Abstract
Purpose
Randomized controlled trials with tirzepatide (TZP) displayed unprecedented glucose and body weight lowering efficacy in individuals with type 2 diabetes and/or obesity and a safety profile similar to that of glucagon-like peptide-1 receptor agonists (GLP-1RA), mainly characterized by gastrointestinal (GI) adverse events (AE). Concerns on diabetic retinopathy, pancreato-biliary disorders, and medullary thyroid cancer were also addressed. We aimed to investigate whether the same safety issues emerged from the FDA Adverse Event Reporting System (FAERS) post-marketing surveillance database.
Methods
OpenVigil 2.1-MedDRA-v24 and AERSMine (data 2004Q1-2023Q3) were used to query the FAERS database. Reports of GI AE, diabetic retinopathy, pancreato-biliary disorders, and medullary thyroid cancer were investigated. The analysis was then filtered for age, gender, and designation as primary suspect. AE occurrence with TZP was compared to insulin, sodium-glucose cotransporter-2 inhibitors, metformin, and GLP-1RA.
Results
Disproportionate reporting of GI [i.e., nausea (ROR 4.01, 95% CI 3.85–4.19)] and pancreato-biliary disorders [i.e., pancreatitis (ROR 3.63, 95% CI 3.15–4.19)], diabetic retinopathy (ROR 4.14, 95% CI 2.34–7.30), and medullary thyroid cancer (ROR 13.67, 95% CI 4.35–42.96) was detected. TZP exhibited a similar risk of GI AE and medullary thyroid cancer and a lower risk of most pancreato-biliary AE and diabetic retinopathy vs. GLP-1RA.
Conclusions
TZP was associated with an increased risk of specific AE. However, its safety profile was similar to that of GLP-1RA, without increased risk of pancreato-biliary AE, diabetic retinopathy, and medullary thyroid cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tirzepatide (TZP) is a dual glucose-dependent insulinotropic (GIP)/glucagon-like peptide-1 (GLP-1) receptor agonist approved by the Food and Drug Administration (FDA) for the management of diabetes since May 2022 and obesity since November 2023. In the latest version of the American Diabetes Association’s Standard of Medical Care in Diabetes, TZP has been listed among the most efficacious drugs for achieving glucose- and/or body weight (BW)-lowering [1]. Furthermore, a recent network meta-analysis has showed TZP to be superior to other currently available incretin-based treatment strategies in reducing HbA1c [i.e. −0.40%, 95% CI (−0.66; −0.14) vs. iDegLira] and BW [i.e. −6.56 kg, 95% CI (−7.38; −5.73) vs. semaglutide 2 mg] [2]. Randomized controlled trials (RCT) have also shown the safety profile of TZP to be similar to that of GLP-1 receptor mono-agonists (GLP-1RA) and mainly characterized by gastrointestinal (GI) adverse events (AE) [3]. Of note, both RCT [4] and real-world studies [5] with GLP-1RA have arisen concerns on other AE, including pancreato-biliary disorders, diabetic retinopathy, and thyroid (especially medullary) cancer [5], while evidence on these issues is still scarce and inconclusive for TZP. A systematic review and meta-analysis of 9 RCT showed that the administration of TZP was associated with a similar risk of pancreatitis compared to basal insulin or placebo or selected GLP-1RA, while the risk of composite gallbladder or biliary diseases vs. basal insulin or placebo was found to be increased [6]. However, a very limited number of cases of pancreato-biliary AE were reported in the 9687 patients involved in the SURPASS program [7,8,9,10,11,12,13,14,15]. Also, very few cases of diabetic retinopathy and no cases of medullary thyroid cancer were detected [7,8,9,10,11,12,13,14,15].
The FDA Adverse Event Reporting System (FAERS) database is a publicly available repository for post-marketing surveillance of FDA-approved therapies, collecting manufacturer- or customer-initiated reports of AE, product quality complaints, and medication errors as coded using the Medical Dictionary for Regulatory Activities (MedDRA) terminology. Despite intrinsic limitations, analysis of real-world data such as those collected in the FAERS database may be informative and complement the information from RCT [16]. In this study, we aimed to investigate the real-world safety profile of TZP as depicted by the FAERS database, with a particular focus on GI and pancreato-biliary AE, diabetic retinopathy, and medullary thyroid cancer.
Research design and methods
OpenVigil 2.1-MedDRA-v24 and AERSMine [17] (data 2004Q1-2023Q3) were used to query FAERS. A positive signal of disproportionality was defined as a proportional reporting ratio (PRR) of 2 or greater, chi-squared of at least 4, and 3 or more cases according to Evans’ criteria [18]. The number of total AE and of AE fulfilling Evans’ criteria was extracted for TZP vs. all other drug. Then, in agreement with the MedDRA terminology, reports of AE identified by the preferred terms (PT) under the following high level terms (HLT) were retrieved: “gastrointestinal signs and symptoms nec”, “gastrointestinal disorders nec”, “nausea and vomiting symptoms”, “dyspeptic signs and symptoms”, “diarrhoea (excl infective)”, “gastrointestinal atonic and hypomotility disorders nec”, “flatulence, bloating and distention”, “gastrointestinal and abdominal pains (excl oral and throat)”, “acute and chronic pancreatitis”, “cholecystitis and cholelithiasis”, “bile duct infections and inflammations”, “diabetic complications ophthalmic”, “thyroid neoplasms”, “thyroid disorders nec” (Supplementary Table 1). Automatic data deduplication is provided by the software and based on case and individual safety reports (ISR) numbers. The PRR and the reporting odds ratio (ROR) were extracted to assess the disproportionality reporting between cases and non-cases. The analysis of disproportionality allows to detect a higher reporting frequency of a certain adverse event with the investigated drug in comparison with a reference represented by the overall database or another specific drug [18]. Then, we repeated and restricted the search to reports indicating TZP as primary suspect drug for each AE with a positive signal of disproportionality at initial evaluation. Also, search was filtered for reports regarding female or male and adult (aged 18–65 years) or elderly (aged > 65 years) patients for all AE showing disproportionate reporting. The OpenVigil 2 × 2 contingency table (https://openvigil.pharmacology.uni-kiel.de/contingency-table-calculator.php) was used to assess difference in AE reporting according to age or gender retrieving chi-squared values with Yates’ correction, PRR and ROR. This tool was also used to assess differences in AE reporting in TZP users compared to patients on insulin ("insulin (human)" "insulin lispro" "insulin aspart" "insulin glulisine" "insulin glargine" "insulin detemir" "insulin degludec" "insulin icodec"), GLP-1RA (“exenatide”, “lixisenatide”, “liraglutide”, “albiglutide”, “semaglutide”, “dulaglutide”) as a group and individually, sodium-glucose cotransporter-2 inhibitors (SGLT-2i: “dapagliflozin”, “canagliflozin”, “empagliflozin”, “ertugliflozin”, “ipragliflozin”, “sotagliflozin”, “luseogliflozin”, “bexagliflozin”), and metformin. Concomitant use of TZP was excluded. In addition, we performed a sensitivity analysis by excluding concomitant insulin or GLP-1RA use when comparing TZP with non-insulin and non-incretin-based treatments, respectively.
Figures were created with RStudio 2023.12.1 Build 402 (MacOS, Apple Silicon version), R 4.3.3 (2024-02-29) and R package ggplot 2 version 3.4.4.
Results
TZP was associated with a total of 20,409 reports related to 1432 AE, 116 of which fulfilled Evans’ criteria. Interestingly, 44 out of 116 (38%) AE concerned administration site and procedural complications [i.e., injection site injury, ROR 52.78, 95% confidence interval (CI) 45.75–60.89; incorrect dose administered, ROR 43.66, 95% CI 42.33–45.01], 20 (17%) GI disorders and 14 (12%) nutrition and metabolism disorders (i.e. “starvation”, ROR 41.57, 95% CI 27.22–63.48) (Supplementary Table 2).
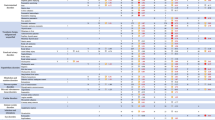
Tirzepatide vs. all other drugs
With respect to the pre-specified HLT, 397 AE were classified as “gastrointestinal signs and symptoms nec”, 236 as “gastrointestinal disorders nec”, 2895 as “nausea and vomiting symptoms”, 678 as “dyspeptic signs and symptoms”, 1085 as “diarrhoea (excl infective)”, 890 as “gastrointestinal atonic and hypomotility disorders nec”, 361 as “flatulence, bloating and distention”, 578 as “gastrointestinal and abdominal pains (excl oral and throat)”, 218 as “acute and chronic pancreatitis”, 56 as “cholecystitis and cholelithiasis”, 9 as “bile duct infections and inflammations”, 12 as “diabetic complications ophthalmic”, 20 as “thyroid neoplasms”, and 25 as “thyroid disorders nec”. Disproportionate reporting of several adverse GI events was detected. Specifically, “abdominal discomfort” (ROR 2.20, 95% CI 1.97–2.45), “abdominal pain upper” (ROR 2.25, 95% CI 2.04–2.49), “abdominal rigidity” (ROR 3.39, 95% CI 1.61–7.13), “constipation” (ROR 4.12, 95% CI 3.81–4.45), “diarrhoea” (ROR 2.15, 95% CI 2.02–2.29), “dyspepsia” (ROR 4.02, 95% CI 3.61–4.48), “early satiety” (ROR 2.96, 95% CI 1.23–7.13), “eructation” (ROR 30.25, 95% CI 27.38–33.42), “flatulence” (ROR 4.31, 95% CI 3.75–4.96), “food poisoning” (ROR 3.59, 95% CI 2.12–6.07), “gastrooesophageal reflux” (ROR 2.41, 95% CI 2.06–2.82), “gastrointestinal disorder” (ROR 2.73, 95% CI 2.37–3.15), “impaired gastric emptying” (ROR 13.3, 95% CI 10.7–16.7), “pancreatitis” (ROR 3.63, 95% CI 3.15–4.19), “pancreatitis necrotising” (ROR 2.81, 95% CI 1.26–6.26), “biliary colic” (ROR 2.83, 95% CI 1.41–5.67), “nausea” (ROR 4.01, 95% CI 3.85–4.19), “vomiting” (ROR 2.44, 95% CI 2.29–2.61) and “vomiting projectile” (ROR 4.07, 95% CI 2.11–7.85) were all likely related to the administration of TZP according to Evans’ criteria (Fig. 1). A positive signal was also detected for “diabetic retinopathy” (ROR 4.13, 95% CI 2.34–7.29) among “diabetic complications ophthalmic”, and for “medullary thyroid cancer” (ROR 13.67, 95% CI 4.35–42.96) and “thyroid mass” (ROR 4.48, 95% CI 2.47–8.12) among “thyroid neoplasms” and “thyroid disorders nec” (Fig. 1). Such associations persisted after restricting the analysis to TZP as primary suspect, with the exception of “pancreatitis necrotising” (Supplementary Table 3). No signal for other gallbladder and biliary-related AE was found (i.e., ROR 1.69, 95% CI 1.05–2.72, for cholecystitis; ROR 1.35, 95% CI 0.98–1.87, for cholelithiasis).
Disproportionately reported adverse events (AE) of interest for tirzepatide vs. all other drugs in the FAERS database. The forest plot shows reporting odds ratios (ROR) with 95% confidence intervals for gastrointestinal, pancreato-biliary, eye-related, and thyroid-related AE for tirzepatide vs. control drugs
Safety of tirzepatide according to age and gender
A greater number of AE reports were submitted for females (13,845) than for males (3578). However, females displayed a lower risk of “abdominal discomfort”, “diarrhoea”, “eructation”, “flatulence”, “gastrointestinal disorder”, “pancreatitis”, “biliary colic” and a greater risk of “nausea” compared to males (Fig. 2). Also, a greater number of AE reports were filed for individuals aged 18–65 years (6475) rather than above 65 years (896). Nonetheless, older patients exhibited a greater risk of “abdominal discomfort”, “abdominal pain upper”, “constipation”, “diarrhoea”, “dyspepsia”, “flatulence” and “thyroid mass” occurrence (Fig. 3).
Reporting odds ratio (ROR) of adverse events (AE) of interest for tirzepatide vs. all other drugs in females vs. males. The forest plot shows ROR with 95% confidence intervals for gastrointestinal, pancreato-biliary, eye-related, and thyroid-related AE for tirzepatide vs. control drugs in females vs. males. A ROR < 1.0 indicates a disproportional lower rate of AE among reports for females
Reporting odds ratio of adverse events (AE) of interest for tirzepatide vs. all other drugs in individuals aged > 65 vs. 18–65 years. The forest plot shows reporting odds ratios (ROR) with 95% confidence intervals for gastrointestinal, pancreato-biliary, eye-related, and thyroid-related AE for tirzepatide vs. control drugs in individuals aged > 65 years (old) vs. individuals aged 18–65 years (young). A ROR < 1.0 indicates a disproportional lower rate of AE among reports for individuals aged > 65 years
Tirzepatide vs. GLP-1RA
When compared to GLP-1RA as a class, TZP displayed a lower risk of “abdominal discomfort”, “abdominal pain upper”, “gastrooesophageal reflux disease”, “nausea”, “vomiting”, “vomiting projectile”, “pancreatitis”, “pancreatitis necrotising”, “thyroid mass” and “diabetic retinopathy” and a greater risk of “constipation”, “eructation” and “gastrointestinal disorder” (Fig. 4A). The overall GI tolerability of TZP appeared to be greater than semaglutide (Fig. 4B) and worse than lixisenatide and albiglutide (Supplementary Figs. 1 and 2). Some differences in GI AE were also detected vs. exenatide, liraglutide, and dulaglutide, roughly in line with the observations regarding GLP-1RA as a class (Supplementary Figs. 3, 4, and 5). No difference in the risk of “biliary colic” was described between TZP and GLP-1RA, although TZP was associated with reduced occurrence of “cholecystitis”, “cholecystitis acute”, “cholecystitis chronic” and “cholelithiasis” (Supplementary Table 4).
Reporting odds ratio (ROR) of adverse events (AE) of interest for tirzepatide vs. all glucagon-like peptide-1 receptor agonists (GLP-1RA, A), semaglutide (B), insulin (C), sodium-glucose cotransporter-2 inhibitors (SGLT-2i, D). The forest plot shows ROR with 95% confidence intervals for gastrointestinal, pancreato-biliary, eye-related, and thyroid-related AE for tirzepatide vs. all GLP-1RA (A), semaglutide (B), insulin (C), and SGLT-2i (D). A ROR < 1.0 indicates a disproportional lower rate of AE among reports for tirzepatide
TZP was associated with a lower risk of “diabetic retinopathy” vs. GLP-1RA as a class, which persisted vs. lixisenatide, liraglutide, semaglutide and dulaglutide, and following restriction of the analysis to exclude patients on concomitant insulin treatment (Fig. 4A, B; Supplementary Figs. 1, 3, 4, and 5). Also, TZP and GLP-1RA displayed a similar risk of “medullary thyroid cancer”, yet with a lower risk for TZP vs. liraglutide and semaglutide.
Tirzepatide vs. insulin and SGLT-2i
As expected, TZP was associated with a greater risk of GI AE vs. insulin and SGLT-2i (Fig. 4C, D). Notably, no disproportionate reporting of “pancreatitis” and “biliary colic” was observed vs. SGLT-2i, while a greater risk was described vs. insulin (ROR 1.58, 95% CI 1.37–1.82, for “pancreatitis”, and ROR 2.40, 95% CI 1.16–4.94, for “biliary colic”) (Fig. 4C, D).
TZP was associated with a similar risk of “diabetic retinopathy” (ROR 0.74, 95% CI 0.41-1.35) and “medullary thyroid cancer” (ROR 2.53, 95% CI 0.78-8.21) vs. SGLT-2i. With respect to insulin, TZP was associated with a lower risk of “diabetic retinopathy” (ROR 0.14, 95% CI 0.08–0.24) and a greater risk of “medullary thyroid cancer” (ROR 2.88, 95% CI 1.37–1.82). When restricting the analysis to exclude patients on concomitant GLP-1RA, a lower risk of “diabetic retinopathy” vs. insulin persisted (ROR 0.12, 95% CI 0.06–0.22).
Tirzepatide vs. metformin
With respect to metformin, TZP was associated with a greater risk of GI AE, a similar risk of “pancreatitis”, “pancreatitis necrotising”, “biliary colic”, “medullary thyroid cancer” and “thyroid mass” (Supplementary Fig. 6), and lower risk of “diabetic retinopathy” (ROR 0.41, 95% CI 0.23–0.72) (Supplementary Fig. 6). However, when restricting the analysis to exclude patients on concomitant insulin treatment, no difference was found between TZP and metformin in the risk of “diabetic retinopathy” (ROR 0.57, 95% CI 0.29–1.11).
Conclusions
Real-world data from the FAERS database confirmed that treatment with TZP could increase the risk of GI AE. Disproportionate reporting for “diabetic retinopathy” and “medullary thyroid cancer” was also detected, while no signal for gallbladder and biliary-related AE was found apart from “biliary colic”.
In line with data from the SURPASS program [3], nausea, diarrhoea, and vomiting were the most commonly reported GI AE (Supplementary Table 3). Constipation, eructation, abdominal pain, and dyspepsia also emerged as frequent complaints. As expected, TZP showed a greater risk of GI AE vs. metformin, SGLT-2i and insulin, and a similar GI tolerability profile compared to GLP-1RA. Interestingly, TZP showed a lower risk of “nausea” and “vomiting” compared to GLP-1RA. This finding may have a biological explanation, as GIP receptor agonism hindered malaise and vomiting related to GLP-1 receptor agonism in three animal models [19]. GIP receptors are expressed in gamma-aminobutyric acid (GABA) ergic neurons of the area postrema of the brainstem and promote the inhibition of neurons responsible for nausea and emesis [19]. Instead, a differential effect in gastric emptying delay is unlikely to be involved, as both animal and human studies showed effects of similar magnitude for long-acting GLP-1RA and TZP [20]. Also, optimal dose and dose escalation modalities might be crucial in maximizing efficacy and tolerability of TZP, as a slower dose escalation schedule with lower initial dose and smaller subsequent dose increments improved its GI tolerability [21]. Importantly, BW reduction with TZP occurred independently of GI AE, and TZP induced a greater BW loss vs. GLP-1RA despite a similar GI tolerability [3].
Our analysis did not detect disproportionate reporting of single gallbladder and biliary-related AE with TZP except for “biliary colic”, in line with a recent meta-analysis of the SURPASS RCT program describing a significant increase in the risk of the composite of gallbladder and biliary disease only if considered as a group [6]. In addition, we found that TZP had a more favorable profile compared to GLP-1RA, which are known to be associated with an increased yet small risk of gallbladder and biliary-related disorders both in patients treated for type 2 diabetes and obesity [22]. In fact, GLP-1RA hinder gallbladder motility and emptying by reducing cholecystokinin secretion [23]. Gasbjerg et al. showed that endogenous GIP, and not GLP-1, also induced gallbladder relaxation. Dedicated studies are needed to investigate whether GIP still affects gallbladder motility in the presence of diabetes and whether these effects are replicated by TZP, as with endogenous GLP-1 and GLP-1RA [24].
Being an incretin-based medication, TZP inherited GLP-1RA-related concerns of diabetic retinopathy worsening, which peaked especially following the dissemination of the SUSTAIN-6 trial results with subcutaneous semaglutide [25]. However, this association remains controversial as meta-analyses of RCT and real-world data from the FAERS database found that GLP-1RA did not increase the risk of diabetic retinopathy outcomes vs. placebo or other glucose-lowering medications [26]. Instead, HbA1c reduction was associated with increased risk of diabetic retinopathy in a meta-regression of GLP-1RA cardiovascular outcome trials [27]. These concerns have affected the design of all subsequent trials with incretin-based medications, which in most cases excluded participants with proliferative retinopathy or retinopathy requiring immediate intervention. The ongoing FOCUS trial (NCT03811561) was also designed to assess the effects of semaglutide on diabetic retinopathy over a 5-year follow-up. Our analysis identified only 12 “diabetic retinopathy” events; TZP was associated with an increased risk of “diabetic retinopathy” compared to all other drug but with a consistently lower risk vs. GLP-1RA and insulin use, which could represent a proxy for more advanced stages of disease. A meta-analysis of the SURPASS program RCT showed a neutral effect of TZP on diabetic retinopathy, although an exiguous number of events occurred and high risk patients were excluded from these trials [28]. The role of endogenous GIP and TZP in the development of diabetic retinopathy is unknown in humans, while experiments in diabetic rats are limited to the description of GIP and GIP receptor expression in the retina [29].
The risk of medullary thyroid cancer was investigated due to the presence of a black box warning for GLP-1RA in patients at risk for this condition, despite conflicting evidence [30]. A positive signal for medullary thyroid cancer was found for TZP, although based on only 3 events. However, a higher expression of GIP receptor was found in tumor rather than normal tissue in rats and human specimens of medullary thyroid cancer, and the stimulation of GIP receptor resulted in increased secretion of calcitonin [31]. The implications of the GIP/GIP receptor axis stimulation on the occurrence of medullary thyroid cancer and patients’ prognosis remains to be elucidated.
As frequently observed with pharmacovigilance databases [32], we found that a greater number of reports of AE with TZP concerned females. This could be due to several reasons, such as a different access to healthcare services, biological differences in AE occurrence and perception between genders, and pre-existing social and structural barriers [32]. In our analysis, females appeared to be at a lower risk of some GI-related AE vs. males, although it should be acknowledged that approximately 2900 reports were not informative on patients’ gender. These findings conflict with data coming mostly from Asian studies showing that GI AE with GLP-1RA are more common in females [33] and require further confirmation in studies with TZP enrolling patients with diverse ethnicity.
Patients’ age was also underreported, as this information was missing in approximately 13,000 reports. We found that elderly patients displayed a greater risk of several GI AE and “thyroid mass”, in agreement with the notion that frailty and polypharmacy might predispose to the development of AE. Moreover, aging induces GI changes which may facilitate GI AE occurrence, and is also a well-known risk factor for cancer development [34].
The main limitations of this work are related to the intrinsic features of the FAERS database. Firstly, the FAERS includes spontaneous reports of AE without necessarily implying a cause-effect relationship with the designated primary suspect drug. Moreover, not only healthcare professionals, but also patients and their families, representatives, and even manufacturers are allowed to file AE reports. This could lead to duplicates and incomplete reporting, with clinically relevant information such as drug dose, indication for prescription and patients’ gender and age often missing or being inappropriately transmitted. AE reporting could also be affected by public awareness of certain drug-AE associations, ethnicity, geography, and timing of approval and introduction to the market [35]. Moreover, discrimination of oral or injectable semaglutide and daily or weekly exenatide was often unfeasible, preventing from assessing whether differences vs. TZP were due to the pharmacokinetic and pharmacodynamic properties of oral vs. injectable and short vs. long acting formulations, respectively. Finally, available data refer to approximately the first 16 months of TZP availability on the U.S. market, and this could at least partially account for the retrieval of a small number of less common non-GI-related AE, demanding a cautious approach to the interpretation of these findings.
In summary, real-world evidence from the FAERS database depicts a reassuring safety profile for TZP. While exhibiting impressive efficacy, TZP maintains a similar GI tolerability compared to the widely used class of GLP-1RA without increased risk of pancreatitis, diabetic retinopathy, and medullary thyroid cancer.
Data availability
The data that support the findings of this study are available from the corresponding author, F.G., upon reasonable request.
References
American Diabetes Association Professional Practice Committee (2024) 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes-2024. Diabetes Care 47:S158–S178. https://doi.org/10.2337/dc24-S009
Caruso I, Di Gioia L, Di Molfetta S, Cignarelli A, Palmer SC, Natale P et al (2023) Glucometabolic outcomes of GLP-1 receptor agonist-based therapies in patients with type 2 diabetes: a systematic review and network meta-analysis. EClinicalMedicine 64:102181. https://doi.org/10.1016/j.eclinm.2023.102181
Patel H, Khunti K, Rodbard HW, Bajaj HS, Bray R, Kindracki Z et al (2024) Gastrointestinal adverse events and weight reduction in people with type 2 diabetes treated with tirzepatide in the SURPASS clinical trials. Diabetes Obes Metab 26:473–481. https://doi.org/10.1111/dom.15333
Trujillo J (2020) Safety and tolerability of once-weekly GLP-1 receptor agonists in type 2 diabetes. J Clin Pharm Ther 45(Suppl 1):43–60. https://doi.org/10.1111/jcpt.13225
Bezin J, Gouverneur A, Pénichon M, Mathieu C, Garrel R, Hillaire-Buys D et al (2023) GLP-1 receptor agonists and the risk of thyroid cancer. Diabetes Care 46:384–390. https://doi.org/10.2337/dc22-1148
Zeng Q, Xu J, Mu X, Shi Y, Fan H, Li S (2023) Safety issues of tirzepatide (pancreatitis and gallbladder or biliary disease) in type 2 diabetes and obesity: a systematic review and meta-analysis. Front Endocrinol 14:1214334. https://doi.org/10.3389/fendo.2023.1214334
Gao L, Lee BW, Chawla M, Kim J, Huo L, Du L et al (2023) Tirzepatide versus insulin glargine as second-line or third-line therapy in type 2 diabetes in the Asia-Pacific region: the SURPASS-AP-Combo trial. Nat Med 29:1500–1510. https://doi.org/10.1038/s41591-023-02344-1
Kadowaki T, Chin R, Ozeki A, Imaoka T, Ogawa Y (2022) Safety and efficacy of tirzepatide as an add-on to single oral antihyperglycaemic medication in patients with type 2 diabetes in Japan (SURPASS J-combo): a multicentre, randomised, open-label, parallel-group, phase 3 trial. Lancet Diabetes Endocrinol 10(9):634–644. https://doi.org/10.1016/s2213-8587(22)00187-5
Rosenstock J, Wysham C, Frías JP, Kaneko S, Lee CJ, Fernández Landó L et al (2021) Efficacy and safety of a novel dual GIP and GLP-1 receptor agonist tirzepatide in patients with type 2 diabetes (SURPASS-1): a double-blind, randomised, phase 3 trial. Lancet 398:143–155. https://doi.org/10.1016/S0140-6736(21)01324-6
Frías JP, Davies MJ, Rosenstock J, Pérez Manghi FC, Fernández Landó L, Bergman BK et al (2021) Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. N Engl J Med 385:503–515. https://doi.org/10.1056/NEJMoa2107519
Ludvik B, Giorgino F, Jódar E, Frias JP, Fernández Landó L, Brown K et al (2021) Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in patients with type 2 diabetes (SURPASS-3): a randomised, open-label, parallel-group, phase 3 trial. Lancet 398:583–598. https://doi.org/10.1016/S0140-6736(21)01443-4
Del Prato S, Kahn SE, Pavo I, Weerakkody GJ, Yang Z, Doupis J et al (2021) Tirzepatide versus insulin glargine in type 2 diabetes and increased cardiovascular risk (SURPASS-4): a randomised, open-label, parallel-group, multicentre, phase 3 trial. Lancet 398:1811–1824. https://doi.org/10.1016/S0140-6736(21)02188-7
Dahl D, Onishi Y, Norwood P, Huh R, Bray R, Patel H et al (2022) Effect of subcutaneous tirzepatide vs placebo added to titrated insulin glargine on glycemic control in patients with type 2 diabetes: the SURPASS-5 randomized clinical trial. JAMA 327:534–545. https://doi.org/10.1001/jama.2022.0078
Rosenstock J, Frías JP, Rodbard HW, Tofé S, Sears E, Huh R et al (2023) Tirzepatide vs insulin lispro added to basal insulin in type 2 diabetes: the SURPASS-6 randomized clinical trial. JAMA 330:1631–1640. https://doi.org/10.1001/jama.2023.20294
Inagaki N, Takeuchi M, Oura T, Imaoka T, Seino Y (2022) Efficacy and safety of tirzepatide monotherapy compared with dulaglutide in Japanese patients with type 2 diabetes (SURPASS J-mono): a double-blind, multicentre, randomised, phase 3 trial. Lancet Diabetes Endocrinol 10(9):623–633. https://doi.org/10.1016/s2213-8587(22)00188-7
Patel A, Billot L (2017) Reality and truth: balancing the hope and the hype of real-world evidence. Circulation 136(3):260–262. https://doi.org/10.1161/CIRCULATIONAHA.117.029233
Sarangdhar M, Tabar S, Schmidt C, Kushwaha A, Shah K, Dahlquist JE et al (2016) Data mining differential clinical outcomes associated with drug regimens using adverse event reporting data. Nat Biotechnol 34:697–700. https://doi.org/10.1038/nbt.3623
Evans SJ, Waller PC, Davis S (2001) Use of proportional reporting ratios (PRRs) for signal generation from spontaneous adverse drug reaction reports. Pharmacoepidemiol Drug Saf 10:483–486. https://doi.org/10.1002/pds.677
Borner T, Geisler CE, Fortin SM, Cosgrove R, Alsina-Fernandez J, Dogra M et al (2021) GIP receptor agonism attenuates GLP-1 receptor agonist-induced nausea and emesis in preclinical models. Diabetes 70:2545–2553. https://doi.org/10.2337/db21-0459
Urva S, Coskun T, Loghin C, Cui X, Beebe E, O’Farrell L et al (2020) The novel dual glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 (GLP-1) receptor agonist tirzepatide transiently delays gastric emptying similarly to selective long-acting GLP-1 receptor agonists. Diabetes Obes Metab 22:1886–1891. https://doi.org/10.1111/dom.14110
Frias JP, Nauck MA, Van J, Benson C, Bray R, Cui X et al (2020) Efficacy and tolerability of tirzepatide, a dual glucose-dependent insulinotropic peptide and glucagon-like peptide-1 receptor agonist in patients with type 2 diabetes: a 12-week, randomized, double-blind, placebo-controlled study to evaluate different dose-escalation regimens. Diabetes Obes Metab 22:938–946. https://doi.org/10.1111/dom.13979
He L, Wang J, Ping F, Yang N, Huang J, Li Y et al (2022) Association of glucagon-like peptide-1 receptor agonist use with risk of gallbladder and biliary diseases: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med 182:513–519. https://doi.org/10.1001/jamainternmed.2022.0338
Rehfeld JF, Knop FK, Asmar A, Madsbad S, Holst JJ, Asmar M (2018) Cholecystokinin secretion is suppressed by glucagon-like peptide-1: clue to the mechanism of the adverse gallbladder events of GLP-1-derived drugs. Scand J Gastroenterol 53:1429–1432. https://doi.org/10.1080/00365521.2018.1530297
Gasbjerg LS, Helsted MM, Hartmann B, Sparre-Ulrich AH, Veedfald S, Stensen S et al (2020) GIP and GLP-1 receptor antagonism during a meal in healthy individuals. J Clin Endocrinol Metab 105(3):dgz175. https://doi.org/10.1210/clinem/dgz175
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jódar E, Leiter LA et al (2016) Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Eng J Med 375(19):1834–1844. https://doi.org/10.1056/NEJMoa1607141
Fadini GP, Sarangdhar M, Avogaro A (2018) Glucagon-like peptide-1 receptor agonists are not associated with retinal adverse events in the FDA Adverse Event Reporting System. BMJ Open Diabetes Res Care 6(1):e000475. https://doi.org/10.1136/bmjdrc-2017-000475
Bethel MA, Diaz R, Castellana N, Bhattacharya I, Gerstein HC, Lakshmanan MC (2021) HbA change and diabetic retinopathy during GLP-1 receptor agonist cardiovascular outcome trials: a meta-analysis and meta-regression. Diabetes Care 44:290–296. https://doi.org/10.2337/dc20-1815
Popovic DS, Patoulias D, Karakasis P, Koufakis T, Papanas N (2024) Effect of tirzepatide on the risk of diabetic retinopathy in type 2 diabetes. Diabetes Obes Metab 26(6):2497–2500. https://doi.org/10.1111/dom.15535
Seino Y, Yabe D (2013) Glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1: Incretin actions beyond the pancreas. J Diabetes Investig 4(2):108–130. https://doi.org/10.1111/jdi.12065
Espinosa De Ycaza AE, Brito JP, McCoy R, Shao H, Singh Ospina NM (2024) GLP-1 receptor agonists and thyroid cancer: a narrative review. Thyroid 34(4):403–418. https://doi.org/10.1089/thy.2023.0530
Regazzo D, Bertazza L, Galletta E, Barollo S, Mondin A, Zovato S et al (2022) The GIP/GIPR axis in medullary thyroid cancer: clinical and molecular findings. Endocr Relat Cancer 29(5):273–284. https://doi.org/10.1530/ERC-21-0258
Lee KMN, Rushovich T, Gompers A, Boulicault M, Worthington S, Lockhart JW et al (2023) A gender hypothesis of sex disparities in adverse drug events. Soc Sci Med 339:116385. https://doi.org/10.1016/j.socscimed.2023.116385
Rentzeperi E, Pegiou S, Koufakis T, Grammatiki M, Kotsa K (2022) Sex differences in response to treatment with glucagon-like peptide 1 receptor agonists: opportunities for a tailored approach to diabetes and obesity care. J Pers Med 12(3):454. https://doi.org/10.3390/jpm12030454
Dumic I, Nordin T, Jecmenica M, Stojkovic Lalosevic M, Milosavljevic T, Milovanovic T (2019) Gastrointestinal tract disorders in older age. Can J Gastroenterol Hepatol 2019:6757524. https://doi.org/10.1155/2019/6757524
Zhou C, Peng S, Lin A, Jiang A, Peng Y, Gu T et al (2023) Psychiatric disorders associated with immune checkpoint inhibitors: a pharmacovigilance analysis of the FDA Adverse Event Reporting System (FAERS) database. EClinicalMedicine 59:101967. https://doi.org/10.1016/j.eclinm.2023.101967
Acknowledgements
We acknowledge Dr. Ruwen Böhm and Dr. Mayur Sarangdhar for providing prompt assistance and information on OpenVigil 2.1-MedDRA-v24 and AERSMine, respectively.
Funding
Open access funding provided by Università degli Studi di Bari Aldo Moro within the CRUI-CARE Agreement. We acknowledge co-funding from the Fondazione per la Ricerca Biomedica “Saverio e Isabella Cianciola” and from Next Generation EU, in the context of the National Recovery and Resilience Plan, Investment PE8 – Project Age-It: “Ageing Well in an Ageing Society”. This resource was co-financed by the Next Generation EU [DM 1557 11.10.2022]. The views and opinions expressed are only those of the authors and do not necessarily reflect those of the European Union or the European Commission; neither the European Union nor the European Commission can be held responsible for them.
Author information
Authors and Affiliations
Contributions
I.C., A.C. and F.G. conceived this work. I.C., L.D.G., M.C., and S.D.M. researched data. I.C. and L.D.G. performed statistical analysis. I.C. wrote the first draft of the manuscript. L.D.G., M.C., S.D.M., and F.G. contributed to discussion. A.C., G.P.S., L.L., and F.G. reviewed and edited the manuscript. All authors approved the final version of the manuscript. F.G. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflicts of interest
AC: AstraZeneca, Eli Lilly, Novo Nordisk, Roche Diagnostics, Sanofi Aventis. FG: AstraZeneca, Boehringer-Ingelheim, Eli Lilly, Lifescan, Medimmune, Merck Sharp & Dohme, Medtronic, Novo Nordisk, Roche Diabetes Care, Sanofi Aventis. GPS: Amgen, Amryt, Eli Lilly, Farmitalia, Novo Nordisk, Sanofi; IC: Eli Lilly, Novo Nordisk; LDG: Eli Lilly, Lusofarmaco, Medtronic, MOVI SpA, Novo Nordisk, Roche Diabetes Care, Sanofi Aventis. LL: Abbott, AstraZeneca, Boehringer-Ingelheim, Eli Lilly, Merck Sharp & Dohme, Medtronic, Menarini, MOVI SpA, Mundipharma, Novo Nordisk, Roche Diabetes Care, Sanofi Aventis, Terumo. MC: AstraZeneca, Eli Lilly, Guidotti, Novo Nordisk; SDM: Ascensia Diabetes Care, Eli Lilly, MOVI SpA, Roche Diabetes Care.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Caruso, I., Di Gioia, L., Di Molfetta, S. et al. The real-world safety profile of tirzepatide: pharmacovigilance analysis of the FDA Adverse Event Reporting System (FAERS) database. J Endocrinol Invest (2024). https://doi.org/10.1007/s40618-024-02441-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40618-024-02441-z