Abstract
Background
Conflicting evidence exists regarding the relationship between socioeconomic status and access to or outcomes after kidney transplantation. This study analyzed the effects of individual and neighborhood socioeconomic status on kidney transplant access and outcomes in Taiwan.
Methods
We used a retrospective cohort study design and performed comparisons using the Cox proportional hazards model after adjusting for risk factors. Data were collected from the National Health Insurance Bureau of Taiwan data (2003–2012).
Results
Patients with high individual and neighborhood socioeconomic status had higher chances of receiving kidney transplants than those with low individual and neighborhood socioeconomic status [adjusted hazard ratio (aHR) = 2.04; 95% CI: (1.81–2.31), p < 0.001]. However, there were no significant differences in post-transplant graft failure or patient mortality in Taiwan between individuals of varying socioeconomic status after five years. When we stratified kidney transplants by domestic and overseas transplantation, there were no significant differences in post-transplant mortality and graft failure, but individuals who received a kidney graft in Taiwan with high individual and neighborhood socioeconomic status experienced lower risks of graft failure (aHR = 0.55; [95% CI 0.33–0.89], p = 0.017).
Conclusion
A relevant disparity exists in accessing kidney transplantation in Taiwan, depending on individual and neighborhood socioeconomic status. However, results post transplantation were not different after five years. Improved access to waitlisting, education, and welfare support may reduce disparities.
Graphical Abstract

Similar content being viewed by others
Introduction
Taiwan has the highest incidence of end-stage kidney disease (ESKD) worldwide. The prevalence of ESKD reached 3546 per million people by 2021 [1]. Furthermore, at least 20% of Taiwan’s population consists of elderly people, making it an extreme-aged society, according to the definition of “aged society” as having more than 14% of elderly people [2]. Aging is associated with an increased prevalence of chronic diseases, such as hypertension and diabetes mellitus, and the use of herbs with and without aristolochic acid in Taiwan has contributed to the incidence of ESKD [3, 4]. Taiwan’s current healthcare system, the National Health Insurance (NHI), is a single-payer compulsory social insurance plan providing healthcare to all Taiwanese residents. Coverage reached 99% of the population at the end of 2004. The health insurance system is inexpensive and provides care to patients undergoing dialysis. At present, the 5-year survival rate for dialysis patients in Taiwan is nearly 60%, compared to 40.3% and 41.3% for US hemodialysis patients and peritoneal dialysis patients, respectively, but similar to Korean dialysis patients [1, 5]. Care for patients undergoing dialysis is a financial burden on the healthcare system. As they live longer, the number of dialysis patients has increased. The medical community prefers transplantation to dialysis because of its advantages on life expectancy, health outcomes, quality of life, and lower medical costs [6]. Kidney transplantation rates vary across countries. In 2021, the incidence of KT was highest in Brunei Darussalam (109 per million general population [PMP]), followed by the U.S. (77 PMP), Jalisco (58 PMP), and Israel (56 PMP). Most European countries reported rates of 30–40 PMP [1]. However, KT rates in Taiwan are lower, at only 15 PMP. Only approximately 345 people in Taiwan undergo successful kidney transplantation per year, accounting for 0.4% of ESKD patients, compared with 50% in England and Scandinavian countries [1].
Access to organ transplantation is determined by the availability of organs and healthcare. There are two organ sharing systems: the China Organ Registry Center, which was established in 2008, and the Taiwan Organ Registry and Sharing Center, which was established in 2002 to serve as a bridge between donors, recipients, organ procurement hospitals, and organ transplantation hospitals [7,8,9,10]. Only deceased donor and living-related kidney transplants are currently performed in China, and there have been no living-unrelated donors since January 1, 2015 [7,8,9]. In Taiwan, patients can register on kidney transplant waiting lists in Taiwan and China because of China’s political policy. Hence, they can receive kidney transplants in both China and Taiwan. However, when receiving kidney transplants in China, patients must pay the medical cost of transplantation, as the Taiwanese health insurance does not cover the medical fees in China. Fundamental inequalities exist in access to transplantation after waiting list acceptance for adults in both the USA and Europe [11,12,13,14,15,16,17]. Medical conditions and non-medical factors affect whether patients receive a transplant. Patient characteristics include age; chronic diseases, such as diabetes mellitus; gender [11,12,13,14]; race [16]; socioeconomic factors, such as educational level, and area of residence, a proxy of income [11, 12]. Few studies have examined the interactions between individual socioeconomic status and neighborhood deprivation, and so far the findings are heterogeneous [12,13,14,15, 17, 18]. Death rates for adults with low socioeconomic status were the highest in high-socioeconomic status neighborhoods and lowest in low-socioeconomic status neighborhoods [18]. The Taiwanese government reports that 95% of Taiwan's population is of Han Chinese ethnicity. Over 2% of the population consists of indigenous Taiwanese. Twenty-one thousand Westerners live in Taiwan, accounting for 0.1% of its total population. There were 300,000–400,000 South Asian residents (Indonesians, Filipinos, Thai, Vietnamese) in Taiwan from 2003 to 2012, representing 1.3–1.7% of the country's population [19]. Hence, choosing the Taiwanese population as the study group eliminated racial bias since the presence of socioeconomic disparities may impact long-term graft survival. Further research is needed to examine the mechanisms contributing to disparities in kidney transplantation and post-transplant survival, to ultimately intervene with culturally sensitive approaches.
We designed a population-based study using data from the Taiwan NHI Administration to investigate the role of individual and neighborhood socioeconomic status on access to domestic and overseas kidney transplantation. Furthermore, we investigated survival rates after transplantation according to different subgroups.
Methods
Ethics statement
This study was approved by the Ethics Committee of Kaohsiung Veterans General Hospital (VGHKS18-CT10-07). The requirement for informed consent was waived because the data were anonymized.
Database
The NHI Program database contains registration files and original claims data for reimbursement. Large computerized databases derived from this system by the NHI Administration are provided to scientists in Taiwan for research purposes. This dataset can be accessed from the NHI Research Database (NHIRD) website (http://nhird.nhri.org.tw/). The NHIRD provides extensive information, including age, sex, date of admission, mortality, International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) medical procedures, diagnostic codes, comorbidities, and emergency care details. In Taiwan, all chronic dialysis payments are covered by the NHI program; in other words, all patients with ESKD (based on ICD-9-CM code 585) are included in the NHIRD. The diagnosis of ESKD with ICD-9-CM code 585 can only be made by certified nephrologists and revalidated by nephrologists selected from other hospitals. In the original study, the NHI Bureau of Taiwan randomly reviewed the charts of 1 out of every 100 ambulatory cases in the year 2000, and the study groups were followed up from 2003 to 2012 based on Taiwan’s NHIRD. For the protection of personal information, all data were de-identified as secondary data.
Measurement
Patient selection and definition
This study included all working-age patients (20–65 years old) with ESKD in Taiwan between 2003 and 2012 using the database of major illnesses (based on the ICD-9-CM codes 585.6), with patient demographics obtained at diagnosis of ESKD, including age, sex, medical comorbidities, number of admissions, and hospital characteristics. We obtained data on all patients who had received kidney transplants based on the ICD-9-CM codes V42.0. In Taiwan, all patients undergoing kidney transplantation receive a medical claim review by nephrologists or urologists from different medical facilities. To identify domestic or overseas kidney transplants, we checked transplant recipients (ICD-9-CM codes V42.0) to determine whether they had undergone kidney transplant surgery (ICD-9-CM codes 76020A, 76020B, and 97416K). Kidney transplantation and surgery codes were defined as domestic kidney transplants. A kidney transplant code without a surgery code was defined as an overseas kidney transplant. Overseas kidney transplant recipients were validated using the NHI-based registry of catastrophic illness to exempt co-payment. Allograft failure was identified based on the patient’s dialysis re-entry (defined as > 10 dialysis sessions 90 days after transplantation), including hemodialysis and peritoneal dialysis (ICD-9-CM codes 58001C, 58027C, 58029C, and 58002C). Patient death could be identified by the NHI system. Non-transplant patients were censored at the date of death or end of the follow-up period. Living patients were censored at the end of the follow-up period. Kidney transplantation was considered as a time-dependent covariate.
We selected individual and neighborhood socioeconomic status and survival as the main independent variables.
Individual-level measures
In this study, we used income-related insurance payment amounts as a proxy for individual socioeconomic status. After confirming that the use of this proxy was validated in a previous study [20], we selected US$698 (New Taiwan Dollar [NT$] 21,500) per month as the low-income cut-off point because this was the government-stipulated minimum wage for full-time employees in Taiwan in 2007 [21].
Neighborhood-level socioeconomic status
We divided Taiwan into 369 areas, including townships and small cities, for socioeconomic analysis. To characterize township-level socioeconomic conditions, we first identified information from Taiwan’s census statistics depicting neighborhood and household economic conditions. Variables associated with known socioeconomic differences were also included. We defined neighborhood socioeconomic status based on the percentage of households and average family income in Taiwan. In this census, the neighborhood household income of a township was the per-capita income determined by the Taiwan Ministry of Finance based on 2003 tax statistics (Supplementary Figure S1) [21]. The neighborhoods were sorted according to their median incomes; high- and low-socioeconomic status neighborhoods had higher and lower-than-median household incomes, respectively. We stratified population density, number of outpatients followed-up, number of inpatients, and residential urbanization [20, 22].
Others
In this study, other comorbidities were classified as congestive heart failure (ICD-9-CM code 428.x), chronic obstructive pulmonary disease (ICD-9-CM codes 491.2x, 493.2x, and 496), hypertension (ICD-9-CM code 401.9), diabetes mellitus (ICD-9-CM code 250.x), stroke (ICD-9-CM code 433.xx–434.xx), and coronary artery disease (ICD-9-CM codes 410.x–414.x). We categorized diseases with ≥ 3 outpatient visits into the high outpatient group and those with ≥ 1 inpatient admission into the high inpatient group. We used the accreditation level to distinguish hospitals as medical centers, regional hospitals, or district hospitals.
Statistics
Statistical analyses were performed using the Statistical Product and Service Solutions (SPSS) software (version 22; SPSS, Inc., Chicago, IL, USA) and Statistical Analysis Software (SAS) version 9.3. Pearson’s chi-squared test was used to analyze categorical variables (level of urbanization, sex, category, and geographic region of residence) and hospital characteristics (medical center, district, and regional). The primary outcome was the association between individual and neighborhood socioeconomic status and access to kidney transplants, including deceased-donor or living-donor kidney transplants. The secondary outcome was the association between individual and neighborhood socioeconomic status and recipient mortality or graft failure, which was analyzed using the Kaplan–Meier survival curve and log-rank test. The Cox proportional hazards regression model was used to compare the results of different socioeconomic status categories before and after adjusting for patient characteristics (sex, age, and area of residence), comorbidities, and hospital characteristics (medical center, district, and regional). Statistical significance was defined as a two-sided p-value of < 0.05.
Results
Study process flowchart (Fig. 1)
Overall, 57,508 patients with ESKD aged 20–65 years were included in this study. Only 3004 patients (2.7%) received kidney transplants.
Demographic data and socioeconomic status characteristics
Table 1 shows the distribution of demographic and social variables, and how the variables differed depending on socioeconomic status for all patients. Compared with the disadvantaged socioeconomic status group, the advantaged socioeconomic status group was younger, consisted of more men, had higher turnaround times for receiving kidney transplants, and experienced less congestive heart disease, diabetes mellitus, and cardiovascular disease (p < 0.01).
The association of individual and neighborhood socioeconomic status on access to kidney transplantation (Fig. 2 and Table 2)
Age, sex, and comorbidities can decrease access to kidney transplantation. The proportional hazard assumption tests were checked by the survival time as the horizontal axis and the logarithmic survival (Supplementary Figure S2) and Schoenfeld residual analysis (Supplementary Figure S3). We found that patients with higher individual socioeconomic status who lived in more advantaged neighborhoods had a higher adjusted hazard ratio [(aHR) = 2.04, 95% CI 1.81–2.31, p < 0.001] for kidney transplantation after adjusting for other variables than the patients with low individual socioeconomic status who lived in disadvantaged areas (Table 2). Moreover, patients with low individual socioeconomic status living in advantaged neighborhoods had a higher rate of kidney transplantation (aHR = 1.32, 95% CI (1.16–1.53), p < 0.001) even after adjusting for age, sex, and individual comorbidities (Table 2).
The association of individual and neighborhood socioeconomic status on access to overseas or domestic kidney transplantation
Of those who received transplants, 39.8% of patients did so overseas and 60.2 percent underwent tranplantation in Taiwan. As shown in Table 3, for overseas kidney transplantation, patients with high individual socioeconomic status also had a higher transplantation rate than those with low individual socioeconomic status after adjusting for variables (aHR = 2.51, 95% CI 2.09–3.02, p < 0.001). For domestic kidney transplantation, patients with high individual socioeconomic status living in advantaged areas had the highest rate of kidney transplantation (aHR = 2.01, 95% CI 1.74–2.34, p < 0.001).
The association of individual and neighborhood socioeconomic status on graft failure or patient mortality in overall kidney transplantation
In overall kidney transplantation of Taiwanese patients (domestic and overseas), we found no significant differences in 5-year graft failure or life mortality in groups sorted for individual or neighborhood socioeconomic status after adjusting for age, sex, outpatient follow-up duration, number of admissions, hospital characteristics, area of residence, and comorbidities (Table 4).
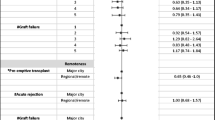
The association of individual and neighborhood socioeconomic status on graft failure and patient mortality in overseas and domestic kidney transplantation (Figs. 3, Fig. 4)
In domestic kidney transplantation (Table 5), there were no differences in the survival of patients with different individual and neighborhood socioeconomic status (p > 0.05). However, for graft failure, the group with high individual socioeconomic status, living in advantaged areas had a lower risk (0.55; 95% CI, 0.33–0.89) compared to the group with low individual socioeconomic status living in disadvantaged areas. Regarding overseas kidney transplants (Table 5), we found no significant difference in mortality or graft failure between individual- and neighborhood-level socioeconomic status after adjusting for age, sex, outpatient follow-up duration, number of admissions, hospital characteristics, area of residence, and comorbidity (Table 5).
Discussion
This population-based study in Taiwan assessed the combined effects of individual and neighborhood socioeconomic status on access to kidney transplantation in patients with ESKD. We investigated post-transplant patient readmission rates and graft survival using data provided by the NHI system. Data show that only 3004 patients (2.7% of ESKD patients) underwent kidney transplantation between 2003 and 2012 (10 years). Furthermore, patients with lower individual and neighborhood socioeconomic status had a lower chance of kidney transplantation despite Taiwan’s universal care and donor care system. We divided the transplant population into two groups, those who received a kidney transplant overseas and in Taiwan; the disparity in access to kidney transplants remained, and was associated with patients’ socioeconomic status and place of residence. However, these inequalities, including mortality and graft failure, were less relevant after transplantation. In the subgroup analysis, disparities existed only within domestic kidney transplant graft survival rates.
Concerning overseas kidney transplants, patients with low socioeconomic status cannot afford the fees for travel, surgery, and immunosuppressive drugs. Thus, it is reasonable to assume that disparities exist between overseas kidney transplant recipients and domestic ones. Previous studies have shown an association between individual or area socioeconomic status inequalities and access to kidney transplantation [12,13,14,15, 17, 18]. Socioeconomically disadvantaged patients may have more comorbidities and lower medication adherence rates. Potential barriers along the path to transplantation have been identified in the United States. Several studies show that transplantation rates are associated with socioeconomic and geographical factors, and vary significantly across different ages, races, and sex [11,12,13,14,15,16,17,18]. There are also some findings regarding culturally-related and local barriers to kidney transplantation among Asians and Pacific Islanders, particularly those residing in resource-deprived neighborhoods [23]. Moreover, a higher social adaptability index is associated with an increased likelihood of being wait-listed for kidney transplant [24]. In our study, we found that only 12.2% of ESKD patients were on the domestic kidney transplant waiting list. Despite Taiwan being a small island, patients with lower individual socioeconomic status and those living in deprived neighborhoods also have less access to transplants. This suggests the existence of several barriers. According to the Taiwan organ-sharing system, patients with ESKD need to return to the outpatient clinic regularly to maintain waitlisting. Patients who did not return beyond 6 months were excluded from the waiting list. Despite the fact that access to the organ share system is universal and free of charge in Taiwan, patients with lower income experience other difficulties, such as the need to work extra hours to support family and the financial burden of transportation to attend medical appointments. Therefore, if patients have low socioeconomic status or live in disadvantaged areas, they may be less likely to return for checkups. Furthermore, low socioeconomic status is associated with lower education in understanding their rights to use social welfare and medical systems. A Canadian study found that Canadians with lower-socioeconomic status used primary care more frequently, but when adjusted for their healthcare needs, they were less likely to receive specialty care [25].
Socioeconomic factors drive outcomes in many areas of healthcare, including access to primary and specialty healthcare, compliance with therapy, ability to afford medications, and outcomes after surgical procedures. This suggests that access to primary care may be a pathway through which income inequality affects mortality rates. Socioeconomic status-driven health inequalities are pronounced even in countries with universal healthcare. A recent study from Canada showed higher mortality among men with lower income, education, and occupational status for several causes of death [26]. In England, socioeconomic status disparities persisted and even widened after the establishment of the National Health Service [28]. The provision of universal coverage was insufficient to offset broader economic and social changes and inequalities. Socioeconomic status differences may be exacerbated by policies that require co-payment for drugs such as intravenous immunoglobulins, or that limit coverage to only several months post-transplantation [12]. However, in our study, individual and neighborhood socioeconomic status are not significantly associated with graft and patient survival after kidney transplantation. This can be attributed to the medical healthcare provided by Taiwan’s NHI and the social welfare system which provides free health coverage to low-income people.
The number of overseas transplants increased rapidly, perhaps because of improved transplantation outcomes, increased brokering activity, and organ supply in China. The number of overseas transplantations in Taiwan increased after 2000, peaked in 2005, and decreased after 2007 [27,28,29]. Taiwanese people can still register in China’s organ-sharing system and undergo kidney transplant in China because Taiwan is considered a part of China. Subgroup analysis revealed no significant differences in the overseas post-transplant mortality and graft failure rates. The Taiwanese healthcare system provides the same post-transplant care for overseas and domestic kidney transplant recipients. However, subgroup analysis for domestic kidney transplants revealed that individuals with high personal and neighborhood socioeconomic status experienced lower risks of graft failure (aHR = 0.55; [95% CI 0.33–0.89], p = 0.017) in domestic kidney transplants, suggesting that there is still need to reduce inequalities. The kidney transplant screening process could be one of the causes of the differences in graft failure. In Taiwan, all kidney transplant recipients receive an insurance that covers complement-dependent lymphocytotoxic cross-match tests to avoid rejection. However, further tests, such as donor-specific antibody screening (Luminex solid-phase assay or C1q assay) and antibody removal treatments, are not covered by this health insurance, and some patients cannot afford these tests. It is desirable that these treatments will be covered by the health insurance.
The strength of this study is that it used a nationwide cohort of ESKD patients to try to avoid selection biases and obtain a sufficient sample size to detect differences among patients with kidney transplantation with different individual and neighborhood socioeconomic status. Choosing the Taiwanese population as a study group may reduce the element of racial differences because over 95% of Taiwan's population is Han Chinese [19]. Furthermore, the diagnosis of ESKD related to dialysis and kidney transplantation is accurate because all medical charts must be reviewed by other hospital experts to confirm the diagnosis and avoid misclassification. However, this study has several limitations. In this study, we did not have detailed patient data, such as the cause of kidney disease and history of sensitization of patients to human leukocyte antigens in the NHIRD. Second, kidney transplantation candidates are selected and those with poor physical or mental health are less likely to be waitlisted. Confounding biases, such as low socioeconomic status, are also often associated with poorer overall health. Hence, the effects of low individual socioeconomic status may be underestimated because this analysis only included patients who successfully completed the process of evaluation and wait-listing. Even though multiple confounding variables such as medical comorbidity (Table 1) were controlled or adjusted for, residual confounding variables may still exist.
In conclusion, this study demonstrates the independent and combined effects of individual and neighborhood socioeconomic status on access to kidney transplantation, but not with the 5-year post-transplantation survival rate. Patients with individual and neighborhood deprivation were less likely to undergo kidney transplantation than those with individual deprivation and neighborhood advantage. However, differences in post-transplantation care are reduced through the follow-up offered by the Taiwanese healthcare system. Improved access to waitlisting through outreach clinics, education, or welfare support may further reduce disparities.
Availability of data and material
The datasets used, analyzed, or both during the current study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
USRDS. Chapter 11: international comparisons. united stated renal data system annual data report. 2023 US renal data system. https://usrds-adr.niddk.nih.gov/2023. Accessed 14 Nov 2023
https://www.ndc.gov.tw/en/Content_List.aspx?n=85E9B2CDF4406753. Accessed 14 Nov 2023
Kuo HW, Tsai SS, Tiao MM, Yang CY (2007) Epidemiological features of CKD in Taiwan. Am J Kidney Dis 49:46–55. https://doi.org/10.1053/j.ajkd.2006.10.007
Guh JY, Chen HC, Tsai JF, Chuang LY (2007) Herbal therapy is associated with the risk of CKD in adults not using analgesics in Taiwan. Am J Kidney Dis 49:626–633. https://doi.org/10.1053/j.ajkd.2007.02.259
Jin DC, Yun SR, Lee SW, Han SW, Kim W, Park J, Kim YK (2018) Current characteristics of dialysis therapy in Korea: 2016 registry data focusing on diabetic patients. Kidney Res Clin Pract 37(1):20–29. https://doi.org/10.23876/j.krcp.2018.37.1.20
Loubeau PR, Loubeau JM, Jantzen R (2001) The economics of kidney transplantation versus hemodialysis. Prog Transplant 11:291–297. https://doi.org/10.1177/152692480101100411
Chinese Medical Association. The Clinical Guideline for Organ Transplantation (2010 version). Beijing: People's Medical Publishing House (PMPH). 2010.
Danovitch GM, Delmonico FL (2015) A path of hope for organ transplantation in China? Nephrol Dial Transplant 30:1413–1414. https://doi.org/10.1093/ndt/gfv206
Viklicky O (2020) First registry report on kidney transplantation in China. Transpl Int 33(7):713–714. https://doi.org/10.1111/tri.13590
Wang TH, Lee PC, Chiang YJ (2017) Taiwan’s organ donation and transplantation: observation from national registry point of view. J Formos Med Assoc 116(9):649–651. https://doi.org/10.1016/j.jfma.2017.02.017
Eckhoff DE, Young CJ, Gaston RS, Fineman SW, Deierhoi MH, Foushee MT, Brown RN, Diethelm AG (2007) Racial disparities in renal allograft survival: a public health issue? J Am Coll Surg 204:894–902. https://doi.org/10.1016/j.jamcollsurg.2007.01.024
Axelrod DA, Dzebisashvili N, Schnitzler MA, Salvalaggio PR, Segev DL, Gentry SE, Tuttle-Newhall J, Lentine KL (2010) The interplay of socioeconomic status, distance to center, and interdonor service area travel on kidney transplant access and outcomes. Clin J Am Soc Nephrol 5:2276–2288. https://doi.org/10.2215/CJN.04940610
Kalil RS, Heim-Duthoy KL, Kasiske BL (1992) Patients with a low income have reduced renal allograft survival. Am J Kidney Dis 20:63–69. https://doi.org/10.1016/s0272-6386(12)80318-0
Garg J, Karim M, Tang H, Sandhu GS, DeSilva R, Rodrigue JR, Pavlakis M, Hanto DW, Baird BC, Goldfarb-Rumyantzev AS (2012) Social adaptability index predicts kidney transplant outcome: a single-center retrospective analysis. Nephrol Dial Transplant 27:1239–1245
Taber DJ, Hamedi M, Rodrigue JR, Gebregziabher MG, Srinivas TR, Baliga PK, Egede LE (2016) Quantifying the race stratified impact of socioeconomics on graft outcomes in kidney transplant recipients. Transplantation 100:1550–1557
Butkus DE, Meydrech EF, Raju SS (1992) Racial differences in the survival of cadaveric renal allografts: overriding effects of HLA matching and socioeconomic factors. N Engl J Med 327:840–845. https://doi.org/10.1056/NEJM199209173271203
Moosa MR, Grobbelaar C, Swanevelder SA, EdelsteinC L (1992) The influence of race and the impact of socioeconomic and clinical factors on primary renal allograft survival. Transplant Proc 24:1754–1756
Taylor CB, Ahn D, Winkleby MA (2006) Neighborhood and individual socioeconomic determinants of hospitalization. Am J Prev Med 31(2):127–134. https://doi.org/10.1016/j.amepre.2006.03.025
Executive Yuan, The Republic of China (Taiwan) (2013) The Republic of China yearbook. https://issuu.com/eyroc/docs/rocyearbook_2013. Accessed 13 Nov 2023
Chen CL, Liang CK, Yin CH, Lin YT, Lee CC, Chen NC (2020) Effects of socioeconomic status on Alzheimer disease mortality in Taiwan. Am J Geriatr Psychiatry. 28(2):205–216. https://doi.org/10.1016/j.jagp.2019.06.010. (Epub 2019 Jun 24)
National Statistics Republic of China, 2004. Report on the Survey of Family Income and Expenditure, 2021 (stat.gov.tw).
Taiwan income map (2003) https://kiang.github.io/salary/map. Accessed 14 Jan 2020
Wang JY, Wang CY, Juang SY, Huang KY, Chou P, Chen CW, Lee CC (2014) Low socioeconomic status increases short-term mortality of acute myocardial infarction despite universal health coverage. Int J Cardiol 172:82–87. https://doi.org/10.1016/j.ijcard.2013.12.082
Hall YN, O’Hare AM, Young BA, Boyko EJ, Chertow GM (2008) Neighborhood poverty and kidney transplantation among US Asians and Pacific Islanders with end-stage renal disease. Am J Transplant 8(11):2402–2409. https://doi.org/10.1111/j.1600-6143.2008.02413.x
Goldfarb-Rumyantzev AS, Sandhu GS, Baird BC, Khattak M, Barenbaum A, Hanto DW (2011) Social Adaptability Index predicts access to kidney transplantation. Clin Transplant 25(6):834–842. https://doi.org/10.1111/j.1399-0012.2010.01391.x
Olah ME, Gaisano G, Hwang SW (2013) The effect of socioeconomic status on access to primary care: an audit study. CMAJ 185(6):E263–E269. https://doi.org/10.1503/cmaj.121383
Wood E, Sallar AM, Schechter MT, Hogg RS (1999) Social inequalities in male mortality amenable to medical intervention in British Columbia. Soc Sci Med 48:1751–1758. https://doi.org/10.1016/s0277-9536(99)00081-7
Gray AM (1982) Inequalities in health. The Black Report: a summary and comment. Int J Health Serv 12(3):349–380. https://doi.org/10.2190/XXMM-JMQU-2A7Y-HX1E
Wu MY, Wu MS (2018) Taiwan renal care system: a learning health-care system. Nephrology (Carlton) 23(Suppl 4):112–115. https://doi.org/10.1111/nep.13460
Tsai DF, Huang SW, Holm S, Lin YP, Chang YK (2017) Hsu CC (2017) The outcomes and controversies of transplant tourism-Lessons of an 11-year retrospective cohort study from Taiwan. PLoS ONE 12(6):e0178569. https://doi.org/10.1371/journal.pone.0178569.eCollection
Tsai SF, Lin MH, Hsu CC, Wu MJ, Wang IK, Chen CH (2022) Trends of kidney transplantation from the 2020 annual report on kidney disease in Taiwan. J Formos Med Assoc 121(Suppl 1):S20–S29. https://doi.org/10.1016/j.jfma.2021.12.009
Acknowledgements
The authors express their appreciation to the Department of Medical Education and Research and the Research Center of Medical Informatics at Kaohsiung Veterans General Hospital for their inquiries and assistance with data processing.
Funding
This study was partly supported by the Kaohsiung Veterans General Hospital (Grant nos. VGHKS109-154, KSVGH111-159, and KSVGH111-D08-1). The funders had no role in the study design, data collection and analysis, or decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We do not have any actual or potential conflicts of interest, including any financial, personal, or other relationships with people or organizations.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board Ethics Committee of Kaohsiung Veterans General Hospital (VGHKS18-CT10-07) institution in charge of the studies to confirm that all methods were carried out in accordance with relevant guidelines and regulations. The requirement for informed consent was waived by the KAOHSIUNG V.G.H. Institutional Review Board Ethics Committee because the data were de-identified.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chung, TL., Chen, NC., Yin, CH. et al. The association of socioeconomic status on kidney transplant access and outcomes: a nationwide cohort study in Taiwan. J Nephrol (2024). https://doi.org/10.1007/s40620-024-01928-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40620-024-01928-5