Abstract
Background
Improved responsiveness to erythropoiesis stimulating agents (ESAs) in patients on on-line post-dilution hemodiafiltration (Post-HDF) compared with conventional hemodialysis (HD) was reported by some authors but challenged by others. This prospective, cross-over randomized study tested the hypothesis that an alternative infusion modality of HDF, mixed-dilution HDF (Mixed HDF), could further reduce ESAs requirement in dialysis patients compared to the traditional Post-HDF.
Methods
One-hundred-twenty prevalent patients from 6 Dialysis Centers were randomly assigned to two six-months treatment sequences: A–B and B–A (A, Mixed HDF; B, Post-HDF). Primary outcome was comparative evaluation of ESA (darbepoetin alfa) requirement and ESA resistance. Treatments efficiency, iron and vitamins status, inflammation and nutrition parameters were monitored.
Results
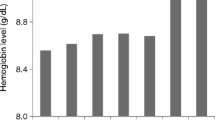
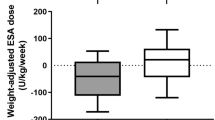
In sequence A, darbepoetin requirement decreased during Mixed HDF from 29.5 to 23.7 µg/month and increased significantly during Post-HDF (32.3 µg/month at 6th month) while, in sequence B, it increased during Post-HDF from 38.2 to 43.7 µg/month and decreased during Mixed HDF (23.9 µg/month at 6th month). Overall, EPO doses at 6 months on Mixed and Post-HDF were 23.8 and 38.4 µg/month, respectively, P < 0.01. A multiple linear model confirmed that Mixed HDF vs Post-HDF reduced significantly ESA requirement and ESA resistance (P < 0.0001), by a mean of 29% (CI 23–35%) in the last three months of the observation periods.
Conclusions
Mixed HDF decreased darbepoetin-alfa requirement in dialysis patients. This might help preventing the untoward side effects of high ESA doses, besides having a remarkable economic impact. Additional evidence is needed to confirm this potential benefit of Mixed-HDF.



Similar content being viewed by others
References
Locatelli F, Covic A, Eckardt KU, Wiecek A, Vanholder R, on behalf of the ERA-EDTA ERBP Advisory Board. Anemia management in patients with chronic kidney disease: a position statement by the Anemia Working Group of European. Renal Best Practice (ERBP). Nephrol Dial Transplant 2009; 24: 348–354.
McFarlane PA, Pisoni RL, Eichleay MA, Wald R, Port FK, Mendelssohn D (2010) International trends in erythropoietin use and hemoglobin levels in hemodialysis patients. Kidney Int 78(2):215–223
MacDougall IC, Cooper AC (2002) Erythropoietin resistance: the role of inflammation and pro-inflammatory cytokines. Nephrol Dial Transpl 17(Suppl 11):39–43
Alves MT, Vilaca SS, Carvalho M, Fernandes AP, Dusse LM, Gomes KB (2015) Resistance of dialyzed patients to erythropoietin. Rev Bras Hematol Hemoter 37:190–197
Solomon SD, Uno H, Lewis EF, Eckardt KU, Lin J, Burdmann EA et al (2010) Erythropoietic response and outcomes in kidney disease and type 2 diabetes. N Engl J Med 363:1146–1155
Rene E, Lazrak HH, Laurin LP, Elftouh N, Vallee M, Lafrance JP (2017) Association of erythropoiesis-stimulating agents and the incidence risk of cancer diagnosis among chronic dialysis patients: a nested case-control study. Nephrol Dial Transpl 32(6):1047–1052
Luo J, Jensen DE, Maroni BJ, Brunelli SM (2016) Spectrum and burden of erythropoiesis-stimulating agent hyporesponsiveness among contemporary hemodialysis Patients. Am J Kidney Dis 68(5):763–771
Perez-Garcia R, Varas J, Cives A, Martin-Malo A, Aljama P, Ramos R et al (2018) Increased mortality in hemodialysis patients administered high doses of erythropoiesis-stimulating agents: a propensity score-matched analysis. Nephrol Dial Transpl 33:690–699
Marcelli D, Bayh I, Merello JI, Ponce P, Heaton A, Kircelli F et al (2016) Dynamics of the erythropoiesis stimulating agent resistance index in incident hemodiafiltration and high-flux hemodialysis patients. Kidney Int 90(1):192–202
Panichi V, Scatena A, Rosati A, Giusti R, Ferro G, Malagnino E et al (2015) High-volume online hemodiafiltration improves erythropoiesis-stimulating agent (ESA) resistance in comparison with low-flux bicarbonate dialysis: results of the REDERT study. Nephrol Dial Transpl 30:682–689
Pedrini LA, De Cristofaro V, Comelli M, Casino FG, Prencipe M, Baroni A et al (2011) Long-term effects of high-efficiency on-line hemodiafiltration on uraemic toxicity A multicentre prospective randomized study. Nephrol Dial Transplant 26(8):2617–2624
Vaslaki L, Major L, Berta K, Karatson A, Misz M, Pethoe F et al (2006) On-line hemodiafiltration versus hemodialysis: stable haematocrit with less erythropoietin and improvement of other relevant blood parameters. Blood Purif 24:163–173
Tessitore N, Poli A, Bedogna V et al (2018) A single dialysis session of hemodiafiltration with sorbent-regenerated endogenous ultrafiltrate reinfusion (HFR) removes hepcidin more efficiently than bicarbonate hemodialysis: a new approach to containing hepcidin burden in dialysis patients? J Nephrol 31:297–306
Locatelli F, Altieri P, Andrulli S, Sau G, Bolasco P, Pedrini LA et al (2012) Predictors of hemoglobin levels and resistance to erythropoiesis-stimulating agents in patients treated with low-flux hemodialysis, haemofiltration and hemodiafiltration: results of a multicentre randomized and controlled trial. Nephrol Dial Transpl 27:3594–3600
Oates T, Pinney JH, Davenport A (2011) Hemodiafiltration versus high-flux hemodialysis: effects on phosphate control and erythropoietin response. Am J Nephrol 33:70–75
van der Weerd NC, Den Hoedt CH, Blankestijn PJ, Bots ML, van der Dorpel MA, Levesque R et al (2014) Resistance to erythropoiesis stimulating agents in patients treated with online hemodiafiltration and ultrapure low-flux hemodialysis: results from a randomized controlled trial (CONTRAST). PLoS ONE 9:e94434
Maduell F, Moreso F, Pons M, Ramos R, Mora-Macia J, Carreras J et al (2013) High-efficiency postdilution online hemodiafiltration reduces all-cause mortality in hemodialysis patients. J Am Soc Nephrol 24:487–497
Pedrini LA, Zawada AM, Winter AC, Pham J, Klein G, Wolf M et al (2019) Effects of high-volume online mixed-hemodiafiltration on anemia management in dialysis patients. PLoS ONE. https://doi.org/10.1371/journal.pone.0212795
Pedrini LA, Cozzi G, Faranna P, Mercieri A, Ruggiero P, Zerbi S et al (2006) Transmembrane pressure modulation in high-volume mixed hemodiafiltration to optimize efficiency and minimize protein loss. Kidney Int 69(3):573–579
Pedrini LA, Wiesen G (2011) Overcoming the limitations of post-dilution on-line hemodiafiltration: mixed dilution hemodiafiltration. Contrib Nephrol 175:129–140
Shirazian S, Rios-Rojas L, Drakakis J, Dikkala S, Dutka P, Duey M et al (2012) The effect of hemodialysis ultrafiltration on changes in whole blood viscosity. Hemodial Int 16(3):342–350
Bergstrom J, Wehle B (1987) No change in corrected β2-microglobulin concentration after cuprophane hemodialysis. Lancet 1:628–629
Daugirdas JT (1995) Simplified equations for monitoring Kt/V, PCRn, eKt/V, and ePCRn. Adv Ren Ther 2:295–304
Marcelli D, Kirchgessner J, Amato C, Steil H, Mitteregger A, Moscardo V et al (2001) EuCliD (European Clinical Database): a database comparing different realities. J Nephrol 14:S94–S100
Fleiss JL (1986) The cross-over study. In: Wiley, ed. The design and analysis of clinical experiments. New York, 263–281
The R Developement Core Team. R version 1.7.1. https://www.R-project.org. 2003. Vienna, Austria. Accessed 11 Dec 2019
Maduell F, del Pozo C, Garcia H, Sanchez L, Hdez-Jaras J, Albero MD et al (1999) Change from conventional hemodiafiltration to on-line hemodiafiltration. Nephrol Dial Transpl 14(5):1202–1207
Stefansson BV, Abramson M, Nilsson U, Haraldsson B (2012) Hemodiafiltration improves plasma 25-hepcidin levels: a prospective, randomized, blinded, cross-over study comparing hemodialysis and hemodiafiltration. Nephron Extra 2(1):55–65
Georgatzakou HT, Antonelou MH, Papassideri IS, Kriebardis AG (2016) Red blood cell abnormalities and the pathogenesis of anemia in end stage renal disease. Proteomics Clin Appl 10:778–790
Antonelou MH, Kriebardis AG, Velentzas AD, Kokkalis AC, Georgakopoulou SC, Papassideri IS (2011) Oxidative stress-associated shape transformation and membrane proteome remodeling in erythrocytes of end stage renal disease patients on hemodialysis. J Proteomics 74:2441–2452
Bonomini M, Ballone E, Di Stante S, Bucciarelli T, Dottori S, Arduino A, Urbani A, Sirolli V (2004) Removal of uremic plasma factor(s) using different dialysis modalities reduces phosphatidylserine exposure in red blood cells. Nephrol Dial Transpl 19:68–74
Bonomini V, Arduino A, Sirolli V, Di Pietro N, Pandolfi A (2017) Erythtocyte abnormalities and their possible role in cardiovascular complications of uremia. G Ital Nephrol. 34:1–15
Polaschegg HD (2009) Red blood cell damage from extracorporeal circulation in hemodialysis. Semin Dial 22:524–531
Watanabe N, Shimada T, Hakozaki M, Hara R (2018) Visualization of erythrocyte deformation induced by supraphysiological shear stress. Int J Artif Organs 41:838–844
Horobin JT, Sabapathy S, Simmonds MJ (2017) Repetitive supra-physiological shear stress impairs red blood cell deformability and induces hemolysis. Artif Organs 41(11):1017–1025
Yen JH, Chen SF, Chern MK, Lu PC (2014) The effect of turbulent viscous shear stress on red blood cell hemolysis. Int J Artif Organs 17(2):178–185
Simmonds MJ, Meiselman HJ (2016) Prediction of the level and duration of shear stress exposure that induces subhemolytic damage to erythrocytes. Biorheology 53(5–6):237–249
McNamee AP, Tansley GD, Sabapathy S, Simmonds MJ (2016) Biphasic impairment of erythrocyte deformability in response to repeated, short duration exposures of supraphysiological, subhaemolytic shear stress. Biorheology 53(3–4):137–149
Jones SA (1995) A relationship between Reynolds stresses and viscous dissipation: implications to red cell damage. Ann Biomed Eng 23(1):21–28
Pedrini LA, De Cristofaro V, Pagliari B, Samà F (2000) Mixed pre- and postdilution on-line hemodiafiltration: efficiency and safety compared with the traditional infusion modes. Kidney Int 58:2155–2165
Olia S, Maul T, Antaki J, Kameneva M (2016) Mechanical blood trauma in assisted circulation: sublethal RBC damage preceding hemolysis. Int J Artif Organs 39(4):150–159
Cozette P, Gaillard S, Rose E, Carnielo M (1979) Rheological effects of normovolemic hemodilution. Ann Anesthesiol Fr 20(9):775–783
Masakane I, Kikuchi K, Kawanishi I (2017) Evidence for the clinical advantages of predilution on-line hemodiafiltration. Contrib Nephrol 189:17–23
Acknowledgements
The authors thank all physicians and nurses working at the 6 NephroCare Dialysis Centers participating in this study for their efforts in handling the EuCliD data, which made this project possible. Centers participating in this study were: Nephrology and Dialysis Unit NephroCare, Bolognini Hospital, Seriate, and Dialysis Centers of “S.Isidoro” Hospital, Trescore Balneario, “Briolini” Hospital, Gazzaniga, “Faccanoni” Hospital, Sarnico, “Locatelli” Hospital, Piario, “Capitanio e Gerosa Hospital”, Lovere. All the Hospitals belong to the Azienda Socio-Sanitaria Territoriale Bergamo-Est, Italy, and Dialysis Centers operate within a public–private participation with NephroCare S.p.a., Italy.
Funding
We did not receive any financial support for this study.
Author information
Authors and Affiliations
Contributions
Study conception and design: LAP, AF, SS. Analysis and interpretation of data: LAP, PR, MC, LA. Data acquisition: VM, AC, MP, GG, GC, MA. Writing of manuscript draft: LAP, MC. Providing intellectual content of critical importance to the work: all authors. All authors take responsibility for the integrity and accuracy of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
LAP has a consultancy agreement with NephroCare, Italy, as Medical Director of the Unit of Nephrology and Dialysis of the Bolognini Hospital, Seriate, managed by NephroCare in the frame of a public–private participation with the Azienda Socio Sanitaria territoriale (ASST) Bergamo-Est, Italy. ADB, AF, VM, AC,MP, GG, MA are Nephrologists employees of NephroCare, Italy. SS is employee of Fresenius Medical Care, Germany. LAP is the patent holder “'The present invention refers to a method for blood purification by means of hemodialysis and/or hemofiltration, wherein to the blood in the extra-corporeal circuit of the hemodialysis and/or hemofiltration device a substitution solution is added upstream as well as downstream of the hemodialyser and/or hemofilter.” Documented at the following link: https://patents.google.com/patent/US6821441B2/en?inventor=luciano+pedrini&assignee=Fresenius+Medical+Care+Deutschland+Gmbh.
Ethical statement
The study was conducted in accordance with the basic principles of the Declaration of Helsinki and the rules of Good Clinical Practice and the protocol was approved by the local Ethic Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pedrini, L.A., Comelli, M., Ruggiero, P. et al. Mixed hemodiafiltration reduces erythropoiesis stimulating agents requirement in dialysis patients: a prospective randomized study. J Nephrol 33, 1037–1048 (2020). https://doi.org/10.1007/s40620-020-00709-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-020-00709-0