Abstract
Purpose
Coronavirus disease (COVID-19) lockdowns have impacted on management of osteoporosis and the use of telemedicine is increasingly widespread albeit supported by little evidence so far. The aim of the study is to assess adherence to denosumab and incidence of non-traumatic fractures during the lockdown compared to the pre-COVID-19 year and to explore the effectiveness of telemedicine in the management of osteoporotic patients.
Methods
Retrospective, longitudinal, single-center study on patients receiving subcutaneous denosumab therapy every 6 months. Each patient was scheduled to undergo 2 visits: one during the pre-COVID-19 period (March 2019–March 2020) and another visit during the lockdown period (March 2020–March 2021). Data on new fractures, adherence, risk factors for osteoporosis and the modality of visit (telemedicine or face-to-face) were collected.
Results
The prevalence of non-adherent patients was higher during the lockdown (35 of 269 patients, 13.0%) than the pre-COVID-19 period (9 of 276 patients, 3.3%) (p < 0.0001). During the lockdown, the number of new non-traumatic fractures was higher than the pre-COVID-19 year (p < 0.0001): 10 patients out of 269 (3.7%) experienced a fragility fracture and 2 patients (0.7%) a probable rebound fracture during the lockdown period, whereas no patient had fragility/rebound fractures during the pre-COVID-19 period. No difference was found in the prevalence of non-adherence and new non-traumatic fractures comparing patients evaluated with tele-medicine to those evaluated with face-to-face visit.
Conclusion
Non-adherent patients and new non-traumatic fractures (including rebound fractures) were more prevalent during the lockdown in comparison to the pre-COVID-19 period, regardless of the modality of medical evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Denosumab is a fully human monoclonal antibody approved for the treatment of osteoporosis both in women and men [1, 2]. This anti-bone resorption agent is administered as a single 60 mg subcutaneous injection every 6 months [1].
In contrast to bisphosphonates, denosumab discontinuation leads to a complete and rapid reversal of its effects in terms of bone turnover markers levels and bone mineral density (BMD), so-called rebound effect [3, 4], raising concerns among clinicians about the off-treatment fracture risk. Six months after the last injection of denosumab, indeed, bone turnover markers increase above baseline within 3 months, reach a peak at 6 months, and return to baseline values at 24 months [5, 6]. Similarly, BMD gains at all skeletal sites are lost with a return to pre-treatment baseline values after 1–2 years off-treatment [5, 6]. As a consequence, denosumab withdrawal is associated with a 3- to fivefold higher risk for vertebral, major osteoporotic, and hip fractures [7,8,9]. The risk of rebound fractures is reported as early as 4–8 weeks after interruption in injection schedule, and therefore, it is recommended that injections of denosumab should not be delayed by more than 7 months after the previous dose [1, 10].
Coronavirus disease 19 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was characterized as a pandemic by the World Health Organization (WHO) on March 11, 2020 [11]. In response to COVID-19 pandemic, many countries have implemented a series of unprecedented measures to mitigate the spread of the virus, including national lockdowns [12]. In Italy, starting from the first national lockdown, from March to May 2020, out-patient visits have been abruptly stopped and the access to hospitals has been restricted only to emergencies. Inevitably, these restrictions have impacted management of chronic diseases such as osteoporosis.
For this reason, in the perspective of guaranteeing adherence to anti-osteoporotic treatments and trying to prevent the harmful rebound phenomenon after denosumab discontinuation, the use of tele-medicine tools (e.g., by telephone or e-mail) has been highly recommended by experts for the management of patients with osteoporosis during COVID-19 pandemic [13,14,15,16]. However, these recommendations are based primarily on expert opinions since there is little evidence about the effectiveness of tele-medicine in the management of chronic diseases so far. Indeed, only in the last months, a few studies have been published aiming at exploring the efficacy of tele-medicine, mainly in terms of adherence to treatment and clinical outcomes, in comparison to traditional face-to-face visits.
To date, data on the impact of COVID-19 pandemic on the management of osteoporotic patients are scanty. With this in mind, the aim of this study was to assess adherence rate to denosumab during the lockdown year in comparison to the pre-COVID-19 year. The second aim was to explore the occurrence of fragility fractures during the lockdown period, with particular attention to the rebound fractures among patients who interrupted denosumab. Finally, we aimed to investigate which role tele-medicine has played in helping patients to adhere denosumab treatment.
Materials and methods
Study design
A single-center, retrospective, longitudinal study was carried out.
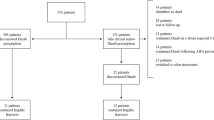
Outpatients referring to our Unit of Endocrinology, University of Modena and Reggio Emilia, Azienda Ospedaliero-Universitaria (AOU) of Modena, in the period between March 2019 and March 2021, who were receiving treatment with denosumab for osteoporosis, were enrolled (Fig. 1). Each patient was scheduled to undergo two visits: one visit during the pre-COVID-19 period (8 March 2019–8 March 2020) and another visit during the lockdown period (8 March 2020–8 March 2021) for clinical re-evaluation and renewal of the prescription for denosumab (Fig. 1). We considered the date of March 8, 2020 as watershed since it established the beginning of the first lockdown in Italy. Visits scheduled during the lockdown period could be carried out in two different modalities: tele-medicine or standard face-to-face visits (see below).
Distribution of enrolled patients in relation to the year of initiation of denosumab. Each patient underwent two visits in the period of study: the first in the year before COVID-19 pandemic (yellow area) and the second one during the COVID-19 lockdown (blue area). Dotted boxes represent years of ongoing denosumab
Data about the adherence rate to denosumab and the occurrence of non-traumatic fractures collected at both visits were compared between the pre-COVID-19 and the lockdown period.
Participants
Osteoporotic patients receiving denosumab treatment initiated before March 2020, in agreement with AIFA note 79, were retrospectively recruited (Fig. 1).
Inclusion criteria were age > 18 years, and ongoing treatment with denosumab with date of initiation before March 8, 2020. For enrolled patients, we collected from the patients’ record charts the following parameters that are routinely explored in the real-life practice at out-patient clinics for osteoporosis: age, gender, weight, height, medication use, prior history of any fracture, osteoporosis-related risk factors, date of start and of last injection of denosumab, and date of renewal of its therapeutic plan.
No exclusion criterion was provided.
Main outcomes measures
Adherence to denosumab
In Italy, denosumab prescription is regulated by Italian Drug Agency (AIFA) note 79 [17] by means of a therapeutic plan, which must be issued by an endocrinologist or another bone specialist. This prescription allows patients to obtain every 6 months one pre-filled pen of the drug. In Emilia Romagna, denosumab is dispensed by hospital pharmacies and drug injection is administered at home by the patient him/herself or by his/her caregiver.
Adherence to denosumab was defined as receiving the scheduled denosumab injection on time, i.e., at 6 months (with an allowable delay of another 4 weeks) after the date of the previous injection. During the visit, each enrolled patient was asked whether the scheduled dose of denosumab was regularly administered, delayed of at least 4 weeks, or almost discontinued. We decided to give only a 4-week allowance (grace period) because most previous adherence studies for osteoporosis treatments (oral or otherwise) have used similar windows of allowable delay [18, 19]. Therefore, international osteoporosis recommendations have also recommended denosumab injection not be delayed beyond 4 weeks from when it is due [1].
New non-traumatic bone fracture during denosumab treatment
The occurrence of new traumatic and non-traumatic fractures was recorded during the pre-COVID-19 period during the lockdown period. Non-traumatic fractures were further classified in fragility, rebound, and atypical fractures. Fragility fractures result from mechanical forces that would not ordinarily result in a fracture, known as low-level (or 'low energy') trauma. WHO has quantified this as forces equivalent to a fall from a standing height or less. Fractures occurred 4–8 weeks after denosumab discontinuation were considered probable rebound fractures, as explained in the introduction. Atypical fractures are rare type of fractures that have been associated with the long-term use of antiresorptive bone medications. They originate in the lateral shaft of the femur and occur with minimal or no trauma [20].
The occurrence of a new fracture, not present at baseline, were collected based on radiological investigations (X-ray, computerized tomography [CT]) performed in agreement with real-life clinical care demands.
Modality of medical evaluation during the COVID-19 lockdown: tele-medicine and face-to-face visits
Endocrine out-patient clinic at AOU of Modena covers all fields of endocrinology, from the first level to the most complex cases requiring dedicated expertise and multi-disciplinary evaluation. Among second-level endocrinology out-patient clinics, there is one dedicated to osteoporosis and disorders of calcium–phosphorus metabolism. During COVID-19 outbreak, the re-organization of the out-patient clinic was necessary and all planned visits could be performed with two modalities: tele-medicine and face-to-face visits. At least 5 days before the scheduled visit appointment, an endocrinologist called the patient by phone to check patient’s health status (signs/symptoms related to COVID-19 infection and to endocrine disease) and to make the decision between tele-medicine and face-to-face visit. After phone-agreement with the patient, tele-medicine was generally proposed in case of: (1) follow-up visits; (2) recognized ability to use e-mail (with the help of family members/caregivers if needed); (3) clinical assessment considered to be not absolutely necessary; (4) fragile and older patients. If the patient agreed to tele-medicine, all the medical reports had to be sent to a dedicated e-mail address. Thus, the endocrinologist completed the visit asking the patient (by mail or phone) detailed information regarding correct assumption of drugs (in this case the date of last injection of denosumab was recorded) and commenting clinical reports sent by e-mail. The visit report form, together with the prescription of the next control, results of examinations and therapeutic plan for denosumab, was finally sent to the patient by ordinary mail.
Risk factors for osteoporosis and history of fractures
Patient self-reports, clinical history, physical examination (e.g., low body mass index [BMI]), and drug-tracing criteria obtained from patients’ record charts were used to identify the presence or absence of conditions inducing bone loss. Risk factors for osteoporosis are age > 65 years, sedentary lifestyle, low BMI, alcohol consumption, smoking habits, family history of fragility fractures, chronic glucocorticoid therapy, low calcium intake [21]. For women, age at menopause < 45 years was considered as a further risk factor. Medical conditions associated to osteoporosis were also explored (e.g., malabsorption, primary hyperparathyroidism, hyperthyroidism, diabetes mellitus, idiopathic hypercalciuria, rheumatoid arthritis), together with the current use of drugs associated to bone loss. Documented prior history of non-traumatic bone fractures was recorded.
Furthermore, we considered if patients received previously and for at least 12 months, bisphosphonates and/or teriparatide and if a supplementation with calcium and/or vitamin D was ongoing.
Statistical analysis
Proportions and rates were calculated for categorical data; continuous data were reported as median and interquartile range (IQR).
The non-parametric Mann–Whitney U test was used for comparisons of continuous variables since they resulted not normally distributed at the Kolmogorov–Smirnov test. Categorical variables were compared by Pearson’s Chi-squared test.
Multinomial logistic regressions were used to determine if factors that may play a role in adherence/fractures (i.e., age, sex, fracture history, BMI, previous use of other anti-osteoporotic agents, comorbidities and risk factors for osteoporosis) were associated with non-adherence to denosumab and to the occurrence of new non-traumatic fractures.
Statistical analyses were performed using the Statistical Package for the Social Sciences’ (SPSS) software for Windows (version 27.0; SPSS Inc, Chicago, IL, USA). For all comparisons, p < 0.05 was considered statistically significant.
Results
Age, sex and clinical characteristics of enrolled patients are summarized in Table 1.
A total of 276 patients initiated on denosumab before March 2020 were enrolled, in agreement with inclusion and exclusion criteria. Seven patients out of 276 were not able to undergo the second visit since 4 of them died during the COVID-19 period, and for 3 patients, denosumab therapies were stopped on medical advice; moreover, we recorded 12 drop-out patients.
A total of 235 patients (85.5%) had a previous history of fragility fractures, thus, suffering from a severe form of osteoporosis (Table 1). The majority of patients had already undergone a previous treatment for osteoporosis before denosumab: 209 patients (75.7%) had been previously treated with bisphosphonates, while 75 (27.2%) had completed the two-year period with Teriparatide (Table 1). At the moment of the enrollment, the median duration of treatment with denosumab was 1.92 year (IQR 0.97–2.94) and the median age at the start of denosumab was 74.7 years (IQR 69.0–81.0) (Table 1).
Adherence to denosumab therapy
Considering an allowed delay of 4 weeks from the scheduled dose of denosumab, we calculated the prevalence of adherent and non-adherent patients before and during the lockdown (Table 2).
In the pre-COVID-19 period, 267 patients out of 276 (96.7%) were adherent and 9 patients (3.3%) were found to be non-adherent (Table 2). In the lockdown period, 234 patients out of 269 (87.0%) were adherent and 35 patients (13.0%) were found to be non-adherent (Table 2; Fig. 2). Hence, the prevalence of non-adherent patients was significantly higher in the lockdown period, compared to the pre-COVID-19 period (p < 0.0001) (Table 2; Fig. 2).
The majority of patients who were non-adherent and/or discontinued denosumab during the COVID-19 lockdown returned for regular follow-up once pandemic restrictions ceased; indeed, we recorded only 12 out of 276 (4.3%) drop-out patients. Investigating the individual reason of non-adherence during the lockdown period, we found that 17 patients out of 269 (6.3%) were afraid of coming to the hospital due to the COVID-19 contagion risk, 5 patients (1.9%) forgot to make the injection of denosumab, and 1 patient (0.4%) interrupted denosumab for intercurrent illness.
Patients undergoing visit in the lockdown period were subdivided into adherent and non-adherent groups, as reported in Table 3. The prevalence of primary hyperparathyroidism and diabetes mellitus was higher among adherent than non-adherent patients (p = 0.038 and p = 0.035, respectively). At the multivariate logistic regression including all available parameters, no factor was found to be predictive of non-adherence to denosumab in the lockdown period.
Prevalence of fractures
During the lockdown period, the prevalence of new non-traumatic fractures was significantly higher compared to the pre-COVID-19 period (p < 0.0001) (Table 2). In particular, 10 patients out of 269 (3.7%) experienced a documented fragility fracture and 2 patients (0.7%) a rebound fracture during the lockdown period, whereas no patient had fragility or rebound fractures during the pre-COVID-19 period (Table 2). The 2 patients with rebound fractures were both female, 85 and 90 years old, respectively, and had history of previous fragility fractures; even the duration of denosumab treatment was similar of about 2 years for both (2.22 and 2.11 years, respectively). Fragility fractures were symptomatic, confirmed by radiological examinations (X-ray or CT), and occurred at vertebral site (lumbar or dorsal) for 6 patients, hip for 2 patients, wrist for 1 patient, and ribs for 1 patient; both rebound fractures were hip fractures. Thereafter, we re-analyzed the occurrence of fractures restricting the analysis to those patients (N = 185) receiving denosumab since at least 12 months. We confirmed that during the lockdown period the prevalence of new non-traumatic fractures was significantly higher compared to the pre-COVID-19 period (p = 0.004). In particular, 6 patients out of 185 (3.2%) experienced a fragility fracture and 2 patients (1.0%) a rebound fracture during the lockdown period, whereas no patient had fragility or rebound fractures during the pre-COVID-19 period. These patients were subdivided into fractured and non-fractured subgroups during the lockdown, as reported in Table 4. Fractured patients were older (p = 0.003) and initiated denosumab at more advanced age (p = 0.005) than non-fractured (Table 4). However, performing multivariate logistic regression including all available parameters only diabetes mellitus predicted fracture during the lockdown, though with a wide confidence interval (p = 0.044, OR 17.94, CI 95%, 1.08–296.7).
Tele-medicine vs face-to-face visits
The prevalence of non-adherent patients during the lockdown period did not differ between patients evaluated by tele-medicine compared to those who underwent face-to-face visit (Tables 3, 4). Similarly, no difference was found in the prevalence of new non-traumatic fractures comparing patients evaluated with tele-medicine to patients evaluated with face-to-face visit (Tables 3, 4).
Discussion
This study is among the first studies providing data on the out-patients clinic re-organization during a pandemic outbreak. Our findings suggest that tele-medicine is as effective as standard face-to-face visits in continuing the follow-up for patients with chronic endocrine disorders assuming long-term treatment, such as osteoporotic patients with ongoing denosumab treatment. Furthermore, this study provides real-world quantifiable information on the adherence rates to denosumab and on the occurrence of fragility fractures during the critical period of the lockdown that was part of the containment efforts for COVID-19 worldwide.
This single-center study reveals that tele-medicine might be considered an alternative strategy in the management of osteoporotic patients, not negatively impacting the compliance to a parenteral anti-osteoporotic drug such as denosumab. Indeed, in our cohort the prevalence of non-adherent patients increased during the COVID-19 pandemic regardless of the modality of medical evaluation (tele-medicine or face-to-face visit). As suggested by another study [22], the use of tele-medicine (e.g., virtual clinics, video-consultations) for chronic endocrine patients might be potentiated in future to reduce visitors in the busy hospital, and to preserve hospital capacity for acutely ill patients. These platforms can also be potentially helpful to emphasize adherence to medications and can be used to remind patients about timely administration especially of parenteral medications. Obviously, more studies are needed to prove the effectiveness of tele-medicine in the long-term period.
In our real-life series, adherence rates to denosumab decreased significantly during the lockdown year in comparison to the pre-COVID-19 year. These findings corroborate what reported by the only one previous study quantifying adherence to denosumab during the COVID-19 lockdown in Singapore, through an electronic medical record and a pharmacy claims database [23]. In the literatures, conflicting results have been reported about the association between adherence to denosumab therapy and demographic factors (gender, age) [18, 23,24,25,26] or medical history (previous fractures, previous anti-osteoporotic treatment) [18, 23, 27, 28]. In our study, we did not observe any significant association between adherence rate and any of these factors.
The majority of patients who were non-adherent and/or discontinued denosumab during the COVID-19 lockdown returned for regular follow-up once pandemic restrictions ceased; indeed, we recorded only 12 drop-out patients. This gave us the possibility to explore the exact individual reasons of their non-adherence during the lockdown, revealing that concerns of acquiring the infection by attending hospitals, to renew the therapeutic prescription and to get denosumab from hospital pharmacy, were the most frequent cause of interruption. A few patients discontinued denosumab for negligence and only one patient for intercurrent illness, including SARS-CoV-2 infection, that required hospitalization.
Our data also showed a significant increase in the number of non-traumatic (fragility and rebound) fractures during the COVID-19 lockdown period compared to the pre-COVID-19 period. In agreement, the rise in fragility [29, 30] and rebound [31] fractures during the pandemic has been shown by few recent studies. Notably, only patients with symptomatic fractures came to our attention. It is highly possible that the impact on fracture incidence due the pandemic is even underestimated than what we observed [31]. The general increase of fracture events may be explained, at least in part, by the higher prevalence of non-adherent patients during the pandemic, even though we did not find a significant association, probably due to the small numbers of fractures. Indeed, it is known that non-persistence and non-compliance with osteoporotic medications is associated with lower effectiveness in terms of fracture risk [32] and BMD [19], and it is also well-known that denosumab withdrawal is associated with a 3- to 5-fold higher risk for rebound fractures [7,8,9]. Though conflicting data exist about the maximum allowable delay of denosumab injection before fracture risk increases, the general recommendation is that injections should not be delayed by more than 7 months after the previous injection [33].
On the one hand, the increase of fractures may theoretically collide with the lockdown restrictions and stay-at-home policies. On the other hand, we can speculate that precisely due to the social isolation policy, support obtained from caregivers to prevent falls and to administer pharmacological therapies may have been reduced for older patients; this could have inadvertently been a cause of the increased hip fractures occurring at home. At the same time, lower sun exposure and physical activity may have contributed to the rise in fractures. This contrasts with other studies reporting a decrease in the number of hip and forearm fractures during the early phase of pandemic [34,35,36].
Different from literature data that describe the multiple vertebral fractures as the most typical presentation of rebound fractures [8, 9], the two fractures off-denosumab therapy recorded in our cohort were both localized at femoral neck. Recently, hip fractures were also reported in a small case series in this setting [37]. This is in line with previous larger observational studies which showed that loss of BMD during the off-treatment period is not only localized at the spine, but that hip BMD loss is equal to or even greater than the gain achieved during treatment [3]. Our finding might be also explained by the fact that vertebral fractures, in contrast to hip ones, are more often clinically silent and might remain undiagnosed if spinal X-rays are not performed [38].
The finding that diabetes mellitus was able to predict a new fracture confirms the increased risk of fractures in diabetic patients, already described in literature [39, 40]. Although it is logical to suppose a multifactorial nature of bone fragility in diabetes, the exact pathophysiology remains to be elucidated [40, 41].
Our study has several strengths and limitations. First, we believe that no selection bias is present since all patients who received a denosumab prescription at our Unit of Endocrinology during the period of study were included. Furthermore, our study is the first to provide information about the adherence rates to denosumab therapy and the reasons of non-adherence during pre-Covid-19 and pandemic years. On the other hand, information about the educational level of patients or the presence/absence of caregiver support is missing. Both these may have an impact on adherence, even though the fact that we did not find that age had an impact on adherence in our study mitigates the lack of the latter information. Data were collected using methods, such as conducting interviews and surveys, that may be hampered by reporting biases, missing data, and inaccurate recall by patients. However, it is unlikely that patients who regularly underwent medical visits or contacted our Unit (by phone or e-mail) in case of impossibility to travel during the lockdown, were non-adherent to therapy. Therefore, we specifically investigated medical conditions inducing bone loss, such as diabetes or androgen-deprivation treatment, while a parameter for comorbidity in its entirety (e.g., frailty index, Charlson comorbidity index) is lacking. In literature, there are other ways to measure adherence to drugs which, however, are not considered appropriate in the case of denosumab. For example, proportion of days covered (PDC) is calculated as the total number of days covered by the medication, divided by the number of days in the period for the individual patient [19]. Hence, a patient who is on time for one injection but delays the next one by 2 months will have the same PDC as someone who delays both injections by 1 month each, but the two patients will likely have differing risks of rebound bone loss and fractures. Finally, considering that rebound fractures are not so common, a larger sample size would have been more adequate for this endpoint.
In conclusion, our study shows that the COVID-19 pandemic has negatively impacted on clinical outcomes of osteoporotic patients with ongoing denosumab treatment, revealing a higher prevalence of non-adherent patients and a higher number of new non-traumatic fractures (including rebound fractures) during the lockdown period in comparison to the pre-COVID-19 period, regardless of the modality of medical evaluation. Hence, tele-medicine seems to be an alternative strategy to standard face-to-face visits in guaranteeing the continuity of follow-up in osteoporotic patients and short-term compliance to denosumab.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Reid IR, Billington EO (2022) Drug therapy for osteoporosis in older adults. Lancet 399:1080–1092
Vilaca T, Eastell R, Schini M (2022) Osteoporosis in men. Lancet Diabetes Endocrinol 10:273–283
Tsourdi E, Langdahl B, Cohen-Solal M, Aubry-Rozier B, Eriksen EF et al (2017) Discontinuation of denosumab therapy for osteoporosis: a systematic review and position statement by ECTS. Bone 105:11–17
Tripto-Shkolnik L, Fund N, Rouach V, Chodick G, Shalev V et al (2020) Fracture incidence after denosumab discontinuation: real-world data from a large healthcare provider. Bone 130:115150
Bone HG, Bolognese MA, Yuen CK, Kendler DL, Miller PD et al (2011) Effects of denosumab treatment and discontinuation on bone mineral density and bone turnover markers in postmenopausal women with low bone mass. J Clin Endocrinol Metab 96:972–980
Miller PD, Bolognese MA, Lewiecki EM, McClung MR, Ding B et al (2008) Effect of denosumab on bone density and turnover in postmenopausal women with low bone mass after long-term continued, discontinued, and restarting of therapy: a randomized blinded phase 2 clinical trial. Bone 43:222–229
Anastasilakis AD, Makras P, Yavropoulou MP, Tabacco G, Naciu AM et al (2021) Denosumab discontinuation and the rebound phenomenon: a narrative review. J Clin Med 10:152
Anastasilakis AD, Polyzos SA, Makras P, Aubry-Rozier B, Kaouri S et al (2017) Clinical features of 24 patients with rebound-associated vertebral fractures after denosumab discontinuation: systematic review and additional cases. J Bone Miner Res 32:1291–1296
Burckhardt P, Faouzi M, Buclin T, Lamy O (2021) Fractures after denosumab discontinuation: a retrospective study of 797 cases. J Bone Miner Res 36:1717–1728
McClung MR, Wagman RB, Miller PD, Wang A, Lewiecki EM (2017) Observations following discontinuation of long-term denosumab therapy. Osteoporos Int 28:1723–1732
Yu EW, Tsourdi E, Clarke BL, Bauer DC, Drake MT (2020) Osteoporosis management in the era of COVID-19. J Bone Miner Res 1009–1013
Rosenbaum L (2020) The untold toll—the pandemic’s effects on patients without Covid-19. N Engl J Med 382:2368–2371
Zou J, Song DW, Niu JJ, Shi JW, Yang HL (2020) Standardized out-patient diagnosis and treatment process for osteoporosis clinics during the COVID-19 pandemic. Eur Rev Med Pharmacol Sci 24:5778–5782
Napoli N, Elderkin AL, Kiel DP, Khosla S (2020) Managing fragility fractures during the COVID-19 pandemic. Nat Rev Endocrinol 16:467–468
Girgis CM, Clifton-Bligh RJ (2020) Osteoporosis in the age of COVID-19. Osteoporos Int 31:1189–1191
Gittoes NJ, Criseno S, Appelman-Dijkstra NM, Bollerslev J, Canalis E et al (2020) Endocrinology in the time of Covid-19: management of calcium metabolic disorders and osteoporosis. Eur J Endocrinol 183:G57-g65
AIFA (2017) https://www.aifa.gov.it/sites/default/files/Determinazione_446-2017_agg_nota79.pdf
Silverman SL, Siris E, Belazi D, Recknor C, Papaioannou A et al (2018) Persistence at 24 months with denosumab among postmenopausal women with osteoporosis: results of a prospective cohort study. Arch Osteoporos 13:85
Siris ES, Selby PL, Saag KG, Borgström F, Herings RM et al (2009) Impact of osteoporosis treatment adherence on fracture rates in North America and Europe. Am J Med 122:S3-13
Tile L, Cheung AM (2020) Atypical femur fractures: current understanding and approach to management. Ther Adv Musculoskelet Dis 12:1759720x20916983
Vescini F, Attanasio R, Balestrieri A, Bandeira F, Bonadonna S et al (2016) Italian association of clinical endocrinologists (AME) position statement: drug therapy of osteoporosis. J Endocrinol Invest 39:807–834
Ceccato F, Voltan G, Sabbadin C, Camozzi V, Merante Boschin I et al (2021) Tele-medicine versus face-to-face consultation in Endocrine Outpatients Clinic during COVID-19 outbreak: a single-center experience during the lockdown period. J Endocrinol Invest 44:1689–1698
Chandran M, Hao Y, Kwee AK, Cheen MHH, Chin YA et al (2022) Adherence to dosing schedule of denosumab therapy for osteoporosis during COVID-19 lockdown: an electronic medical record and pharmacy claims database study from Asia. Osteoporos Int 33:251–261
van Boven JF, de Boer PT, Postma MJ, Vegter S (2013) Persistence with osteoporosis medication among newly-treated osteoporotic patients. J Bone Miner Metab 31:562–570
Briesacher BA, Andrade SE, Fouayzi H, Chan KA (2008) Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacotherapy 28:437–443
Lekkerkerker F, Kanis JA, Alsayed N, Bouvenot G, Burlet N et al (2007) Adherence to treatment of osteoporosis: a need for study. Osteoporos Int 18:1311–1317
Tremblay É, Perreault S, Dorais M (2016) Persistence with denosumab and zoledronic acid among older women: a population-based cohort study. Arch Osteoporos 11:30
Fahrleitner-Pammer A, Papaioannou N, Gielen E, Feudjo Tepie M, Toffis C et al (2017) Factors associated with high 24-month persistence with denosumab: results of a real-world, non-interventional study of women with postmenopausal osteoporosis in Germany, Austria, Greece, and Belgium. Arch Osteoporos 12:58
Arafa M, Nesar S, Abu-Jabeh H, Jayme MOR, Kalairajah Y (2020) COVID-19 pandemic and hip fractures: impact and lessons learned. Bone Jt Open 1:530–540
Dolci A, Marongiu G, Leinardi L, Lombardo M, Dessì G et al (2020) The Epidemiology of fractures and muskulo-skeletal traumas during COVID-19 lockdown: a detailed survey of 17591 patients in a Wide Italian Metropolitan Area. Geriatr Orthop Surg Rehabil 11:2151459320972673
Minisola S, Cipriani C, Vigna E, Sonato C, Colangelo L, et al. (2022) COVID pandemic and denosumab adherence. In: Osteoporos Int. 943–944.
Ross S, Samuels E, Gairy K, Iqbal S, Badamgarav E et al (2011) A meta-analysis of osteoporotic fracture risk with medication nonadherence. Value Health 14:571–581
Lyu H, Yoshida K, Zhao SS, Wei J, Zeng C et al (2020) Delayed denosumab injections and fracture risk among patients with osteoporosis : a population-based cohort study. Ann Intern Med 173:516–526
Ciatti C, Maniscalco P, Quattrini F, Gattoni S, Magro A et al (2021) The epidemiology of proximal femur fractures during COVID-19 emergency in Italy: a multicentric study. Acta Biomed 92:e2021398
Wilk R, Adamczyk P, Pluskiewicz W, Skrzypek M, Hajzyk M et al (2022) One year of the COVID-19 pandemic in Poland—the incidence of osteoporotic forearm, arm, and hip fractures. Arch Osteoporos 17:38
Malik-Tabassum K, Crooks M, Robertson A, To C, Maling L et al (2020) Management of hip fractures during the COVID-19 pandemic at a high-volume hip fracture unit in the United Kingdom. J Orthop 20:332–337
Sosa Henríquez M, de Tejada G, Romero MJ, Escudero-Socorro M, Torregrosa Suau O (2019) Hip fractures following denosumab discontinuation: three clinical cases reports. J R Soc Med 112:472–475
Pizzato S, Trevisan C, Lucato P, Girotti G, Mazzochin M et al (2018) Identification of asymptomatic frailty vertebral fractures in post-menopausal women. Bone 113:89–94
Kurra S, Fink DA, Siris ES (2014) Osteoporosis-associated fracture and diabetes. Endocrinol Metab Clin North Am 43:233–243
Hofbauer LC, Busse B, Eastell R, Ferrari S, Frost M et al (2022) Bone fragility in diabetes: novel concepts and clinical implications. Lancet Diabetes Endocrinol 10:207–220
Ferrari SL, Abrahamsen B, Napoli N, Akesson K, Chandran M et al (2018) Diagnosis and management of bone fragility in diabetes: an emerging challenge. Osteoporos Int 29:2585–2596
Funding
No funds, Grants, or other support was received.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by SV, DD, BM, and VR. The first draft of the manuscript was written by SV and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was conducted in accordance with the ethical standards of the Helsinki Declaration (1975, revised in 2013) and the study protocol was approved by the North Emilia Vast Area (AVEN) Ethics Committee (protocol number AOU 0036075/21).
Consent to participate
In view of the retrospective nature of the study, Informed Consent was waived by the AVEN Ethics Committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
De Vincentis, S., Domenici, D., Ansaloni, A. et al. COVID-19 lockdown negatively impacted on adherence to denosumab therapy: incidence of non-traumatic fractures and role of telemedicine. J Endocrinol Invest 45, 1887–1897 (2022). https://doi.org/10.1007/s40618-022-01820-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-022-01820-8