Abstract
Purpose
The aim of this review is to discuss the role of androgens in the progression of endometrial carcinoma (EC) with particular focus on the different kinds of androgenic hormones, androgen receptor (AR) and intracrine androgen metabolism.
Methods
A comprehensive literature search within PubMed was performed. Selected publications related to androgens and EC were reviewed.
Results
There are different kinds of androgenic hormones, and different kinds of androgens may have different effects. Elevated androgens (especially testosterone) have been associated with an increased EC risk in postmenopausal women. 5α-reductases (5α-Reds) and 17β-hydroxysteroid dehydrogenase type 2 (17βHSD2) pathway may inhibit the progression of EC mediated by dihydrotestosterone (DHT), but aromatases stimulate further progression of EC. The most of studies accessing the prognostic value of AR have found that AR expression may be a favorable prognostic indicator.
Conclusion
Androgens may have both oncogenic and tumor suppressive roles. Androgen-specific biases in metabolism and the expression of AR may contribute to the different prognosis of patients with EC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endometrial carcinoma (EC) is the most commonly diagnosed gynecological cancer in women and ranked second in gynecological cancer-related deaths [1]. Risks for EC are associated with an excess-estrogen environment. And the role of unopposed estrogen in EC has been well described. To our best knowledge, one of the estrogen productions is aromatization of androstenedione to estrone within the ovaries and extragonadal tissues. Of note, the main source of estrogen production in women after menopause is from peripheral aromatization in adipose tissues [2]. All of these suggest the potential of androgens in the carcinogenesis of EC. In this review, we particularly focus on observational and mechanistic studies assessing the effects of androgens in women with EC. And the mechanistic studies mainly include the metabolism and androgen receptor that are most studied. We summarize some of the recent insights into androgen-regulated pathways that may pave the ways for untreatable cancers such as EC, at present.
Androgens and the risk of EC
Endometrial growth is mediated by circulating sex hormones including androgens. There are several kinds of hormones that can exert androgenic effects, including dehydroepiandrosterone-sulfate (DHEAS), DHEA, androstenedione, testosterone and dihydrotestosterone (DHT) in the order of high to low level. Among them, DHT exerts the most potency of androgen, while androstenedione and DHEA exhibit only 10 and 5% of the potency of testosterone [3].
Some studies have examined the potential role of circulating androgens as risk factors for EC. In general, elevated serum testosterone level has been associated with an increased EC risk in postmenopausal women (Table 1). However, the association between increased testosterone levels and EC risk has not been observed among premenopausal women. Interesting, the association of androgens with EC risk is weaker when the levels of serum estrogens are taken into account [4, 5], suggesting that the conversion of testosterone into estrogen may contribute to the association between androgen and EC risk. An excess-estrogen environment is specially associated with type I EC, but few significant difference was revealed when type I cancer patients compared with type II cancer patients [6].
The increased EC risks with androstenedione (A4) were also found in most studies after menopause (Table 1). After adjustment for estrogen, the positive association was attenuated but the directions of the effect were unchanged [5, 7]. These results indicate that androgens affect endometrium carcinogenesis through not only conversion into estrogen but also androgenic pathways.
To date, very few studies focused on the dihydrotestosterone (DHT), more potent than testosterone, in the role of EC risk. DHT is metabolized by 5α-reductase pathway and the reaction is not reversible (Fig. 1). Existing studies have not definitively indicated an increased EC risk associated with DHT levels. However, it is worth to note that a reduced risk for EC was associated with increasing DHT levels especially after adjustment for estrogen [5].
Selected aspects of androgen metabolism in endometrial cancer. The five androgen hormones are in red. DHEAS dehydroepiandrosterone-sulfate, DHEA dehydroepiandrosterone, STS steroid sulfatase, A4 Androstenedione, T Testosterone, DHT Dihydrotestosterone, 17βHSD2 17β-hydroxysteroid dehydrogenase type 2, 17βHSD5 17β-hydroxysteroid dehydrogenase type 5, 5α-Red 5α-reductases
The link between endometrial safety and androgen treatment has been investigated in postmenopausal women treated with androgens for diminished sexual wellbeing. Recent data form a meta-analysis showed that androgen treatment did not increase endometrial thickness in postmenopausal women [8]. However, the included studies in this meta-analysis had a relatively short follow-up period (˂ 2 years), which may not be sufficient to observe serious adverse endometrial effects. The effect of exogenous testosterone treatments on endometrium tissues has also been studied in transsexuals. No morphological changes associated with EC risk have been observed in hysterectomy tissues [9]. Given that gender reassignment surgery-hysterectomy usually occurs relatively soon (˂ 3 years), the morphological changes could not be observed, limiting the utility of the data. In female-to-male (F-to-M) breast tissues, it has been observed that expression of breast cancer-related genes overlaps with these in F-to-M breast tissues [10]. It is tempting to investigate whether or not changes in cancer-related gene expression have existed.
Androgens metabolism and EC
Once inside the cells, androgens and their precursors can be further metabolized and converted into bioavailable androgen in specific tissues containing the appropriate enzymes [2, 11]. In target tissues, the most of active androgens are produced locally from circulating adrenal and/or ovarian precursors [12, 13]. Differences in intracrine pathway are now accepted as a key way in which target tissues such as endometrium can respond to physiological demands. This may have the potential to confound the interpretation of studies investigating the association between androgen and EC. Therefore, it is important to elucidate the metabolic pathways that modulate intracellular levels of androgen in the endometrium. The expression of metabolic enzymes that have been implicated in EC are described in Table 2.
Steroid sulfatase
One of the primary roles of steroid sulfatase (STS) is to hydrolyze DHEAS to DHEA. Also, STS acts on substrates like estradiol-S and estrone-S. STS mRNA and protein levels were detected both in cancer tissues and normal endometrium, but no significant difference was found [14, 15]. A larger cohort consisting of 175 tumor samples suggests that high STS levels are more associated with endometrioid histology which predicts a better prognosis but also with high grade (G2 and G3) which means poor prognosis [16]. Interesting, the clinical outcomes were also influenced by the STS/estrogen sulfotransferase expression ratio. Increasing this ratio predicted a poor outcome [17]. In EC tissues, the presence of STS may be more involved in estrogen supplement [14, 15]. Whether or not STS expression alters androgen levels in EC is still not known.
3β-Hydroxysteroid dehydrogenase
3β-Hydroxysteroid dehydrogenase (3βHSD) enzymes catalyze the conversion of DHEA to A4 and androstenediol to testosterone. Little is known about it in the role of EC, with only one study suggesting no significant changes in EC compared with normal tissues [18]. Correlations between 3βHSD expression and clinic-pathological markers have not been observed. And the correlation between 3βHSD and androgens is still unknown.
17β-Hydroxysteroid dehydrogenase type 1
The most potent estrogen estradiol (E2) is produced via 17β-hydroxysteroid dehydrogenase type 1 (17βHSD1). To date, the role of 17βHSD1 in EC has been investigated more in relation to the production of estrogen rather than androgen. An increase in the levels of 17βHSD1 has been shown to be associated with increased levels of E2 in EC [19, 20]. Estrogen is a well-established risk factor for EC, since it could drive EC progression [21, 22]. A decrease in levels of 17βHSD1 has been shown to be associated with better prognosis [16]. However, similar to STS, the function of 17βHSD1 may more contribute to the regulation of estrogen action in this disease. Whether or not expression of 17βHSD1 in EC influences androgen actions is needed to study further.
17β-Hydroxysteroid dehydrogenase type 2
17β-Hydroxysteroid dehydrogenase type 2 (17βHSD2) is responsible for generating A4 from testosterone and the reversible conversion between estrone and estradiol. Studies assessing the clinical significance of 17βHSD2 in EC have suggested conflicting findings. A relatively well-designed cohort study identified that 17βHSD2 was significantly higher in tumors compared with normal tissues, especially in endometrioid type II cancers [23]. Furthermore, survival analyses confirmed that patients with high level of 17βHSD2 had a better prognosis than the remaining women [16, 24]. In EC, interactions between androgens and 17βHSD2 have been suggested. A study on HEC-1B cells treated with DHT, which were inhibited growth, indicated that anti-proliferative effects of DHT were mediated through an increase in 17βHSD2 levels [24]. This is consistent with the finding from an observational study that increasing DHT level reduced risk for EC occurrence [5]. These lines of evidence suggest that the tumor-suppressive role of androgens may be partly attributed to the expression of 17βHSD2. However, this hypothesis is yet to test in a clinical setting.
17β-Hydroxysteroid dehydrogenase type 5
In contrast to the role of 17βHSD2, 17β-hydroxysteroid dehydrogenase type 5 (17βHSD5) is involved in the conversion of A4 into T.
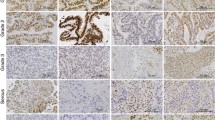
To date, 17βHSD5 expression in cancer tissues as opposed to normal endometrium is still uncertain. The largest published study identified a decreased 17βHSD5 level measured by immunohistochemistry (IHC) in 123 EC specimens compared with adjacent normal endometrium. Further survival analysis revealed that increased expression of 17βHSD5 in endometrioid endometrial cancer was associated with better cumulative and disease-specific survival [25]. 17βHSD5 can convert A4 to T. Therefore, the lower 17βHSD5 expression in EC may contribute to T loss in the diseased endometrium. One study examined the intratumoral T concentration of EC, but did not find significant difference between the intratumoral concentration of T in EC and the normal endometrium [26]. The small numbers of patients included make definitive conclusions difficult. Therefore, there is clearly a need for well-designed, larger numbers included studies to uncover the role of 17βHSD5-mediated androgens conversion.
5α-Reductases
5α-Reductases (5α-Reds), which have three different isoforms-5α-Red1, 5α-Red2, and 5α-Red3, catalyze the conversion of testosterone to DHT. In EC, 5α-Red1 is the most widely investigated among them. 5α-Red1 was considered the main isoform in EC tissues and expressed more frequently than 5α-Red2. And the levels of 5α-Red1 expression were upregulated compared with matched tissues [27,28,29]. However, the increased DHT concentration within cancerous tissues was not observed. It is noteworthy that 5α-Red1 was an independent prognostic factor in EC, where its expression was significantly associated with lower tumor grade and progression-free survival (PFS) in positive group was longer than that in negative group. Additionally, 5α-Red1 rather than 5α-Red2 was positively associated with intertumoral DHT, suggesting its higher affinity for testosterone than 5α-Red2 [26]. Combined with the results from clinical data [5], it is tempting to suggest us that the conversion of testosterone to DHT via 5α-Reds may weaken the oncogenic role of testosterone. Further studies are needed to identify it.
5α-Reds, especially 5α-Red1, are also involved in progesterone metabolism. As we know, progesterone can counteract the effect of estrogens within the endometrium. The suppressive effect of 5α-Red1 may be involved in androgens and/or progesterone actions in endometrium tumorigenesis, indicating the need for a better understanding of it to better define the role of 5α-Red1 in EC.
The importance of 5α-Red2 and 5α-Red3 in EC is known little. Deceased levels of 5α-Red2 and increased 5α-Red3 expression were detected in EC [27, 30], although significant effects of 5α-Red2 and 5α-Red3 on prognosis have not been reported. Further studies are needed to be done to understand the specific role of 5α-Red2 and 5α-Red3 in EC.
Aromatase
The aromatases encoded by CYP19A1 gene catalyze the last steps of estrogen biosynthesis, which stimulates the cell proliferation in EC. This forms the basis for aromatase inhibition as a therapeutic strategy for EC. When aromatase inhibitors (AIs) reduce the peripheral conversion of androgens to estrogen, the levels of androgens increase in peripheral circulation and/or EC tissues. It has been reported that DHT could inhibit the proliferation of EC cells induced by estrogen [31]. Therefore, it is tempting to speculate that the findings of increased EC risk associated with androgen levels are largely the result of conversion to estrogen by aromatase in endometrium. As shown in Table 1, one study has evaluated the connection influenced by estrogen and found that the effect of elevated testosterone on EC risk is ameliorated when the conversion of testosterone to estradiol is taken into account [4]. Further interactions between androgen signaling and aromatase have not been suggested at the molecular level. However, there is no association between mRNA levels of aromatase and serum testosterone [32]. Given the sample size of this study, there is clearly a need for well-designed, larger scale studies to understand the mechanism in it.
The role of androgen receptor in normal endometrium
Evidence that the endometrium is an androgen-target tissue is supported by detection of AR in the tissue [33]. Normal adult endometrium including epithelial and stromal cells detected the expression of AR. And AR expression was more abundant in the stromal cells during the proliferative phase of the menstrual cycle. As for epithelial cells, AR was nearly undetectable in the proliferative phase, while weak in the secretory phase [28, 34]. Interestingly, AR may play both a growth stimulatory and inhibitory role. The primary role of epithelial AR appears to induce epithelial cell apoptosis. Stromal AR may function as stimulator of endometrial cells proliferation [35].
AR knockout (ARKO) mice are important for the study of AR in EC. In these animals, normal but smaller uteri and reduced uterine growth at oestrous or in response to exogenous gonadotrophins are found. Besides, AR appears to involve in the development of pups and placental. The number of pups per litter is significantly decreased before ovarian failure exists in ARKO mice. Placentomegaly and abnormal placental development are more frequent during pregnancy in these animals [36].
The role of AR in EC
Traditionally, EC has been categorized as type I or type II based on histology. In type II EC, high-level AR expression was restricted to serous cancer in concert with ER and PR expression. Although this study did not provided data on the association between AR and EC outcomes, the patients with AR-positive malignancies were older than those with AR-negative tumors [37]. AR staining was not detected within uterine carcinosarcoma, endometrial stromal sarcoma, or clear cell cancers [38, 39]. Of rare histologic types like undifferentiated/dedifferentiated carcinomas, the presence of AR has been reported. Loss of AR indicates the possibility of more advanced disease [40].
Type I endometrioid adenocarcinomas comprise most cases. Most of the related studies focused on the relationship among AR levels in the primary tumor, clinical characteristics, and disease outcome. AR is widely expressed in EC and its expression in metastatic is significantly higher than that in primary tumors [41]. Most of the studies accessing the prognostic value of AR have found that AR expression may be a favorable prognostic indicator. AR expression correlated with lower histological grade, absence of lymphovascular invasion, a lower proliferation index (Ki67), increased disease-free survival, and overall survival [26, 41,42,43]. There also exist some studies drawing opposing conclusions [37, 39]. The difference among studies may be explained by the following factors, including ⑴ differences in sample size, length of follow-up and prior treatment regimens; ⑵ use of different antibodies and detection techniques; ⑶ use of different cut-off scores to define AR positivity. Existing shortcomings in these studies limit their use in accessing the prognostic value of AR.
In mouse models of type I EC, short-term enzalutamide treatment, an inhibitor of AR signaling, reduced endometrial tumor burden and increased cancer cell apoptosis in a dose-dependent way. However, enzalutamide increased the incidence of invasive and metastatic tumor [44]. This study suggested that AR signaling may have both oncogenic and tumor-suppressive roles. Oncogenic role of AR may be more involved in EC initiation. Later stages of invasion and metastasis in EC may be partly due to inactivation of cancer suppressive AR signaling.
What makes the relationship between androgens and EC difficult to assess?
In the circulation, testosterone is highly protein-bound, with a small fraction dissolved freely. The rest of testosterone is bound to sex hormone-binding globulin (SHBG) and albumin. The SHBG-bound fraction is biologically inactive because of the high binding affinity of SHBG for testosterone [45]. Total or free testosterone seems not to be perfectly indicative of the bioactive testosterone concentrations. Some studies have suggested an inverse association of SHBG levels with EC [4, 46]. If subtracting SHBG-bound fraction from total testosterone level, the association between remaining androgens and EC risk is not clear. It has been observed a protective effect of bioavailable testosterone (the component of testosterone calculated to be unbound to SHBG) in estrogen receptor-negative breast cancer among postmenopausal women [47].
Another obvious influential issue is that hyperandrogenism is often combined with several components such as insulin resistance (IR) and visceral adiposity [48,49,50], which contribute to the development of EC. The metabolic syndrome is characterized by a constellation of symptoms and clinical features, including glucose intolerance, IR, central obesity, dyslipidemia, and hypertension [51]. The association between metabolic syndrome and EC has been observed (reviewed by Yang) [52]. It is difficult to assess which is more important in increasing the likelihood of endometrial carcinogenesis, whether androgen itself or androgen-associated comorbidities. For example, it is noted that testosterone was associated with increased EC risk for women with BMI over 24 kg/m2 [48]. After adjustment for BMI and other confounding factors, a decrease in the effect of testosterone was observed [4].
Androgens exert their effects on many cellular targets, including cells of the inflammatory and immune system. A comprehensive review showed that inflammatory cytokines were associated with an increased risk of EC. And they could activate the PI3K/Akt/mTOR signaling pathway that is the most frequently altered pathway in EC [53]. It has been demonstrated that androgens could blunt CD4 + T-cell (Th1)-driven inflammatory response in the vagina while promoting Th2/M2 [54]. Th2/M2 could also be observed at precancerous stage of cervical cancer development [55].
Concluding remarks
Unfortunately, we are unable to conclude that androgens are the killer or helper in EC. This condition is complex. There are different kinds of androgenic hormones, and different kinds of androgens may have different effects. Elevated androgens (especially testosterone) in EC patients mean that they maybe the potential inciting factor of EC. However, androgen-specific biases in metabolism and the expression of AR may contribute to the different prognosis of patients with EC. For example, 5α-Reds and 17βHSD2 pathway may inhibit the progression of EC mediated by DHT, but aromatases stimulate further progression of EC. However, the downstream signaling pathways have remained unknown. Further experimental studies are clearly required to uncover the impact of related enzymes and AR on carcinogenesis in endometrium.
References
Siegel RL, Miller KD, Fuchs HE et al (2021) Cancer statistics. Cancer J Clin 71(1):7–33
Simpson E, Rubin G, Clyne C et al (2000) The role of local estrogen biosynthesis in males and females. Trends Endocrinol Metab 11(5):184–188
Gubbels Bupp MR, Jorgensen TN (2018) Androgen-induced immunosuppression. Front Immunol 9:794
Lukanova A, Lundin E, Micheli A et al (2004) Circulating levels of sex steroid hormones and risk of endometrial cancer in postmenopausal women. Int J Cancer 108(3):425–432
Michels KA, Brinton LA, Wentzensen N et al (2019) Postmenopausal androgen metabolism and endometrial cancer risk in the women’s health initiative observational study. JNCI cancer spectrum. 3(3):pkz029
Audet-Walsh E, Lépine J, Grégoire J et al (2011) Profiling of endogenous estrogens, their precursors, and metabolites in endometrial cancer patients: association with risk and relationship to clinical characteristics. J Clin Endocrinol Metab 96(2):E330–E339
Annekatrin L, Eva L, Andrea M et al (2004) Circulating levels of sex steroid hormones and risk of endometrial cancer in postmenopausal women. Int J Cancer 108(3):425
Islam RM, Bell RJ, Green S et al (2019) Safety and efficacy of testosterone for women: a systematic review and meta-analysis of randomised controlled trial data. Lancet Diabetes Endocrinol 7(10):754–766
Grimstad FW, Fowler KG, New EP et al (2018) Uterine pathology in transmasculine persons on testosterone: a retrospective multicenter case series. Am J Obstet Gynecol 220(3):257
Bentz EK, Pils D, Bilban M et al (2010) Gene expression signatures of breast tissue before and after cross-sex hormone therapy in female-to-male transsexuals. Fertil Steril 94(7):2688–2696
Giorgi EP, Stein WD (1981) The transport of steroids into animal cells in culture. Endocrinology 108(2):688–697
Schiffer L, Arlt W, Storbeck KH (2018) Intracrine androgen biosynthesis, metabolism and action revisited. Mol Cell Endocrinol 15(465):4–26
Cellai I, Di Stasi V, Comeglio P et al (2021) Insight on the intracrinology of menopause: androgen production within the human vagina. Endocrinology. https://doi.org/10.1210/endocr/bqaa219
Maša S, Tamara K, Maja A et al (2017) The significance of the sulfatase pathway for local estrogen formation in endometrial cancer. Front Pharmacol. https://doi.org/10.3389/fphar.2017.00368
Cornel KMC, Delvoux B, Saya T et al (2018) The sulfatase pathway as estrogen supply in endometrial cancer. Steroids 139:45–52
Cornel KM, Krakstad C, Delvoux B et al (2017) High mRNA levels of 17β-hydroxysteroid dehydrogenase type 1 correlate with poor prognosis in endometrial cancer. Mol Cell Endocrinol 15(442):51–57
Utsunomiya H, Ito K, Suzuki T et al (2004) Steroid sulfatase and estrogen sulfotransferase in human endometrial carcinoma. Clin Cancer Res 10(17):5850–5856
Sinreih M, Hevir N, Rižner TL (2013) Altered expression of genes involved in progesterone biosynthesis, metabolism and action in endometrial cancer. Chem-Biol Interact 202(1–3):210
Cornel KM, Kruitwagen RF, Delvoux B et al (2012) Overexpression of 17beta-hydroxysteroid dehydrogenase type 1 increases the exposure of endometrial cancer to 17beta-estradiol. J Clin Endocrinol Metab 97(4):E591-601
Konings GF, Cornel KM, Xanthoulea S et al (2018) Blocking 17beta-hydroxysteroid dehydrogenase type 1 in endometrial cancer: a potential novel endocrine therapeutic approach. J Pathol 244(2):203–214
Zhu Y, Shen J, Gao L et al (2016) Estrogen promotes fat mass and obesity-associated protein nuclear localization and enhances endometrial cancer cell proliferation via the mTOR signaling pathway. Oncol Rep 35(4):2391–2397
Zhang Z, Zhou D, Lai Y et al (2012) Estrogen induces endometrial cancer cell proliferation and invasion by regulating the fat mass and obesity-associated gene via PI3K/AKT and MAPK signaling pathways. Cancer Lett 319(1):89–97
Lépine J, Audet-Walsh E, Grégoire J et al (2010) Circulating estrogens in endometrial cancer cases and their relationship with tissular expression of key estrogen biosynthesis and metabolic pathways. J Clin Endocrinol Metab 95(6):2689–2698
Chiaki H, Yasuhiro M, Sota T et al (2018) 17β-Hydroxysteroid dehydrogenase type 2 expression is induced by androgen signaling in endometrial cancer. Int J Mol Sci 19(4):1139
Hojnik M, Kenda Šuster N, Smrkolj Š et al (2020) AKR1C3 is associated with better survival of patients with endometrial carcinomas. J Clini Med 9(12):4105
Tanaka S, Miki Y, Hashimoto C et al (2015) The role of 5α-reductase type 1 associated with intratumoral dihydrotestosterone concentrations in human endometrial carcinoma. Mol Cell Endocrinol 5(401):56–64
Sinreih M, Hevir N, Rižner TL (2013) Altered expression of genes involved in progesterone biosynthesis, metabolism and action in endometrial cancer. Chem Biol Interact 202(1–3):210–217
Ito K, Suzuki T, Akahira J et al (2002) Expression of androgen receptor and 5alpha-reductases in the human normal endometrium and its disorders. Int J Cancer 99(5):652–657
Wasniewski T, Woclawek-Potocka I (2018) Altered expression of lysophosphatidic acid receptors, in association with the synthesis of estrogens and androgens in type 1 endometrial cancer biology. Gynecol Endocrinol 34(5):422–427
Wang ZH, Zhang YZ, Wang YS et al (2019) Identification of novel cell glycolysis related gene signature predicting survival in patients with endometrial cancer. Cancer Cell Int 19:296
Hashimoto C, Miki Y, Tanaka S et al (2018) 17beta-Hydroxysteroid dehydrogenase type 2 expression is induced by androgen signaling in endometrial cancer. Int J Mol Sci 19(4):1139
Kazmierczak W, Skalba P, Dabkowska-Huc A et al (2006) Expression of aromatase and 5-alpha-reductase genes in endometrial adenocarcinoma. Pathol Res Pract 202(11):789–791
Simitsidellis I, Saunders PTK, Gibson DA (2018) Androgens and endometrium: new insights and new targets. Mol Cell Endocrinol 15(465):48–60
Younas K, Quintela M, Thomas S et al (2019) Delayed endometrial decidualisation in polycystic ovary syndrome; the role of AR-MAGEA11. J Mol Med 97(9):1315–1327
Wang T, Zhang J, Hu M et al (2019) Differential expression patterns of glycolytic enzymes and mitochondria-dependent apoptosis in PCOS patients with endometrial hyperplasia, an early hallmark of endometrial cancer, in vivo and the impact of metformin in vitro. Int J Biol Sci 15(3):714–725
Cloke B, Christian M (2012) The role of androgens and the androgen receptor in cycling endometrium. Mol Cell Endocrinol 358(2):166–175
Zadeh SL, Duska LR, Mills AM (2018) Androgen receptor expression in endometrial carcinoma. Int J Gynecol Pathol 37(2):167–173
Koivisto-Korander R, Butzow R, Koivisto AM et al (2011) Immunohistochemical studies on uterine carcinosarcoma, leiomyosarcoma, and endometrial stromal sarcoma: expression and prognostic importance of ten different markers. Tumour Biol 32(3):451–459
Hashmi AA, Hussain ZF, Qadri A et al (2018) Androgen receptor expression in endometrial carcinoma and its correlation with clinicopathologic features. BMC Res Notes 11(1):289
Cao J, Hacking S, Chavarria-Bernal HD et al (2021) Androgen receptor immunohistochemical expression in undifferentiated/dedifferentiated endometrial carcinoma. Int J Gynecol Pathol 41(1):28–34 (Publish Ahead of Print)
Kamal AM, Bulmer JN, DeCruze SB et al (2016) Androgen receptors are acquired by healthy postmenopausal endometrial epithelium and their subsequent loss in endometrial cancer is associated with poor survival. Br J Cancer 114(6):688–696
Tangen IL, Onyango TB, Kopperud R et al (2016) Androgen receptor as potential therapeutic target in metastatic endometrial cancer. Oncotarget 7(31):49289–49298
Mahdi Z, Abdulfatah E, Pardeshi V et al (2017) The impact of androgen receptor expression on endometrial carcinoma recurrence and survival. Int J Gynecol Pathol 36(5):405–411
Koivisto CS, Parrish M, Bonala SB et al (2020) Evaluating the efficacy of enzalutamide and the development of resistance in a preclinical mouse model of type-I endometrial carcinoma. Neoplasia 22(10):484–496
Vermeulen A, Verdonck L, Kaufman JM (1999) A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab 84(10):3666–3672
Mullee A, Dimou N, Allen N et al (2021) Testosterone, sex hormone-binding globulin, insulin-like growth factor-1 and endometrial cancer risk: observational and Mendelian randomization analyses. Br J Cancer 125(9):1308–1317
Farhat GN, Cummings SR, Chlebowski RT et al (2011) Sex hormone levels and risks of estrogen receptor-negative and estrogen receptor-positive breast cancers. J Natl Cancer Inst 103(7):562–570
Teng F, Ma X, Yu X et al (2020) High serum androgen and insulin concentrations increase the tendency of endometrial carcinoma. J Cancer 11(19):5656–5664
Franks S, Berga SL (2012) Does PCOS have developmental origins? Fertil Steril 97(1):2–6
de Zegher F, Lopez-Bermejo A, Ibáñez L (2009) Adipose tissue expandability and the early origins of PCOS. Trends Endocrinol Metab 20(9):418–423
Eckel RH, Grundy SM, Zimmet PZ (2005) The metabolic syndrome. Lancet 365(9468):1415–1428
Yang X, Wang J (2019) The role of metabolic syndrome in endometrial cancer: a review. Front Oncol 9:744
Borghi C, Indraccolo U, Scutiero G et al (2018) Biomolecular basis related to inflammation in the pathogenesis of endometrial cancer. Eur Rev Med Pharmacol Sci 22(19):6294–6299
Maseroli E, Cellai I, Filippi S et al (2020) Anti-inflammatory effects of androgens in the human vagina. J Mol Endocrinol 65(3):109–124
Wang Y, He M, Zhang G et al (2021) The immune landscape during the tumorigenesis of cervical cancer. Cancer Med 10(7):2380–2395
Allen NE, Key TJ, Dossus L et al (2008) Endogenous sex hormones and endometrial cancer risk in women in the European Prospective Investigation into Cancer and Nutrition (EPIC). Endocr Relat Cancer 15(2):485–497
Clendenen TV, Hertzmark K, Koenig KL et al (2016) Premenopausal circulating androgens and risk of endometrial cancer: results of a prospective study. Hormones Cancer 7(3):178–187
Cornel KMC, Krakstad C, Delvoux B et al (2017) High mRNA levels of 17β-hydroxysteroid dehydrogenase type 1 correlate with poor prognosis in endometrial cancer. Mol Cell Endocrinol 442:51
Vladislav Z, Hsueh-Kung L, Joseph A et al (2010) Suppressed expression of type 2 3alpha/type 5 17beta-hydroxysteroid dehydrogenase (AKR1C3) in endometrial hyperplasia and carcinoma. Int J Clin Exp Pathol 3(6):608
Hevir-Kene N, Rižner TL (2015) The endometrial cancer cell lines Ishikawa and HEC-1A, and the control cell line HIEEC, differ in expression of estrogen biosynthetic and metabolic genes, and in androstenedione and estrone-sulfate metabolism. Chem Biol Interact 5(234):309–319
Sinreih M, Anko M, Zukunft S et al (2015) Important roles of the AKR1C2 and SRD5A1 enzymes in progesterone metabolism in endometrial cancer model cell lines. Chem Biol Interact 5(234):297–308
Acknowledgements
This study was funded by the National Natural Science Foundation of China (no. 81572568), the Tianjin Municipal Science and Technology Bureau, China [Grant Number: 20JCZDJC00330] and the grant (No. QB2021002) from the Youth Research grant of Nantong Commission of Health. We are thankful to the Key Laboratory of Female Reproductive Health and Eugenics of Tianjin Medical University General Hospital for the support of writing this review.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, X., Zhang, K., Zhong, X. et al. Androgens in endometrial carcinoma: the killer or helper?. J Endocrinol Invest 46, 457–464 (2023). https://doi.org/10.1007/s40618-022-01916-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01916-1