Abstract
Introduction
Little is known about the comparative effects of sodium glucose cotransporter-2 inhibitors (SGLT2i), glucagon-like peptide-1 receptor agonists (GLP1-RA), or dipeptidyl peptidase-4 inhibitors (DPP-4i) on the risk of acute kidney injury (AKI) in routine care, which may differ from the controlled setting of trials.
Methods
Observational study comparing risks of AKI among new users of SGLT2i, GLP1-RA or DPP-4i in the region of Stockholm, Sweden, during 2008–2018. AKI was defined by ICD-10 codes and creatinine-based KDIGO criteria. We used inverse probability of treatment weighting (IPTW) to adjust for 60 potential confounders, weighted Kaplan–Meier curves and Cox regression to estimate hazard ratios and absolute risks.
Results
We included 17,407 participants who newly initiated DPP-4i (N = 10,605), GLP1-RA (N = 4448) or SGLT2i (N = 2354). Mean age was 63 years (39% women) and median (IQR) eGFR was 89 (73–100) ml/min/1.73 m2. During a median follow-up of 2.5 years, 1411 participants experienced AKI. SGLT2i users had the lowest incidence rate of AKI, 18.3 [CI 95% 14.1–23.4] per 1000 person years, followed by GLP1-RA (22.5; 19.9–25.3) and DPP-4i (26.6; 25–28.2). The weighted 3-year absolute risk for AKI was 5.79% [3.63–8.52] in the SGLT2i group, compared with 7.03% [5.69–8.69] and 7.00% [6.43–7.58] in the GLP1-RA and DPP-4i groups, respectively. The adjusted hazard ratio was 0.73 [CI 95% 0.45–1.16] for SGLT2i vs. DPP-4i, and 0.98 [CI 95% 0.82–1.18] for GLP1-RA vs. DPP-4i.
Conclusion
This study of routine care patients initiating novel glucose-lowering drugs showed similar occurrence of AKI between therapies, and suggests lower risk for SGLT2i.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus type 2 (T2DM) is a global health problem with a high risk of complications and death [1]. Sodium glucose cotransporter-2 inhibitors (SGLT2i) are novel oral diabetes medications that, in addition to glucose lowering effects, have been shown in clinical trials to reduce the risk of hospitalization for heart failure, kidney disease progression, kidney failure, death from renal or cardiovascular causes, and all-cause mortality [2,3,4,5,6,7]. On the basis of these trials, clinical guidelines recommend administering SGLT2i in addition to metformin to patients with or at high risk for atherosclerotic cardiovascular disease, those with clinical heart failure, and those with chronic kidney disease (CKD) [8, 9].
There is often an acute drop in estimated glomerular filtration rate (eGFR) during the first weeks of SGLT2i therapy, [4] which may lead to acute kidney injury (AKI) [10]. A review of more than 100 spontaneous reports of confirmable cases of AKI related to SGLT2i led the US Federal Drug Administration (FDA) to issue a warning in December 2015 stating that SGLT2 inhibitors might cause AKI [11]. The FDA recommended following and quantifying this risk in post-marketing surveillance studies [10, 11].
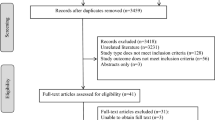
Case reports contrast with trial data: a recent network meta-analysis of RCTs indicates that SGLT2 inhibitors may have a lower AKI risk compared with dipeptidyl peptidase 4 (DPP-4) inhibitors and glucagon-like peptide 1 receptor agonists (GLP-1RAs) [12]. However, in these trials, AKI was documented as an adverse event rather than a prespecified outcome, and the strict inclusion/exclusion criteria alongside stringent monitoring protocols may have led to an underestimation of adverse event rates. In the heterogeneous setting of routine clinical practice, various North American studies have reported similar AKI event rates among new users of SGLT2i compared to other oral diabetes medications [13,14,15]. However, the family of oral diabetes medications is heterogeneous, and risks may be better ascertained through comparative safety analyses. Three studies have compared AKI risks of SGLT2i versus DPP-4 inhibitors and GLP-1RAs, observing either no difference between therapies, [16] or a lower AKI risk for SGLT2i [17, 18]. Identified limitations for these studies include the use of administrative codes to identify AKI, which are insensitive, lack information on baseline eGFR, which may modulate subsequent AKI risks, and restrictions by certain health insurance companies, or to persons older than 65 years. Replication of consistent adverse drug event relationships across geographically distinct health systems and variations in prescribing practices may provide greater confidence in results. Against this background, we conducted an observational study comparing risks of AKI among routine care users of novel glucose-lowering drugs in Stockholm (Fig. 1).
Cumulative incidence curve, overall and with the Y axis magnified. Kaplan–Meier plots for weighted cumulative incidence of acute kidney injury (AKI) stratified by DPP-4i, GLP1-RA or SGLT2i treatment. Light-colored areas represent 95% confidence intervals. X axis truncated at 5.5 years. DPP-4i dipeptidyl peptidase-4 inhibitor, GLP1-RA glucagon-like peptide-1 receptor agonist, SGLT2i sodium-glucose cotransporter-2 inhibitor (color figure online)
Materials and methods
Data source
The study population was derived from the Stockholm CREAtinine Measurements (SCREAM) project, a health care utilization cohort that includes all residents of the region of Stockholm, Sweden, between 2006–2019 [19]. In 2019, the region had a population of approximately 2.3 million citizens, to whom a single unified health system provides universal health care access. Using the unique personal identification number of each Swedish resident, administrative databases containing extensive information on demographics, health care utilization and comorbidities, laboratory test results and drug dispensation records were linked, thereby providing comprehensive structured health records.
Study design
We included any adult (age ≥ 18 years old) residing in Stockholm with a clinical diagnosis of diabetes, who newly initiated SGLT2i, GLP1-RA or DPP-4i therapy between 2008-01-01 and 2018-12-31. We established that the patient should have had at least one outpatient serum/plasma creatinine test in the year prior to therapy start to calculate his/her kidney function (Supplemental Figure S1). The date of treatment initiation was defined as the index date and start of follow-up. Then, we excluded patients with type 1 or gestational diabetes mellitus, as well as those with previous history of AKI (by issued clinical diagnosis), with eGFR < 15 ml/min/1.73 m2, on dialysis treatment or that had a history of kidney transplantation.
Exposure and covariates
The study exposure was new initiation of SGLT2i, GLP1-RA or DPP-4i therapy, defined as the first dispense during the study period with an absence of any dispensation of the drugs of interest over the previous 12 months. We did not consider treatment switches during follow-up, if any, in the analysis. We extracted information at index date for 60 covariates including demographics (age and sex, year of therapy start and highest attained level of education), laboratory tests (eGFR and HbA1c), history of comorbidities, ongoing medications, and recent healthcare utilization. eGFR was calculated using routine ambulatory isotope-dilution-mass-spectrometry–traceable plasma creatinine measurements and applying the 2009 CKD-EPI equation without correction for race [20]. eGFR at baseline was defined as the average of all outpatient creatinine measurements performed in the preceding 12 months and categorized as per KDIGO criteria in stages of G severity [21]. To capture healthcare utilization and disease severity, we also considered the number of overall and disease-specific outpatient/inpatient encounters in the 12 months prior to the index date. Defining algorithms are detailed in Supplemental Table S1.
Study outcome
The study outcome was the occurrence of AKI during follow-up. AKI was identified by a combination of diagnoses (ICD-10 code N17) in outpatient or hospital care, the need for acute renal replacement therapy, and transient creatinine elevations during hospitalization according to KDIGO criteria [22] (increase in creatinine ≥ 26 μmol/l over 48 h or ≥ 1.5 times within 7 days). We defined the “baseline” creatinine as the mean of the last outpatient creatinine measurements 7–365 days prior to hospital admission. Definitions are detailed in Supplemental Table S2. Patients were followed until occurrence of AKI, death, emigration from the region or administrative censoring on 2018–12-31. There was no loss to follow-up.
Statistical analyses
Categorical variables were reported as frequencies and percentages. Continuous variables were reported as median with interquartile range (IQR). There were no missing data in any of the covariates assessed, except for attained level of education, which was missing in < 3% of participants. Due to the low amount of missingness, we treated “missingness” as a separate category for this variable in the analysis.
We used inverse probability of treatment weighting (IPTW) to control for baseline confounding [23]. We estimated the probability of receiving GLP1-RA or SGLT2i versus DPP-4i (reference) as a function of the baseline covariates listed above using a multivariable logistic regression model. Weighting was considered appropriate if the standardized mean difference (SMD) between treatment groups was < 0.1. Weights were stabilized to increase precision by adding the marginal probability of treatment to the numerator of the weights.
We first estimated the total number of events and incidence rates for each group without weighting. We then used weighted Cox regression to estimate hazard ratios (HR) and 95% confidence intervals (95% CI) between treatment groups, with time since initiation as the underlying time scale. In order to compare outcome rates between SGLT2i and GLP1-RA, we additionally repeated the weighting with GLP1-RA as the reference. Covariates that did not achieve balance after IPTW were controlled for by adding them as covariates to the model.
Weighted Kaplan–Meier curves were plotted to display the cumulative incidence of outcomes over the follow-up period for each medication. We then obtained weighted absolute risks and risk differences and used a bootstrap resampling technique to construct 95% confidence intervals, using 1000 samples [24]. As a sensitivity analysis, we tested the robustness of IPTW weighting by comparing against an alternative method of overlapping weights [25]. All the analyses were performed using R statistical software.
Results
We included 17,407 participants who met the inclusion and exclusion criteria (Figure S1). Of these, 10,605 initiated DPP-4i treatment (61%), 4448 initiated GLP1-RA (26%) and 2354 initiated SGLT2i (13%). Overall, mean age was 62.8 years, 61% were male and median (IQR) eGFR was 89 (73–100) ml/min/1.73m2. Unweighted characteristics by treatment group are shown in Supplemental Table S3. In brief, DPP-4i users were generally older and with a slightly lower median eGFR level than participants who started on GLP1-RA or SGLT2i. Users of SGLT2i (of whom 59% started on empagliflozin, 40.5% on dapagliflozin, and < 1% on canagliflozin) included a higher proportion of men and with cardiovascular comorbidities, mainly history of ischemic events. There were no major differences in baseline HbA1c between groups, but patients on GLP1-RA tended to have a higher proportion of concomitant insulin treatment. After weighting, most covariates achieved balance (shown in Table 1 with additional covariates listed in Tables S3 and S4), except for calendar year and CKD stage.
During a median follow-up of 2.5 (IQR 0.96, 4.84) years, 1411 (8.1%) participants experienced AKI (Table 2). Users of SGLT2i exhibited the lowest crude incidence rate of AKI (18.3 [CI 95% 14.1–23.4] per 1000 person-years), followed by GLP1-RA users (22.5 [CI 95% 19.9–25.3] per 1000 person-years) and DPP-4i users (26.6 [CI 95% 25–28.2] per 1000 person-years). The weighted absolute risk of AKI at 3 years was 5.79% [95% CI 3.63–8.52] for the SGLT2i group, 7.03% [95% CI 5.69–8.69] for the GLP1-RA group and 7.00% [95% CI 6.43–7.58] for the DPP-4i group. In weighted Cox regression, and compared to DPP-4i, risks of AKI were similar for GLP1-RA (0.98 [CI 95% 0.82–1.18]) or SGLT2i (0.73 [CI 95% 0.45–1.16]). Although broad confidence intervals rendered associations statistically non-significant, risk magnitudes were lowest for patients on SGLT2i. Compared to GLP1-RA, the risk of AKI for patients started on SGLT2i did not differ, with a weighted HR of 0.74 [CI 95% 0.46–1.19].
Sensitivity analyses applying overlapping weights yielded similar results to our main analysis (Supplemental Table S6), with a HR for AKI of 0.89 [95% CI 0.66–1.20] among SGLT2i users compared to DPP-4i, and 0.79 [95% CI 0.57–1.09] compared to GLP1-RA.
Discussion
Concerns about the safety of SGLT2i have been raised by the US FDA [11] after reviewing voluntary reporting of cases in the “Adverse Event Reporting System (FAERS)”. Such possible risks were not noted by pivotal clinical trials [3, 4, 6, 7]. However, AKI is a rare outcome, and these clinical trials were underpowered to assess it robustly. Post-marketing surveillance studies in the heterogeneous routine clinical care are thus a necessary complement to assess the safety of SGLT2i. In this study, we compared the risk of detected AKI among users of novel glucose-lowering drugs in Stockholm´s routine healthcare. We observed that after balancing for an extensive range of confounders, AKI occurrence did not statistically differ between therapies. Instead, we observed numerically lower AKI risk magnitudes among users of SGLT2i compared to DPP4i and GLP1-RA. Results were robust to alternative methods of weighting for confounders and, collectively, add to growing evidence on the safety of initiating SGLT2i in adults with T2DM.
We studied and compared the health trajectories of 17,407 individuals with T2DM initiating these novel oral diabetes medications in our region and can now provide results that agree with and expand previous observations. Two administrative studies from Sweden and Denmark found that SGLT2i were associated with a lower risk of AKI compared with DPP-4 inhibitors (HR, 0.41 [95% CI, 0.32–0.52]) and GLP-1RA (HR, 0.69 [95% CI, 0.45–1.05]) [16, 18]. More recently, Zhuo et al. [17] reported a lower risk for SGLT2i vs DPP4i (HR 0.71, [95% CI 0.65–0.76]) and SGLT2i vs GLP1-RA groups (HR 0.81, [95% CI 0.75–0.87]) among Medicare users in the US. Important limitations of these studies were that they lacked information on the patient’s eGFR and that they identified AKI events through ICD diagnostic codes, which have low sensitivity. However, together with our findings, they provide reassurance on the safety of SGLT2i with respect to the risk of AKI and suggest that SGLT2i may prevent AKI events compared with alternative diabetes treatments. The mechanisms by which SGLT2i may protect against AKI compared with other glucose-lowering agents are still under investigation [26], and may include attenuation of glomerular hyperfiltration [27, 28], possibly due to tubular-glomerular feedback mechanisms through increased sodium delivery to macula densa [28]. Other postulated mechanisms involve altered renal oxygen homeostasis [29], reduced renal inflammation and decreased ischemic proximal tubular cell injury [30].
Our study has several strengths. Regarding the exposure, we ascertained it through pharmacy dispensations, which are better indicators of therapy initiation than prescription claims, in a country that provides universal healthcare access with almost all medication costs financed by the Government. This reduces healthcare access bias and increases face validity. However, we cannot guarantee that the medications dispensed at the pharmacy were taken by the patient. Regarding the outcome, we ascertained AKI events through both inpatient diagnostic codes and transient creatinine elevations according to KDIGO classification. This is important because AKI diagnoses are specific, but have low sensitivity [31]. By applying an active comparator new user design, we were able to minimize both confounding by indication and time-related bias, and we could identify and account for a large battery of confounders through propensity score weighting.
Our study also had limitations. Although our data source covers the healthcare of Stockholm region during 2008–2018, our study was limited in both size and length of follow-up and was also underpowered to compare single SGLT2i subclasses. This data represents AKI risks associated to these therapies in Stockholm between 2008 and 2018. Since then, new indications for SGLT2i have been approved, including a lower eGFR [3, 4, 32] and use in patients with CVD [33]. Future studies should confirm our observations in the broader use of this medication. Some of the currently most popular SGLT2i, such as dapagliflozin, empagliflozin and canagliflozin were approved by the European Medicines Agency (EMA) in 2012–2014, [34,35,36], and patients who started SGLT2i during the introduction of these therapies may differ in severity or characteristics from those who start today. Our study had a median follow-up of 2.5 years and it could be argued that, with longer duration of treatment, AKI signals may be more prominent. However, more than half of the AKI cases reported to the Adverse Event Reporting System (58 cases) occurred within 1 month of SGLT2i initiation. As in any observational study, residual and unknown confounding may still exist, and our results only report associations, not causal effects.
To conclude, in this region-representative study of routine care patients with T2DM initiating novel glucose-lowering drugs, we observed similar occurrence of AKI between therapies. Although not-statistically significant, we also observed a lower AKI risk associated to SGLT2i compared with DPP-4 inhibitor and GLP-1RA initiation. Our data thus offer support to mounting evidence on the safety of initiating SGLT2i.
Data availability statement
Datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request for collaborative research that is compliant with GDPR regulations.
References
Zheng Y, Ley SH, Hu FB (2018) Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol 14(2):88–98
Gallo LA, Wright EM, Vallon V (2015) Probing SGLT2 as a therapeutic target for diabetes: basic physiology and consequences. Diabetes Vasc Dis Res 12(2):78–89
Heerspink HJL et al (2020) Dapagliflozin in patients with chronic kidney disease. N Engl J Med 383(15):1436–1446
Perkovic V et al (2019) Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med 380(24):2295–2306
Neal B et al (2017) Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 377(7):644–657
Wanner C et al (2016) Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 375(4):323–334
Zinman B et al (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373(22):2117–2128
Buse JB et al (2020) 2019 Update to: management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 63(2):221–228
Cosentino F et al (2020) 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 41(2):255–323
Hahn K et al (2016) Acute kidney injury from SGLT2 inhibitors: potential mechanisms. Nat Rev Nephrol 12(12):711–712
FDA Drug Safety Communication: FDA strengthens kidney warnings for diabetes medicines canagliflozin (Invokana, Invokamet) and dapagliflozin (Farxiga, Xigduo XR). 2016. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-strengthens-kidney-warnings-diabetes-medicines-canagliflozin. Accessed Jan 2022
Zhao M et al (2020) Network meta-analysis of novel glucose-lowering drugs on risk of acute kidney injury. Clin J Am Soc Nephrol 16(1):70–78
Rampersad C et al (2020) Acute kidney injury events in patients with type 2 diabetes using SGLT2 inhibitors versus other glucose-lowering drugs: a retrospective cohort study. Am J Kidney Dis 76(4):471 e1-479 e1
Iskander C et al (2020) Use of sodium-glucose cotransporter-2 inhibitors and risk of acute kidney injury in older adults with diabetes: a population-based cohort study. CMAJ 192(14):E351–E360
Nadkarni GN et al (2017) Acute kidney injury in patients on SGLT2 inhibitors: a propensity-matched analysis. Diabetes Care 40(11):1479–1485
Ueda P et al (2018) Sodium glucose cotransporter 2 inhibitors and risk of serious adverse events: nationwide register based cohort study. BMJ 363:k4365
Zhuo M et al (2021) SGLT2 inhibitors and the risk of acute kidney injury in older adults with type 2 diabetes. Am J Kidney Dis 79(6):858–867. https://doi.org/10.1053/j.ajkd.2021.09.015
Pasternak B et al (2020) Use of sodium-glucose co-transporter 2 inhibitors and risk of serious renal events: Scandinavian cohort study. BMJ 369:m1186
Carrero JJ, Elinder CG (2022) The Stockholm CREAtinine Measurements (SCREAM) project: fostering improvements in chronic kidney disease care. J Intern Med 291(3):254–268
Levey AS et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Kidney Disease Improving Global Outcomes (KDIGO) 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. 2012. https://kdigo.org/guidelines/ckd-evaluation-and-management/. Accessed Jan 2022
(2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138.
McCaffrey DF et al (2013) A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat Med 32(19):3388–3414
Austin PC, Small DS (2014) The use of bootstrapping when using propensity-score matching without replacement: a simulation study. Stat Med 33(24):4306–4319
Fu EL et al (2019) Merits and caveats of propensity scores to adjust for confounding. Nephrol Dial Transplant 34(10):1629–1635
Nespoux J, Vallon V (2018) SGLT2 inhibition and kidney protection. Clin Sci (Lond) 132(12):1329–1339
Vallon V et al (2013) Knockout of Na-glucose transporter SGLT2 attenuates hyperglycemia and glomerular hyperfiltration but not kidney growth or injury in diabetes mellitus. Am J Physiol Ren Physiol 304(2):F156–F167
Cherney DZ et al (2014) Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation 129(5):587–597
O’Neill J et al (2015) Acute SGLT inhibition normalizes O2 tension in the renal cortex but causes hypoxia in the renal medulla in anaesthetized control and diabetic rats. Am J Physiol Ren Physiol 309(3):F227–F234
Dekkers CCJ et al (2018) Effects of the SGLT-2 inhibitor dapagliflozin on glomerular and tubular injury markers. Diabetes Obes Metab 20(8):1988–1993
Grams ME et al (2014) Performance and limitations of administrative data in the identification of AKI. Clin J Am Soc Nephrol 9(4):682–689
Kidney Disease Improving Global Outcomes Diabetes Work, G., KDIGO (2020) 2020 Clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int 98(4S):S1–S115
McDonagh TA et al (2021) 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 42(36):3599–3726
Forxiga (Dapagliflozin). Summary of European public assessment report (EPAR).
Invokana (Canagliflozin). Summary of European public assessment report (EPAR).
Jardiance (Empagliflozin). Summary of European public assessment report (EPAR).
Acknowledgements
This study was presented as a ‘free communication’ at the 2022 European Renal Association (ERA) Congress in Paris and ranked amongst the top 30 contributions by young researchers.
Funding
Open access funding provided by Karolinska Institute. Research reported in this publication was supported by the Swedish Research Council (#2019-01059, to J.J.C.), the Westman Foundation (to J.A.) and the Martin Rind Foundation (to J.A.). E.L.F. received support by a Rubicon Grant of the Netherlands.
Author information
Authors and Affiliations
Contributions
JA, ALF and JJC conceived the project; JA performed statistical analyses with support from AS and AB. JA developed the first draft, which was reviewed and developed to its final form by all coauthors.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests to report.
Ethical approval
The study received ethical approval by the regional ethical review board and the Swedish National Board of Welfare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alkas, J., Bosi, A., Sjölander, A. et al. Novel glucose-lowering drugs and the risk of acute kidney injury in routine care; the Stockholm CREAtinine Measurements (SCREAM) project. J Nephrol 36, 705–711 (2023). https://doi.org/10.1007/s40620-022-01505-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-022-01505-8