Abstract
Purpose
The clinical significance of metabolic syndrome (MetS) versus its single components in erectile dysfunction (ED) is conflicting. Thus, the purpose is to analyze the available evidence on the relationship between MetS—along with its components—and ED.
Methods
All prospective and retrospective observational studies reporting information on ED and MetS were included. In addition, we here reanalyzed preclinical and clinical data obtained from a previously published animal model of MetS and from a consecutive series of more than 2697 men (mean age: 52.7 ± 12), respectively.
Results
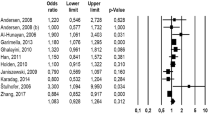
Data derived from this meta-analysis showed that MetS was associated with an up to fourfold increased risk of ED when either unadjusted or adjusted data were considered. Meta-regression analysis, performed using unadjusted statistics, showed that the MetS-related risk of ED was closely associated with all the MetS components. These associations were confirmed when unadjusted analyses from clinical models were considered. However, fully adjusted data showed that MetS-associated ED was more often due to morbidities included (or not) in the algorithm than to the MetS diagnostic category itself. MetS is also associated with low testosterone, but its contribution to MetS-associated ED—as derived from preclinical and clinical models—although independent, is marginal.
Conclusions
The results of our analysis suggest that MetS is a useless diagnostic category for studying ED. However, treating the individual MetS components is important, because they play a pivotal role in determining ED.






Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Lotti F, Marchiani S, Corona G, Maggi M (2021) Metabolic syndrome and reproduction. Int J Mol Sci 22(4):1988. https://doi.org/10.3390/ijms22041988
Esposito K, Giugliano F, Martedì E, Feola G, Marfella R, D’Armiento M et al (2005) High proportions of erectile dysfunction in men with the metabolic syndrome. Diabetes Care 28(5):1201–1203
Corona G, Mannucci E, Schulman C, Petrone L, Mansani R, Cilotti A et al (2006) Psychobiologic correlates of the metabolic syndrome and associated sexual dysfunction. Eur Urol 50(3):595–604 (discussion)
Demir T, Demir O, Kefi A, Comlekci A, Yesil S, Esen A (2006) Prevalence of erectile dysfunction in patients with metabolic syndrome. Int J Urol 13(4):385–388
Liu LH, Zhang T, Zhang YR, Liu TS, Zhang HB, Chen FZ et al (2014) Metabolic syndrome and risk for ED: a meta-analysis. Int J Impot Res 26(5):196–200
Besiroglu H, Otunctemur A, Ozbek E (2015) The relationship between metabolic syndrome, its components, and erectile dysfunction: a systematic review and a meta-analysis of observational studies. J Sex Med 12(6):1309–1318
Corona G, Rastrelli G, Isidori AM, Pivonello R, Bettocchi C, Reisman Y et al (2020) Erectile dysfunction and cardiovascular risk: a review of current findings. Expert Rev Cardiovasc Ther 18(3):155–164
Antonio L, Wu FCW, Moors H, Matheï C, Huhtaniemi IT, Rastrelli G et al (2022) Erectile dysfunction predicts mortality in middle-aged and older men independent of their sex steroid status. Age Ageing 51(4):afac094. https://doi.org/10.1093/ageing/afac094
Corona G, Rastrelli G, Balercia G, Lotti F, Sforza A, Monami M et al (2012) Hormonal association and sexual dysfunction in patients with impaired fasting glucose: a cross-sectional and longitudinal study. J Sex Med 9(6):1669–1680
Corona G, Monami M, Rastrelli G, Melani C, Balzi D, Sforza A et al (2011) Is metabolic syndrome a useless category in subjects with high cardiovascular risk? Results from a cohort study in men with erectile dysfunction. J Sex Med 8(2):504–511
Corona G, Maggi M (2022) The role of testosterone in male sexual function. Rev Endocr Metab Disord 23(6):1159–1172
Corona G, Rastrelli G, Vignozzi L, Maggi M (2022) Androgens and male sexual function. Best Pract Res Clin Endocrinol Metab 36(4):101615. https://doi.org/10.1016/j.beem.2022.101615
Corona G, Torres LO, Maggi M (2020) Testosterone therapy: what we have learned from trials. J Sex Med 17(3):447–460
Rastrelli G, Corona G, Maggi M (2018) Testosterone and sexual function in men. Maturitas 112:46–52
Rastrelli G, Guaraldi F, Reismann Y, Sforza A, Isidori AM, Maggi M et al (2019) Testosterone replacement therapy for sexual symptoms. Sex Med Rev. 7(3):464–475
Corona G, Monami M, Rastrelli G, Aversa A, Tishova Y, Saad F et al (2011) Testosterone and metabolic syndrome: a meta-analysis study. J Sex Med 8(1):272–283
Filippi S, Vignozzi L, Morelli A, Chavalmane AK, Sarchielli E, Fibbi B et al (2009) Testosterone partially ameliorates metabolic profile and erectile responsiveness to PDE5 inhibitors in an animal model of male metabolic syndrome. J Sex Med 6(12):3274–3288
Morelli A, Filippi S, Comeglio P, Sarchielli E, Cellai I, Pallecchi M et al (2019) Physical activity counteracts metabolic syndrome-induced hypogonadotropic hypogonadism and erectile dysfunction in the rabbit. Am J Physiol Endocrinol Metab 316(3):E519–E535
Marchiani S, Vignozzi L, Filippi S, Gurrieri B, Comeglio P, Morelli A et al (2015) Metabolic syndrome-associated sperm alterations in an experimental rabbit model: relation with metabolic profile, testis and epididymis gene expression and effect of tamoxifen treatment. Mol Cell Endocrinol 401:12–24
Morelli A, Sarchielli E, Comeglio P, Filippi S, Vignozzi L, Marini M et al (2014) Metabolic syndrome induces inflammation and impairs gonadotropin-releasing hormone neurons in the preoptic area of the hypothalamus in rabbits. Mol Cell Endocrinol 382(1):107–119
Corona G, Mannucci E, Petrone L, Fisher AD, Balercia G, De Scisciolo G et al (2006) Psychobiological correlates of delayed ejaculation in male patients with sexual dysfunctions. J Androl 27(3):453–458
Corona G, Ricca V, Bandini E, Mannucci E, Petrone L, Fisher AD et al (2008) Association between psychiatric symptoms and erectile dysfunction. J Sex Med 5(2):458–468
Bal K, Oder M, Sahin AS, Karataş CT, Demir O, Can E et al (2007) Prevalence of metabolic syndrome and its association with erectile dysfunction among urologic patients: metabolic backgrounds of erectile dysfunction. Urology 69(2):356–360
Yeh HC, Wang CJ, Lee YC, Hsiao HL, Wu WJ, Chou YH et al (2008) Association among metabolic syndrome, testosterone level and severity of erectile dysfunction. Kaohsiung J Med Sci 24(5):240–247
Demir O, Demir T, Kefi A, Secil M, Comlekci A, Yesil S et al (2009) Penile vascular impairment in erectile dysfunction patients with metabolic syndrome: penile Doppler ultrasound findings. Urol Int 82(2):175–178
Gatti A, Mandosi E, Fallarino M, Radicioni A, Morini E, Maiani F et al (2009) Metabolic syndrome and erectile dysfunction among obese non-diabetic subjects. J Endocrinol Investig 32(6):542–545
Koca O, Calışkan S, Oztürk M, Güneş M, Kılıçoğlu G, Karaman MI (2010) Vasculogenic erectile dysfunction and metabolic syndrome. J Sex Med 7(12):3997–4002
Lee YC, Liu CC, Huang CN, Li WM, Wu WJ, Yeh HC et al (2010) The potential impact of metabolic syndrome on erectile dysfunction in aging Taiwanese males. J Sex Med 7(9):3127–3134
Aktas BK, Gokkaya CS, Bulut S, Dinek M, Ozden C, Memis A (2011) Impact of metabolic syndrome on erectile dysfunction and lower urinary tract symptoms in benign prostatic hyperplasia patients. Aging Male 14(1):48–52
Pohjantähti-Maaroos H, Palomäki A (2011) Comparison of metabolic syndrome subjects with and without erectile dysfunction—levels of circulating oxidised LDL and arterial elasticity. Int J Clin Pract 65(3):274–280
Tan WS, Ng CJ, Khoo EM, Low WY, Tan HM (2011) The triad of erectile dysfunction, testosterone deficiency syndrome and metabolic syndrome: findings from a multi-ethnic Asian men study (The Subang Men’s Health Study). Aging Male 14(4):231–236
Chao JK, Kuo WH, Chiang HS, Hwang TI, Chao IC, Chiang SK (2012) Association of metabolic syndrome, atherosclerosis risk factors, sex hormones in ED in aboriginal Taiwanese. Int J Impot Res 24(4):141–146
Chen K, Mi H, Gao Y, Tan A, Lu Z, Wu C et al (2012) Metabolic syndrome: a potential and independent risk factor for erectile dysfunction in the Chinese male population. Urology 80(6):1287–1292
García-Cruz E, Leibar-Tamayo A, Romero J, Piqueras M, Luque P, Cardeñosa O et al (2013) Metabolic syndrome in men with low testosterone levels: relationship with cardiovascular risk factors and comorbidities and with erectile dysfunction. J Sex Med 10(10):2529–2538
Weinberg AE, Eisenberg M, Patel CJ, Chertow GM, Leppert JT (2013) Diabetes severity, metabolic syndrome, and the risk of erectile dysfunction. J Sex Med 10(12):3102–3109
Aslan Y, Guzel O, Balci M, Tuncel A, Yildiz M, Atan A (2014) The impact of metabolic syndrome on serum total testosterone level in patients with erectile dysfunction. Aging Male 17(2):76–80
Gorgel SN, Gorgel A, Sefik E (2014) Sexual function in male patients with metabolic syndrome and effective parameters on erectile dysfunction. Int Braz J Urol 40(1):56–61
Park JH, Cho IC, Kim YS, Kim SK, Min SK, Kye SS (2015) Body mass index, waist-to-hip ratio, and metabolic syndrome as predictors of middle-aged men’s health. Korean J Urol 56(5):386–392
Chaudhary RK, Shamsi BH, Tan T, Chen HM, Xing JP (2016) Study of the relationship between male erectile dysfunction and type 2 diabetes mellitus/metabolic syndrome and its components. J Int Med Res 44(3):735–741
De Nunzio C, Lombardo R, Gacci M, Nacchia A, Presicce F, Alkhatatbeh H et al (2017) Metabolic syndrome does not increase the risk of ejaculatory dysfunction in patients with lower urinary tract symptoms and benign prostatic enlargement: an Italian single-center cohort study. Urology 105:85–90
Erkoc M, Besiroglu H, Otunctemur A, Polat EC, Bozkurt M (2020) Metabolic syndrome is associated worsened erectile function in patients undergoing TURP due to benign prostatic hyperplasia. Aging Male 23(5):533–537
Salama MN, Eid AA, Hatem A, Swidan AK (2020) Prevalence of erectile dysfunction in Egyptian males with metabolic syndrome. Aging Male 23(4):257–263
Bolat MS, Ozbek ML, Şahin B, Yılmaz M, Kocamanoglu F, Buyukalpelli R et al (2021) Impact of high visceral adiposity index associated with metabolic syndrome on erectile function in sexually active men: results of a cross-sectional study. Int J Clin Pract 75(6):e14111
Neuzillet Y, Dreyfus JF, Raynaud JP, Rouanne M, Schneider M, Roupret M et al (2021) Relationship of preoperative androgen levels and metabolic syndrome with quality of life and erectile function in patients who are to undergo radical prostatectomy. Asian J Androl 23(5):520–526
Rosen RC, Allen KR, Ni X, Araujo AB (2011) Minimal clinically important differences in the erectile function domain of the International Index of Erectile Function scale. Eur Urol 60(5):1010–1016
Corona G, Rastrelli G, Vignozzi L, Barbonetti A, Sforza A, Mannucci E et al (2021) The role of testosterone treatment in patients with metabolic disorders. Expert Rev Clin Pharmacol 14(9):1091–1103. https://doi.org/10.1080/17512433.2021.1938548
Corona G, Goulis DG, Huhtaniemi I, Zitzmann M, Toppari J, Forti G et al (2020) European Academy of Andrology (EAA) guidelines on investigation, treatment and monitoring of functional hypogonadism in males: endorsing organization: European Society of Endocrinology. Andrology 8(5):970–987
Salonia A, Bettocchi C, Boeri L, Capogrosso P, Carvalho J, Cilesiz NC et al (2021) European Association of urology guidelines on sexual and reproductive health-2021 update: male sexual dysfunction. Eur Urol 80(3):333–357
Isidori AM, Aversa A, Calogero A, Ferlin A, Francavilla S, Lanfranco F et al (2022) Adult- and late-onset male hypogonadism: the clinical practice guidelines of the Italian Society of Andrology and Sexual Medicine (SIAMS) and the Italian Society of Endocrinology (SIE). J Endocrinol Invest 45(12):2385–2403. https://doi.org/10.1007/s40618-022-01859-
Wong SK, Chin KY, Suhaimi FH, Fairus A, Ima-Nirwana S (2016) Animal models of metabolic syndrome: a review. Nutr Metab (Lond) 13:65
Fahed G, Aoun L, Bou Zerdan M, Allam S, Bou Zerdan M, Bouferraa Y et al (2022) Metabolic syndrome: updates on pathophysiology and management in 2021. Int J Mol Sci 23(2):786. https://doi.org/10.3390/ijms23020786
Pitsavos C, Panagiotakos D, Weinem M, Stefanadis C (2006) Diet, exercise and the metabolic syndrome. Rev Diabet Stud 3(3):118–126
Vignozzi L, Filippi S, Comeglio P, Cellai I, Morelli A, Marchetta M et al (2014) Estrogen mediates metabolic syndrome-induced erectile dysfunction: a study in the rabbit. J Sex Med 11(12):2890–2902
Maggi R, Zasso J, Conti L (2014) Neurodevelopmental origin and adult neurogenesis of the neuroendocrine hypothalamus. Front Cell Neurosci 8:440
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA et al (2005) Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 112(17):2735–2752
Rastrelli G, Filippi S, Sforza A, Maggi M, Corona G (2018) Metabolic syndrome in male hypogonadism. Front Horm Res 49:131–155
Von Korff M, Wagner EH, Saunders K (1992) A chronic disease score from automated pharmacy data. J Clin Epidemiol 45(2):197–203
Rastrelli G, Corona G, Maggi M (2020) Both comorbidity burden and low testosterone can explain symptoms and signs of testosterone deficiency in men consulting for sexual dysfunction. Asian J Androl 22(3):265–273
Brand JS, Rovers MM, Yeap BB, Schneider HJ, Tuomainen TP, Haring R et al (2014) Testosterone, sex hormone-binding globulin and the metabolic syndrome in men: an individual participant data meta-analysis of observational studies. PLoS ONE 9(7):e100409
Petrone L, Mannucci E, Corona G, Bartolini M, Forti G, Giommi R et al (2003) Structured interview on erectile dysfunction (SIEDY): a new, multidimensional instrument for quantification of pathogenetic issues on erectile dysfunction. Int J Impot Res 15(3):210–220
Corona G, Sansone A, Pallotti F, Ferlin A, Pivonello R, Isidori AM et al (2020) People smoke for nicotine, but lose sexual and reproductive health for tar: a narrative review on the effect of cigarette smoking on male sexuality and reproduction. J Endocrinol Investig 43(10):1391–1408
Marieke D, Joana C, Giovanni C, Erika L, Patricia P, Yacov R et al (2020) Sexual desire discrepancy: a position statement of the european society for sexual medicine. Sex Med 8(2):121–131
Dewitte M, Bettocchi C, Carvalho J, Corona G, Flink I, Limoncin E et al (2021) A psychosocial approach to erectile dysfunction: position statements from the European Society of Sexual Medicine (ESSM). Sex Med 9(6):100434
Boddi V, Corona G, Fisher AD, Mannucci E, Ricca V, Sforza A et al (2012) “It takes two to tango”: the relational domain in a cohort of subjects with erectile dysfunction (ED). J Sex Med 9(12):3126–3136
Corona G, Ricca V, Bandini E, Rastrelli G, Casale H, Jannini EA et al (2012) SIEDY scale 3, a new instrument to detect psychological component in subjects with erectile dysfunction. J Sex Med 9(8):2017–2026
Grossmann M, Mg Tang Fui M, Cheung AS (2020) Late-onset hypogonadism: metabolic impact. Andrology 8(6):1519–1529
Corona G, Isidori AM, Aversa A, Burnett AL, Maggi M (2016) Endocrinologic control of men’s sexual desire and arousal/erection. J Sex Med 13(3):317–337
Corona G, Rastrelli G, Ricca V, Jannini EA, Vignozzi L, Monami M et al (2013) Risk factors associated with primary and secondary reduced libido in male patients with sexual dysfunction. J Sex Med 10(4):1074–1089
Bhasin S, Brito JP, Cunningham GR, Hayes FJ, Hodis HN, Matsumoto AM et al (2018) Testosterone therapy in men with hypogonadism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 103(5):1715–1744
Lunenfeld B, Mskhalaya G, Zitzmann M, Corona G, Arver S, Kalinchenko S et al (2021) Recommendations on the diagnosis, treatment and monitoring of testosterone deficiency in men. Aging Male 24(1):119–138
Sun K, Ren M, Liu D, Wang C, Yang C, Yan L (2014) Alcohol consumption and risk of metabolic syndrome: a meta-analysis of prospective studies. Clin Nutr 33(4):596–602
Sun K, Liu J, Ning G (2012) Active smoking and risk of metabolic syndrome: a meta-analysis of prospective studies. PLoS ONE 7(10):e47791
Lee G, Choi HY, Yang SJ (2015) Effects of dietary and physical activity interventions on metabolic syndrome: a meta-analysis. J Korean Acad Nurs 45(4):483–494
Castro VMF, Melo AC, Belo VS, Chaves VE (2017) Effect of allopurinol and uric acid normalization on serum lipids hyperuricemic subjects: a systematic review with meta-analysis. Clin Biochem 50(18):1289–1297
Kwon OY, Choi JY, Jang Y (2023) The effectiveness of ehealth interventions on lifestyle modification in patients with nonalcoholic fatty liver disease: systematic review and meta-analysis. J Med Internet Res 25:e37487
Sansone A, Reisman Y, Jannini EA (2022) Relationship between hyperuricemia with deposition and sexual dysfunction in males and females. J Endocrinol Investig 45(4):691–703
Hasanain AFA, Mahdy RE, Mahran AMA, Safwat ASM, Mohamed AO, Abdel-Aal SM (2017) Erectile dysfunction in patients with nonalcoholic fatty liver disease. Arab J Gastroenterol 18(1):21–24
Wang XY, Huang W, Zhang Y (2018) Relation between hypertension and erectile dysfunction: a meta-analysisof cross-section studies. Int J Impot Res 30(3):141–146
Behr-Roussel D, Gorny D, Mevel K, Compagnie S, Kern P, Sivan V et al (2005) Erectile dysfunction: an early marker for hypertension? A longitudinal study in spontaneously hypertensive rats. Am J Physiol Regul Integr Comp Physiol 288(1):R276–R283
Fibbi B, Morelli A, Marini M, Zhang XH, Mancina R, Vignozzi L et al (2008) Atorvastatin but not elocalcitol increases sildenafil responsiveness in spontaneously hypertensive rats by regulating the RhoA/ROCK pathway. J Androl 29(1):70–84
Corona G, Mannucci E, Lotti F, Fisher AD, Bandini E, Balercia G et al (2009) Pulse pressure, an index of arterial stiffness, is associated with androgen deficiency and impaired penile blood flow in men with ED. J Sex Med 6(1):285–293
Corona G, Monami M, Boddi V, Rastrelli G, Melani C, Balzi D et al (2011) Pulse pressure independently predicts major cardiovascular events in younger but not in older subjects with erectile dysfunction. J Sex Med 8(1):247–254
Farmakis IT, Pyrgidis N, Doundoulakis I, Mykoniatis I, Akrivos E, Giannakoulas G (2021) Effects of major antihypertensive drug classes on erectile function: a network meta-analysis. Cardiovasc Drugs Ther 36(5):903–914
Farmakis IT, Pyrgidis N, Doundoulakis I, Mykoniatis I, Akrivos E, Giannakoulas G (2022) Effects of major antihypertensive drug classes on erectile function: a network meta-analysis. Cardiovasc Drugs Ther 36(5):903–914
Kouidrat Y, Pizzol D, Cosco T, Thompson T, Carnaghi M, Bertoldo A et al (2017) High prevalence of erectile dysfunction in diabetes: a systematic review and meta-analysis of 145 studies. Diabet Med 34(9):1185–1192
Corona G, Rastrelli G, Silverii A, Monami M, Sforza A, Forti G et al (2013) The identification of prediabetes condition with ARIC algorithm predicts long-term CV events in patients with erectile dysfunction. J Sex Med 10(4):1114–1123
Jin M, Yuan S, Wang B, Yi L, Wang C (2021) Association between prediabetes and erectile dysfunction: a meta-analysis. Front Endocrinol (Lausanne) 12:733434
Fedele D, Bortolotti A, Coscelli C, Santeusanio F, Chatenoud L, Colli E et al (2000) Erectile dysfunction in type 1 and type 2 diabetics in Italy. On behalf of Gruppo Italiano Studio Deficit Erettile nei Diabetici. Int J Epidemiol 29(3):524–531
Corona G, Bianchini S, Sforza A, Vignozzi L, Maggi M (2015) Hypogonadism as a possible link between metabolic diseases and erectile dysfunction in aging men. Hormones (Athens) 14(4):569–578
Sansone A, Mollaioli D, Ciocca G, Limoncin E, Colonnello E, Jannini EA (2022) Sexual dysfunction in men and women with diabetes: a reflection of their complications? Curr Diabetes Rev 18(1):e030821192147
Li M, Ma Z, Zhang XL, Guo LQ, Yuan MZ (2020) Significance of blood lipid parameters as effective markers for arteriogenic erectile dysfunction. Andrology 8(5):1086–1094
Corona G, Cipriani S, Rastrelli G, Sforza A, Mannucci E, Maggi M (2016) High triglycerides predicts arteriogenic erectile dysfunction and major adverse cardiovascular events in subjects with sexual dysfunction. J Sex Med 13(9):1347–1358
Xu ZH, Xu HX, Jiang S, Xu QF, Ding K, Zhang DX et al (2021) Effect of high-density lipoprotein on penile erection: a cross-sectional study. Andrologia 53(5):e13979
Uittenbogaard A, Shaul PW, Yuhanna IS, Blair A, Smart EJ (2000) High density lipoprotein prevents oxidized low density lipoprotein-induced inhibition of endothelial nitric-oxide synthase localization and activation in caveolae. J Biol Chem 275(15):11278–11283
Li XP, Zhao SP, Zhang XY, Liu L, Gao M, Zhou QC (2000) Protective effect of high density lipoprotein on endothelium-dependent vasodilatation. Int J Cardiol 73(3):231–236
Rämet ME, Rämet M, Lu Q, Nickerson M, Savolainen MJ, Malzone A et al (2003) High-density lipoprotein increases the abundance of eNOS protein in human vascular endothelial cells by increasing its half-life. J Am Coll Cardiol 41(12):2288–2297
Lotti F, Rastrelli G, Maseroli E, Cipriani S, Guaraldi F, Krausz C et al (2019) Impact of metabolically healthy obesity in patients with andrological problems. J Sex Med 16(6):821–832
Rastrelli G, Lotti F, Reisman Y, Sforza A, Maggi M, Corona G (2019) Metabolically healthy and unhealthy obesity in erectile dysfunction and male infertility. Expert Rev Endocrinol Metab 14(5):321–334
Molloy GJ, Stamatakis E, Randall G, Hamer M (2009) Marital status, gender and cardiovascular mortality: behavioural, psychological distress and metabolic explanations. Soc Sci Med 69(2):223–228
Corona G, Rastrelli G, Monami M, Maseroli E, Jannini EA, Balercia G et al (2013) Frequency of sexual activity and cardiovascular risk in subjects with erectile dysfunction: cross-sectional and longitudinal analyses. Andrology 1(6):864–871
Maggi M, Corona G (2011) Love protects lover’s life. J Sex Med 8(4):931–935
Corona G, Bandini E, Fisher A, Elisa M, Boddi V, Balercia G et al (2010) Psychobiological correlates of women’s sexual interest as perceived by patients with erectile dysfunction. J Sex Med 7(6):2174–2183
Waite LJ (1995) Does marriage matter? Demography 32(4):483–507
Nizamani S, McFarlane RA, Knight-Agarwal CR, Somerset S (2022) Couples-based behaviour change interventions to reduce metabolic syndrome risk. A systematic review. Diabetes Metab Syndr 16(12):102662
Corona G, Pizzocaro A, Vena W, Rastrelli G, Semeraro F, Isidori AM et al (2021) Diabetes is most important cause for mortality in COVID-19 hospitalized patients: systematic review and meta-analysis. Rev Endocr Metab Disord 22(2):275–296
Zhang J, Shi W, Zou M, Zeng Q, Feng Y, Luo Z et al (2023) Prevalence and risk factors of erectile dysfunction in COVID-19 patients: a systematic review and meta-analysis. J Endocrinol Invest 46(4):795–804. https://doi.org/10.1007/s40618-022-01945-w
Katz J, Yue S, Xue W, Gao H (2022) Increased odds ratio for erectile dysfunction in COVID-19 patients. J Endocrinol Investig 45(4):859–864
Pizzol D, Shin JI, Trott M, Ilie PC, Ippoliti S, Carrie AM et al (2022) Social environmental impact of COVID-19 and erectile dysfunction: an explorative review. J Endocrinol Investig 45(3):483–487
Paoli D, Pallotti F, Anzuini A, Bianchini S, Caponecchia L, Carraro A et al (2023) Male reproductive health after 3 months from SARS-CoV-2 infection: a multicentric study. J Endocrinol Investig 46(1):89–101
Corona G, Vena W, Pizzocaro A, Pallotti F, Paoli D, Rastrelli G et al (2022) Andrological effects of SARS-Cov-2 infection: a systematic review and meta-analysis. J Endocrinol Invest 45(12):2207–2219. https://doi.org/10.1007/s40618-022-01801-x
Corona G, Baldi E, Isidori AM, Paoli D, Pallotti F, De Santis L et al (2020) SARS-CoV-2 infection, male fertility and sperm cryopreservation: a position statement of the Italian Society of Andrology and Sexual Medicine (SIAMS) (Società Italiana di Andrologia e Medicina della Sessualità). J Endocrinol Investig 43(8):1153–1157
Corona G (2022) Erectile dysfunction and premature ejaculation: a continuum movens supporting couple sexual dysfunction. J Endocrinol Investig 45(11):2029–2041
Corona G, Rastrelli G, Bartfai G, Casanueva FF, Giwercman A, Antonio L et al (2021) Self-reported shorter than desired ejaculation latency and related distress-prevalence and clinical correlates: results from the European male ageing study. J Sex Med 18(5):908–919
Brody S, Weiss P (2015) Erectile dysfunction and premature ejaculation: interrelationships and psychosexual factors. J Sex Med 12(2):398–404
Li H, Xu W, Wang T, Wang S, Liu J, Jiang H (2022) Effect of weight loss on erectile function in men with overweight or obesity: a meta-analysis of randomised controlled trials. Andrologia 54(1):e14250
Gale EA (2005) The myth of the metabolic syndrome. Diabetologia 48(9):1679–1683
Kahn R, Buse J, Ferrannini E, Stern M (2005) The metabolic syndrome: time for a critical appraisal: joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 28(9):2289–2304
Reaven GM (2005) The metabolic syndrome: requiescat in pace. Clin Chem 51(6):931–938
Reaven G (2005) Counterpoint: just being alive is not good enough. Clin Chem 51(8):1354–1357
Grundy SM (2005) Point: the metabolic syndrome still lives. Clin Chem 51(8):1352–1354
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by GC and MM. The first draft of the manuscript was written by GC and MM, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors declared any conflict of interest.
Research involving human participants and/or animals
All the data provided were collected as part of the routine clinical procedure, according to our hospital’s approval protocol (L99-A08 292/2014) for the diagnostic workup for each patient referred to our unit for Sexual dysfunction.
Informed consent
For this type of the study no informed consent was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Corona, D.G., Vena, W., Pizzocaro, A. et al. Metabolic syndrome and erectile dysfunction: a systematic review and meta-analysis study. J Endocrinol Invest 46, 2195–2211 (2023). https://doi.org/10.1007/s40618-023-02136-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-023-02136-x