Abstract
Background
People with metabolically healthy (MHO) and metabolically unhealthy obesity (MUO) differ for the presence or absence of cardio-metabolic complications, respectively.
Objective
Based on these differences, we are interested in deepening whether these obesity phenotypes could be linked to changes in microbiota and metabolome profiles. In this respect, the overt role of microbiota taxa composition and relative metabolic profiles is not completely understood. At this aim, biochemical and nutritional parameters, fecal microbiota, metabolome and SCFA compositions were inspected in patients with MHO and MUO under a restrictive diet regimen with a daily intake ranging from 800 to 1200 kcal.
Methods
Blood, fecal samples and food questionnaires were collected from healthy controls (HC), and an obese cohort composed of both MHO and MUO patients. Most impacting biochemical/anthropometric variables from an a priori sample stratification were detected by applying a robust statistics approach useful in lowering the background noise. Bacterial taxa and volatile metabolites were assessed by qPCR and gas chromatography coupled with mass spectrometry, respectively. A targeted GC–MS analyses on SCFAs was also performed.
Results
Instructed to follow a controlled and restricted daily calorie intake, MHO and MUO patients showed differences in metabolic, gut microbial and volatilome signatures. Our data revealed higher quantities of specific pro-inflammatory taxa (i.e., Desulfovibrio and Prevotella genera) and lower quantities of Clostridium coccoides group in MUO subset. Higher abundances in alkane, ketone, aldehyde, and indole VOC classes together with a lower amount of butanoic acid marked the faecal MUO metabolome.
Conclusions
Compared to MHO, MUO subset symptom picture is featured by specific differences in gut pro-inflammatory taxa and metabolites that could have a role in the progression to metabolically unhealthy status and developing of obesity-related cardiometabolic diseases. The approach is suitable to better explain the crosstalk existing among dysmetabolism-related inflammation, nutrient intake, lifestyle, and gut dysbiosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is a worldwide spread chronic condition characterized by an unbalanced between energy intake and disposal which leads to an excessive adipose tissue expansion as well as to develop a low-grade inflammation state and long-term metabolic consequences. The incidence of obesity is continuously growing and the pathology will affect one adult out of five in 2025 [1]. In this condition, the limited expandability of adipose tissue leads to increased fat accumulation in both visceral and ectopic compartments thus increasing the risk of metabolic disorders including coronary heart disease, hypertension and stroke, cancer, type 2 diabetes (T2D), dyslipidaemia [2]. Although some critical biochemical pathways dedicated to macronutrients utilization and autoimmune or inflammatory response [3] are impaired under obesity, not all obese patients develop inflammation and metabolic derangements. Indeed, recent findings describe two different phenotypes of obesity: metabolically healthy obesity (MHO), characterized by the absence of metabolic alterations, and metabolically unhealthy obesity (OB), characterized by the presence of visceral adiposity in association with least two co-morbidities [4].
Obesity is a multifactorial disease whose onset and progression are often associated with a reduction in gut alpha-diversity as well as changes in specific species abundances. Different studies reported that eubiosis is necessary for the maintenance of energy balance and lipid deposition in adipose tissues [5]. Indeed, in the presence of intestinal dysbiosis a pronounced energy absorption and accumulation were observed which in turn result in weight gain [6]. The main microbiota-derived regulators of energy balance and bodyweight are the short-chain fatty acids (SCFAs) which control satiety or hunger feelings by promoting the release of peptide YY (PYY), ghrelin, insulin, and glucagon-like peptide 1 (GLP-1), all factors directly involved in the regulation of appetite, food intake, and insulin secretion [7]. SCFAs also affect the intestinal functionality by regulating the tight junction and mucin layer, and may lead to chronic inflammation and metabolic dysfunction at long-term [8]. Furthermore, these compounds have been previously correlated with clinical [9] (e.g., transaminase, HbA1c, cholesterol) and anthropometric parameters, including BMI or weight, in presence of dysmetabolic conditions and inflammation [10].
Nowadays, differences in gut microbiota and fecal metabolites in MHO and MUO individuals were not deeply explored yet. Undoubtedly, targeting VOC profiles can help in elucidating the crosstalk among dysmetabolism-related inflammation, nutrient intake, lifestyle, and gut dysbiosis [8]. At this aim, we investigated clinical and dietary parameters, gut microbiota and fecal volatilome, in subjects affected by MHO, MUO and in healthy controls (HC). For the first time, our study highlighted statistically significant differences in metabolic, taxonomic and volatilome signature between MUO and MHO patients who underwent the same restrictive caloric intake.
Methods
Study groups
A cross-sectional prospective observational study based on subjects affected by metabolically healthy obesity (MHO) and metabolically unhealthy obesity (MUO) was here conducted. More precisely, MHO and MUO subsets were composed of 18 and 27 patients, respectively. A group of 12 healthy control subjects (HC) was included. All volunteers agreed to undergo a comprehensive clinical evaluation based on the protocol approved by the Independent Ethical Committee (IEC). The study and the informed consent process were carried out in accordance with the ethical principles of the Declaration of Helsinki, the Regulation (EU) 2016/679, the Legislative Decree 101/2018, the International Ethical Guidelines for Biomedical Research involving subjects CIOMS-WHO (2016), and the Recommendation on Research on Biological Materials of Human Origin Rec (2006). Subjects were recruited from a clinical center located at University-Hospital Consortium Polyclinic of Bari—Department of Precision and Regenerative Medicine and Ionian Area, Section of Internal Medicine, Endocrinology, Andrology and Metabolic Diseases.
HC subjects were enrolled according to the following inclusion criteria: 18–70 years old, BMI range between 18.5 and 27.0 kg/m2, adherence to an omnivorous diet. Subjects with obesity followed the same age and diet criteria but presented a BMI ≥ 30 kg/m2. Moreover, MUO individuals were characterized by other comorbidities including insulin-resistance, prediabetes or T2D, dyslipidaemia, cardiovascular diseases (hypertension), or respiratory diseases (obstructive sleep apnoea). On the other hand, as defined, MHO patients were featured by only one or no comorbidity cardio-metabolic or respiratory diseases [4]. Furthermore, among the exclusion criteria we considered: the suffering from current or previous infectious diseases (caused by HAV, HBV, HCV, HIV, Cytomegalovirus, and Epstein-Barr virus), chronic liver disease, history of Clostridium difficile infection, recent pharmacological therapy (3 months before the study), immunosuppressant therapy, chemotherapy, chronic therapy with proton pump inhibitors, recent use of probiotics (3 months before the study), use of laxatives, drugs or supplements, history of organ transplant, recent appearance of diarrhea, chronic diarrhea, chronic constipation, previous gastrointestinal surgery (e.g. gastric bypass), or recurrent urinary tract infections (three cases per year). Moreover, in compliance with the above mentioned protocol, study participants must not have suffered from acute cardiovascular diseases (myocardial infarction, stroke), arterial hypertension or chronic gastrointestinal diseases or systemic inflammatory diseases, did not have an estimated Glomerular Filtration Rate (eGFR) less than 60 mL/minute, did not have a diagnosis of nephropathy, or previous history of malignancy (< 5 years), autoimmune diseases or a history of chronic and systemic autoimmune disorders, and neurodegenerative disorders with psychiatric conditions. In addition, pregnant or lactating women, health workers, and anyone working with animals were excluded from the study. In addition to the inclusion/exclusion criteria listed here, all enrolled subjects had a diet regimen ranging from 800 to 1200 kcal in terms of average daily intake (Fig. 1). This was useful in balancing the effect of diet on gut microbiota metabolism on different subjects. Considering that generally healthy subjects have a higher energy metabolism than MHO and MUO patients [11], who have a lifestyle that is associated with sedentary lifestyle, we also considered as inclusion criteria a calorie intake threshold of 1000 kcal/day. The threshold was used to stratify HC individuals versus patients with obesity.
Experimental design. A cross-sectional prospective observational study was performed in three different cohorts: healthy (HC), metabolically healthy obesity (MHO), and metabolically unhealthy obesity (MUO). During the first visit, subjects were addressed to clinical assessment and hypocaloric diet (800–1200 kcal). After 14 days, patients underwent to a second visit for SARS-COV-2 test, blood analysis and fecal samples collection
Clinical biochemical analysis
At first medical examination, volunteers provided their signed informed consent, they filled out an anamnestic questionnaire, and they were subjected to the following procedures: evaluation of inclusion and exclusion criteria, ID assignment, and medical history evaluation. Kit for fecal samples collection were delivered to eligible participants. Fecal samples were collected in two devices with RNAlater™ Stabilization Solution (Sigma-Aldrich), ratio 1:1. One sample was used both to carry out analysis of volatile profile using Gas Chromatography coupled with Mass Spectrometry (GC–MS) and to characterize the microbiota composition based on quantitative PCR technique. In addition, participants received instructions on how to register their dietary intake by completing a 3-day food questionnaire, including a weekend day.
During the second examination, participants delivered fecal samples and provided the completed 3-day diet record. In addition, the following procedures were executed: blood test analyses, evaluation of new signs or symptoms (filling a new amnestic questionnaire), and molecular test for SARS-COV-2 (Fig. 1). Biological material from suitable volunteers was used for biobank stocking and for experimental research purposes. Medical centers stocked fecal aliquots at − 80 °C and provided for their transfer in dry ice to the Department of Soil, Plant and Food Science (DiSSPA) at University of Bari.
Food questionnaire analysis
To avoid exogenous confounding factors that could have affected the composition of the microbiota, 14 days before recruitment all subjects were invited to have a dietary caloric intake of approximately 1000 kcal. Both MUO and MHO patients showed high compliance to diet as they were candidate for bariatric surgery requiring a consolidated pre-operative weight loss through a very low calorie diet. In addition, to investigate dietary habits, subjects have drawn up a three-day food questionnaire (two working days and one in the weekend of the second week). Food questionnaires were analysed using the WinFood® software. Averages of diet nutritional values (daily caloric intake, macronutrients, and micronutrients) were returned as outputs.
Fecal volatilomics, real time PCR, and statistical analyses
Details relative to fecal volatilome analysis, and real time PCR as well as statistical methods used have been included within the Online Supporting Information.
Results
Subject characteristics
According to the adopted inclusion criteria, 12 HC, 18 MHO, and 27 MUO subjects were enrolled in our cross-sectional prospective observational study. Patient anthropometric measurements/descriptions together with biochemical gathered parameters were reported in Table 1.
Participants had an average age ranging between 32 and 53 years. No significant differences in age distribution have been observed between both obesity phenotypes even though MUO group appears to have an older age trend as compared to MHO. Nevertheless, as indicated by the high standard deviation in each group, a high heterogeneity marked the age values. In addition, both MUO and MHO had a similar disease course length, considering that we enrolled patients suffering from obesity up to 5 years. After performing a two-group corrected statistical comparison, weight and BMI values were significantly higher in MHO and MUO subjects as compared to HC (Table 1).
Minor significant differences emerged when biochemical parameters from HC and MHO subjects were compared, i.e., Alpha2 and Beta1 globulins, resulted higher in MHO patients. Interestingly, some parameters differentiated the two obese patient subsets. In detail, the MUO subset reported significant higher levels of glycated haemoglobin (HbA1c), homeostatic model assessment for insulin resistance (HOMA-IR) index, total cholesterol, triglycerides, AST and ALT aminotransferases, and fasting blood glucose (FBG), whereas MHO showed higher level of GFR and albumin. Noteworthy, as compared to HC, MUO exhibited statistically significant differences dealing with the quantity of white blood cells, platelets, insulinemia, C-reactive protein (CRP), high-sensitivity CRP (hs-CRP), erythrocyte sedimentation rate (ESR), HOMA-IR index, albumin/creatinine ratio (ACR), triglycerides, AST and ALT aminotransferases, calcemia, and thyroid-stimulating hormone (TSH), all parameters with higher levels in MUO subjects. On the contrary, 25-OH Vitamin D, albumin/globulin ratio (A/G ratio), and albumin resulted lower in MUO as compared to HC.
Next, to highlight the most impacting variables which could influence the stratification of the analysed samples, a pattern matrix analysis was performed.
Thus, based on Rotated factor loadings the total set of 16 identified latent variables was reduced into three factors that can be attributed to different processes/profiles (Table 2). We chose to discuss those variables with loading greater than 0.5 and with uniqueness lower than 0.5, where 1 represents commonality. Due to the heterogeneous nature of measured parameters, a mixture of hormonal, anthropometric and biochemical variables constitute each identified factor.
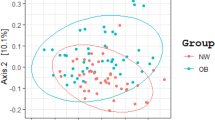
Discriminant analysis of principal components
A discriminant analysis of principal components (DAPC) was performed to understand if, based on variable loading, a sample stratification subsists without any group assignment. As emerged from the BIC curve (Supplementary Fig. S1) the better model provides for the separation of samples into three a priori clusters. When sample were “a posterior” assigned to groups, the three cohorts of subjects (HC, MHO, and MUO) plotted in three differentiated groups (Fig. 2A) and confirmed the a priori group stratification. The DAPC loading plot evidenced those variables (Fig. 2B) that had the greatest impact i.e., BMI, calcemia, erythrocyte sedimentation rate (ESR), CRP, total testosterone (TT), testosterone (T) free, thyroxine (FT4), and follicle stimulating hormone (FSH).
Food questionnaires analysis
The nutritional values of volunteer’ diets have been estimated and results were reported in Supplementary Table S1. As expected, the whole average caloric intakes were similar in the three groups (P-value > 0.05).
Some statistically significant differences emerged for macronutrient and micronutrient values. In detail, two-group statistics elucidated how compared to HC volunteers, MUO and MHO diets reported greater amount of starch, edible part, total mineral salts, vitamin B1 (Thiamine), C18:1 oleic, and a lower amount of manganese. Moreover, compared to controls, MUO diets exhibited significantly lower quantities of sodium, potassium, iodine, and alpha-tocopherol, and higher cysteine.
By comparing diets from the two sub-cohorts, MUO showed higher quantities of cystine and C22:0 behenic acid, whereas MHO diet was characterized by greater quantities of tyrosine, vitamin B3 (niacin), and vitamin B6 (pyridoxine).
Fecal volatilome
VOCs from fecal samples were analysed and quantified using HS-SPME GC–MS analyses. One hundred and seventeen volatile metabolites, ascribed to aldehyde, ester, ketone, indole, terpene, and alkane classes, were overall identified. Specifically, 112 volatiles were harboured by HC, 98 by the MHO group, and 96 by the MUO group. Eighty-nine compounds out of the total had the 100% of prevalence with respect to all the evaluated groups, whereas 7 of them (i.e., 2-methyl-1-butanol, trimethyl-pyrazine, propanoic acid butyl ester, butanoic acid-2-methylpropyl ester, dimethyl pentasulfide, acetic acid butyl ester, and 3-phenylpropanol) were absent in the two cohorts of obesity.
A list of statistically significant VOCs emerged when groups were compared by meaning of non-parametric Wilcoxon rank-sum test combined with fold change (FC) analysis. Moreover, as shown in the volcano plot (Fig. 3A), the MHO group presented lower quantity of tetradecane, 2H-indol-2-one-1,3-dihydro, 2-tridecanone, benzeneacetaldehyde, butanal-3-methyl-2, and gamma terpinene versus HC. Compared to the healthy group, MUO subjects showed greater amount of nonanoic acid, gamma terpinene, cyclohexanecarboxylic acid, pentanoic acid, butyl ester, alpha phelladrene, and humulene and an up-regulation of 2-pentadecanone, 2-undecanone and 2-hexadecanone (Fig. 3B). Finally, lower levels of nonadecane, indole, 1H-pyrrole-2,5-dione, 3-ethyl-4-methyl, 2-pentadecanone, 2-undecanone, and 2-hexadecanone were observed in MHO as compared to MUO (Fig. 3C).
Statistically significant VOCs emerged from non-parametric Wilcoxon rank-sum test combined with fold change (FC) analysis. Because of the chosen comparison direction MHO/HC (panel (A)), MUO/HC (panel (B)), and MHO/MUO (panel (C)) increased and decreased metabolite concentrations in HC, MUO, and MHO groups have been marked as down (blue) and up (red) regulated, respectively. The -log10 (p values) is meaningful of the level of significance of each VOC and has been plotted versus the log2 fold change. It represents the difference between the levels of expression for each VOC between the two groups
SCFA quantification
A targeted GC–MS analyses of SCFAs was carried out. In detail, acetic, propanoic, butanoic, isobutyric, and isovaleric acids were analysed and (p value > 0.05) except for butanoic acid, whose concentrations resulted lower (p value < 0.05) in MUO subjects compared to MHO group, did not statistically differed (Supplementary Fig. S2).
Real time PCR
To inspect the commensal taxa representative as much as possible of the gut microbiota, qPCR primers were selected for the identification of known genera, groups, and species harbouring the human gut. qPCR copy number log values have been reported in Supplementary Table S2. Few investigated taxa significantly differed between groups (Fig. 4).
Statistically significant qPCR tested taxa emerging from pairwise comparison among healthy (HC), metabolically healthy obesity (MHO), and metabolically unhealthy obesity (MUO) sample cohorts. Groups were compared by applying a Benjamini–Hochberg corrected Welch’ test and corrected P-values (q-values) have been reported
In detail, C. coccoides group resulted to have lower CN log values in obesity groups than HC. Gut microbiota of MHO subjects presented increased amounts of Lactobacillus genus and Lp. plantarum than HC volunteers. Finally, MUO subjects showed a higher abundance of Prevotella and Desulfovibrio genera, compared to both HC and MHO subjects, and higher Lp. plantarum CN log compared to HC group.
Discussion
This observational clinical study relies on the power of statistical multivariate approaches useful in reducing low-impacting variable noise, and in selecting the most contributing variables that discriminated MHO, MUO and HC cohorts. In addition, for the first time, groups of obese patients and healthy subjects followed a restrictive caloric diet in the range 800 < x < 1200 kcal per day. This allowed us to lower the impact of diet regimens on considered sample stratifications. Downstream to all the inspected statistical results, specific markers of obesity-related comorbidities, i.e. inflammation, liver damage, immunity response, and hormone metabolism profiled MUO patients Although some significant variables including BMI and weight were shared between MHO and MUO, the metabolic profile confirmed the well-known differences between the two obese phenotypes. Specifically, higher levels of HbA1c, HOMA-IR, total cholesterol, triglycerides, AST, ALT, and FBG, as well as lower GFR and albumin levels were detected in MUO, corroborating the association of visceral adiposity with reduced insulin sensitiveness, metabolic alterations, and low-grade inflammation. Lower GFR and hypoalbuminemia are also known to correlate with morbid obesity, thus increasing the risk of chronic kidney disease onset [12]. In addition, higher levels in AST and ALT enzymes observed in MUO as compared to HC and MHO, describe the presence of liver disease and the progression of hepatic dysfunction [13].
The worsening of renal conditions is a clear indication of inflammation, as stated for patients suffering from pathological obesity, that are characterized by impaired insulin sensitivity and higher levels of HbA1c too [14], a diagnostic marker of pre-diabetes and T2D diabetes.
Moreover, HOMA-IR resulted to be higher in MUO compared to MHO patients, and our rotating factor analysis included it as part of the second high-loading factor (greater than 0.7).
MUO reported lower level of albumin compared to MHO. Reduced albumin serum levels have been weighted as marker of alteration in energy intake metabolism and liver damage. In addition, we found the presence of dyslipidaemia (increased triglycerides and cholesterol) in MUO as compared to HC.
Other inflammatory markers, part of the first rotating analysis factor, associated with systemic inflammation in patients with obesity i.e., CRP, hsCRP, and ESR, were increased in MUO versus HC. In these pathologic conditions, further evidence is prompted by the white blood cells and platelets that significantly increased compared to HC. Cytokines derived by inflammation, along with adipokines, such as leptin, induce leucocytosis together with a higher pituitary secretion of TSH. This hormone impacts adiposity, adipogenesis regulation, appetite, insulin resistance, and weight gain [15].
Furthermore, as expected, we also detected higher levels of insulin in MUO patients compared to HC, associated with obesity and inflammation [16].
Finally, levels of 25-OH vitamin D, an anti-inflammatory and anti-adipogenic factor, were significantly reduced in MUO compared to HC group. Vitamin D is a fat-soluble mediator mainly stored in adipose tissue and its circulating reduction in obesity could reflect a volumetric dilution in fat compartment [17]. Noteworthy, the 25-OH vitamin D levels of MHO patients showed no statistically significant differences as compared to HC subjects. This indicates a different distribution of adipose tissue in two obese phenotypes that could differently impact on the factor release.
Although the caloric range in the three groups was equivalent, some statistically significant differences emerged for specific nutrients. Both groups of obesity showed a higher consumption of starch and manganese, but lower intake of total mineral salts, thiamine, and oleic acid when compared to HC group. Similar results have been obtained by previous studies where an excessive blood level of manganese resulted positively associated with increased visceral adipose tissue mass [18], as well as low consumption of MUFA resulted associated with a higher risk of obesity and metabolic consequences [19].
Interestingly, MUO individuals showed differences in the consumption of some micronutrients: a lower intake of iodine, known to enhance thyroid problems [20], together with reduced levels of alpha-tocopherol, a vitamin able to favour glycaemic control, and inversely related to BMI in morbid obesity [21]. Conversely, higher intake of cystine, an amino acid with adipogenic property and frequently related with fat accumulation [22], was observed in MUO as compared to HC. Interestingly, cystine intake resulted higher in MUO also in comparison with MHO subjects, suggesting that this amino acid could differentiate these two different obesity phenotypes. A comparable intake of pyridoxine, vitamin with positive metabolic effectiveness [23], and niacin, with a potential role in improving cardiovascular risk and dyslipidaemia [24], was observed between MHO and HC, but not in MUO individuals, thus suggesting that these micronutrients could prevent the metabolic worsening of MHO towards a more severe obesity phenotype.
By targeting the intestinal microbial population qPCR analysis showed that MHO individuals were characterized by higher abundance of Lactobacillus genus compared to HC. The microbiota of both MUO and MHO showed higher levels of Lactiplantibacillus plantarum versus HC. Although species included in Lactobacillus genus exert beneficial effects and anti-obesity properties, studies revealed that some species were associated with obesity [25]. Armougom et al. [26] reported a correlation between the concentration of Lactobacillus spp. and the weight gain in patients with obesity, compared to healthy and anorexic subjects.
In addition, MUO were characterized by higher quantities of Prevotella and Desulfovibrio genera when compared with MHO and HC. Previous studies showed high prevalence of Prevotella genus in patients with obesity and observed differences in terms of abundances in both the metabolic obesity classes [27]. Recent literature findings reported how subjects who underwent a restrictive Mediterranean diet exhibit a decrease in Prevotella copri species with a concomitant improvement in insulin resistance [28] and, at the same time, indicated how an increase in Prevotella/Bacteroidetes ratio reflects a metabolic shift that included important changes in carbohydrate metabolism [29, 30].
Noteworthy, the inspection of fiber enriched diet effects, including a reduction in BMI and waist circumference levels, revealed a strong correlation with Prevotella genus increased abundances [31,32,33].
This action on weight reduction would be dependent on the higher levels of SCFAs, in particular propionate [31], with an enhanced activity of Prevotella in the liver. Moreover, this taxa is active in reducing serum cholesterol and hepatic lipogenesis, acting on anti-inflammatory pathways, thus preventing weight gain in human and rodents [34]. Thus the restricted caloric regimen in our cohort definitely led Prevotella to increase in MUO compared to MHO and HC sample sets.
In a rat model, Prevotella appeared to regulate feeding behaviour since its abundance was positively associated with appetite-regulating hormones as ghrelin, known to stimulate the sense of hungry, and, was negatively correlated with leptin, the anorectic hormone [35]. Furthermore, as discussed above, leptin promotes the differentiation of granulocytes, inducing leucocytosis, the well-known process which accompain the low-grade of inflammation of morbid obesity [36]. On the other hand, Desulfovibrio is positively correlated with different dysmetabolic conditions [37]. Furthermore, this genus plays a role in the development of NAFLD where it could lead to increase the intestinal permeability and the upregulation of the gene involved in fat storage of liver cells [38].
Of note, lower concentrations of Clostridium coccoides group were observed in obese sets as compared to HC. The controversial role of C. coccoides is still under debate; some studies reported a positive correlation with the worsening of obesity [39], while others discussed the lower abundance in mice exposed to high-fat diet [40]. Furthermore, over the negative correlation with insulin level and HOMA-IR, this taxon was found to be negatively associated with the ghrelin level [7]. Some evidence also support the beneficial role of this taxon as a butyrate-producer [41]. In fact, a reduction of C. coccoides group observed in MUO was accompanied by the decrease of fecal amount of butanoic acid versus MHO. Butanoic acid impacts the i) increase of leptin release and insulin sensitivity, ii) decrease of hypercholesterolemia and hepatic steatosis, iii) decrease of HOMA-IR index and iv) modulation of cellular events that regulate the assembly and delivery of lipoproteins.
Based on fecal volatilome profiles, MUO subjects reported significant lower concentration of 2H-indol-2-one-1,3-dihydro and nonanoic acid as compared to HC. Nonanoic acid is associated with beneficial effects and antimicrobial properties [42]. 2H-indol-2-one-1,3-dihydro has been described to activate the aryl hydrocarbon receptor [43], whose activation prevents cytokine induction and defends gut barrier integrity against damage in obesity [44]. Indole, a compound associated to major adverse cardiovascular events [45] resulted higher in MUO compared to MHO group.
Furthermore, compared to HC, MUO showed lower quantities of humulene, gamma-terpinene, and alpha-phellandrene, present in herbs with antioxidant, anti-inflammatory, and anti-obesity properties [46].
MUO group reported higher concentration of hexadecanoic acid, a derivative of 2-hexadecanone, known to correlate with insulin resistance and T2D, by increasing the synthesis of deleterious lipids and inflammatory mediators [47]. Similarly, 2-undecanone, an healthy metabolite able to mediate anti-inflammatory and antioxidant effects whose production is ascribed to L. plantarum [48] increase in MUO. This ketone inhibits some proteins and cytokines related to nuclear factor-kB (NF-kB) pathway involved in the antioxidant response [49]. Therefore, the greater amounts of 2-undecanone and L. plantarum observed in MUO individuals probably could be related to the inflammatory milieu associated with morbid obesity. Among ketone compound class, 2-tetradecanone was less represented in fecal samples of MHO patients as compared to controls. Some evidence reported antioxidant, anti-inflammatory, and anti-diabetic activities of its ester derivative ethyl tridecanoate [50]. In addition, MUO group as compared to HC showed lower levels of cyclohexanecarboxylic acid whose derivative, the 4-phenylpiperidine-1-carbonyl cyclohexanecarboxylic acid is known to inhibit the diacylglycerol acyltransferase 1, an enzyme involved in triglyceride biosynthesis [51]. Finally, a reduction of pentanoic acid butyl ester amount was observed in MUO than HC. This compound belongs to fatty acid ester derivative class, which reported beneficial effects against obesity, by regulating serum lipid profiles and by inducing adipocyte apoptosis [52].
Although preliminary, our investigation approach has some limitations. The here applied analytical strategy, based on caloric intake data gathered as three-day food questionnaires, prevents the introduction of biases related to non-adherent subjects. Dealing with the number of samples, due to its explanatory nature, this pilot investigation targeting MUO and MHO obese patients does not rely on a statistical power calculation.
Undoubtedly, the reported real time PCR findings would take advantage from a metataxonomics sequencing analysis that would crucially strengthen the connection between VOCs and fecal taxa.
Conclusions
In our observational study, we analysed for the first time the significant differences in clinical biochemical parameters, selected intestinal microbial taxa, and volatilome between subjects with metabolically healthy and unhealthy obesity, compared to healthy control volunteers with a daily calorie intake set in a specific range. Based on a strong statistical rationale, all conducted analyses made us confident in ascertaining a MUO specific clinical signature, highlighting how metabolically healthy obesity most likely represents a transient obesity phenotype. These data could represent as a prognostic marker tool useful in monitoring the obesity-associated metabolic comorbidities. Future studies are needed to understand the molecular mechanisms beyond the intestinal dysbiosis in the development and progression of obesity.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
NCD Risk Factor Collaboration (NCD-RisC) (2017) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017(390):2627–2642
Genchi VA, Rossi E, Lauriola C et al (2022) Adipose tissue dysfunction and obesity-related male hypogonadism. Int J Mol Sci 23:8194
Calabrese FM, Porrelli A, Vacca M et al (2021) Metaproteomics approach and pathway modulation in obesity and diabetes: a narrative review. Nutrients 14:47
Porro S, Genchi VA, Cignarelli A et al (2021) (2021) Dysmetabolic adipose tissue in obesity: morphological and functional characteristics of adipose stem cells and mature adipocytes in healthy and unhealthy obese subjects. J Endocrinol Invest 44:921–941
Abenavoli L, Scarpellini E, Colica C et al (2019) Gut microbiota and obesity: a role for probiotics. Nutrients 11:2690
Krajmalnik-Brown R, Ilhan Z-E, Kang D-W, DiBaise JK (2012) Effects of gut microbes on nutrient absorption and energy regulation. Nutr Clin Pract 27:201–214
Gomes AC, Hoffmann C, Mota JF (2018) The human gut microbiota: metabolism and perspective in obesity. Gut Microbes 9:308–325
Caër C, Wick MJ (2020) Human intestinal mononuclear phagocytes in health and inflammatory bowel disease. Front Immunol 11:410
Szczuko M, Kikut J, Maciejewska D, Kulpa D, Celewicz Z, Ziętek M (2020) The associations of SCFA with anthropometric parameters and carbohydrate metabolism in pregnant women. Int J Mol Sci 21:9212
Lin H-M, Helsby NA, Rowan DD, Ferguson LR (2011) Using metabolomic analysis to understand inflammatory bowel diseases. Inflamm Bowel Dis 17:1021–1029
Belfort-DeAguiar R, Seo D (2018) Food cues and obesity: overpowering hormones and energy balance regulation. Curr Obes Rep 7:122–129
Guebre-Egziabher F, Brunelle C, Thomas J et al (2019) Estimated glomerular filtration rate bias in participants with severe obesity regardless of deindexation. Obesity (Silver Spring) 27:2011–2017
Giannini EG, Testa R, Savarino V (2005) Liver enzyme alteration: a guide for clinicians. CMAJ 172:367–379
Yu M, Zhang S, Wang L et al (2022) Association of metabolically healthy obesity and glomerular filtration rate among male steelworkers in North China. Int J Environ Res Public Health 19:11764
Teixeira PD, Dos Santos PB, Pazos-Moura CC (2020) The role of thyroid hormone in metabolism and metabolic syndrome. Ther Adv Endocrinol Metab 11:2042018820917869
Zhang AMY, Wellberg EA, Kopp JL, Johnson JD (2021) Hyperinsulinemia in obesity, inflammation, and cancer. Diabetes Metab J 45:285–311
Drincic AT, Armas LAG, van Diest EE, Heaney RP (2012) Volumetric dilution, rather than sequestration best explains the low vitamin D status of obesity. Obesity 20:1444–1448
Tao C, Huang Y, Huang X et al (2022) Association between blood manganese levels and visceral adipose tissue in the United States: a population-based study. Nutrients 14:4770
Chen W, Ao Y, Lan X et al (2023) Associations of specific dietary unsaturated fatty acids with risk of overweight/obesity: population-based cohort study. Front Nutr. https://doi.org/10.3389/fnut.2023.1150709
Moleti M, Di Mauro M, Paola G, Olivieri A, Vermiglio F (2021) Nutritional iodine status and obesity. Thyroid Res 14:25
Botella-Carretero JI, Balsa JA, Vázquez C, Peromingo R, Díaz-Enriquez M, Escobar-Morreale HF (2010) Retinol and α-tocopherol in morbid obesity and nonalcoholic fatty liver disease. Obes Surg 20:69–76
Elshorbagy AK, Church C, Valdivia-Garcia M, Smith AD, Refsum H, Cox R (2012) Dietary cystine level affects metabolic rate and glycaemic control in adult mice. J Nutr Biochem 23:332–340
Haidari F, Mohammadshahi M, Zarei M, Haghighizadeh MH, Mirzaee F (2021) The effect of pyridoxine hydrochloride supplementation on leptin, adiponectin, glycemic indices, and anthropometric indices in obese and overweight women. Clin Nutr Res 10:230–242
Zhang X, Zhu B, Lin P et al (2022) Niacin exacerbates β cell lipotoxicity in diet-induced obesity mice through upregulation of GPR109A and PPARγ2: inhibition by incretin drugs. Front Endocrinol (Lausanne) 7(13):1057905
Angelakis E, Armougom F, Million M, Raoult D (2012) The relationship between gut microbiota and weight gain in humans. Future Microbiol 7:91–109
Armougom F, Henry M, Vialettes B, Raccah D, Raoult D (2009) Monitoring bacterial community of human gut microbiota reveals an increase in Lactobacillus in obese patients and Methanogens in anorexic patients. PLoS ONE 4:e7125
Zhong X, Harrington JM, Millar SR, Perry IJ, O’Toole PW, Phillips CM (2020) Gut microbiota associations with metabolic health and obesity status in older adults. Nutrients 12:2364
Meslier V, Laiola M, Roager HM et al (2020) Mediterranean diet intervention in overweight and obese subjects lowers plasma cholesterol and causes changes in the gut microbiome and metabolome independently of energy intake. Gut 69:1258–1268
Caputo M, Pigni S, Antoniotti V et al (2023) Targeting microbiota in dietary obesity management: a systematic review on randomized control trials in adults. Crit Rev Food Sci Nutr 63:11449–11481
Dong TS, Guan M, Mayer EA et al (2022) Obesity is associated with a distinct brain-gut microbiome signature that connects Prevotella and Bacteroides to the brain’s reward center. Gut Microbes 14:2051999
Hjorth MF, Christensen L, Larsen TM et al (2020) Pretreatment Prevotella-to-Bacteroides ratio and salivary amylase gene copy number as prognostic markers for dietary weight loss. Am J Clin Nutr 1(111):1079–1086
Grembi JA, Nguyen LH, Haggerty TD et al (2020) Gut microbiota plasticity is correlated with sustained weight loss on a low-carb or low-fat dietary intervention. Sci Rep 10:1405
Benítez-Páez A, Hess AL, Krautbauer S et al (2021) Sex, food, and the gut microbiota: disparate response to caloric restriction diet with fiber supplementation in women and men. Mol Nutr Food Res 65:e2000996
Chambers ES, Viardot A, Psichas A et al (2015) Effects of targeted delivery of propionate to the human colon on appetite regulation, body weight maintenance and adiposity in overweight adults. Gut 64:1744–1754
Queipo-Ortuño MI, Seoane LM, Murri M et al (2013) Gut microbiota composition in male rat models under different nutritional status and physical activity and its association with serum leptin and ghrelin levels. PLoS ONE 8:e65465
Purdy JC, Shatzel JJ (2021) The hematologic consequences of obesity. Eur J Haematol 106:306–319
Qin J, Li Y, Cai Z et al (2012) A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490:55–60
Lin Y-C, Lin H-F, Wu C-C, Chen C-L, Ni Y-H (2022) Pathogenic effects of Desulfovibrio in the gut on fatty liver in diet-induced obese mice and children with obesity. J Gastroenterol 57:913–925
Munukka E, Wiklund P, Pekkala S et al (2012) Women with and without metabolic disorder differ in their gut microbiota composition. Obesity (Silver Spring) 20:1082–1087
Cani PD, Amar J, Iglesias MA et al (2012) Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56:1761–1772
Singh V, Lee G, Son H et al (2023) Butyrate producers, “The Sentinel of Gut”: their intestinal significance with and beyond butyrate, and prospective use as microbial therapeutics. Front Microbiol. https://doi.org/10.3389/fmicb.2022.1103836
Sun E, Zhang X, Zhao Y et al (2021) Beverages containing Lactobacillus paracasei LC-37 improved functional dyspepsia through regulation of the intestinal microbiota and their metabolites. J Dairy Sci 104:6389–6398
Dong F, Hao F, Murray IA et al (2020) Intestinal microbiota-derived tryptophan metabolites are predictive of Ah receptor activity. Gut Microbes 12:1788899
Postal BG, Ghezzal S, Aguanno D et al (2020) AhR activation defends gut barrier integrity against damage occurring in obesity. Mol Metab 39:101007
Sanchez-Gimenez R, Ahmed-Khodja W, Molina Y et al (2022) Gut microbiota-derived metabolites and cardiovascular disease risk: a systematic review of prospective cohort studies. Nutrients 14:2654
Mandal D, Sarkar T, Chakraborty R (2023) Critical review on nutritional, bioactive, and medicinal potential of spices and herbs and their application in food fortification and nanotechnology. Appl Biochem Biotechnol 195:1319–1513
Palomer X, Pizarro-Delgado J, Barroso E, Vázquez-Carrera M (2018) Palmitic and oleic acid: the yin and yang of fatty acids in type 2 diabetes mellitus. Trends Endocrinol Metab 29:178–190
Rajasekharan SK, Shemesh M (2022) The bacillary postbiotics, including 2-undecanone, suppress the virulence of pathogenic microorganisms. Pharmaceutics 14:962
Song G, Yu S, Zhang Y, Sun M, Zhang B, Peng M (2023) 2-Undecanone alleviates asthma by inhibiting NF-κB pathway. Biochem Cell Biol 101:101–111
Rout D, Chandra Dash U, Kanhar S, Swain SK, Sahoo AK (2020) The modulatory role of prime identified compounds in the bioactive fraction of Homalium zeylanicum in high-fat diet fed-streptozotocin-induced type 2 diabetic rats. J Ethnopharmacol 260:113099
Kandre S, Bhagat PR, Reddy MMK et al (2014) Synthesis and evaluation of cyclohexane carboxylic acid head group containing isoxazole and thiazole analogs as DGAT1 inhibitors. Eur J Med Chem 79:203–215
Yao Y, Li X-B, Zhao W et al (2010) Anti-obesity effect of an isoflavone fatty acid ester on obese mice induced by high fat diet and its potential mechanism. Lipids Health Dis 9:49
Funding
Open access funding provided by Università degli Studi di Bari Aldo Moro within the CRUI-CARE Agreement. This paper was funded by the Italian Ministry for Universities and Research and the Europe Union FSE, within the program PON Ricerca e Innovazione 2014–2020 and FSC, Asse 2, Azione II, 2 Cluster – Ricerca industriale e sviluppo sperimentale – Area di specializzazione “Salute” – Project name: BIOMIS – Costituzione della biobanca del microbiota intestinale e salivare umano: dalla disbiosi alla simbiosi (grant number ARS0101220).
Author information
Authors and Affiliations
Contributions
Conception and design: GF, PS, GL, SS and MDA. Analysis and interpretation of the data: FMC, GC, NS, VAG, MV, GP, and SP. Critical revision of the article for important intellectual content: FMC, VAG, NS and SP. Final approval of the article: FMC and SP.
Corresponding authors
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding authors state that there is no conflict of interest.
Ethical approval
Ethics committee approval no. 0771/ 2020 project BIOMIS-endo n. 6278 (Project Code: ARS01_01220) Establishment of the Human Intestinal and Salivary Microbiota Biobank – Obesity. ClinicalTrials.GOV: NCT04698135.
Informed consent
This study involved human participants whose informed consent was subscribed before the trial engagement.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Calabrese, F.M., Genchi, V.A., Serale, N. et al. Gut microbiota and fecal volatilome profile inspection in metabolically healthy and unhealthy obesity phenotypes. J Endocrinol Invest (2024). https://doi.org/10.1007/s40618-024-02379-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40618-024-02379-2