed for the SLI of the nose. For graphical display diagrams were plotted in R Statistics and Excel (Microsoft, Redmond, WA, USA).
Results
In a comparison of the predicted and the actual start dates of the 2018 seasons, birch showed the lowest divergence with a prediction between 0–9 days prior to the actual season start. Followed by grasses with differences between 3–12 days earlier (ATR4, ATR5, ATR6 and ATR7) and 2–13 days later (ATR1, ATR2 and ATR3). The prediction of the ragweed pollen season showed high variability with 14 or more days in four biogeographic regions (ATR1, ATR4, ATR5 and ATR7), moderate variability of 12 days earlier in ATR6 and only low variability of 1–4 days delay in ATR2 and ATR3.
The 2018 birch pollen season started with a delay of 1–2 weeks compared to the historic average (Fig. 2) and reached above average intensity throughout Austria (except ATR5). The 2018 grass pollen season in Austria (Fig. 3) started slightly earlier than the historic data suggests but was otherwise of average intensity. The abundance of ragweed in the eastern parts of Austria is clearly visible in the data (Fig. 4), as only the regions ATR1, ATR2, ATR3 and ATR4 (Fig. 4a–d) show a distinct ragweed pollen season. In ATR1 the ragweed season was below average, whereas ATR2, ATR3 and ATR4 recorded a pollen season comparable to the 5‑year average.
Data from 102 birch, 92 grass and 21 ragweed pollen allergy sufferers were recorded in the corresponding seasons resulting in adherence rates of 70.3% for birch, 77.3% for grass and 32.8% for ragweed respectively (Table 2). To gain additional insights on the performance of the food supplement the symptom data of study participants were compared with the baseline. After the filtering process this baseline included up to 65 (birch), 63 (grass) and 15 (ragweed) significant positive correlated users per day respectively for each biogeographical region. Due to the strict inclusion criteria of users the baseline is a significant reference value. The reduction of the mean overall and nasal SLI values of participants compared to the baseline is shown in Table 2. For the overall SLI only study participants sensitized to ragweed recorded a significantly lower SLI than the baseline (∆ = −2.67; p-value < 0.001). Participants sensitized to birch and grasses recorded a lower mean overall SLI than the baseline as well but was not statistically significant.
For the nasal SLI all participants recorded a significantly lower value (Table 2). On average the participants reported values during the ragweed season that were 1.27 units (p-value < 0.001) than the baseline. During the grass and birch pollen season the average was 0.37 units (p-value < 0.001) and 0.29 units lower (p-value < 0.001) respectively.
The KOSAN Pharma questionnaire (Online Resource 1) was completed by 141(97.2%) birch, 110 (92.4%) grass and 63 (98.4%) ragweed pollen allergy sufferers. Participants recorded a decreasing severity of symptoms in all three groups (Online Resource 2). Throughout the birch pollen season, the percentage of high and moderate burden decreased from 36% to 14% and from 39% to 23% respectively, whereas the number of participants reporting low burden increased from 16% to 54%. During the grass pollen season high burden dropped from 45% to 9% and moderate burden from 43% to 18%, whereas the low burden increased from 7% to 54%. During the ragweed pollen season high burden dropped from 33% to 8% and medium burden from 48% to 32%, whereas low burden increased from 13% to 51%.
For nasal symptoms a reduced burden was recorded as well. For the symptom “blocked nose” 68% of the birch, 81% of the grass and 70% of the ragweed pollen allergy sufferers stated a reduction of the symptom severity. For the symptom “sneezing” similar values were recorded with 65% for birch, 73% for grass and 79% for ragweed pollen allergy sufferers. Symptom relief was also reported for “runny nose” in 67% of birch, 75% of grass and 83% of ragweed pollen allergy sufferers.
Discussion
Pollen season
Applying the EAN season definition to historical pollen data for predicting the start of the 2018 pollen season worked properly for birch. The actual start of the birch pollen season took place 0–9 days prior to the calculated start and therefore already within the puffer period where the participants started to take in the food supplement. For the grass pollen season the predictions had some higher variation ranging from 3–12 days earlier to 2–13 days later but stayed within the puffer period as well thus, resulting in no potential negative effects as well. The season prediction for ragweed showed the highest variability and was not as precise since it is strongly influenced by long-distance transport of pollen in parts of Austria where the plant rarely occurs. In ATR1 calculations determined a season start in the beginning of May. However, this is not supported by phenological observations, since ragweed is usually flowering in late summer and autumn [30]. This is one flaw of the here used season definition, as it is susceptible for errors if the APIn is too low. By using the 5‑year average for predicting the start of the ragweed pollen season the result became more congruent to phenological observations and therefore replaced the actual start date in ATR1 (10 August 2018) for the analysis of adherence and symptom data. Similar observations were detected for the regions ATR4, ATR5, ATR6 and ATR7. The start date of the ragweed pollen season for ATR4 was predicted long before the actual start of the season in 2018. This discrepancy was caused by the withdrawal of service by two monitoring stations in this biogeographical region in mid 2016. For the regions ATR5, ATR6 and ATR7 the season prediction does not result in accurate starting dates either, because ragweed is not an abundant weed in these areas [31, 32]. Therefore, the results from the EAN season definition calculations are neither representative nor congruent to phenological observations. The pollen concentrations in ATR5 are caused mainly by long-distance transport of ragweed pollen from the surrounding areas, whereas ATR6 and ATR7 record only low concentrations caused by locally restricted ragweed populations [31, 32]. These populations may cause a local burden but do not provide a solid base for a regional season definition. Such effects must be monitored more carefully in future studies to provide more accurate pollen season predictions. In ATR2 and ATR3, the forecasting model calculated start dates that were 2–5 days after the actual start of the 2018 ragweed pollen season. Therefore, all participants already started with the food supplement intake.
Symptom load index
The symptom load index (SLI) is a robust parameter to display the burden of pollen allergy sufferers [24, 27, 28]. It combines symptoms of eyes, nose and lungs with a medication score [24]. The allergenic burden of various pollen allergy sufferers can be compared by calculating the SLI despite the individual reaction pattern of each person [33]. It should be mentioned that many participants, by nature, were sensitized to more than one aeroallergen [34].
The SLI allows the comparison of study participants with other users of the PHD who were combined to the baseline in this study. While the present study shows a slight trend that the participants recorded a lower SLI than the baseline for all three pollen seasons, no significant differences between participants and baseline were recorded for birch and grasses (Table 2). Only during the ragweed pollen season was a highly significant difference between the two groups detected, as the mean SLI of participants was 2.67 units lower than the mean of the baseline (Table 2).
SLI nose score
A retrospective analysis of the symptom data was conducted to compare the nasal SLI scores of the participants and the baseline since this symptom complex impacts the quality of life of pollen allergy sufferers the most [27]. The study participants recorded a significantly lower burden than the baseline during the three pollen seasons indicating that the food supplement positively affects the study participants quality of life. The highest difference between participants and baseline were recorded for ragweed, followed by grasses and birch (Table 2) indicating that the food supplement positively affects the study participants quality-of-life during the three tested pollen seasons.
Comparison to the KOSAN questionnaire
At the end of the 2018 pollen season a one-time questionnaire from the food supplement manufacturer was distributed to all study participants (Online Resource 1). Over 90% of participants completed this questionnaire whose results support that the participants suffered from less severe allergic symptoms (especially in the organ complex nose), which ultimately led to a higher quality-of-life.
Participant adherence, study design and possible improvements
The aim of this work was to test a new approach to increase the adherence of participants during a study. The main aspect to achieve this was to reduce the individual efforts, by replacing the necessity of blood samples with symptom data from the PHD while using the tested food supplement. This task requires a maximum of 5 min per day and can be done via a web browser or an app. Despite these low requirements the current study was not able to reach a dropout rate of less than 15% and was therefore poorer than a RCT that tested a similar food supplement [19].
Based on long-term observations of the PHD-user behaviour it becomes apparent that pollen allergy sufferers tend to enter their symptom data more consistently during the time they experience severe allergenic burden [24]. Even though the present study was conducted during the predicted main pollination period of the three aeroallergens only 70.3% of the participants entered data during the birch pollen season, 77.3% during the grass pollen season and 32.8% during the ragweed pollen season. The benefits of personalized pollen information and the provision of free food supplement for 8 weeks did not increase the adherence of the participants as expected. Still, the simple study design allowed the recruitment of a large number of participants within a short timeframe and a comprehensive statistical analysis. The presented study which combines symptom data of study participants with crowd-sourced data as a baseline should not be discarded since the results are convincing and the baseline of PHD users is robust. During future studies, the data entry frequency of study participants must be monitored more precisely. In case some users forget to enter their daily symptom data either a push notification via the app, or an e‑mail reminder seem promising to further increase participant adherence. Moreover, a reward system could be developed to improve adherence during the study period even further. The effect of daily reminders on the adherence rate could be evaluated in upcoming studies. Depending on the effect of this adaptation and the available budget, financial compensation for a complete data track might also be an option.
Conclusion
The study design based on crowd sourced symptom data shows potential to be used for similar purposes after performing the proposed improvements to enhance the participant’s adherence. Despite evidence of numerous beneficial effects of the active agents in Astragalus membranaceus extracts, the current approach did not record a statistically significant reduction in the overall symptom load index (SLI), but only for the symptom complex nose (nasal SLI). However, the collected symptom data show a trend towards a reduced symptom load supported by the KOSAN quality-of-life questionnaire.
Availability of data
Users were guaranteed anonymity, so no raw data or individual user data is available.
Abbreviations
- APIn:
-
Annual pollen integral
- ATR1‑7:
-
Austrian biogeographic region in the patients hay-fever diary
- EAN:
-
European Aeroallergen Network
- PHD:
-
Patients Hay-fever Diary
- RCT:
-
Randomized controlled trial
- SLI:
-
Symptom load index
References
Asher MI, Montefort S, Björkstén B, Lai CKW, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multicountry cross-sectional surveys. Lancet. 2006;368:733–43. https://doi.org/10.1016/S0140-6736(06)69283-0.
Zuberbier T, Lötvall J, Simoens S, Subramanian SV, Church MK. Economic burden of inadequate management of allergic diseases in the European union: a GA 2 LEN review. Allergy. 2014;69:1275–9. https://doi.org/10.1111/all.12470.
Dorner T, Rieder A, Lawrence K, Kunze M. Österreichischer Allergiebericht. Verein Altern mit Zukunft. 2006.
Holgate ST, Polosa R. Treatment strategies for allergy and asthma. Nat Rev Immunol. 2008;8:218–30. https://doi.org/10.1038/nri2262.
Hariton E, Locascio JJ. Randomised controlled trials—the gold standard for effectiveness research. BJOG. 2018;125:1716–1716. https://doi.org/10.1111/1471-0528.15199.
Speich B, von Niederhäusern B, Schur N, Church MK, Fürst T, Bhatnagar N, et al. Systematic review on costs and resource use of randomized clinical trials shows a lack of transparent and comprehensive data. J Clin Epidemiol. 2018;96:1–11. https://doi.org/10.1016/j.jclinepi.2017.12.018.
Bell ML, Kenward MG, Fairclough DL, Horton NJ. Differential dropout and bias in randomised controlled trials: when it matters and when it may not. BMJ. 2013;346:e8668–e8668. https://doi.org/10.1136/bmj.e8668.
Kern J, Bielory L. Complementary and Alternative Therapy (CAM) in the treatment of allergic rhinitis. Curr Allergy Asthma Rep. 2014;14:479. https://doi.org/10.1007/s11882-014-0479-8.
Domínguez Díaz L, Fernández-Ruiz V, Cámara M. The frontier between nutrition and pharma: the international regulatory framework of functional foods, food supplements and nutraceuticals. Crit Rev Food Sci Nutr. 2020;60:1738–46. https://doi.org/10.1080/10408398.2019.1592107.
The European Parliament and the Council of the European Union. Regulation (EC) no 1924/2006 of the European parliament and of the council of 20 december 2006 on nutrition and health claims made on foods. Off J Eur Union L. 2006on;404:9–25.
Tang W, Eisenbrand G. Chinese drugs of plant origin. Berlin, Heidelberg: Springer Berlin Heidelberg; 1992.
Lee D‑Y, Noh H‑J, Choi J, Lee K‑H, Lee M‑H, Lee J‑H, et al. Anti-inflammatory cycloartane-type saponins of astragalus membranaceus. Molecules. 2013;18:3725–32. https://doi.org/10.3390/molecules18043725.
Tohda C, Tamura T, Matsuyama S, Komatsu K. Promotion of axonal maturation and prevention of memory loss in mice by extracts of astragalus mongholicus. Br J Pharmacol. 2006;149:532–41. https://doi.org/10.1038/sj.bjp.0706865.
Zhang W‑D, Chen H, Zhang C, Liu R‑H, Li H‑L, Chen H‑Z. Astragaloside IV from astragalus membranaceus shows cardioprotection during myocardial ischemia in vivo and in vitro. Planta Med. 2006;72:4–8. https://doi.org/10.1055/s-2005-873126.
Lei H, Wang B, Li W‑P, Yang Y, Zhou A‑W, Chen M‑Z. Anti-aging effect of astragalosides and its mechanism of action. Acta Pharmacol Sin. 2003;24:230–4.
Cho WCS, Leung KN. In vitro and in vivo anti-tumor effects of astragalus membranaceus. Cancer Lett. 2007;252:43–54. https://doi.org/10.1016/j.canlet.2006.12.001.
Zhang W‑J, Hufnagl P, Binder B, Wojta J. Antiinflammatory activity of astragaloside IV is mediated by inhibition of NF-κB activation and adhesion molecule expression. Thromb Haemost. 2003;90:904–14. https://doi.org/10.1160/TH03-03-0136.
Rios JL, Waterman PG. A review of the pharmacology and toxicology of Astragalus. Phytother Res. 1997;11:411–8. https://doi.org/10.1002/(SICI)1099-1573(199709)11:6%3C411::AID-PTR132%3E3.0.CO;2-6.
Matkovic Z, Zivkovic V, Korica M, Plavec D, Pecanic S, Tudoric N. Efficacy and safety of astragalus membranaceus in the treatment of patients with seasonal allergic rhinitis. Phytother Res. 2010;24:175–81. https://doi.org/10.1002/ptr.2877.
Bastl K, Kmenta M, Berger UE. Defining pollen seasons: background and recommendations. Curr Allergy Asthma Rep. 2018;18:73. https://doi.org/10.1007/s11882-018-0829-z.
Galán C, Ariatti A, Bonini M, Clot B, Crouzy B, Dahl A, et al. Recommended terminology for aerobiological studies. Aerobiologia. 2017;33:293–5. https://doi.org/10.1007/s10453-017-9496-0.
Karatzas K, Voukantsis D, Jäger S, Berger UE, Smith M, Brandt O, et al. The patient’s hay-fever diary: three years of results from Germany. Aerobiologia. 2014;30:1–11. https://doi.org/10.1007/s10453-013-9303-5.
Kmenta M, Bastl K, Jäger S, Berger UE. Development of personal pollen information—the next generation of pollen information and a step forward for hay fever sufferers. Int J Biometeorol. 2014;58:1721–6. https://doi.org/10.1007/s00484-013-0776-2.
Bastl K, Kmenta M, Jäger S, Bergmann KC, Berger UE. Development of a symptom load index: enabling temporal and regional pollen season comparisons and pointing out the need for personalized pollen information. Aerobiologia. 2014;30:269–80. https://doi.org/10.1007/s10453-014-9326-6.
Voukantsis D, Karatzas K, Jäger S, Berger UE, Smith M. Analysis and forecasting of airborne pollen–induced symptoms with the aid of computational intelligence methods. Aerobiologia. 2013;29:175–85. https://doi.org/10.1007/s10453-012-9271-1.
Kmenta M, Bastl K, Kramer MF, Hewings SJ, Mwange J, Zetter R, et al. The grass pollen season 2014 in Vienna: a pilot study combining phenology, aerobiology and symptom data. Sci Total Environ. 2016;566–567:1614–20. https://doi.org/10.1016/j.scitotenv.2016.06.059.
Bastl K, Bastl M, Bergmann KC, Berger M, Berger UE. Translating the burden of pollen allergy into numbers: 10-year observational study of electronically generated symptom data from the patient’s hayfever diary in Austria and Germany. J Med Internet Res. 2020;22:e16767. https://doi.org/10.2196/16767.
Bastl K, Kmenta M, Geller-Bernstein C, Berger UE, Jäger S. Can we improve pollen season definitions by using the symptom load index in addition to pollen counts? Environ Pollut. 2015;204:109–16. https://doi.org/10.1016/j.envpol.2015.04.016.
R Core Team. R: a language and environment for statistical computing. R foundation for statistical computing, Vienna, Austria. 2021. https://www.R-project.org/..
Fischer MA, Oswald K, Adler W. Exkursionsflora für Österreich, Liechtenstein und Südtirol. Land Oberösterreich, Biologiezentrum der Oberösterr. Landesmuseen, Linz; 2008.
Storkey J, Stratonovitch P, Chapman DS, Vidotto F, Semenov MA. A process-based approach to predicting the effect of climate change on the distribution of an invasive allergenic plant in Europe. PloS One. 2014;9:e88156. https://doi.org/10.1371/journal.pone.0088156.
Essl F, Dullinger S, Kleinbauer I. Changes in the spatio-temporal patterns and habitat preferences of Ambrosia artemisiifolia during its invasion of Austria. Preslia. 2009;81:119–33.
Bastl M, Bastl K, Dirr L, Berger M, Berger UE. Variability of grass pollen allergy symptoms throughout the season: comparing symptom data profiles from the patient’s hayfever diary from 2014 to 2016 in Vienna (Austria). World Allergy Organ J. 2021;14:100518. https://doi.org/10.1016/j.waojou.2021.100518.
Mari A. Multiple Pollen Sensitization: A Molecular Approach to the Diagnosis. Int Arch Allergy Immunol. 2001;125:57–65. https://doi.org/10.1159/000053797.
Acknowledgements
Christoph Jäger is thanked for providing data from the European aeroallergen network database and the patients hay-fever diary, and Alexander Kowarik for assisting with the statistical analyses. We are also indebted to KOSAN Pharma GmbH and Jochen Schilling for the financial support that enabled this study.
Funding
This work was supported by KOSAN Pharma GmbH. The company supplied the food supplement for free to the study participants. The author group conducted the study, analysed the data and published the results without any influence from KOSAN Pharma GmbH.
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Contributions
LD and KB drafted the main body of the manuscript and supervised the analyses. MB performed the analyses and prepared the tables. JB prepared the figures. UB and FG initiated and supervised the study. All authors took part in writing and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
L. Dirr, K. Bastl, M. Bastl, J.M. Bouchal, U.E. Berger and F. Grímsson declare that they have no competing interests.
Ethical standards
This is an observational study. No ethics approval was needed. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Online Resource 1
Questionnaire provided and designed by KOSAN Pharma GmbH for a one-time assessment in German (original) and English language (translation)
Online Resource 2
Graphical display of the relevant questions from the KOSAN Pharma GmbH questionnaire for the three pollen seasons
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dirr, L., Bastl, K., Bastl, M. et al. Crowd-sourced symptom data in pollen allergy: testing a novel study approach for assessing the efficacy of food supplements. Allergo J Int 33, 180–189 (2024). https://doi.org/10.1007/s40629-024-00283-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40629-024-00283-y