Abstract
Background
Conversion from conventional hemodialysis (CHD) to in-centre nocturnal hemodialysis (INHD) is associated with left ventricular (LV) mass regression, but the underlying mechanisms are not fully understood. Using cardiac MRI (CMR), we examined the effects of INHD on epicardial adipose tissue (EAT) and paracardial adipose tissue (PAT), and the relationships between EAT, PAT and LV remodeling, biomarkers of nutrition, myocardial injury, fibrosis and volume.
Methods
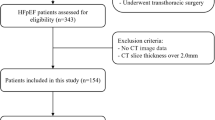
We conducted a prospective multicenter cohort study of 37 patients transitioned from CHD to INHD and 30 patients on CHD (control). Biochemical markers and CMR were performed at baseline and 52 weeks. CMR images were analyzed by independent readers, blinded to order and treatment group.
Results
Among 64 participants with complete CMR studies at baseline (mean age 54; 43% women), there were no significant differences in EAT index (60.6 ± 4.3 mL/m2 vs 64.2 ± 5.1 mL/m2, p = 0.99) or PAT index (60.0 ± 5.4 mL/m2 vs 53.2 ± 5.9 mL/m2, p = 0.42) between INHD and CHD groups. Over 52 weeks, EAT index and PAT index did not change significantly in INHD and CHD groups (p = 0.21 and 0.14, respectively), and the changes in EAT index and PAT index did not differ significantly between INHD and CHD groups (p = 0.30 and 0.16, respectively). Overall, changes in EAT index inversely correlated with changes in LV end-systolic volume index (LVESVI) but not LV end-diastolic volume index (LVEDVI), LV mass index (LVMI), and LV ejection fraction (LVEF). Changes in PAT index inversely correlated with changes in LVESVI, LVMI and positively correlated with changes in LVEF. There were no correlations between changes in EAT index or PAT index with changes in albumin, LDL, triglycerides, troponin-I, FGF-23, or NT-proBNP levels over 52 weeks (all p > 0.30).
Conclusions
INHD was not associated with any changes in EAT index and PAT index over 12 months. Changes in EAT index were not significantly associated with changes in markers of LV remodeling, nutrition, myocardial injury, fibrosis, volume status. In contrast, changes in PAT index, which paradoxically is expected to exert less paracrine effect on the myocardium, were correlated with changes in LVESVI, LVMI and LVEF. Larger and longer-term studies may clarify the role of PAT in cardiac remodeling with intensified hemodialysis.
ClinicalTrials.gov Identifier
NCT00718848.

Similar content being viewed by others
References
Canadian Institute for Health Information (2003) Canadian organ replacement register annual report: treatment of end-stage organ failure in Canada, 2003 to 2012. CIHI, Ottawa
Curtis BM, Parfrey PS (2005) Congestive heart failure in chronic kidney disease: disease-specific mechanisms of systolic and diastolic heart failure and management. Cardiol Clin 23(3):275–284
Wald R, Goldstein MB, Perl J, Kiaii M, Yuen D, Wald RM et al (2016) The association between conversion to in-centre nocturnal hemodialysis and left ventricular mass regression in patients with end-stage renal disease. Can J Cardiol 32(3):369–377
Graham-Brown MP, McCann GP, Burton JO (2015) Epicardial adipose tissue in patients with end-stage renal disease on haemodialysis. Curr Opin Nephrol Hypertens 24(6):517–524
Cheng KH, Chu CS, Lee KT, Lin TH, Hsieh CC, Chiu CC et al (2008) Adipocytokines and proinflammatory mediators from abdominal and epicardial adipose tissue in patients with coronary artery disease. Int J Obes (Lond) 32(2):268–274
Turkmen K, Kayikcioglu H, Ozbek O, Solak Y, Kayrak M, Samur C et al (2011) The relationship between epicardial adipose tissue and malnutrition, inflammation, atherosclerosis/calcification syndrome in ESRD patients. Clin J Am Soc Nephrol 6(8):1920–1925
Erdur MF, Tonbul HZ, Ozbiner H, Ozcicek A, Ozcicek F, Akbas EM et al (2013) The relationship between atherogenic index of plasma and epicardial adipose tissue in hemodialysis and peritoneal dialysis patients. Ren Fail 35(9):1193–1198
van Woerden G, Gorter TM, Westenbrink BD, Willems TP, van Veldhuisen DJ, Rienstra M (2018) Epicardial fat in heart failure patients with mid-range and preserved ejection fraction. Eur J Heart Fail 20(11):1559–1566
Cordeiro AC, Amparo FC, Oliveira MA, Amodeo C, Smanio P, Pinto IM et al (2015) Epicardial fat accumulation, cardiometabolic profile and cardiovascular events in patients with stages 3–5 chronic kidney disease. J Intern Med 278(1):77–87
Mahabadi AA, Massaro JM, Rosito GA, Levy D, Murabito JM, Wolf PA et al (2009) Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: the Framingham Heart Study. Eur Heart J 30(7):850–856
Sicari R, Sironi AM, Petz R, Frassi F, Chubuchny V, De Marchi D et al (2011) Pericardial rather than epicardial fat is a cardiometabolic risk marker: an MRI vs echo study. J Am Soc Echocardiogr 24(10):1156–1162
Rado SD, Lorbeer R, Gatidis S, Machann J, Storz C, Nikolaou K et al (2019) MRI-based assessment and characterization of epicardial and paracardial fat depots in the context of impaired glucose metabolism and subclinical left-ventricular alterations. Br J Radiol 92(1096):20180562
Colak H, Kilicarslan B, Tekce H, Tanrisev M, Tugmen C, Aktas G et al (2015) Relationship between epicardial adipose tissue, inflammation and volume markers in hemodialysis and transplant patients. Ther Apher Dial 19(1):56–62
Ulusal Okyay G, Okyay K, Polattas Solak E, Sahinarslan A, Pasaoglu O, Ayerden Ebinc F et al (2015) Echocardiographic epicardial adipose tissue measurements provide information about cardiovascular risk in hemodialysis patients. Hemodial Int 19(3):452–462
Doesch C, Haghi D, Fluchter S, Suselbeck T, Schoenberg SO, Michaely H et al (2010) Epicardial adipose tissue in patients with heart failure. J Cardiovasc Magn Reson 12:40
Nelson AJ, Worthley MI, Psaltis PJ, Carbone A, Dundon BK, Duncan RF et al (2009) Validation of cardiovascular magnetic resonance assessment of pericardial adipose tissue volume. J Cardiovasc Magn Reson 11:15
Ong JP, Wald R, Goldstein MB, Leipsic J, Kiaii M, Deva DP et al (2019) Left ventricular strain analysis using cardiac magnetic resonance imaging in patients undergoing in-centre nocturnal haemodialysis. Nephrology (Carlton) 24(5):557–563
Altun B, Tasolar H, Eren N, Binnetoglu E, Altun M, Temiz A et al (2014) Epicardial adipose tissue thickness in hemodialysis patients. Echocardiography 31(8):941–946
Noori N, Yan AT, Kiaii M, Rathe A, Goldstein MB, Bello O et al (2017) Nutritional status after conversion from conventional to in-centre nocturnal hemodialysis. Int Urol Nephrol 49(8):1453–1461
Ansaldo AM, Montecucco F, Sahebkar A, Dallegri F, Carbone F (2019) Epicardial adipose tissue and cardiovascular diseases. Int J Cardiol 278:254–260
D’Marco LG, Bellasi A, Kim S, Chen Z, Block GA, Raggi P (2013) Epicardial adipose tissue predicts mortality in incident hemodialysis patients: a substudy of the renagel in new dialysis trial. Nephrol Dial Transplant 28(10):2586–2595
Chang TI, Ngo V, Streja E, Chou JA, Tortorici AR, Kim TH et al (2017) Association of body weight changes with mortality in incident hemodialysis patients. Nephrol Dial Transplant 32(9):1549–1558
Tonbul HZ, Demir M, Altintepe L, Guney I, Yeter E, Turk S et al (2006) Malnutrition-inflammation-atherosclerosis (MIA) syndrome components in hemodialysis and peritoneal dialysis patients. Ren Fail 28(4):287–294
Eriguchi R, Obi Y, Rhee CM, Chou JA, Tortorici AR, Mathew AT et al (2017) Changes in urine volume and serum albumin in incident hemodialysis patients. Hemodial Int 21(4):507–518
Opie LH, Commerford PJ, Gersh BJ, Pfeffer MA (2006) Controversies in ventricular remodelling. Lancet 367(9507):356–367
Gutierrez OM, Mannstadt M, Isakova T, Rauh-Hain JA, Tamez H, Shah A et al (2008) Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis. N Engl J Med 359(6):584–592
Funding
This study was supported by an operating grant from the Canadian Institutes of Health Research and a grant-in-aid from Heart and Stroke Foundation. The study sponsor had no role in the study design, data collection or analysis, interpretation of the findings, writing the manuscript, or the decision to submit the manuscript for publication. ClinicalTrials.gov Identifier: NCT00718848.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical approval
The study was approved by the research ethics boards of St. Michael's hospital and St. Paul’s Hospital (Vancouver, British Columbia).
Informed consent
All patients provided their written informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cai, S., Wald, R., Deva, D.P. et al. Cardiac MRI measurements of pericardial adipose tissue volumes in patients on in-centre nocturnal hemodialysis. J Nephrol 33, 355–363 (2020). https://doi.org/10.1007/s40620-019-00665-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-019-00665-4