Abstract
Background
Optimal fluid balance for peritoneal dialysis (PD) patients requires both water and sodium removal. Previous studies have variously reported that continuous ambulatory peritoneal dialysis (CAPD) removes more or equivalent amounts of sodium than automated PD (APD) cyclers. We therefore wished to determine peritoneal dialysate losses with different PD treatments.
Methods
Peritoneal and urinary sodium losses were measured in 24-h collections of urine and PD effluent in patients attending for their first assessment of peritoneal membrane function. We adjusted fluid and sodium losses for CAPD patients for the flush before fill technique.
Results
We reviewed the results from 659 patients, mean age 57 ± 16 years, 56.3% male, 38.9% diabetic, 24.0% treated by CAPD, 22.5% by APD and 53.5% APD with a day-time exchange, with icodextrin prescribed to 72.8% and 22.7 g/L glucose to 31.7%. Ultrafiltration was greatest for CAPD 650 (300–1100) vs 337 (103–598) APD p < 0.001, vs 474 (171–830) mL/day for APD with a day exchange. CAPD removed most sodium 79 (33–132) vs 23 (− 2 to 51) APD p < 0.001, and 51 (9–91) for APD with a day exchange, and after adjustment for the CAPD flush before fill 57 (20–113), p < 0.001 vs APD. APD patients with a day exchanged used more hypertonic glucose dialysates [0 (0–5) vs CAPD 0 (0–1) L], p < 0.001.
Conclusion
CAPD provides greater ultrafiltration and sodium removal than APD cyclers, even after adjusting for the flush-before fill, despite greater hypertonic usage by APD cyclers. Ultrafiltration volume and sodium removal were similar between CAPD and APD with a day fill.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peritoneal dialysis (PD) is an established treatment for patients with end-stage kidney disease. In addition to obtaining adequate solute clearances, PD should control volume status and sodium balance. After peritonitis [1], failure to achieve adequate ultrafiltration is the next commonest cause of PD technique failure, and just as there are targets for small solute clearances for PD patients the European Automated Peritoneal Dialysis Outcomes Study (EAPOS) recommended a minimum target amount of ultrafiltration to prevent volume overload and PD technique failure [2].
Patients with faster peritoneal transport are reported to have lower technique survival when treated by continuous ambulatory peritoneal dialysis (CAPD) [3]. Longer cycle dwell times risk a reduction in the osmotic gradient that drives ultrafiltration and sodium removal in faster peritoneal transporters treated by CAPD, due to glucose absorption. Failure to achieve adequate sodium removal will lead to extracellular water (ECW) expansion and hypertension, resulting in left ventricular hypertrophy [4] with increased risk of cardiovascular and cerebrovascular events in dialysis patients [5]. The introduction of automated peritoneal dialysis (APD) cyclers has been reported to reduce technique failure rates for faster peritoneal transporters [3], and studies from both the USA and Brazil have reported greater PD technique and patient survival with APD compared to CAPD [6, 7], even after adjustment for patient demographics and co-morbidity [8].
There have been a limited number of studies which have specifically addressed sodium removal by different modes of PD; It has been suggested that CAPD is more effective than APD in terms of both ultrafiltration volumes and sodium removal, probably due to the longer cycle dwell times [9,10,11]. Although these studies may have over-estimated the sodium removal by CAPD by not taking into account the volume used for the flush before fill technique used with CAPD exchanges. Other studies have observed no difference in sodium removal and volume status comparing CAPD and APD with a day time exchange [12]. The differences between studies may reflect the use of 7.5% icodextrin, which has been reported to increase peritoneal sodium removal compared to glucose dialysates for both CAPD and APD patients with a day time exchange [13].
We therefore wished to determine whether sodium removal differed between the different PD modalities, and whether there was any association between sodium removal and ECW excess or hypertension.
Materials and methods
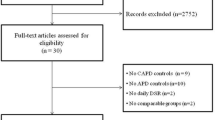
We retrospectively audited consecutive PD outpatients treated with CAPD, APD and APD with a day time exchange (continuous cycling peritoneal dialysis—CCPD) attending for their first assessment of peritoneal membrane function. All patients had a 22.7 g/L exchange prior to attendance. No patient had suffered with peritonitis in the previous 8 weeks or an emergency admission to hospital. We excluded patients with implantable cardiac devices, amputations and those unable to stand.
Patients had standing height measured and were weighed post voiding and with peritoneal dialysate drained out. PD adequacy was calculated by standard methods from 24-h urinary collections and samples from spent dialysates and estimated normalised protein nitrogen appearance (nPNA) [14]. Peritoneal membrane transport was calculated from 4-h peritoneal dialysate dwell and plasma creatine concentrations using a standard 2.0 L 22.7 g/L peritoneal dialysate [14]. In addition to standard biochemical tests, we also measured blood glucose, serum albumin by bromocresol green method and creatinine enzymatically (Roche Modular P® analyser, Roche Diagnostics Limited, Burgess Hill, UK), with sodium in urine and dialysates measured using an indirect ion electrode [15]. Serum sodium values were adjusted if serum glucose was elevated [16]. Sodium removal was calculated by the addition of 24-h urinary sodium to the difference between dialysate sodium instilled and the sodium in 24-h effluent dialysate. Patients and staff were instructed to allow 15 s for the flush before fill CAPD technique, and the median volume measured was 90 mL, as such sodium balance in CAPD patients was then adjusted from an initial volume of 2.15 L in a fresh dialysate bag [17]. We calculated the amount of glucose in the dialysis prescription and report this as glucose exposure (mmol/day). No patient was prescribed a glucose dialysate concentration above 22.7 g/L.
Multifrequency bioelectrical impedance (MFBIA) was measured using a standardised protocol (InBody 720, Seoul, South Korea), with dialysate drained out and after voiding [18, 19]. Blood pressure was recorded in the supine position after the patient had drained out dialysate and rested for a minimum of 30 min and abstained from any stimulants (Dinamap, Critikon Corporation, Tampa, FL, USA). All equipment was regularly serviced and calibrated.
Medications were obtained from hospital computerised records. All patients were provided with dietary advice, from a renally trained dietician, to limit dietary sodium to around 100 mmol/day, and loop diuretics (250 mg/day frusemide) were prescribed as standard treatment for patients with urinary output of ≥ 200 mL/day.
Statistical analysis
Results are expressed as mean ± standard deviation, or median and interquartile range, or percentage. We used standard statistical analysis D’Agostino and Pearson normality test, Chi square analysis with adjustment for small numbers where appropriate. Anova and Kruskal–Wallis analyses for parametric and nonparametric group data, with appropriate correction for multiple analyses by Tukey or Games–Howell ad hoc testing respectively. Univariate analysis was performed by Spearman’s correlation for adjusted PD sodium losses and followed by a multivariable step-backward regression model for higher than median vs lower than median adjusted peritoneal dialysate sodium losses. Variables with univariate association of p < 0.1 were included. Non-parametric data was log transformed, and variables excluded in a back-ward regression model if not significant and did not improve model fit. The model was checked for collinearity and variance inflation factor. Statistical analysis was performed using Graph Pad Prism (version 8.1, Graph Pad, San Diego, CA, USA) and Statistical Package for Social Science version 24.0 (IBM Corporation, Armonk, NY, USA). Statistical significance was taken at or below the 5% level.
Ethics
Our retrospective audit of service development complied with the United Kingdom National Health Service Health Research Authority, guidelines for clinical audit and service development. with all patient data anonymised prior to analysis (https://www.hra.nhs.uk), and complied with United Kingdom National Institute for Clinical Excellence best practices, http://www.nice.org.uk/media/796/23/bestpracticeclinicalaudit.pdf, and registered with the University College department of nephrology.
Results
We reviewed the data on 659 adult PD patients attending for their first assessment of peritoneal membrane function, median duration of peritoneal dialysis 3 (2–7) months. The majority of patients were treated by APD with a day-time exchange (Table 1). Patients dialysed daily, and the median APD cycler session time was 8.0 (8.0–8.0) h. Patients treated by CAPD were older. The majority of CAPD patients and those treated by APD with a day-time exchange were prescribed icodextrin, and more hypertonic glucose exchanges were used by APD patients with a day-time exchange. Patients treated by APD had greater urine output and urinary sodium excretion. Net peritoneal ultrafiltration and sodium removal was greatest with CAPD, although this then fell after adjustment for the fill before flush technique, net ultrafiltration volume and peritoneal sodium loss remained greater for CAPD compared to APD (p < 0.001), but not for APD with a day-time icodextrin exchange (Figs. 1, 2). Peritoneal transporter status, the number of diabetic subjects, body composition and nPNA did not differ between the different PD treatment modes of treatment. Total weekly Kt/Vurea was similar between the different PD modes (Table 1), as was daily net sodium removal, after adjustment for the flush before fill (Fig. 2).
Twenty-4-h sodium balance as the difference between sodium losses in urine and peritoneal dialysate minus sodium infused in peritoneal dialysate, and 24-h peritoneal sodium balance as the difference between sodium in drained peritoneal dialysate minus sodium infused in peritoneal dialysate. Continuous ambulatory peritoneal dialysis (CAPD), automated peritoneal dialysis (APD) cyclers. Adjusted CAPD accounts for the flush before fill technique., ***p < 0.001 vs APD with a day time exchange
Dividing patients according to peritoneal transporter status [14], then more faster transporters were male and diabetic, and treated by CAPD and APD with a day time exchange, use of icodextrin and hypertonic glucose exchanges, but there were no over-all differences in sodium removal (Table 2). Sub-dividing patients according to transporter status and PD treatment mode, there were very few slow transporters, and as such we combined slow and slow-average transporters. There were no differences between peritoneal sodium losses between the different PD treatment modes for slow and slow-average transporters, but peritoneal sodium removal was lower for fast-average and fast transporters for those treated with APD cyclers (Table 2).
To determine the effect of peritoneal transport status and PD modality we used the European Dialysis and Transplant best practice guideline definitions of slow, average and fast transporter [20]. Peritoneal sodium losses were greater for faster CAPD transporters compared to APD (Fig. 3), and slow CAPD transporters were prescribed less glucose compared to patients treated by APD with and without a day time exchange (Slow CAPD vs slow APD p < 0.05, vs average APD and slow APD with day exchange p < 0.01, otherwise p < 0.001) (Table 3).
The effect of peritoneal dialysis modality and peritoneal dialysis transporter status using European Best Practice Guideline definition of slow, average and fast transporter [20]. Continuous ambulatory peritoneal dialysis (CAPD), automated peritoneal dialysis (APD). *p < 0.05, **< 0.01, < 0.001 vs CAPD fast transporter
Univariate analysis demonstrated that net peritoneal sodium loses, adjusted for fill before flush technique were associated with use of peritoneal ultrafiltration volume (r = 0.69, p < 0.001). In addition, there were positive associations with icodextrin and hypertonic glucose exchanges, peritoneal ultrafiltration volume and urea clearance, 4-h dialysate to plasma creatinine ratio, patient age and negatively with 24-h urinary sodium and volume, serum albumin and mean arterial blood pressure (Table 4).
As the peritoneal sodium balance varied from net sodium retention to losses, a multivariable regression model was analysed comparing greater versus lower sodium losses (Table 4). Daily peritoneal ultrafiltration volume, urea clearance and use of icodextrin and hypertonic glucose exchanges and age remained independently associated with peritoneal sodium losses (Table 5).
Discussion
Besides adequate removal of uraemic toxins, one of the other major treatment goals for PD is regulating volume and sodium balance. Previous reports have suggested a minimum peritoneal ultrafiltration target, once residual renal function has been lost [2]. Prior to the advent of APD cyclers and icodextrin dialysates, then faster peritoneal transporters were reported to at greater risk of PD technique failure [3], thought to be due to failure to achieve adequate ultrafiltration and sodium removal. Although, following the introduction of APD cyclers, reports then suggested no difference in technique survival [6], and several studies have not observed any differences in blood pressure or volume control between different PD treatment modalities [21, 22]. However, a recent meta-analysis reported that treatment with CAPD removed more sodium than APD [23]. As many of these studies were based on the results from a small number of patients, we reviewed peritoneal sodium removal in our cohort of more than 600 patients.
In keeping with some earlier reports, we noted that CAPD patients using an overnight icodextrin exchange had greater daily ultrafiltration volumes and peritoneal sodium losses, compared to those treated by APD with and without a day time icodextrin exchange [11]. Whereas volume in-flow measurements are relatively accurate with APD cyclers, CAPD dialysate bags are over-filled to allow for the flush- before fill technique [17], which has been measured range between 50 and 100 mL [11]. Our patients were taught to allow 15 s for the flush, and when we adjusted for this, then there was no difference in daily ultrafiltration volumes or peritoneal sodium losses compared to patients treated by APD with a day-time icodextrin exchange. Although CAPD losses remained grater than those treated by APD alone, although as
These patients had greater residual renal function and urinary sodium losses, thus over-all losses were similar between modalities, supporting the results of smaller studies [10, 24]. As with many centres we practice incremental dialysis, with peritoneal dialysis prescriptions taking into account residual renal function [25], and as such patients with greater residual renal function and urinary sodium losses had correspondingly lower peritoneal sodium losses.
Compared to some previous studies, peritoneal sodium losses were lower in our study [23]. This may have been due to taking into account the additional sodium load of the flush before fill in CAPD patients, greater residual renal function with greater urinary sodium losses and educating patients to reduce dietary sodium intake.
Sodium is predominantly removed by convection with PD, and as such there was a strong association between ultrafiltration volumes and sodium removal. The association was slightly stronger for CAPD than either APD or APD with a day-time exchange (r2 0.56 vs 0.45 vs 0.44 respectively). It has been suggested that the shorter APD dwell cycles, using glucose dialysates, induce a rapid movement of water through aquaporins, but a slower movement of sodium through co- and active transporters, and as such APD cyclers, so reducing sodium removal when using APD cyclers [11].
Peritoneal sodium removal was also associated with the volume of icodextrin prescribed, supporting other studies which have shown that volume status is better maintained with icodextrin compare to 22.7 g/L glucose exchanges [26]. Whereas some smaller earlier studies did not demonstrate an effect of hypertonic glucose dialysates and peritoneal sodium losses [9], we noted a univariate association, which would be expected as hypertonic dialysates would be expected to increase ultrafiltration [10, 24]. There was a weak association between higher mean arterial blood pressure and lower peritoneal sodium losses, and previous studies have either reported a similar association or no effect of peritoneal sodium losses on blood pressure [9, 27]. In keeping with previous reports, we found no over-all association between transporter status and peritoneal sodium losses [11], which may reflect that the great majority of our patients were prescribed icodextrin, and most patients had residual renal function. However, we noted that both fast-average and fast peritoneal transporters had greater sodium removal with CAPD compare to APD. Faster transporters had shorter APD dwell times compared to slow and slow-average, which may account for the difference in sodium removal [11]. In addition, we also noted an effect of age on peritoneal sodium removal, whether this was due to an increased use of CAPD in older compared to younger patients, or due to changes which occur in the peritoneal membrane with age remains to be determined [28].
As with any observational cross-sectional study we can report associations but not causality. Compared to previous cohorts, we report on over 600 patients predominantly treated with APD cyclers and icodextrin, attending for their first assessment of peritoneal membrane function, and we acknowledge that membrane function may change with time in some patients [29]. Initial investigation showed that CAPD removed more sodium than either APD or APD with a daytime exchange. However, after adjusting for the flush-before fill technique, there was no difference between CAPD and APD with a daytime exchange, although patients treated with APD with a daytime exchange received a greater volume and hypertonic glucose exchanges. Thus, although treatment using APD cyclers can achieve similar peritoneal sodium removal as CAPD, it is at a cost of greater peritoneal exposure to hypertonic exchanges.
References
Davenport A (2009) Peritonitis remains the major clinical complication of peritoneal dialysis: the London, UK, peritonitis audit 2002–2003. Perit Dial Int 29(3):297–302
Brown EA, Davies SJ, Rutherford P, Meeus F, Borras M, Riegel W, Divino Filho JC, Vonesh E, van Bree M, EAPOS Group (2003) Survival of functionally anuric patients on automated peritoneal dialysis: the European APD Outcome Study. J Am Soc Nephrol 14(11):2948–2957
Johnson DW, Hawley CM, McDonald SP, Brown FG, Rosman JB, Wiggins KJ, Bannister KM, Badve SV (2010) Superior survival of high transporters treated with automated versus continuous ambulatory peritoneal dialysis. Nephrol Dial Transplant 25(6):1973–1979
Inal S, Erten Y, Okyay GU, Ataş N, Oneç K, Yayla C, Tekbudak MY, Sahin G, Tavil Y, Sindel S (2014) Association between bioimpedance analysis parameters and left ventricular hypertrophy in peritoneal dialysis patients. Int Urol Nephrol 46(9):1851–1856
Findlay M, MacIsaac R, MacLeod MJ, Metcalfe W, Traynor JP, Dawson J, Mark PB (2018) Renal replacement modality and stroke risk in end-stage renal disease—a national registry study. Nephrol Dial Transplant 33(9):1564–1571
Cnossen TT, Usvyat L, Kotanko P, van der Sande FM, Kooman JP, Carter M, Leunissen KM, Levin NW (2011) Comparison of outcomes on continuous ambulatory peritoneal dialysis versus automated peritoneal dialysis: results from a USA database. Perit Dial Int 31(6):679–684
Franco MRG, Bastos MG, Qureshi AR, Schreider A, Bastos KA, Divino-Filho JC, Fernandes NMS (2017) Incident elderly patients on peritoneal dialysis: epidemiological characteristics and modality impact on survival time. Saudi J Kidney Dis Transplant 28(4):782–791
Beduschi Gde C, Figueiredo AE, Olandoski M, Pecoits-Filho R, Barretti P, de Moraes TP (2015) Automated peritoneal dialysis is associated with better survival rates compared to continuous ambulatory peritoneal dialysis: a propensity score matching analysis. PLoS One 10(7):e0134047 (all centers that contributed to the BRAZPD)
Ortega O, Gallar P, Carreño A, Gutierrez M, Rodriguez I, Oliet A, Vigil A, Gimenez E (2001) Peritoneal sodium mass removal in continuous ambulatory peritoneal dialysis and automated peritoneal dialysis: influence on blood pressure control. Am J Nephrol 21(3):189–193
Moor V, Wagner R, Sayer M, Petsch M, Rueb S, Häring HU, Heyne N, Artunc F (2017) Routine monitoring of sodium and phosphorus removal in peritoneal dialysis (PD) patients treated with continuous ambulatory PD (CAPD), automated PD (APD) or combined CAPD + APD. Kidney Blood Press Res 42(2):257–266
Rodriguez-Carmona A, Pérez-Fontán M, Garca-Naveiro R, Villaverde P, Peteiro J (2004) Compared time profiles of ultrafiltration, sodium removal, and renal function in incident CAPD and automated peritoneal dialysis patients. Am J Kidney Dis 44(1):132–145
Davison SN, Jhangri GS, Jindal K, Pannu N (2009) Comparison of volume overload with cycler-assisted versus continuous ambulatory peritoneal dialysis. Clin J Am Soc Nephrol 4(6):1044–1050
Morelle J, Sow A, Fustin CA, Fillée C, Garcia-Lopez E, Lindholm B, Goffin E, Vandemaele F, Rippe B, Öberg CM, Devuyst O (2018) Mechanisms of crystalloid versus colloid osmosis across the peritoneal membrane. J Am Soc Nephrol 29(7):1875–1886
(2007) NKF-DOQI clinical practice guidelines for peritoneal dialysis adequacy. Assessment of nutritional status. Am J Kidney Dis 30(3 Suppl 2), S125–S129
Persaud J, Thomas M, Davenport A (2014) Indirect ion selective electrode methods potentially overestimate peritoneal dialysate sodium losses. Ther Apher Dial 18(4):321–325
Penne EL, Thijssen S, Raimann JG, Levin NW, Kotanko P (2010) Correction of serum sodium for glucose concentration in hemodialysis patients with poor glucose control. Diabetes Care 33(7):e91
McCafferty K, Fan SL (2006) Are we underestimating the problem of ultrafiltration in peritoneal dialysis patients? Perit Dial Int 26(3):349–352
Davenport A (2013) Effect of intra-abdominal dialysate on bioimpedance-derived fluid volume status and body composition measurements in peritoneal dialysis patients. Perit Dial Int 33(5):578–579
Davenport A, Willicombe MK (2009) Hydration status does not influence peritoneal equilibration test ultrafiltration volumes. Clin J Am Soc Nephrol 4(7):1207–1212
Dombros N, Dratwa M, Feriani M, Gokal R, Heimbürger O, Krediet R, Plum J, Rodrigues A, Selgas R, Struijk D, Verger C, EBPG Expert Group on Peritoneal Dialysis (2005) European best practice guidelines for peritoneal dialysis. 7 Adequacy of peritoneal dialysis. Nephrol Dial Transplant 20(Suppl 9):ix24–ix27
Cnossen TT, Konings CJ, Fagel WJ, van der Sande FM, van Geel K, Leunissen KM, Kooman JP (2012) Fluid state and blood pressure control: no differences between APD and CAPD. ASAIO J 58(2):132–136
Davenport A, Willicombe MK (2009) Comparison of fluid status in patients treated by different modalities of peritoneal dialysis using multi-frequency bioimpedance. Int J Artif Organs 32(11):779–786
Borrelli S, La Milia V, De Nicola L, Cabiddu G, Russo R, Provenzano M, Minutolo R, Conte G, Garofalo C, Study Group Peritoneal Dialysis of Italian Society of Nephrology (2019) Sodium removal by peritoneal dialysis: a systematic review and meta-analysis. J Nephrol 32(2):231–239
Mohamed A, Davenport A (2019) Sodium loss, extracellular volume overload and hypertension in peritoneal dialysis patients treated by automated peritoneal dialysis cyclers. Int J Artif Organs. https://doi.org/10.1177/0391398819864368
Neri L, Viglino G, Marinangeli G, Rocca AR, Laudon A, Ragusa A, Cabiddu G, Peritoneal Dialysis (2017) Incremental start to PD as experienced in Italy: results of censuses carried out from 2005 to 2014. J Nephrol 30(4):593–599
Davies SJ, Woodrow G, Donovan K et al (2003) Icodextrin improves the fluid status of peritoneal dialysis patients: results of a double-blind randomized controlled trial. J Am Soc Nephrol 14(9):2338–2344
Boudville NC, Cordy P, Millman K, Fairbairn L, Sharma A, Lindsay R, Blake PG (2007) Blood pressure, volume, and sodium control in an automated peritoneal dialysis population. Perit Dial Int 27(5):537–543
Waniewski J, Antosiewicz S, Baczynski D, Poleszczuk J, Pietribiasi M, Lindholm B, Wankowicz Z (2016) Peritoneal fluid transport rather than peritoneal solute transport associates with dialysis vintage and age of peritoneal dialysis patients. Comput Math Methods Med 2016:8204294
Yu Z, Lambie M, Davies SJ (2014) Longitudinal study of small solute transport and peritoneal protein clearance in peritoneal dialysis patients. Clin J Am Soc Nephrol 9(2):326–334
Acknowledgements
Dr. Sarju Raj Singh Maharjan was in receipt of International Society of Nephrology Kidney Research UK training award.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Ethical approval
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Maharjan, S.R.S., Davenport, A. Comparison of sodium removal in peritoneal dialysis patients treated by continuous ambulatory and automated peritoneal dialysis. J Nephrol 32, 1011–1019 (2019). https://doi.org/10.1007/s40620-019-00646-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-019-00646-7