Abstract
Background
Impaired quality of life is common in patients with end-stage kidney disease. We report the baseline quality of life measures in participants from the PIVOTAL randomized controlled trial and the potential relationship with the primary outcome (all-cause mortality, myocardial infarction, stroke, and heart failure hospitalisation), and associations with key baseline characteristics.
Methods
This was a post hoc analysis of 2141 patients enrolled in the PIVOTAL trial. Quality of life was measured using EQ5D index, Visual Analogue Scale, and the KD-QoL [Physical Component Score and Mental Component Score].
Results
Mean baseline EQ5D index and visual analogue scale scores were 0.68 and 60.7 and 33.7 (Physical Component Score) and 46.0 (Mental Component Score), respectively. Female sex, higher Body Mass Index, diabetes mellitus, history of myocardial infarction, stroke or heart failure were associated with significantly worse EQ5D index and visual analogue scale. Higher C-reactive protein levels and lower transferrin saturation were associated with worse quality of life. Haemoglobin was not an independent predictor of quality of life. A lower transferrin saturation was an independent predictor of worse physical component score. A higher C-reactive protein level was associated with most aspects of worse quality of life. Impaired functional status was associated with mortality.
Conclusion
Quality of life was impaired in patients starting haemodialysis. A higher C-reactive protein level level was a consistent independent predictor of the majority of worse quality of life. Transferrin saturation ≤ 20% was associated with worse physical component score of quality of life. Baseline quality of life was predictive of all-cause mortality and the primary outcome measure.
EudraCT registration number
2013-002267-25.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The global prevalence of chronic kidney disease (CKD) is estimated to be 10–13% and increasing; consequently, demand for dialysis services is also likely to increase worldwide [1]. Few large randomized data sets in the last few years have characterized health-related quality of life (QoL) in patients on haemodialysis (HD) using validated metrics. However, from the available data, haemodialysis is associated with impaired QoL and high morbidity and mortality [2].
Quality of life is defined by the World Health Organization (WHO) as “an individual’s perception of their position in life in the context of their values and culture relative to both where they live and their aspirations, ideas, concerns and expectations” [3]. The subjective awareness of each individual of their physical, mental, social and functional well-being is critical to understanding the possible associations of treatments on QoL [4]. Both physical inactivity and impaired physical function as seen during the COVID-19 pandemic are also strongly associated with high morbidity, mortality and reduced QoL in patients on HD [5]. In prevalent haemodialysis patients a low physical component score (PCS) has been associated with increased adjusted rates of death [hazard ratio (HR), 1.55, 95% confidence interval (CI) 1.19–2.03] and hospitalisation (HR, 1.29, 95% CI 1.09–1.54), and a low mental component score (MCS), with increased rates of hospitalisation (HR, 1.39, 95% CI 1.17–1.65) but no association between the symptoms, effects, and burden of kidney disease subscales [6]. There are no data in incident dialysis patients.
The PIVOTAL (Proactive IV irOn Therapy in hemodiALysis) trial investigated the effects of proactive high-dose versus reactive low-dose intravenous (IV) iron in patients in the first year of haemodialysis who were on erythropoiesis-stimulating agent (ESA) therapy. A pre-specified secondary outcome of PIVOTAL was change in QoL measures using the validated European Quality of life 5-dimension score (EQ5D) and kidney disease quality of life (KD-QoL) questionnaires [7, 8]. This is a blunt health status instrument of the perception of health rather than quality of life per se. These scores were measured at baseline and every 3 months for the first year, then every 6 months until the end of the trial. There were no significant between-treatment (proactive high-dose versus reactive low-dose intravenous iron) differences in QoL during the trial but the results were limited by the number of completed questionnaires available during follow-up for analysis. We now report the detailed baseline data, which are not controlled, related to QoL measures in trial participants enrolled in the study [both the higher-dose approach (proactive regimen) and lower-dose approach (reactive regimen)]. We examine the potential relationship of QoL scores with the primary outcome (all-cause mortality, myocardial infarction (MI), stroke, and hospitalisation for heart failure), as well as associations of QoL scores with other key baseline characteristics including clinical and laboratory factors, presence of anaemia, or iron deficiency Specifically, we examined baseline predictors of QoL, as well as the association of haemoglobin and other variables at baseline on QoL scores. We also investigated whether the presence of iron deficiency, irrespective of haemoglobin, influences QoL, and the associations of baseline QoL measures on the primary outcome measure of the trial.
Methods
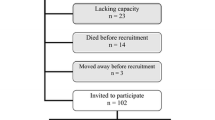
The design, details of baseline characteristics, and the main outcomes of this prospective randomized, controlled study (open-label with blinded end-point evaluation) have been published previously [7, 8]. In brief, a total of 2141 patients with end-stage kidney disease (ESKD) on maintenance haemodialysis initiated ≤ 12 months before randomization were included. At baseline, inclusion criteria included a transferrin saturation (TSAT) < 30% and a ferritin level < 400 ng/mL. Patients were randomized to a proactive regimen of IV (400 mg iron sucrose monthly, with cut-offs to discontinue IV iron therapy if ferritin rose above 700 ng/mL and/or the TSAT increased to over 40%) or to a reactive iron regimen (0–400 mg iron sucrose monthly to maintain a ferritin level of at least 200 ng/mL and a TSAT ≥ 20%). The median cumulative iron dose at one year was 3.8 g in the proactive arm and 1.8 g in the reactive arm. Patients received ESAs at a high enough dose to keep haemoglobin levels between 100 and 120 g/L.
Participants were then requested to complete validated, structured health surveys (EQ5D and KD-QoL). The EQ5D includes overall index and a VAS with a range from 0 to 100, with a higher score indicating better health and 5 separate questions covering mobility, self care, usual activities, pain or discomfort and anxiety/depression. EQ5D has been used in many patient populations including CKD [9, 10]. The KD-QoL is a valid measure of generic but disease-specific health-related QoL scoring system which is separated into 5 subscales consisting of 2 general component summary measures (physical health composite scores (physical functioning (PF) + role physical (RP) + bodily pain (BP) + general health (GH)) and mental health composite scores (vitality (VT) + social functioning (SF) + role emotional (RE) + mental health (MH)). These include eight concept scales which can each be defined as follows; physical functioning—the level of limitation of physical activity caused by health limitations, role-physical—a measure of the limitations of patient-specific physical activity caused by health problems, bodily pain, general health, vitality—measurement of energy and fatigue, social functioning- the level of social life limitations caused by physical and emotional discomfort, role emotional and mental health– the level of psychological stress and well-being. The other 3 subscales consist of kidney disease-targeted specific scores on burden of kidney disease, symptoms of kidney disease and the effects of kidney disease. This score is calculated with norm-based scoring so that 50 is the average score, with higher scores indicating a better QoL [11, 12].
Ethics and regulatory approvals
The trial was conducted in compliance with the principles of the Declaration of Helsinki (1996), the principles of good clinical practice (GCP), and in accordance with all applicable regulatory requirements including, but not limited to the Research Governance Framework and the Medicines for Human Use (Clinical Trial) Regulations 2004, as amended in 2006 and any subsequent amendments. The trial and all elements of the protocol and revised protocols were approved by the South East Coast—Brighton and Sussex Research Ethics Committee (REC number 13/LO/1115), and by the Medicines and Healthcare products Regulatory Agency (MHRA) for Clinical Trial Authorisation.
Written Informed Consent was obtained from eligible patients who had been on haemodialysis for 0–12 months and based on the inclusion, exclusion criteria. Only patients who provided consent were subsequently randomised into the study.
Statistical analysis
Baseline descriptive characteristics and analysis were summarized as means ± standard deviations (SD) for normally distributed data, and medians and inter-quartile ranges for not normally distributed data. Percentages and frequencies were used where appropriate. p-values for between-variable differences based on two sample t-tests, analysis of variance or chi-squared tests/Fisher’s exact tests, as appropriate, are provided. Analyses were performed using SAS software, version 9.4 (SAS Institute), Minitab version 20.3 and R version 3.6.0.
A linear regression model adjusting for significant univariate predictors was used to identify independent predictors of health-related QoL using baseline characteristics and the randomized treatment allocation (proactive high-dose vs reactive low-dose intravenous iron). Time to first event outcomes were analysed using Cox proportional hazards models with estimation of hazard ratios, 95% confidence intervals and p-values from the Wald statistic.
The detailed analysis of QoL data included stratifications based on the following parameters:
-
1.
baseline haemoglobin > 100 g/L vs ≤ 100 g/L
-
2.
serum ferritin > 200 vs ≤ 200 ng/ml
-
3.
TSAT > 20% vs ≤ 20%
-
4.
erythropoiesis-stimulating agent dose (units/week)
-
5.
serum albumin (g/L)
-
6.
sex—males versus females
-
7.
association of social demographic data including age
-
8.
association of aetiology of CKD
-
9.
diabetes vs no diabetes
-
10.
ethnicity
-
11.
vascular access
-
12.
number of comorbidities
Results
Demographic data and disease-related characteristics
The participants’ demographics have been described previously, but in brief a total of 2141 haemodialysis patients (1398 male; 743 female) were randomized, of whom 79% were white, and whose mean age was 62.8 years. At baseline, 41% of patients were dialysed using a central venous catheter while 59% had an arteriovenous graft or fistula. Diabetes was reported to be the cause of ESKD in 587 patients (27.4%). Additional causes of renal disease and co-morbidities are detailed in Table 1, as well as laboratory measurements and ESA doses.
Predictors of the primary endpoint and all-cause mortality
After adjustment for randomized treatment (model 1), then adjusting for other baseline predictive variables (model 2), EQ5D Index (HR: 0.93; 95% CI 0.9–0.97; p < 0.001), EQ5D visual analogue scale (VAS) (0.94: 0.89–0.98; p = 0.006), KD-QoL PCS (0.84: 0.76–0.94) and MCS (0.90: 0.83–0.93) were found to be independently associated with all-cause mortality (Fig. 1). Similar associations were observed for the primary outcome (all-cause death, myocardial infarction, stroke or hospitalisation for heart failure): EQ5D Index (HR 0.93; 95% CI 0.9–0.96; p < 0.001), EQ5D VAS (0.93: 0.87–0.97; p < 0.001), as well as KD-QoL PCS (0.84: 0.77–0.93; p < 0.001) and MCS (0.88: 0.82–0.95; p = 0.0017). There was also an association with symptoms of kidney disease (0.95: 0.90–0.99; p = 0.019) and effects of kidney disease (096: 0.92–1.99; p = 0.046) (Fig. 2).
All-cause mortality forest plot. Model 1 adjusts for randomized treatment group. Model 2 additionally adjusts for log (CRP), albumin, ESA dose, vascular access status, smoking (current former, never), cause of end stage kidney disease (ESKD), age, duration of dialysis and histories (all yes/no) of myocardial infarction (MI), heart failure, atrial fibrillation, peripheral arterial disease and diabetes. PCS physical component score, MCS mental component score. Results are Hazard ratio (HR) and 95% confidence interval (CI). Values for EQ5D index are per 0.1, while all others are per 10
Primary endpoint forest plot (fatal and non fatal myocardial infarction, stroke, hospitalisations for heart failure and all-cause mortality). Model 1 adjusts for randomized treatment group. Model 2 additionally adjusts for log (CRP), albumin, ESA dose, vascular access status, smoking (current former, never), cause of renal disease, age, duration of dialysis and histories (all yes/no) of MI, heart failure, atrial fibrillation, peripheral vascular disease and diabetes. Results are Hazard ratio (HR) and 95% confidence interval (CI). Values for EQ5D index are per 0.1, while all others are per 10
Key laboratory measurements associated with poor QoL were a high CRP level and low TSAT, whilst haemoglobin and ferritin concentrations were not independent predictors of QoL. A low TSAT was an independent predictor of KD-QoL PCS (Suppl Table 2). Variables associated with reduced QoL scores at baseline included age (≤ 65 years) sex (female), BMI (> 27.5), and a history of stroke.
Baseline predictors of quality of life
Variables associated with EQ5D index and EQ5D VAS
At baseline, the mean (SD) EQ5D index overall was 0.68 (0.26) and the mean (SD) overall EQ5D VAS was 60.7 (20.8). In the univariate analysis, being female (p = 0.006 and 0.015), having a higher BMI (p < 0.001: BMI > 27.5) and the presence of more co-morbidities, including diabetes mellitus, a history of MI, stroke or heart failure were associated with significantly worse EQ5D index and EQ5D VAS scores (Table 1 and Suppl Table 1). The lowest scores and hence worse measures were observed in patients with a history of heart failure or stroke. A high CRP level was a consistent association with lower EQ5D index and EQ5D VAS scores.
A Hb level > 100 g/L and TSAT > 20% without raised inflammatory markers (CRP) was associated with better EQ5D index and EQ5D VAS scores in univariable analysis (Table 1). However, after multivariable analysis, haemoglobin was not an independent predictor of any aspect of quality-of-life score at baseline (Suppl Table 4). The variables independently associated with EQ5D index were age, CRP, BMI, sex, heart failure and stroke, and those independently predictive of worse EQ5D VAS score were younger age, higher CRP, female sex and stroke.
Factors associated with KD-QoL PCS and MCS score
At baseline, the mean (SD) PCS overall was 33.7 (10.2) and the mean (SD) overall MCS was 46.0 (11.3). The differences observed across the subgroups examined were qualitatively consistent with those observed for the EQ5D index and EQ5D VAS, although atrial fibrillation was associated with a lower PCS than no atrial fibrillation (Table 2). PCS was substantially lower than MCS in all subgroups examined.
Older age was associated with a better MCS score. After adjustment, a history of stroke (p = 0.048) and myocardial infarction (p = 0.01) remained independent predictors of a worse MCS, while transferrin saturation (of > 20%) was a strong independent predictor of a better PCS score (p = 0.005) (Suppl Table 2). Serum ferritin had no independent effect on QoL scores in any domain analysed (Suppl Table 3).
Factors associated with KD-QoL eight constitute domains analysis of PCS and MCS
Overall scores for RP and RE were much lower than other domains, while PF was lower than the others. Further comparative statistical analysis of the 8 domains of the KD-QoL scores demonstrated higher scores in PF, BP, GH, and VT in males compared to females (p < 0.01; < 0.01; < 0.012 and < 0.003, respectively) (Suppl Table 4). Higher CRP was associated with lower scores on all 8 subdomains including age, sex, BMI, comorbidities of diabetes, stroke and heart failure. In univariate analysis a low haemoglobin level and low TSAT were associated with the domains BP, GH, and social functioning (SF), (Suppl Table 4).
Factors associated with kidney-specific scales: KD-Qol Burden, Symptoms and Effects of kidney disease subscales
The comparative statistical analysis of the scores of KD-QoL burden, symptoms and effects of kidney disease according to the categorical socio-demographic variables and categorical clinical and laboratory parameters are shown in Suppl Table 5. The findings related to burden, symptoms and effects again indicated that males (p = 0.004, 0.046, 0.005, respectively, for burden, symptoms and effects) were independently less affected; the presence of diabetes led to significantly worse scores in all 3 domains (p < 0.001) and the presence of co-morbidities was less important. A higher CRP was again an important significant independent predictive factor of burden (p = 0.001), symptoms (p = 0.004) and effects (p = 0.04) (Suppl Table 5). A low haemoglobin level was associated with increased burden but not symptoms or effects of renal disease.
Discussion
In this post hoc analysis of a large cohort of patients within the first year of commencing haemodialysis in the UK, overall QoL scores were 30% lower than the general population and similar to those found in prevalent dialysis patients, approximately 10% lower than patients on peritoneal dialysis and approximately 12% lower in comparison to kidney transplant patients with regard to the PCS [6, 13, 14]. Specific reductions were seen in our cohort in the subdomains of physical function, role physical and role emotional but not renal-specific subdomains. A worse QoL at baseline was influenced by several parameters, the most consistent independent variable being a high CRP level. Our study showed that at baseline these factors were consistent across several QoL scores, and baseline QoL was predictive of all-cause mortality and the primary outcome measure. This has not been previously studied in patients within the first year of haemodialysis.
In patients with chronic kidney disease not on dialysis, scores tend to be higher and associations exist with hospitalisations. There were strikingly low scores for heart failure and stroke which is not surprising given their association on health. In the Therapeutic Response Evaluation and Adherence Trial (TREAT) trial in patients with CKD and type 2 diabetes, treatment with darbepoetin led to a small improvement in fatigue and overall QoL over placebo, although there was no benefit on other domains [15]. Despite finding in this study that low transferrin saturation or haemoglobin was predictive of poor QoL, the subsequent follow-up data on proactive versus reactive iron did not show any significant benefit which might relate in part to the quantity of missing follow-up data, hence this was not addressed in this current study. Also the lack of association, after adjustment, between a higher haemoglobin level and better measures of health status or quality of life may be due to the relatively small range of haemoglobin seen in the study leading to relatively small corrections in haemoglobin.
Use of the disease-specific elements of the KD-QoL did not add any further information to the generic scores. These again were approximately 15% lower than those in transplant patients but higher than those in prevalent dialysis patients [13, 14].
Our data confirmed that both the PCS component and the MCS component of QoL is lower in the elderly and is associated with death and hospitalisation regardless of demographic data [16]. They were also associated with the composite outcome of all-cause death, myocardial infarction, stroke or hospitalisation for heart failure. Quality of life was an independent prognostic predictor and was associated with mortality, consistent with other studies [15], and increased hospitalisations [17, 18]. Indeed, impaired functional status is associated with early death after commencement of haemodialysis. [19, 20]. Our patient group included incident patients, some of whom would have been in the first three months of dialysis and therefore this may have influenced the association. However, with such a large data set of over 2000 dialysis patients the results remain important and warrant consideration of methods of intervention to reduce the future impact. Both physical inactivity and impaired physical function are strongly associated with increased morbidity, mortality and reduced QoL. Reduced QoL is also independently associated with mortality in patients on haemodialysis [5].
Male patients had better QoL scores, especially for KD-QoL burden, symptoms and effects, but age had less of an association. This was seen in a previous systematic review and meta-analysis and analysis of the Dialysis Outcomes and Practice Patterns Study (DoPPS) data [21, 22]. Chesnaye and colleagues in a recent analysis in patients with advanced chronic kidney disease also noted this association and provided several possible explanations including reduced reporting of physical weakness by men, the applications of different coping strategies, the different perceptions of symptom severity and the higher rates of depression and anxiety in women [23]. A recent analysis of the DoPPS data concerning dialysis patients in Japan found that in 892 maintenance HD patients, those > 70–79 years or > 80 years had lower PCS scores compared to those aged > 60 years (43.1 vs 35.2) [24]. Again in a population of 980 dialysis patients in Singapore, age and male sex had higher scores [13]. Interestingly, in our population, the scores were much lower (34.4 vs 33.6) and were not significantly different. In addition, whereas there was a significant difference in MCS scores in our study which was better in the older age group, Ishiwatari et al. [24] did not find a significant difference in their population of Japanese patients. The reasons for this are unclear but may relate to the age differences examined or cultural differences between the two populations.
Our patient population was identified on the basis of laboratory biomarkers of anaemia and iron deficiency. Both Hb and TSAT led to a statistically significant difference in QoL, with a higher Hb and higher TSAT reflecting better baseline QoL scores for EQ5D index and EQ5D VAS, and amongst the KD-QoL scores, BP,GH, and SF but not VT or PF as seen in other studies of patients with CKD or on dialysis therapy [25,26,27,28,29,30]. However, after analysis for independent variables, only a lower TSAT was an independent predictor of worse QoL for PCS. It may be that TSAT is a better predictor of functional iron deficiency which is associated with functional capacity and possible fatigue scores [31,32,33,34]. The TREAT study led to an improvement in The Functional Assessment of Cancer Therapy-Fatigue (FACT-Fatigue) score in these studies with ESA therapy [15, 35], while the Correction of Hemoglobin Outcomes in Renal Insufficiency Study (CHOIR) demonstrated an improvement in the linear analogue scale assessment in both groups (higher and lower Hb groups) and a trend for increased energy scores in the lower Hb group [36, 37]. However, there was no difference in the KD-QoL scores of energy or physical functioning domains in these studies [15, 35,36,37]. TREAT demonstrated that a 5 point or greater increase in score was clinically meaningful, leading to better outcomes (54% in the ESA group vs 49% in the placebo group; p = 0.027). Our study showed that QoL scores, independent of Hb or iron status at baseline, were predictive of mortality and the primary outcome measure. This finding is perhaps important when considering those patients commencing dialysis therapy, at least in the UK. It would suggest that lower QoL scores are perhaps simply a marker of bad outcomes. Whether trying to improve these factors which affect quality of life, such as anaemia and iron deficiency, prior to commencing dialysis with maximization of preventative therapies to minimize cardiovascular risk (reducing lipids, glycemic control) may impact Quality of life or mortality on dialysis is unknown. In addition, consideration of dialysis therapy itself and strategies such as incremental dialysis which impact patient wellbeing also remains unknown [38, 39].
There have been recent developments in assessing patient-related outcomes measures both generally in patients with CKD and specifically in those with associated anaemia, nonetheless, several of these developments require validation. Health-related QoL represents a patient’s overall perception of the effect of disease and treatment on their QoL, thus measures of health-related QoL are often measures of self-perceived health status. Such measures do not directly capture how patients feel and function. Assessment of patient well-being is valuable for optimal patient care. The SF-36 questionnaire has been widely used to evaluate the impact of anaemia in CKD trials and the vitality domain has been shown to correlate with Hb level and to be beneficially affected by treatment [40]. The Physical function scales and the FACIT-An Total, Fatigue and Anaemia scales, are also reliable and valid measures for assessing health-related quality of life in anaemia associated with CKD [41]. Patient reported outcome measures are being developed [42, 43]. However, the chronic kidney disease Anaemia Questionnaire (CKD-AQ) is the latest advance and appears to be a reliable and sound patient-related outcome measure for use in patients with anaemia of CKD [44]. The objectives of the CKD-AQ questionnaire are to assess the frequency, duration and severity of symptoms and impact associated with anaemia in CKD.
Our study has several strengths and limitations. This was a large study encompassing a diverse real world UK dialysis population with good baseline data collection. However, a prospective analysis of QoL over time was futile due to the volume of missing data. Another possible limitation is the lack of collection of socio- economic level data which has been previously shown to be associated with outcomes [45]. Ferritin was not adjusted for CRP and hence it cannot be said that this is not an explanation for the lack of association of ferritin with QoL. Other possible variables that could have influenced the outcomes and QoL, such as the impact of central venous catheter vs arteriovenous fistula or dialysis adequacy, were not studied in the current model. In addition, it is recognised that within the first three months of commencing dialysis, patients have worse quality of life measures and outcomes; this was not included in the modeling.
A final consideration is that health-related QoL is a term that is commonly and misleadingly used to refer to health status tools such as the KD-QoL and EQ-5D, which may assess health and functioning but do not assess the association of health and functioning on QoL [46, 47]. Health status includes aspects of a person’s life such as their physical ability, daily functioning, and experience of symptoms. Indeed, it is controversial whether these health-status measures should be considered measures of quality of life at all [46]. Therefore, assumptions about the overall quality of life of individual patients should not be based on measures of their health status alone.
Conclusions
Overall, we have shown that in the first year of commencing haemodialysis, baseline QoL is predictive of mortality and the primary outcome measure of the PIVOTAL trial. Several factors influence a poorer quality of life score including female gender, the presence of diabetes and other co-morbidities. Markers of iron deficiency (a low TSAT) and inflammation (a high CRP) were also associated with poorer outcomes in many domains of QoL. Possible earlier optimization of patients (such as reducing cardiovascular risk factors, diabetes control, correcting iron deficiency and lifestyle changes) prior to commencement of dialysis so as to tackle those modifiable factors associated with poor QoL scores needs attention to potentially reduce future mortality.
Data availability
The data associated with the paper are not publicly available but are available from the Glasgow clinical trials unit on reasonable request with the relevant permissions and agreement of Kidney Research UK and Kings College Hospital that served as the sponsor for the study.
References
Himmelfarb J, Vanholder R, Mehrotra R et al (2020) The current and future landscape of dialysis. Nat Rev Nephrol 16:573–585
Jha V, Wang AY-M, Wang HY (2012) The impact of CKD identification in large countries: the burden of illness. Nephrol Dial Transplant 27(suppl 3):32–38
The World Health Organization Quality of Life Assessment (1998) (WHOQOL): development and general psychometric properties. Soc Sci Med 46:1569–1585
Callahan D, The WHO (1973) Definition of health. Hastings Center Stud 1(3):77–87
Baiardi F, Esposit ED, Cocechi R, Fabri A, Sturani A, Valpiani G et al (2002) Effects of clinical and individual variables on quality of life in chronic renal failure patients. J Nephrol 15(1):61–67
Hall RK, Luciano A, Pieper C, Colón-Emeric CS (2018) Association of Kidney Disease Quality of Life (KDQOL-36) with mortality and hospitalization in older adults receiving hemodialysis. BMC Nephrol 19:11. https://doi.org/10.1186/s12882-017-0801-5
Macdougall IC, White C, Anker SD, Bhandari S, Farrington K, Kalra PA, McMurray JJ, Murray H, Steenkamp R, Tomson CRV, Wheeler CD, Winearls CG, Ford I on behalf of the PIVOTAL Study investigators (2019) Randomised controlled trial comparing high-dose versus low-dose intravenous iron supplementation in haemodialysis (PIVOTAL). N Engl J Med 380(5):447–458
Macdougall IC, White C, Anker SD, Bhandari S, Farrington K, Kalra PA, McMurray JJ, Murray H, Steenkamp R, Tomson CRV, Wheeler CD, Winearls CG, Ford I on behalf of the PIVOTAL Study investigators (2018) Randomised controlled trial comparing high-dose versus low-dose intravenous iron supplementation in haemodialysis (PIVOTAL): rationale, study design, and baseline data. Am J Nephrol 48(4):260–268
Brazier J, Jones N, Kind P (1993) Testing the validity of the Euroqol and comparing it with the SF-36 health survey questionnaire. Qual Life Res 2:169–180
Williams A, Buxton M, O’Hanlon M, Rushby J, Pekurinen M, Sintonen H, Bjork S, Lindgren B, Perrson U, Brooks R, Nord E, Allison R, Butler C, Rabin R, Rosser R, Selai C, Bonsel G, Essink-Bot ML, van Hout B, deCharro F, Gudex C, Kind P (1990) EuroQol: a new facility for the measurement of health-related quality of life. The EuroQol Group. Health Policy 16:199–208
Manns BJ, Johnson JA, Taub K, Mortis G, Ghali WA, Donaldson C (2002) Dialysis adequacy and health related quality of life in hemodialysis patients. Asaio J 48:565–569
Brazier JE, Harper R, Jones NM, O’Cathain A, Thomas KJ, Usherwood T, Westlake L (1992) Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ 305:160–164
Joshi VD, Mooppl V, Lim J (2010) Validation of the Kidnet Disease Quality of life Short Form: a cross sectional study of a dialysis-targeted health measure in Singapore. BMC Nephrol 11:36
Czyzewki L, Sacko-Rimer J, Wyzzet S, kwowski A (2014) Assessment of HRQoL of patients after kidney transplantationin comparison to haemodialysis and peritoneal dialysis. Ann Transplant 70:576–585
Lewis EF, Pfeffer MA, Feng A, Uno H, McMurray JJV, Toto R, Gandra SR, Solomon SD, Moustafa M, Macdougall IC, Locatelli F, Parfrey S, for the TREAT Investigators (2011) Darbepoetin alfa impact on health status in diabetes patients with kidney disease: a randomized trial. Clin J Am Soc Nephrol 6:845–855
Mapes DL, Lopes AA, Satayathum S, Cullough KP, Goodkin DA, Locatelli F et al (2003) Health-related quality of life as a predictor of mortality and hospitalization: the Dialysis Outcomes and Practice Patterns Study (DOPPS). Kidney Int 64(1):339–349
Lowrie EG, Curtin RB, LePain SD (2003) Medical outcomes study short form-36: a consistent and powerful predictor of morbidity and mortality in dialysis patients. Am J Kidney Dis 41(6):1286–1292
Perl J, Karaboyas A, Morgenstern H, Sen A, Rayner HC, Vanholder RC et al (2017) Association between changes in quality of life and mortality in hemodialysis patients: results from the DOPPS. Nephrol Dial Transplant 32(3):521–527
kalantar Zadeh K, Kopple J, Block G, Humohreys MH (2002) Association among SF36 quality of life measures and nutrition, hospitalization, and mortality in hemodialysis. J Am Soc Nephrol 12(12):2797–2806
Kurella Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE (2001) Functional status of elderly adults before and after initiation of dialysis. N Engl J Med 361(16):1539–1547
Liem YS, Bosch JL, Hunink MM (2008) Preference-based quality of life of patients on renal replacement therapy: a systematic review and meta-analysis. Value Health 11:733–741
Lopes AA, Bragg-Gresham JL, Goodkin DA, Fukuhara S, Mapes DL, Young EW, Gillespie BW, Akizawa T, Greenwood RN, Andreucci VE, Akiba T, Held PI, Port FK (2007) Factors associated with health-related quality of life among hemodialysis patients in the DOPPS. Qual Life Res 16:545–557
Dhesnaye NC, Meuleman Y, de Rooij ENM, Hoogeveen EK, Dekker FW, Evans M, Pagels AA, Caskey FJ, Tornio C, Porto G, Szymczak M, Drechsler C, Wanner C, Jager KJ, the EQUAL Study Investigators (2022) Health-related Quality-of-life trajectories over time in older men and women with advanced chronic kidney disease. Clin J Am Soc Nephrol 17:205–214
Ishiwatari A, Yamamoto S, Fukuma S, Hasegawa T, Wakai S, Nangaku M (2020) Changes in quality of life in older hemodialysis patients: a cohort study on dialysis outcomes and practice patterns. AM J Nephrol 51:650–658
Dowling TC (2007) Prevalence, etiology, and consequences of anemia and clinical and economic benefits of anemia correction in patients with chronic kidney disease: an overview. Am J Health Syst Pharm 64(13 Suppl 8):S3-7 (4)
Perlman RL, Finkelstein FO, Liu L et al (2005) Quality of life in chronic kidney disease (CKD): a cross-sectional analysis in the renal research institute-CKD study. Am J Kidney Dis 45:658–666
Mujais SK, Stor K, Brouillette J, Takano T, Soroka S, Franek C, Mendelssohn D, Frederic O (2009) Health-related quality of life in CKD patients: correlates and evolution over time. Clin J Am Soc Nephrol 4:1293–1301
Kimel M, Leidy NK, Mannix S, Dixon J (2008) Does epoetin alfa improve health-related quality of life in chronically ill patients with anemia? Summary of trials of cancer, HIV/AIDS, and chronic kidney disease. Value Health 11:57–75
Leaf DE, Goldfarb DS (2009) Interpretation and review of health-related quality of life data in CKD patients receiving treatment for anemia. Kidney Int 75:15–24
Drüeke TB, Locatelli F, Clyne N et al (2006) Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med 355:2071–2084
Bhandari S, Kalra P, Berkowitz M, Belo D, Thomsen LL, Wolf M (2021) Safety and efficacy of iron isomaltoside 1000/ferric derisomaltoside veruss iron sucrose in patients with chronic kidney disease: the FERWON-NEPHRO randomized, open-label, comparative trial. Nephrol Dial Transplant 36(1):111–120
Kassianides X, Gordon A, Sturmey R, Bhandari S (2021) The comparative effect of intravenous iron on oxidative stress and inflammation in patients with Chronic kidney Disease (CKD). A randomized controlled-plot study. Kidney Res Clin Pract. 40(1):89–98
Bhandari S, Allgar V, Lamplugh A, Macdougall I, Kalra PA (2021) A multicentre prospective double blinded randomised controlled trial of intravenous iron (Ferric Derisomaltose (FDI)) in Iron deficient but not anaemic patients with Chronic Kidney Disease on functional status. BMC Nephrol 22:115
Finkelstein FO, van Nooten F, Wiklund I, Trundell D, Cella D (2018) Measurement properties of the Short Form-36 (SF-36) and the Functional Assessment of Cancer Therapy-Anemia (FACT-An) in patients with anemia associated with chronic kidney disease. Health Qual Life Outcomes 16:111
Besarab A, Bolton WK, Browne JK, Egrie JC, Nissenson AR, Okamoto DM, Schwab SJ, Goodkin DA (1998) The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med 339:584–590
Singh AK, Szczech L, Tang KL, Barnhart H, Sapp S, Wolfson M, Reddan D (2007) Anaemia of CKD—the CHOIR study revisited. Nephrol Dial Transplant 22(7):1806–1810
Singh AK, Szczech L, Tang KL, Barnhart H, Sapp S, Wolfson M, Reddan D, Investigators C (2006) Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med 355:2085–2098
Hazara AM, Bhandari S (2020) Early mortality rates after commencement of maintenance haemodialysis: a systematic review and meta-analysis. Ther Apher Dial 24(3):275–284
Hazara AM, Bhandari S (2019) Can incremental hemodialysis reduce early mortality rates in patients starting maintenance hemodialysis? Curr Opin Nephrol Hypertens 28(6):641–647
van Haalen H, Jackson J, Spinowitz B, Milligan G, Moon R (2020) Impact of chronic kidney disease and anemia on health-related quality of life and work productivity: analysis of multinational real-world data. BMC Nephrol 21(1):88
Finkelstein FO, van Nooten F, Wiklund I, Trundell D, Cella D (2018) Measurement properties of the Short Form-36 (SF-36) and the Functional Assessment of Cancer Therapy - Anemia (FACT-An) in patients with anemia associated with chronic kidney disease. Health Qual Life Outcomes 16(1):111
Mathias SD, Blum SI, Sikirica V, Johansen KL, Colwell HH, Okoro T (2020) Symptoms and impacts in anemia of chronic kidney disease. J Patient Rep Outcomes 4(1):64
Parfrey PS, Foley RN, Wittreich BH, Sullivan DJ, Zagari MJ, Frei D (2005) Double-blind comparison of full and partial anemia correction in incident hemodialysis patients without symptomatic heart disease. J Am Soc Nephrol 16(7):2180–2189
Keeley T, Chen WH; Refoios C et al. Psychometric properties of the SF-36 vitality scale in patients with anemia of chronic kidney disease. (Abstract P0660 presented at ASN 2022)
Braga SFM, Peixoto SV, Gomes IC, Acúrcio FdA, Andrade EIG, Cherchiglia ML (2011) Factors associated with health-related quality of life in elderly patients on hemodialysis. Rev Saude Publ 45(6):1127–1136
Bradley C (2001) Importance of differentiating health status from quality of life. Lancet 357:7–8
Covinsky KE, Wu AW, Landefeld CS, Connors AF Jr, Phillips RS, Tsevat J, Dawson NV, Lynn J, Fortinsky RH (1999) Health status versus quality of life in older patients: does the distinction matter? Am J Med 106(4):435–440
Acknowledgements
We would like to thank all the participants of the study.
Funding
The PIVOTAL study received funding from Kidney Research UK via an unrestricted grant from Vifor Fresenius Medical Care Renal Pharma. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Consortia
Contributions
SB participated in all aspects of the study including the study trial design, part of the trial steering committee, prepared the first draft of the manuscript and critically reviewed all subsequent drafts of the manuscript and the final manuscript for submission; PP assisted in review of concept and critically reviewed manuscript; CW Steering Committee and critical review of the manuscript; SDA Steering Committee, trial design, and critical review of the manuscript; KF Steering Committee and critical review of the manuscript; IF Steering Committee, trial design and performed the statistical analysis and critically reviewed the manuscript; PAK Steering Committee and critical review of the manuscript; JJVM Steering Committee and critical review of the manuscript; MR Statistical analysis and critical review of the manuscript; CRVT Steering Committee and critical review of the manuscript; DCW Steering Committee and critical review of the manuscript; ICM Chief Investigator, Steering Committee, trial design, and critical review of the manuscript. The order of authorship was a joint decision of the co-authors based on alphabetical order, with SB as first, main author and corresponding author and ICM as a senior author.
Corresponding author
Ethics declarations
Conflict of interest
SB has received honorarium for lectures, attended expert opinion committees and received educational funds to attend international Nephrology meetings from Pharmacosmos A/S and Vifor Pharma, Astellas, Bayer, Pfizer and GSK; PP has no conflicts of interest; CW has no conflicts of interest; SDA has received grants from Vifor Pharma and Abbott Vascular, and fees for consultancy from Vifor Pharma, Bayer, Boehringer Ingelheim, Novartis, and Servier; KF has no conflicts of interest; IF has received research grants from Vifor Pharma and Pharmacosmos; PAK has received speaker fees, honoraria, and consultancy fees from Pharmacosmos, Vifor Pharma, and Takeda. D.C.W. has received honoraria and consultancy fees from Amgen, Akebia, AstraZeneca, Bayer, Boehringer Ingelheim, Janssen, Napp, and Vifor Fresenius Medical Care; JJVM reports receiving fees (all fees from Bayer, fees for serving on a steering committee, fees for serving on an endpoint committee, and travel support from Cardiorentis, fees for serving on a steering committee and travel support from Amgen, fees for serving on a steering committee and travel support from Oxford. University–Bayer, fees for serving as principal investigator of a trial and travel support from Theracos, fees for serving on a steering committee and travel support from AbbVie, fees for serving on a steering committee from DalCor Pharmaceuticals, fees for serving on a data and safety monitoring committee from Pfizer, fees for serving on a data and safety monitoring committee from Merck, fees for serving on an executive committee, fees for serving as co-principal investigator of a trial, fees for serving on a steering committee, fees for serving on an executive committee, travel support, and advisory board fees from Novartis, fees for serving as co-principal investigator for a trial, fees for serving on a steering committee, and travel support from GlaxoSmithKline, fees for serving on a steering committee from Bristol-Myers Squibb, and fees for serving on a steering committee, fees for serving on an endpoint adjudication committee, and travel support from Vifor Pharma–Fresenius; MR has no conflicts of interest; CRVT has no conflicts of interest; DCW has received honoraria and consultancy fees from Amgen, Akebia, AstraZeneca, Bayer, Boehringer Ingelheim, Janssen, Napp, and Vifor Fresenius Medical Care; ICM has received speaker fees, honoraria, and consultancy fees from several ESA and IV iron manufacturers, including Akebia, AMAG, Astellas, Bayer, FibroGen, GlaxoSmithKline, Pharmacosmos, and Vifor Pharma.
Ethical statement
The trial was conducted in compliance with the principles of the Declaration of Helsinki (1996), the principles of good clinical practice (GCP), and in accordance with all applicable regulatory requirements including but not limited to the Research Governance Framework and the Medicines for Human Use (Clinical Trial) Regulations 2004, as amended in 2006 and any subsequent amendments. The trial and all elements of the protocol and revised protocols were approved by the South East Coast - Brighton and Sussex Research Ethics Committee (REC number 13/LO/1115), and to the Medicines and Healthcare products Regulatory Agency (MHRA) for Clinical Trial Authorisation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bhandari, S., Parfrey, P., White, C. et al. Predictors of quality of life in patients within the first year of commencing haemodialysis based on baseline data from the PIVOTAL trial and associations with the study outcomes. J Nephrol 36, 1651–1662 (2023). https://doi.org/10.1007/s40620-023-01571-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-023-01571-6