Abstract
Background
Hypothyroidism is prevalent at all ages and represents a non-communicable disease with preventable consequences.
Method
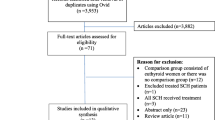
Narrative review.
Review
In children and adolescents, the most devastating consequences of undertreatment with levothyroxine (LT4) are poor growth and development. Delayed treatment in congenital hypothyroidism can lead to permanent brain damage. In young to middle-aged adults, symptoms are often overlooked, and treatment delayed by many years. The resulting consequences are also at this age group compromised brain and physical function but less severe and partly reversible with treatment. The under-treated condition often results in a higher risk of, e.g., increased cardiovascular disease burden, obesity, hypertension, poor physical capacity, and poor quality of life. Excessive replacement is at all adult age groups associated with increased risk of cardiac death, osteoporosis, loss of muscle function, psychological instability and poor quality of life. In young fertile women, the consequences of undertreatment with LT4 are subnormal fertility, recurrent pregnancy loss, compromised fetal growth, and neurocognitive development. On the other hand, excessive LT4 treatment has been related to gestational hypertension, preeclampsia and preterm birth. In the elderly, care must be given to avoid confusing a slightly high age-related serum TSH with requirement for LT4 treatment in a truly hypothyroid patient. Excessive LT4 treatment in patients of high age is associated with an increased mortality.
Conclusion
Suboptimal and excessive LT4 replacement of the preventable non-communicable disease hypothyroidism requires more focus from the healthcare system and from the global political systems to prevent the personally devastating and socioeconomically challenging consequences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypothyroidism (or myxedema) is a common non-communicable endocrine disorder worldwide, depending on the composition of the populations’ age, sex, race, genetics, food intake, environmental factors such as iodine and selenium intake as well as the specific diagnostic criteria and many other influences [1]. In typical cases of overt hypothyroidism, the diagnosis is not difficult, but there are several gray zones such as how to manage the milder or subclinical cases, how to distinguish influence from non-thyroidal illness, and the differences in reference ranges across ages.
Thyroxine (T4) was chemically identified in 1927 [2] and the second thyroid hormone—triiodothyronine (T3) 25 years later [3]. L-thyroxine (LT4) has been commercially available since the 1950ies and remains the cornerstone in treatment of hypothyroidism [4, 5], despite several challenges mainly including that of patients and patient organizations wishing to shift to combination therapy with T3 [1] or to revert to desiccated thyroid preparations [1], none of which is recommended in current guidelines and not used abundantly in, e.g., Denmark [4].
The aim of this narrative review is to give evidence for the long-term efficacy of LT4 and the risks and consequences of both suboptimal and excessive replacement throughout different ages and patient populations.
Causes of hypothyroidism
Globally, the main cause for spontaneous hypothyroidism is still overt iodine deficiency or partial iodine deficiency for special conditions such as pregnancy. In populations of sufficient or moderately iodine deficiency the pattern of hypothyroidism is different. Thus, a large population study in Denmark reported that the most common subtype (present in 84.4% of patients) was spontaneous (presumably autoimmune) hypothyroidism, followed by post-partum (4.7%) and amiodarone-induced hypothyroidism (4.0%). Less common causes were subacute thyroiditis (1.8%), previous radiation or surgery (1.8%) to the thyroid gland, congenital (1.6%) and lithium-associated (1.6%) thyroid failure. Iatrogenic causes have become more frequent due to various immunotherapies [6]. Rarer causes include central (secondary) hypothyroidism, thyroid hormone resistance, overtreatment with antithyroid drugs, effects of other drugs, ingestion of food containing goitrogens (e.g., vegan food), and therapeutic or environmental irradiation [1].
Physiology of thyroid function and diagnosis of hypothyroidism
The diagnosis of overt hypothyroidism can sometimes be based on the phenotype, but in most cases biochemical measurement of thyroid function variables is necessary and recommended, particularly in subtle cases. In some situations, it will also be needed to measure supportive biomarkers [7]. Thyroid hormone secretion is regulated in a negative feedback manner by pituitary thyrotropin (TSH), which in turn is stimulated by the hypothalamic TSH releasing hormone (TRH) [1]. Obtaining a normal euthyroid state is, thus, a delicate balance between the hypothalamus–pituitary function and that of the thyroid gland, regulated in a logarithmic (TSH)/linear (T4 and T3) way.
The reliability of the biochemical measurements on the one hand, and the cut-off values of the hormone measurements between normal and hypothyroid persons on the other, are therefore crucial for a correct diagnosis. Due to the above-mentioned log/linear relationship, serum TSH is the most sensitive variable to assess thyroid function, The diagnosis of primary hypothyroidism is nevertheless based on biochemical demonstration of low circulating T4 in the face of an elevated serum TSH beyond the reference limits of normal people. A universally accepted reference range has been suggested as 0.4–4.0 mU/L, but is unfortunately too simplistic, since there are huge variations among populations in terms of environmental influence such as iodine intake, age, genetics, and many others. Serum TSH is, thus, higher in areas of both overt and partial iodine deficiency [8], very high in neonates [9], variable during pregnancy according to gestation [10], increasing at high age [11] and higher in some genetic population groups such as Ashkenazy Jews [12]. Circulating thyroid hormones show similar reference range differences although less well explored. Consequently, current reference ranges could potentially lead to inappropriate commencement of treatment in older individuals and in certain populations with other genetic traits. However, they could also result in inappropriate treatment at all ages. There is no evidence to support the general use of age-appropriate reference intervals, nor to understand the impact of thyroid hormone variations in younger individuals.
On top of these physiological challenges, there are also a number of pitfalls in the biochemical measurements of the thyroid-related hormones [6, 13, 14]. Although most of them are rare, it is important to know of their existence since they may otherwise result in wrong diagnoses and treatment [6, 15, 16]. Finally, a number of concomitant drug intakes can compromise the absorption of levothyroxine [6, 17] as can gastrointestinal diseases such as coeliac disease, pernicious anemia, ulcerative colitis [18], and many more. Other drug intakes can also influence the thyroid-related hormone measurements as well [6].
Suboptimal and excessive treatment in children and adolescents
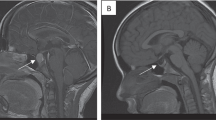
Severe untreated congenital hypothyroidism will result in cretinism with blunted growth, very low IQ, generally failed neurological development and psychological disturbances. In the Western part of the world, such cases are irradicated by introduction of a neonatal TSH screening program. However, despite the available dried blood spots technology since the early 1970s, approximately 70% of the world’s population does not have access to it. Therefore, children still develop cretinism [19]. Congenital hypothyroidism usually cannot be diagnosed on clinical grounds until the child is several months old. The consequent treatment delay therefore leaves these children with permanent neurological damage. To increase the early detection of milder cases of congenital hypothyroidism, the screening TSH level has been lowered, and free T4 measurements have in some countries been added to diagnose also congenital central hypothyroidism [20, 21].
The causes of hypothyroidism occurring later in childhood and in adolescents include iodine deficiency, subtle congenital defects in, e.g., thyroid hormone synthesis, hereditary thyroid disorders (thyroid hormone resistance), autoimmune thyroid disease, and potentially environmental endocrine disruptors. Later occurrence is usually associated with milder symptoms, but also results in impaired growth, behavioral problems and symptoms of attention-deficit/hyperactivity disorder (ADHD), failure of obtaining a proper education and, thus, very often failure to become independent adults. This disorder, therefore, also has high socioeconomic consequences for the individual and society, which might be prevented or reversed if treated early with LT4 [22].
Consequences of excessive LT4 replacement are unfortunately not well explored in this age group (Table 1).
Suboptimal and excessive treatment in adults after puberty until old age
Young or middle-aged adults are also at risk of underdiagnosis and undertreatment for hypothyroidism mostly due to very non-specific symptomatology and few typical features [1]. Since thyroid hormones are responsible for cellular metabolism in all mammalian organs, it is not surprising that symptoms can occur from all organ systems if thyroid hormones are reduced even only slightly. The risks of undertreatment of a diagnosed hypothyroid state are related to poor mental function, ADHD or other behavioral conditions, reduced cardiac output, and decreased physical capacity due to low cardiac output combined with muscle weakness and reduced lung function (1). A reflex overstimulation of catecholamines leads to hypertension, which together with obesity subsequently leads to an increased cardiovascular disease burden. Patients often have hair loss, dry skin, and constipation, and due to a slow metabolism, patients have a low production of many substances, e.g., hemoglobin and adrenal glucocorticoids. Conversely, there is a low degradation of many substances giving rise to, e.g., elevated liver enzymes. Furthermore, patients with under-treated hypothyroidism have a low glomerular filtration rate. Many drugs may have a slow metabolism and thereby risk accumulation or direct poisoning. All of these symptoms and signs result in a poor quality of life and general work-functioning [1].
Other factors may also increase the risk, e.g., protein loss in proteinuria causing urinary loss of LT4 and, therefore, requires an increase of the LT4 replacement dosage, whereas several other drugs or food components can interfere with the gastric absorption of LT4.
Suboptimal and excessive treatment in women during reproductive age
Women of reproductive age face a number of risks of both over- and undertreatment due to challenges related to interpretation of thyroid function tests and varying needs for LT4 treatment. Women with a higher concentration of estrogen, e.g., by use of oral contraceptives or during pregnancy, will have an increased concentration of thyroid hormone binding proteins, which will cause an increase in the total T4 concentration. This will interfere with most immunoassays measuring free T4 as they are unable to sufficiently correct for the extremes found in the high end of the correction curves. Thus, there is a risk of misinterpreting the free T4 concentrations and thereby under- or overtreating the women and correct management will require additional measures of thyroid function. Specifically in pregnancy, the LT4 treatment is not only important to the woman, but also to secure a sufficient placental transfer of T4, which is needed for fetal development and to reduce adverse pregnancy outcomes such as pregnancy loss and preterm birth [23, 24]. To avoid undertreatment, the LT4 dosage should be increased to mimic the physiological increase in T4 in pregnancy [7, 25].
Furthermore, undertreatment of hypothyroid women will often lead to irregular menstrual periods and infertility, which is also the reason for the internationally recommended screening for thyroid dysfunction of all women referred to fertility treatment [25, 26]. Hypothyroid women treated with LT4 will need an increased dose prior to fertility treatments involving controlled ovarian stimulation as such stimulation induces an acute increased TBG production. Women in fertility treatment with untreated subclinical hypothyroidism may need LT4 substitution prior to fertility treatment to support the critical phase of implantation and early pregnancy [27, 28]. On the other hand, slight aberrations in thyroid function may not need to be treated given the risk of overtreatment, which could also lead to (iatrogenic) preeclampsia and preterm birth [28]. Noteworthy, there is no evidence to support a benefit to offspring IQ by LT4 treatment of subclinical hypothyroidism or hypothyroxinemia [29, 30].
Finally, the post-partum period requires changes in dosage to return to pre-pregnancy dosage. However, in women with remaining thyroid gland function and thyroid autoimmunity, there is a risk of post-partum thyroiditis with an initial destructive thyroiditis with release of thyroid hormone and hyperthyroidism, followed by a hypothyroid phase until regeneration of the thyroid function (if any left). The hypothyroid phase requires an increased dose of LT4, which is often transitory, but may become permanent. Monitoring in the post-partum phase is therefore important to secure optimal treatment, which is even more important as there is a risk of suboptimal treatment resulting in a limited capacity to take care of their child due to fatigue, and risk getting a diagnosis of post-partum depression. Women with unexpected symptoms post-partum should, therefore, also have their thyroid function tested to discover and treat hypothyroidism [31].
Suboptimal and excessive treatment of the elderly and people with cardiac diseases
TSH reference ranges in the elderly must be evaluated in the light of the age-dependent shift in serum TSH distribution toward higher concentrations with increasing age. Studies in several populations (Americans, Scottish, Ashkenazi Jews, Chinese) have shown progressively increasing TSH concentrations with age. The 97.5th percentiles of the reference population are considerably higher in the elderly (older than 70 years old) than in younger adults [32,33,34,35], which is not explained only by higher prevalence of thyroid autoimmunity [36, 37]. This phenomenon might reflect an age-related alteration in the TSH set point and/or reduced TSH bioactivity and/or reduced sensitivity of the thyroid gland to TSH, since longitudinal data suggest an inter-individual age-dependent TSH increment not associated with a decline in free T4 [36]. Although an association between increased serum TSH and/or lower levels of thyroid hormones and extended life span have been observed, it is still unclear if it is a positive adaptation or a progressive, negative deterioration [38].
A recent large cohort study found that approximately 1/3 of older hypothyroid patients on LT4 treatment had taken at least one medication that interferes with thyroid hormones [39]. In addition, common chronic conditions such as heart, kidney, liver disease, diabetes, major depression, as well as low caloric intake, which are more prevalent in the elderly, may result in changes in thyroid function as part of the euthyroid sick syndrome. For these reasons, a detailed careful review of drugs and comorbidities should always be conducted before an older individual with hypothyroidism treated with LT4 is classified as under-treated [36]. The age-dependent shift in serum TSH distribution toward higher concentrations with increasing age and an observed relationship between longevity and lower thyroid function prompted experts to recommend a higher TSH level target of, e.g., 6 mIU/L in a 70-year-old patient treated with LT4 [40] considering other factors (drugs, comorbidities) affecting the thyroid function tests.
However, several studies showed insufficiently treated overt and/or subclinical hypothyroidism as well as excessively replaced hypothyroid patients associated with increased early mortality risk in older patients [41,42,43,44]. Furthermore, a recent study found that the cardiovascular mortality risk increased progressively with higher TSH, especially in the older adults [14]. These studies used different criteria and different number of TSH measurements regarding the classification of under-treated patients, but in any case, these findings highlight the importance for further studies on the optimal TSH target in older hypothyroid patients.
The profound negative effect of hypothyroidism, and the beneficial effect of LT4 therapy on cardiac function should be taken into consideration when planning thyroid hormone therapy [36, 45, 46]. A recent retrospective cohort study of more than 150,000 patients with incident hypothyroidism of whom 97% received LT4 therapy during the follow-up period, showed that there was an association between the highest TSH concentration and increased risk of heart failure both in patients younger and older than 65 years; whereas, the increased risk of ischemic heart disease remained significant only in patients ≤ 65 years [43]. The risk of stroke/transient ischemic attack was not increased in any patients. These findings are, thus, not conclusive concerning the level of LT4 treatment in the hypothyroid elderly, particularly when considering the serious risks of excessive LT4 replacement in the elderly (Table 1).
Recently, a comprehensive meta-analysis including 55 studies and a total of 1,898,314 subjects, concluded that the presence of overt hypothyroidism is associated with an increased risk of myocardial ischemia (13%), myocardial infarction (15%), arrhythmias (96%) and overall mortality (25%) when compared to euthyroidism [47]. In another paper, a meta-analysis involved 7 studies and 31,138 subjects concluded that the presence of overt hyperthyroidism increased overall mortality by 13% and the mortality for cardiovascular causes by 21% [48]. Another more recent meta-analysis including 37 studies and enrolling 113,393 hyperthyroid subjects confirmed that overt hyperthyroidism increased the risk of ischemic heart disease, stroke, and cardiovascular mortality [49].
Suboptimal and excessive LT4 replacement in other special situations
In hypothalamus–pituitary–hypothyroidism or central/secondary hypothyroidism, the thyroid hypofunction is due to a failing pituitary production of biologically active TSH. Unfortunately, the biologically inactive TSH molecule is measurable by the TSH immunoassays and therefore useless in the diagnosis of hypothyroidism as well as monitoring of replacement [50]. Total and free T4 measurements (free T4 estimates) are thus the only useful tools by current methodology [51]. In case of multiple pituitary hormone deficiencies, the situation becomes more complex, e.g., in women on estrogen replacement therapy (or on oral contraceptive drugs), except worse, since TSH cannot be used [52]. These women are, therefore, at high risk of suboptimal replacement with a consequent worse metabolic profile [53].
Patients in intensive care units (ICU) are also particularly problematic because they often cannot take tablets orally. In these situations, patients need other administration routes either i.v LT4 or oral liquid formulation [54]. In the monitoring of the biochemical thyroid function, it is important to realize that all patients in ICU have non-thyroidal illness (NTI) [55] with uninterpretable thyroid function tests. The best is to continue the regular replacement dose independent of the false thyroid function measurements to avoid both suboptimal and excessive replacement [56].
Conclusions
Hypothyroidism is very prevalent at all age groups and represents a non-communicable disease in which the risks and consequences are preventable. However, the diagnosis is often delayed for long periods with resulting consequences for the individual and the society. Excessive LT4 overdosing also infers serious risks such as osteoporosis, cardiac arrythmias and heart failure, muscle wasting, poor quality of life, and cognitive disturbances.
Hypothyroidism as a non-communicable disease is not part of any governmental focus. Suboptimal management of the preventable hypothyroidism resulting in a risk of both under- and excessive treatment, therefore, requires more focus both from caretakers in the healthcare system, but also from the global political systems to prevent the personally devastating and socioeconomically challenging consequences.
References
Wiersinga WM (2000) Adult hypothyroidism. In: Feingold KR, Anawalt B, Blackman MR et al (eds) Endotext [Internet]. MDText.com, Inc. South Dartmouth, MA
Harington CR, Barger G (1927) Chemistry of thyroxine: constitution and synthesis of thyroxine. Biochem J 21:169–183. https://doi.org/10.1042/bj0210169
Gross J, Pitt-Rivers R (1952) The identification of 3:5:3’-l-triiodothyronine in human plasma. Lancet 1:439–441. https://doi.org/10.1016/s0140-6736(52)91952-1
Riis KR, Frølich JS, Hegedüs L et al (2021) Use of thyroid hormones in hypothyroid and euthyroid patients: a 2020 THESIS questionnaire survey of members of the Danish Endocrine Society. J Endocrinol Invest 44:2435–2444. https://doi.org/10.1007/s40618-021-01555-y
Hart FD, Maclagan NF (1950) Oral thyroxine in the treatment of myxoedema. Br Med J 1:512–518. https://doi.org/10.1136/bmj.1.4652.512
Chiovato L, Magri F, Carlé A (2019) Hypothyroidism in context: where we’ve been and where we’re going. Adv Ther 36:47–58. https://doi.org/10.1007/s12325-019-01080-8
Feldt-Rasmussen U, Klose M (2000) Clinical strategies in the testing of Thyroid Function. In: Feingold KR, Anawalt B, Boyce A et al (eds) Endotext [Internet]. MDText.com Inc., South Dartmouth, MA
Zimmermann MB, Boelaert K (2015) Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol 3:286–295. https://doi.org/10.1016/S2213-8587(14)70225-6
Naafs JC, Heinen CA, Zwaveling-Soonawala N et al (2020) Age-specific reference intervals for plasma free thyroxine and thyrotropin in term neonates during the first two weeks of life. Thyroid 30:1106–1111. https://doi.org/10.1089/thy.2019.0779
Boas M, Forman JL, Juul A et al (2009) Narrow intra-individual variation of maternal thyroid function in pregnancy based on a longitudinal study on 132 women. Eur J Endocrinol 161:903–910. https://doi.org/10.1530/EJE-09-0579
Taylor PN, Lansdown A, Witczak J et al (2023) Age-related variation in thyroid function - a narrative review highlighting important implications for research and clinical practice. Thyroid Res 16:7. https://doi.org/10.1186/s13044-023-00149-5
Atzmon G, Barzilai N, Surks MI, Gabriely I (2009) Genetic predisposition to elevated serum thyrotropin is associated with exceptional longevity. J Clin Endocrinol Metab 94:4768–4775. https://doi.org/10.1210/jc.2009-0808
Favresse J, Burlacu M-C, Maiter D, Gruson D (2018) Interferences with thyroid function immunoassays: clinical implications and detection algorithm. Endocr Rev 39:830–850. https://doi.org/10.1210/er.2018-00119
Evron JM, Hummel SL, Reyes-Gastelum D et al (2022) Association of thyroid hormone treatment intensity with cardiovascular mortality among US veterans. JAMA Netw Open 5:e2211863. https://doi.org/10.1001/jamanetworkopen.2022.11863
Croce L, Chytiris S, Coperchini F et al (2023) Unexplained hyperthyrotropinemia: a biochemical and clinical challenge. JCM 12:2934. https://doi.org/10.3390/jcm12082934
Hattori N, Ishihara T, Matsuoka N et al (2017) Anti-thyrotropin autoantibodies in patients with macro-thyrotropin and long-term changes in macro-thyrotropin and serum thyrotropin levels. Thyroid 27:138–146. https://doi.org/10.1089/thy.2016.0442
Virili C, Stramazzo I, Centanni M (2021) Gut microbiome and thyroid autoimmunity. Best Pract Res Clin Endocrinol Metab 35:101506. https://doi.org/10.1016/j.beem.2021.101506
Fallahi P, Ferrari SM, Elia G et al (2021) L-T4 therapy in enteric malabsorptive disorders. Front Endocrinol (Lausanne) 12:626371. https://doi.org/10.3389/fendo.2021.626371
Ford G, LaFranchi SH (2014) Screening for congenital hypothyroidism: a worldwide view of strategies. Best Pract Res Clin Endocrinol Metab 28:175–187. https://doi.org/10.1016/j.beem.2013.05.008
Yu A, Alder N, Lain SJ et al (2023) Outcomes of lowered newborn screening thresholds for congenital hypothyroidism. J Paediatr Child Health. https://doi.org/10.1111/jpc.16425
Omuse G, Kawalya D, Mugaine P et al (2023) Neonatal reference intervals for thyroid stimulating hormone and free thyroxine assayed on a Siemens Atellica® IM analyzer: a cross sectional study. BMC Endocr Disord 23:112. https://doi.org/10.1186/s12902-023-01367-6
Maria S (2017) Disorders of the thyroid gland in infancy, childhood and adolescence. https://www.endotext.org/chapter/disorders-of-the-thyroid-gland-in-infancy-childhood-and-adolescence-3/. Accessed 5 Oct 2023
Korevaar TIM, Derakhshan A, Taylor PN et al (2019) Association of thyroid function test abnormalities and thyroid autoimmunity with preterm birth: a systematic review and meta-analysis. JAMA 322:632–641. https://doi.org/10.1001/jama.2019.10931
Bliddal S, Feldt-Rasmussen U, Rasmussen ÅK et al (2019) Thyroid peroxidase antibodies and prospective live birth rate: a cohort study of women with recurrent pregnancy loss. Thyroid 29:1465–1474. https://doi.org/10.1089/thy.2019.0077
Alexander EK, Pearce EN, Brent GA et al (2017) 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid 27:315–389. https://doi.org/10.1089/thy.2016.0457
Krassas GE, Poppe K, Glinoer D (2010) Thyroid function and human reproductive health. Endocr Rev 31:702–755. https://doi.org/10.1210/er.2009-0041
Rao M, Zeng Z, Zhao S, Tang L (2018) Effect of levothyroxine supplementation on pregnancy outcomes in women with subclinical hypothyroidism and thyroid autoimmunity undergoing in vitro fertilization/intracytoplasmic sperm injection: an updated meta-analysis of randomized controlled trials. Reprod Biol Endocrinol 16:92. https://doi.org/10.1186/s12958-018-0410-6
Maraka S, Mwangi R, McCoy RG et al (2017) Thyroid hormone treatment among pregnant women with subclinical hypothyroidism: US national assessment. BMJ 356:i6865. https://doi.org/10.1136/bmj.i6865
Lazarus JH, Bestwick JP, Channon S et al (2012) Antenatal thyroid screening and childhood cognitive function. N Engl J Med 366:493–501. https://doi.org/10.1056/NEJMoa1106104
Casey BM, Thom EA, Peaceman AM et al (2017) Treatment of subclinical hypothyroidism or hypothyroxinemia in pregnancy. N Engl J Med 376:815–825. https://doi.org/10.1056/NEJMoa1606205
Peng CC-H, Pearce EN (2022) An update on thyroid disorders in the postpartum period. J Endocrinol Invest 45:1497–1506. https://doi.org/10.1007/s40618-022-01762-1
Hollowell JG, Staehling NW, Flanders WD et al (2002) Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab 87:489–499. https://doi.org/10.1210/jcem.87.2.8182
Vadiveloo T, Donnan PT, Murphy MJ, Leese GP (2013) Age- and gender-specific TSH reference intervals in people with no obvious thyroid disease in Tayside, Scotland: the thyroid epidemiology, audit, and research study (TEARS). J Clin Endocrinol Metab 98:1147–1153. https://doi.org/10.1210/jc.2012-3191
Atzmon G, Barzilai N, Hollowell JG et al (2009) Extreme longevity is associated with increased serum thyrotropin. J Clin Endocrinol Metab 94:1251–1254. https://doi.org/10.1210/jc.2008-2325
Boucai L, Surks MI (2009) Reference limits of serum TSH and free T4 are significantly influenced by race and age in an urban outpatient medical practice. Clin Endocrinol 70:788–793. https://doi.org/10.1111/j.1365-2265.2008.03390.x
Effraimidis G, Watt T, Feldt-Rasmussen U (2021) Levothyroxine therapy in elderly patients with hypothyroidism. Front Endocrinol 12:641560. https://doi.org/10.3389/fendo.2021.641560
Surks MI, Hollowell JG (2007) Age-specific distribution of serum thyrotropin and antithyroid antibodies in the US population: implications for the prevalence of subclinical hypothyroidism. J Clin Endocrinol Metab 92:4575–4582. https://doi.org/10.1210/jc.2007-1499
Jansen SW, Roelfsema F, van der Spoel E et al (2015) Familial longevity is associated with higher TSH secretion and strong TSH-fT3 relationship. J Clin Endocrinol Metab 100:3806–3813. https://doi.org/10.1210/jc.2015-2624
Livecchi R, Coe AB, Reyes-Gastelum D et al (2022) Concurrent use of thyroid hormone therapy and interfering medications in older US veterans. J Clin Endocrinol Metab 107:e2738–e2742. https://doi.org/10.1210/clinem/dgac216
Garber JR, Cobin RH, Gharib H et al (2012) Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid 22:1200–1235. https://doi.org/10.1089/thy.2012.0205
Akirov A, Shochat T, Shechvitz A et al (2017) Pre-admission TSH levels predict long-term mortality in adults treated for hypothyroidism. Endocrine 58:481–487. https://doi.org/10.1007/s12020-017-1453-8
Akirov A, Gimbel H, Grossman A et al (2017) Elevated TSH in adults treated for hypothyroidism is associated with increased mortality. Eur J Endocrinol 176:57–66. https://doi.org/10.1530/EJE-16-0708
Thayakaran R, Adderley NJ, Sainsbury C et al (2019) Thyroid replacement therapy, thyroid stimulating hormone concentrations, and long term health outcomes in patients with hypothyroidism: longitudinal study. BMJ 366:l4892. https://doi.org/10.1136/bmj.l4892
Lillevang-Johansen M, Abrahamsen B, Jørgensen HL et al (2018) Over- and under-treatment of hypothyroidism is associated with excess mortality: a register-based cohort study. Thyroid 28:566–574. https://doi.org/10.1089/thy.2017.0517
Biondi B (2019) The management of thyroid abnormalities in chronic heart failure. Heart Fail Clin 15:393–398. https://doi.org/10.1016/j.hfc.2019.02.008
Feldt-Rasmussen U (2007) Treatment of hypothyroidism in elderly patients and in patients with cardiac disease. Thyroid 17:619–624. https://doi.org/10.1089/thy.2007.0033
Corona G, Croce L, Sparano C et al (2021) Thyroid and heart, a clinically relevant relationship. J Endocrinol Invest 44:2535–2544. https://doi.org/10.1007/s40618-021-01590-9
Brandt F, Green A, Hegedüs L, Brix TH (2011) A critical review and meta-analysis of the association between overt hyperthyroidism and mortality. Eur J Endocrinol 165:491–497. https://doi.org/10.1530/EJE-11-0299
Sohn SY, Lee E, Lee MK, Lee JH (2020) The association of overt and subclinical hyperthyroidism with the risk of cardiovascular events and cardiovascular mortality: meta-analysis and systematic review of cohort studies. Endocrinol Metab 35:786–800. https://doi.org/10.3803/EnM.2020.728
Persani L (2012) Clinical review: central hypothyroidism: pathogenic, diagnostic, and therapeutic challenges. J Clin Endocrinol Metab 97:3068–3078. https://doi.org/10.1210/jc.2012-1616
Persani L, Brabant G, Dattani M et al (2018) 2018 European Thyroid Association (ETA) Guidelines on the diagnosis and management of central hypothyroidism. Eur Thyroid J 7:225–237. https://doi.org/10.1159/000491388
Feldt-Rasmussen U, Effraimidis G, Klose M (2021) The hypothalamus-pituitary-thyroid (HPT)-axis and its role in physiology and pathophysiology of other hypothalamus-pituitary functions. Mol Cell Endocrinol 525:111173. https://doi.org/10.1016/j.mce.2021.111173
Feldt-Rasmussen U, Klose M (2016) Central hypothyroidism and its role for cardiovascular risk factors in hypopituitary patients. Endocrine 54:15–23. https://doi.org/10.1007/s12020-016-1047-x
Gatta E, Bambini F, Buoso C et al (2022) Liquid levothyroxine formulations in patients taking drugs interfering with L-T4 absorption. Front Endocrinol 13:1080108. https://doi.org/10.3389/fendo.2022.1080108
Peeters RP, Boelen A (2021) Non-thyroidal Illness (NTI). In: Wass JAH, Stewart PM, Amiel SA, Davies M (eds) Oxford textbook of endocrinology and diabetes, 3rd edn. Oxford University Press, Oxford
Feldt-Rasmussen U (2020) Laboratory measurement of thyroid-related hormones, proteins, and autoantibodies in serum. In: Braverman LE, Cooper DS, Kopp P (eds) Werner and Ingbar"s the thyroid: a fundamental and clinical text, 11th edn. Williams & Wilkins, Lippincott, pp 868–907
Acknowledgements
UFR’s research salary was sponsored by The Kirsten and Freddy Johansen’s Fund. SB’s research salary was sponsored by a grant from the Novo Nordisk Foundation (ID 0077221).
Funding
This is study was funded by Kirsten og Freddy Johansens Fond, Novo Nordisk Fonden, ID 0077221, Sofie Bliddal.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
UFR has received speaker honoraria and travel costs from Merck, Darmstadt, Germany and Horizon, Maryland, USA. SB has received a speaker honorary from Merck, Darmstadt, Germany, and Novo Nordisk, Copenhagen, Denmark.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
No informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Feldt-Rasmussen, U., Effraimidis, G., Bliddal, S. et al. Risks of suboptimal and excessive thyroid hormone replacement across ages. J Endocrinol Invest 47, 1083–1090 (2024). https://doi.org/10.1007/s40618-023-02229-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02229-7